pain
Multiple sclerosis (MS) causes a range of different symptoms. Patients with MS have looked for alternative therapies to control their MS progress and treat their symptoms. Non-invasive therapeutic approaches such as massage can have benefits to mitigate some of these symptoms. However, there is no rigorous review of massage effectiveness for patients suffering from MS.
The present systematic review was aimed at examining the effectiveness of different massage approaches on common MS symptoms, including fatigue, pain, anxiety, depression, and spasticity.
A total of 12 studies met the inclusion criteria. The authors rated 5 studies as being of fair and 7 studies of good methodological quality. Fatigue was improved by different massage styles, such as reflexology, nonspecific therapeutic massage, and Swedish massage. Pain, anxiety, and depression were effectively improved by reflexology techniques. Spasticity was reduced by Swedish massage and reflexology techniques.
The authors concluded that different massage approaches effectively improved MS symptoms such as fatigue, pain, anxiety, depression, and spasticity.
Clinical trials of massage therapy face formidable obstacles including:
- difficulties in obtaining funding,
- difficulties in finding expert researchers who are interested in the subject,
- difficulties to control for placebo effects,
- difficulties in blinding patients,
- impossibility of blinding therapists,
- confusion about the plethora of different massage techniques.
Thus, the evidence is often less convincing than one would hope. This, however, does not mean that massage therapy does not have considerable potential for a range of indications. One could easily argue that this situation is similar to spinal manipulation. Yet, there are at least three important differences:
- massage therapy is not as heavily burdened with frequent adverse effects and potentially life-threatening complications,
- massage therapy has a rational basis,
- the existing evidence is more uniformly encouraging.
Consequently, massage therapy (particularly, classic or Swedish massage) is more readily being accepted even in the absence of solid evidence. In fact, in some countries, e.g. Germany and Austria, massage therapy is considered to be a conventional treatment.
Spinal manipulation therapy (SMT) is widely used worldwide to treat musculoskeletal and many other conditions. The evidence that it works for any of them is weak, non-existent, or negative. What is worse, SMT can – as we have discussed so often on this blog – cause adverse events some of which are serious, even fatal.
Spinal epidural hematoma (SEH) caused by SMT is a rare emergency that can cause neurological dysfunction. Chinese researchers recently reported three cases of SEH after SMT. 
- The first case was a 30-year-old woman who experienced neck pain and numbness in both upper limbs immediately after SMT. Her symptoms persisted after 3 d of conservative treatment, and she was admitted to our hospital. Magnetic resonance imaging (MRI) demonstrated an SEH, extending from C6 to C7.
- The second case was a 55-year-old man with sudden back pain 1 d after SMT, numbness in both lower limbs, an inability to stand or walk, and difficulty urinating. MRI revealed an SEH, extending from T1 to T3.
- The third case was a 28-year-old man who suddenly developed symptoms of numbness in both lower limbs 4 h after SMT. He was unable to stand or walk and experienced mild back pain. MRI revealed an SEH, extending from T1 to T2.
All three patients underwent surgery after failed conservative treatment and all recovered to ASIA grade E on day 5, 1 wk, and day 10 after surgery, respectively. All patients returned to normal after 3 mo of follow-up.
The authors concluded that SEH caused by SMT is very rare, and the condition of each patient should be evaluated in full detail before operation. SEH should be diagnosed immediately and actively treated by surgery.
These cases might serve as an apt reminder of the fact that SMT (particularly SMT of the neck) is not without its dangers. The authors’ assurance that SEH is VERY RARE is a little puzzling, in my view (the paper includes a table with all 17 previously published cases). There is, as we often have mentioned, no post-marketing surveillance, surgeons only see those patients who survive such complications long enough to come to the hospital, and they publish such cases only if they feel like it. Consequently, the true incidence is anyone’s guess.
As pointed out earlier, the evidence that SMT might be effective is shaky for most indications. In view of the potential for harm, this can mean only one thing:
The risk/benefit balance for SMT is not demonstrably positive.
In turn, this leads to the conclusion that patients should think twice before having SMT and should inquire about other therapeutic options that have a more positive risk/benefit balance. Similarly, the therapists proposing SMT to a patient have the ethical and moral duty to obtain fully informed consent which includes information about the risk/benefit balance of SMT and other options.
