pain
There is hardly a form of therapy under the SCAM umbrella that is not promoted for back pain. None of them is backed by convincing evidence. This might be because back problems are mostly viewed in SCAM as mechanical by nature, and psychological elements are thus often neglected.
This systematic review with network meta-analysis determined the comparative effectiveness and safety of psychological interventions for chronic low back pain. Randomised controlled trials comparing psychological interventions with any comparison intervention in adults with chronic, non-specific low back pain were included.
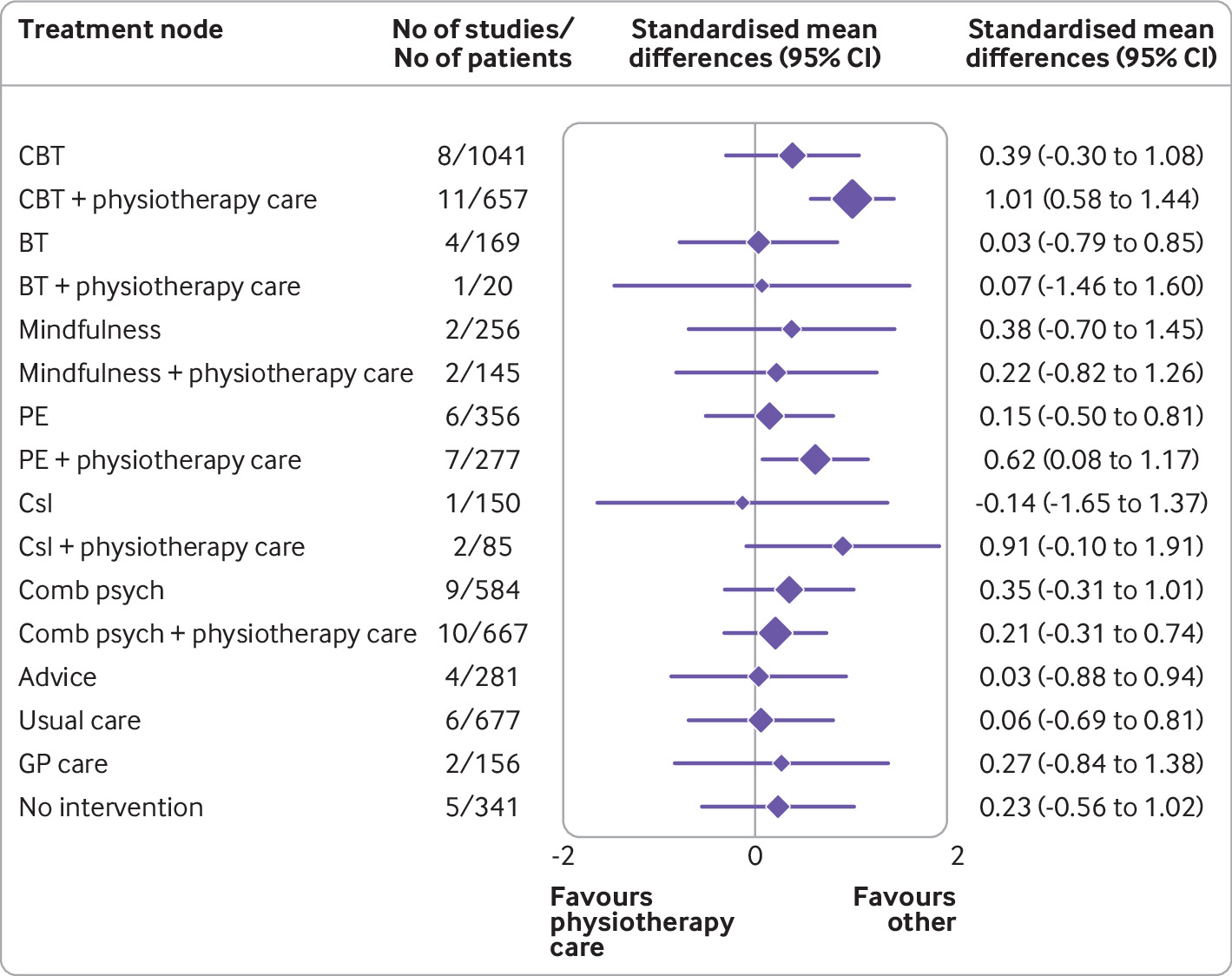
A total of 97 randomised controlled trials involving 13 136 participants and 17 treatment nodes were included. Inconsistency was detected at short term and mid-term follow-up for physical function, and short term follow-up for pain intensity, and were resolved through sensitivity analyses. For physical function, cognitive behavioural therapy (standardised mean difference 1.01, 95% confidence interval 0.58 to 1.44), and pain education (0.62, 0.08 to 1.17), delivered with physiotherapy care, resulted in clinically important improvements at post-intervention (moderate-quality evidence). The most sustainable effects of treatment for improving physical function were reported with pain education delivered with physiotherapy care, at least until mid-term follow-up (0.63, 0.25 to 1.00; low-quality evidence). No studies investigated the long term effectiveness of pain education delivered with physiotherapy care. For pain intensity, behavioural therapy (1.08, 0.22 to 1.94), cognitive behavioural therapy (0.92, 0.43 to 1.42), and pain education (0.91, 0.37 to 1.45), delivered with physiotherapy care, resulted in clinically important effects at post-intervention (low to moderate-quality evidence). Only behavioural therapy delivered with physiotherapy care maintained clinically important effects on reducing pain intensity until mid-term follow-up (1.01, 0.41 to 1.60; high-quality evidence).