These days, I live in France (some of my time) and I am often baffled by the number of osteopaths and the high level of acceptance of osteopathy in this country. The public seems to believe everything osteopaths claim and even most doctors have long given up to object to the idiocies they proclaim.
The website of the Institute of Osteopathy in Renne is but one of many examples. The Institute informed us as follows (my translation):
In addition to back pain, the osteopath can act on functional disorders of the digestive, neurological, cardiovascular systems or conditions related to ear, nose and throat. Osteopaths can promote recovery in athletes, relieve migraines, musculoskeletal disorders such as tendonitis, or treat sleep disorders. Less known for its preventive aspect, osteopathy also helps maintain good health. It can be effective even when everything is going well because it will prevent the appearance of pain. Osteopathy is, in fact, a manual medicine that allows the rebalancing of the major systems of the body, whatever the age of the patient and his problems. The osteopath looks for the root cause of your complaint in order to develop a curative and preventive treatment.
Who are osteopathic consultations for?
Osteopathic consultations at the Institute of Osteopathy of Rennes-Bretagne are intended for the following types of patients and pathologies
BABY / CHILD
GERD (gastric reflux), plagiocephaly (cranial deformities), recurrent ENT disorders (sinusitis, ear infections…), digestive, sleep and behavioural disorders, motor delay, following a difficult birth…
ADULT
Prevention, comfort treatment of osteoarthritis, musculoskeletal pain, functional abdominal pain, digestive disorders, headaches, dizziness, postural deficiency, facial pains…
PREGNANT WOMAN
Musculoskeletal pain (lumbago, back pain), digestive disorders, preparation for childbirth, post-partum check-up.
COMPANY
Prevention and treatment of MSDs (musculoskeletal disorders) linked to workstation ergonomics, stress, pain due to repetitive movements, poor posture at work, etc.
ADOLESCENT
Scoliosis, prevention of certain pathologies linked to growth, fatigue, stress, follow-up of orthodontic treatment.
SPORTSMAN
Musculoskeletal pain, tendonitis, osteopathic preparation for competition, osteopathic assessment according to the sport practised, repetitive injury.
In case you are not familiar with the evidence for osteopathy, let me tell you that as good as none of the many claims made in the above text is supported by anything that even resembles sound evidence.
So, how can we explain that, in France, osteopathy is allowed to thrive in a virtually evidence-free space?
In France, osteopathy started developing in the 1950s. In 2002, osteopathy received legislative recognition in France, and today, it is booming; between 2016 and 2018, 3589 osteopaths were trained in France. Osteopaths can be DO doctors, DO physiotherapists, DO nurses, DO midwives, DO chiropodists, or even DO dentists.
Thus, in 2018, and out of a total of 29,612 professionals practising osteopathy, there were 17,897 osteopaths DO and 11,715 DO health professionals. The number of professionals using the title of osteopath has roughly tripled in 8 years (11608 in 2010 for 29612 in 2018). There are currently around 30 osteopathic schools in France. About 3 out of 5 French people now consult osteopaths.
But this does not answer my question why, in France, osteopathy is allowed to thrive in a virtually evidence-free space! To be honest, I do not know its answer.
Perhaps someone else does?
If so, please enlighten me.
Myofascial release (also known as myofascial therapy or myofascial trigger point therapy) is a type of low-load stretch therapy that is said to release tightness and pain throughout the body caused by the myofascial pain syndrome, a chronic muscle pain that is worse in certain areas known as trigger points. Various types of health professionals provide myofascial release, e.g. osteopaths, chiropractors, physical or occupational therapists, massage therapists, or sports medicine/injury specialists. The treatment is usually applied repeatedly, but there is also a belief that a single session of myofascial release is effective. This study was a crossover clinical trial aimed to test whether a single session of a specific myofascial release technique reduces pain and disability in subjects with chronic low back pain (CLBP).
A total of 41 participants were randomly enrolled into 3 situations in a balanced and crossover manner:
- experimental,
- placebo,
- control.
The subjects underwent a single session of myofascial release on thoracolumbar fascia and the results were compared with the control and placebo groups. A single trained and experienced therapist applied the technique.
For the control treatment, the subjects were instructed to remain in the supine position for 5 minutes. For the muscle release session, the subjects were in a sitting position with feet supported and the thoracolumbar region properly undressed. The trunk flexion goniometry of each participant was performed and the value of 30° was marked with a barrier to limit the necessary movement during the technique. The trained researcher positioned their hands on all participants without sliding over the skin or forcing the tissue, with the cranial hand close to the last rib and at the T12–L1 level on the right side of the individual’s body and the caudal hand on the ipsilateral side between the iliac crest and the sacrum. Then, the researcher caused slight traction in the tissues by moving their hands away from each other in a longitudinal direction. Then, the participant was instructed to perform five repetitions of active trunk flexion-extension (30°), while the researcher followed the movement with both hands simultaneously positioned, without losing the initial tissue traction and position. The same technique and the same number of repetitions of active trunk flexion-extension were repeated with the researcher’s hands positioned on the opposite sides. This technique lasted approximately five minutes.
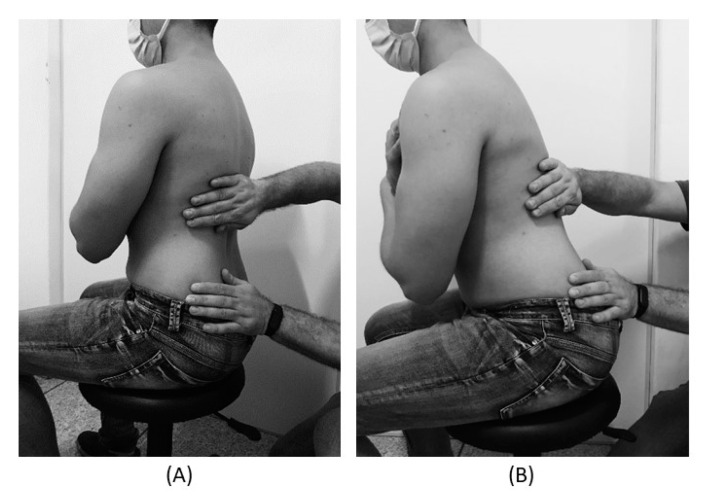
For the placebo treatment, the subjects were not submitted to the technique of manual thoracolumbar fascia release, but they slowly performed ten repetitions of active trunk flexion-extension (30°) in the same position as the experimental situation. Due to the fact that touch can provide not only well-recognized discriminative input to the brain, but also an affective input, there was no touch from the researcher at this stage.
The outcomes, pain, and functionality, were evaluated using the numerical pain rating scale (NPRS), pressure pain threshold (PPT), and Oswestry Disability Index (ODI).
The results showed no effects between-tests, within-tests, nor for interaction of all the outcomes, i.e., NPRS (η 2 = 0.32, F = 0.48, p = 0.61), PPT (η2 = 0.73, F = 2.80, p = 0.06), ODI (η2 = 0.02, F = 0.02, p = 0.97).
The authors concluded that a single trial of a thoracolumbar myofascial release technique was not enough to reduce pain intensity and disability in subjects with CLBP.
Surprised?
I’m not!
Recently, I received this comment from a reader:
Edzard-‘I see you do not understand much of trial design’ is true BUT I wager that you are in the same boat when it comes to a design of a trial for LBP treatment: not only you but many other therapists. There are too many variables in the treatment relationship that would allow genuine , valid criticism of any design. If I have to pick one book of the several listed elsewhere I choose Gregory Grieve’s ‘Common Vertebral Joint Problems’. Get it, read it, think about it and with sufficient luck you may come to realize that your warranted prejudices against many unconventional ‘medical’ treatments should not be of the same strength when it comes to judging the physical therapy of some spinal problems as described in the book.
And a chiro added:
EE: I see that you do not understand much of trial design
Perhaps it’s Ernst who doesnt understand how to research back pain.
“The identification of patient subgroups that respond best to specific interventions has been set as a key priority in LBP research for the past 2 decades.2,7 In parallel, surveys of clinicians managing LBP show that there are strong views against generic treatment and an expectation that treatment should be individualized to the patient.6,22.”
Journal of Orthopaedic & Sports Physical Therapy
Published Online:January 31, 2017Volume47Issue2Pages44-48
Do I need to explain why the Grieve book (yes, I have it and yes, I read it) is not a substitute for evidence that an intervention or technique is effective? No, I didn’t think so. This needs to come from a decent clinical trial.
And how would one design a trial of LBP (low back pain) that would be a meaningful first step and account for the “many variables in the treatment relationship”?
How about proceeding as follows (the steps are not necessarily in that order):
- Study the previously published literature.
- Talk to other experts.
- Recruit a research team that covers all the expertise you need (and don’t have yourself).
- Formulate your research question. Mine would be IS THERAPY XY MORE EFFECTIVE THAN USUAL CARE FOR CHRONIC LBP? I know LBP is but a vague symptom. This does, however, not necessarily matter (see below).
- Define primary and secondary outcome measures, e.g. pain, QoL, function, as well as the validated methods with which they will be quantified.
- Clarify the method you employ for monitoring adverse effects.
- Do a small pilot study.
- Involve a statistician.
- Calculate the required sample size of your study.
- Consider going multi-center with your trial if you are short of patients.
- Define chronic LBP as closely as you can. If there is evidence that a certain type of patient responds better to the therapy xy than others, that might be considered in the definition of the type of LBP.
- List all inclusion and exclusion criteria.
- Make sure you include randomization in the design.
- Randomization should be to groups A and B. Group A receives treatment xy, while group B receives usual care.
- Write down what A and B should and should not entail.
- Make sure you include blinding of the outcome assessors and data evaluators.
- Define how frequently the treatments should be administered and for how long.
- Make sure all therapists employed in the study are of a high standard and define the criteria of this standard.
- Train all therapists of both groups such that they provide treatments that are as uniform as possible.
- Work out a reasonable statistical plan for evaluating the results.
- Write all this down in a protocol.
Such a trial design does not need patient or therapist blinding nor does it require a placebo. The information it would provide is, of course, limited in several ways. Yet it would be a rigorous test of the research question.
If the results of the study are positive, one might consider thinking of an adequate sham treatment to match therapy xy and of other ways of firming up the evidence.
As LBP is not a disease but a symptom, the study does not aim to include patients that all are equal in all aspects of their condition. If some patients turn out to respond better than others, one can later check whether they have identifiable characteristics. Subsequently, one would need to do a trial to test whether the assumption is true.
Therapy xy is complex and needs to be tailored to the characteristics of each patient? That is not necessarily an unsolvable problem. Within limits, it is possible to allow each therapist the freedom to chose the approach he/she thinks is optimal. If the freedom needed is considerable, this might change the research question to something like ‘IS THAT TYPE OF THERAPIST MORE EFFECTIVE THAN THOSE EMPLOYING USUAL CARE FOR CHRONIC LBP?’
My trial would obviously not answer all the open questions. Yet it would be a reasonable start for evaluating a therapy that has not yet been submitted to clinical trials. Subsequent trials could build on its results.
I am sure that I have forgotten lots of details. If they come up in discussion, I can try to incorporate them into the study design.
Acupuncture is a veritable panacea; it cures everything! At least this is what many of its advocates want us to believe. Does it also have a role in supportive cancer care?
Let’s find out.
This systematic review evaluated the effects of acupuncture in women with breast cancer (BC), focusing on patient-reported outcomes (PROs).
A comprehensive literature search was carried out for randomized controlled trials (RCTs) reporting PROs in BC patients with treatment-related symptoms after undergoing acupuncture for at least four weeks. Literature screening, data extraction, and risk bias assessment were independently carried out by two researchers. The authors stated that they followed the ‘Preferred Reporting Items for Systematic Review and Meta-Analyses’ (PRISMA) guidelines.
Out of the 2, 524 identified studies, 29 studies representing 33 articles were included in this meta-analysis. The RCTs employed various acupuncture techniques with a needle, such as hand-acupuncture and electroacupuncture. Sham/placebo acupuncture, pharmacotherapy, no intervention, or usual care were the control interventions. About half of the studies lacked adequate blinding.
At the end of treatment (EOT), the acupuncture patients’ quality of life (QoL) was measured by the QLQ-C30 QoL subscale, the Functional Assessment of Cancer Therapy-Endocrine Symptoms (FACT-ES), the Functional Assessment of Cancer Therapy–General/Breast (FACT-G/B), and the Menopause-Specific Quality of Life Questionnaire (MENQOL), which depicted a significant improvement. The use of acupuncture in BC patients lead to a considerable reduction in the scores of all subscales of the Brief Pain Inventory-Short Form (BPI-SF) and Visual Analog Scale (VAS) measuring pain. Moreover, patients treated with acupuncture were more likely to experience improvements in hot flashes scores, fatigue, sleep disturbance, and anxiety compared to those in the control group, while the improvements in depression were comparable across both groups. Long-term follow-up results were similar to the EOT results. Eleven RCTs did not report any information on adverse effects.
The authors concluded that current evidence suggests that acupuncture might improve BC treatment-related symptoms measured with PROs including QoL, pain, fatigue, hot flashes, sleep disturbance and anxiety. However, a number of included studies report limited amounts of certain subgroup settings, thus more rigorous, well-designed and larger RCTs are needed to confirm our results.
This review looks rigorous on the surface but has many weaknesses if one digs only a little deeper. To start with, it has no precise research question: is any type of acupuncture better than any type of control? This is not a research question that anyone can answer with just a few studies of mostly poor quality. The authors claim to follow the PRISMA guidelines, yet (as a co-author of these guidelines) I can assure you that this is not true. Many of the included studies are small and lacked blinding. The results are confusing, contradictory and not clearly reported. Many trials fail to mention adverse effects and thus violate research ethics, etc., etc.
The conclusion that acupuncture might improve BC treatment-related symptoms could be true. But does this paper convince me that acupuncture DOES improve these symptoms?
No!
This study describes the use of so-called alternative medicine (SCAM) among older adults who report being hampered in daily activities due to musculoskeletal pain. Cross-sectional European Social Survey (EES) Round 7 (2014) data from 21 countries were examined for participants aged 55 years and older, who reported musculoskeletal pain that hampered daily activities in the past 12months. From a total of 35,063 individuals who took part in the ESS study, 13,016 (37%) were aged 55 or older; of which 8183 (63%) reported the presence of pain, with a further 4950 (38%) reporting that this pain hampered their daily activities in any way.
Of the 4950 older adult participants reporting musculoskeletal pain that hampered daily activities, the majority (63.5%) were from the West of Europe, reported secondary education or less (78.2%), and reported at least one other health-related problem (74.6%). In total, 1657 (33.5%) reported using at least one SCAM treatment in the previous year. Manual body-based therapies (MBBTs) were most used, including massage therapy (17.9%) and osteopathy (7.0%). Alternative medicinal systems (AMSs) were also popular with 6.5% using homeopathy and 5.3% reporting herbal treatments. A general trend of higher SCAM use in younger participants was noted.
SCAM usage was associated with
- physiotherapy use,
- female gender,
- higher levels of education,
- being in employment,
- living in West Europe
- having multiple health problems.
The authors concluded that a third of older Europeans with musculoskeletal pain report SCAM use in the previous
12 months. Certain subgroups with higher rates of SCAM use could be identified. Clinicians should comprehensively and routinely assess SCAM use among older adults with musculoskeletal pain.
Such studies have the advantage of large sample sizes, and therefore one is inclined to consider their findings to be reliable and informative. Yet, they resemble big fishing operations where all sorts of important and unimportant stuff is caught in the net. When studying such papers, it is wise to remember that associations do not necessarily reveal causal relationships!
Having said this, I find very little information in these already outdated results (they originate from 2014!) that I would not have expected. Perhaps the most interesting aspect is the nature of the most popular SCAMs used for musculoskeletal problems. The relatively high usage of MBBTs had to be expected; in most of the surveyed countries, massage therapy is considered to be not SCAM but mainstream. The fact that 6.5% used homeopathy to ease their musculoskeletal pain is, however, quite remarkable. I know of no good evidence to show that homeopathy is effective for such problems (in case some homeopathy fans disagree, please show me the evidence).
In my view, this indicates that, in 2014, much needed to be done in terms of informing the public about homeopathy. Many consumers mistook homeopathy for herbal medicine (which btw may well have some potential for musculoskeletal pain), and many consumers had been misguided into believing that homeopathy works. They had little inkling that homeopathy is pure placebo therapy. This means they mistreated their conditions, continued to suffer needlessly, and caused an unnecessary financial burden to themselves and/or to society.
Since 2014, much has happened (as discussed in uncounted posts on this blog), and I would therefore assume that the 6.5% figure has come down significantly … but, as you know:
I am an optimist.
I believe in progress.
Homeopathy is sometimes claimed to be effective for primary dysmenorrhoea (PD), but the claim is not supported by sound evidence. This study was undertaken to examine the efficacy of individualized homeopathic medicines (IH) against placebo in the treatment of PD.
A double-blind, randomized, placebo-controlled trial was conducted at the gynecology outpatient department of Mahesh Bhattacharyya Homoeopathic Medical College and Hospital, West Bengal, India. Patients were randomized to receive either IH (n=64) or identical-looking placebo (n=64). Primary and secondary outcome measures were 0-10 numeric rating scales (NRS) measuring the intensity of pain of dysmenorrhea and verbal multidimensional scoring system (VMSS) respectively, all measured at baseline, and every month, up to 3 months.
The two groups were comparable at baseline. The attrition rate was 10.9% (IH: 7, placebo: 7). Differences between groups in both pain NRS and VMSS favored IH over placebo at all time points with medium to large effect sizes. Natrum muriaticum and Pulsatilla nigricans were the most frequently prescribed medicines. No harms, serious adverse events, or intercurrent illnesses were recorded in either group.
The authors concluded that homeopathic medicines acted significantly better than placebo in the treatment of PD. Independent replication is warranted.
A previously published RCT could not show any significant effect of homeopathy on primary dysmenorrhea in comparison with placebo. The authors of the new study claim that the discrepant findings might be due to the fact that IH requires great skill. In other words, negative studies are according to this explanation negative not because homeopathy does not work but because the prescribers are not up to it. Such notions have often been voiced on this blog and elsewhere and are used as a veritable ‘get-out clause’ for homeopathy: ONLY THE POSITIVE RESULTS ARE VALID! Consequently, systematic reviews of the evidence must only consider positive trials. And this, of course, means that the findings are invariable positive.
I find this more than a little naive and would much prefer to wait for an independent replication where ‘independent’ means that the trial is run by experts who are not advocates of homeopathy (as in the present trial).
I have reported about the risks of chiropractic manipulation many times before. This is not because, as some seem to believe, I have an axe to grind but because the subject is important. This week, another case of stroke after chiropractic manipulation was in the news. Some will surely say that it is alarmist to mention such reports which lack lots of crucial details. Yet, as long as chiropractors do not establish a proper monitoring system where serious adverse effects of spinal manipulation are noted, I think it is important to record even incomplete cases in this fashion.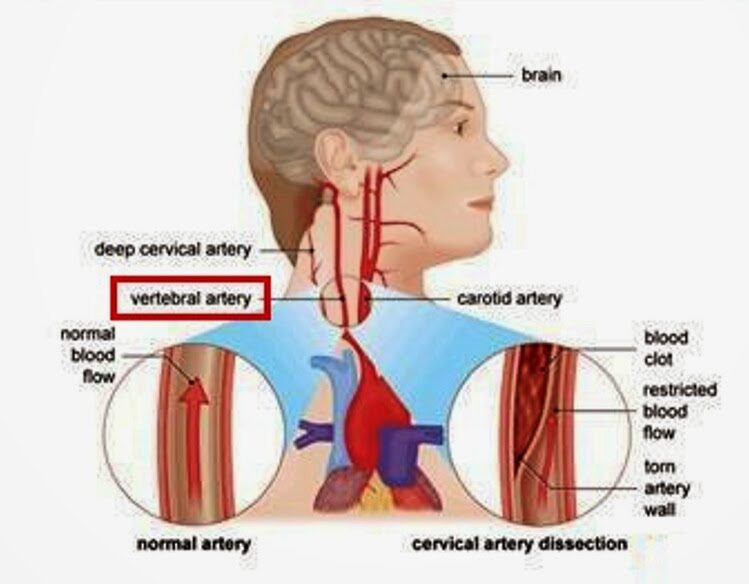
Barbara Shand is a working mom who lives in Alberta, Canada. She went to see a chiropractor because she had neck pain. “Near the very end of the appointment, the chiropractor asked: ‘Do you want your neck adjusted?’ I said: ‘Sure.’” “As soon as she did it, everything went black,” Shand recalls.
The patient was then rushed to a hospital by ambulance. “When I did open my eyes, I couldn’t focus. It was all blurry, I had massive vertigo, I didn’t know what was up or down,” Shand told the journalist. The diagnosis, Shand explains, was a right vertebral artery dissection, followed by a stroke. Mrs. Sands continues to struggle with coordination and balance.
The Alberta College and Association of Chiropractors acknowledges “there have been reported cases of stroke associated with visits to various healthcare practitioners, including those that provide cervical spine manipulation.” But they claim it is rare. They did not comment on the informed consent which, according to Shand’s description, was more than incomplete.
The fact that the ACAC admits that such events have happened before is laudable and a step in the right direction (some chiropractic organizations don’t even go that far). Yet, their caveat that such cases are rare is problematic. Without a monitoring system, nobody can tell how frequent they are! What we do see is merely the tip of a much bigger iceberg. There have been hundreds of cases like Mrs. Shand. The truth of the matter is this: Chiropractic neck manipulations are not supported by sound evidence of effectiveness for any condition. This means that even rare risks (if they are truly rare) would tilt the risk/benefit balance into the negative.
The conclusion is, I think, to avoid neck manipulations at all costs. Or, as one neurologist once put it:
don’t let the buggars touch your neck!
A new study evaluated the effects of yoga and eurythmy therapy compared to conventional physiotherapy exercises in patients with chronic low back pain.
In this three-armed, multicentre, randomized trial, patients with chronic low back pain were treated for 8 weeks in group sessions (75 minutes once per week). They received either:
- Yoga exercises
- Eurythmy
- Physiotherapy
The primary outcome was patients’ physical disability (measured by RMDQ) from baseline to week 8. Secondary outcome variables were pain intensity and pain-related bothersomeness (VAS), health-related quality of life (SF-12), and life satisfaction (BMLSS). Outcomes were assessed at baseline, after the intervention at 8 weeks, and at a 16-week follow-up. Data of 274 participants were used for statistical analyses.
The results showed no significant differences between the three groups for the primary and secondary outcomes. In all groups, RMDQ decreased comparably at 8 weeks but did not reach clinical meaningfulness. Pain intensity and pain-related bothersomeness decreased, while the quality of life increased in all 3 groups. In explorative general linear models for the SF-12’s mental health component, participants in the eurythmy arm benefitted significantly more compared to physiotherapy and yoga. Furthermore, within-group analyses showed improvements of SF-12 mental score for yoga and eurythmy therapy only. All interventions were safe.
Everyone knows what physiotherapy or yoga is, I suppose. But what is eurythmy?
It is an exercise therapy that is part of anthroposophic medicine. It consists of a set of specific movements that were developed by Rudolf Steiner (1861–1925), the inventor of anthroposophic medicine, in conjunction with Marie von Sievers (1867-1948), his second wife.
Steiner stated in 1923 that eurythmy has grown out of the soil of the Anthroposophical Movement, and the history of its origin makes it almost appear to be a gift of the forces of destiny. Steiner also wrote that it is the task of the Anthroposophical Movement to reveal to our present age that spiritual impulse that is suited to it. He claimed that, within the Anthroposophical Movement, there is a firm conviction that a spiritual impulse of this kind must enter once more into human evolution. And this spiritual impulse must perforce, among its other means of expression, embody itself in a new form of art. It will increasingly be realized that this particular form of art has been given to the world in Eurythmy.
Consumers learning eurythmy are taught exercises that allegedly integrate cognitive, emotional, and volitional elements. Eurythmy exercises are based on speech and direct the patient’s attention to their own perceived intentionality. Proponents of Eurythmy believe that, through this treatment, a connection between internal and external activity can be experienced. They also make many diffuse health claims for this therapy ranging from stress management to pain control.
There is hardly any reliable evidence for eurythmy, and therefore the present study is exceptional and noteworthy. One review concluded that “eurythmy seems to be a beneficial add-on in a therapeutic context that can improve the health conditions of affected persons. More methodologically sound studies are needed to substantiate this positive impression.” This positive conclusion is, however, of doubtful validity. The authors of the review are from an anthroposophical university in Germany. They included studies in their review that were methodologically too weak to allow any conclusions.
So, does the new study provide the reliable evidence that was so far missing? I am afraid not!
The study compared three different exercise therapies. Its results imply that all three were roughly equal. Yet, we cannot tell whether they were equally effective or equally ineffective. The trial was essentially an equivalence study, and I suspect that much larger sample sizes would have been required in order to identify any true differences if they at all exist. Lastly, the study (like the above-mentioned review) was conducted by proponents of anthroposophical medicine affiliated with institutions of anthroposophical medicine. I fear that more independent research would be needed to convince me of the value of eurythmy.