Forest plot of network meta-analysis results for physical function at post-intervention. *Denotes significance at p<0.05. BT=behavioural therapy; CBT=cognitive behavioural therapy; Comb psych=combined psychological approaches; Csl=counselling; GP care=general practitioner care; PE=pain education; SMD=standardised mean difference. Physiotherapy care was the reference comparison group
The authors concluded that for people with chronic, non-specific low back pain, psychological interventions are most effective when delivered in conjunction with physiotherapy care (mainly structured exercise). Pain education programmes (low to moderate-quality evidence) and behavioural therapy (low to high-quality evidence) result in the most sustainable effects of treatment; however, uncertainty remains as to their long term effectiveness. Although inconsistency was detected, potential sources were identified and resolved.
The authors’ further comment that their review has identified that pain education, behavioural therapy, and cognitive behavioural therapy are the most effective psychological interventions for people with chronic, non-specific LBP post-intervention when delivered with physiotherapy care. The most sustainable effects of treatment for physical function and fear avoidance are achieved with pain education programmes, and for pain intensity, they are achieved with behavioural therapy. Although their clinical effectiveness diminishes over time, particularly in the long term (≥12 months post-intervention), evidence supports the clinical benefits of combining physiotherapy care with these specific types of psychological interventions at the onset of treatment. The small total sample size at long term follow-up (eg, for physical function, n=6986 at post-intervention v n=2469 for long term follow-up; for pain intensity, n=6963 v n=2272) has resulted in wide confidence intervals at this time point; however, the magnitude and direction of the pooled effects seemed to consistently favour the psychological interventions delivered with physiotherapy care, compared with physiotherapy care alone.
Commenting on their paper, two of the authors, Ferriera and Ho, said they would like to see the guidelines on LBP therapy updated to provide more specific recommendations, the “whole idea” is to inform patients, so they can have conversations with their GP or physiotherapist. Patients should not come to consultations with a passive attitude of just receiving whatever people tell them because unfortunately people still receive the wrong care for chronic back pain,” Ferreira says. “Clinicians prescribe anti-inflammatories or paracetamol. We need to educate patients and clinicians about options and more effective ways of managing pain.”
Is there a lesson here for patients consulting SCAM practitioners for their back pain? Perhaps it is this: it is wise to choose the therapy that has been demonstrated to be effective while having the least potential for harm! And this is not chiropractic or any other form of SCAM. It could, however, well be a combination of physiotherapeutic exercise and psychological therapy.
S-adenosyl methionine – SAMe for short – is a popular dietary supplement available freely via the Internet. It is a naturally occurring methyl radical donor involved in enzymatic transmethylation reactions in humans and animals. It has been used for treating postpartum depression, cholestatic jaundice, osteoarthritis, and numerous other conditions. SAM-e has poor oral bioavailability. SAM-e has so far been thought of as safe. The most frequent adverse effects reported were gastrointestinal, such as nausea, and skin rashes.
I have been involved in two systematic reviews that produced positive evidence for the effectiveness of SAMe:
- One review found “consistent evidence that … S-adenosyl methionine was effective in the management of osteoarthritis.”
- Another review showed that for fibromyalgia “the effects of … S-adenosylmethionine … showed at least one statistically significant improved outcome compared with placebo.”
Now the safety of SAMe has been questioned by new research. A team from Manchester and Kyoto universities reported that the supplement can break down inside the body into substances that cause a wide range of medical problems, including kidney and liver damage. Their study showed that “excess S-adenosylmethionine disrupts rhythms and, rather than promoting methylation, is catabolized to adenine and methylthioadenosine, toxic methylation inhibitors.”
Jean-Michel Fustin, of Manchester University, said experiments that he and his collaborators had carried out had revealed that SAMe breaks down into adenine and methylthioadenosine in the body. These substances are known to be toxic, he added. “This discovery came out of the blue,” Fustin said last week. “When we gave the supplement to mice we expected they would become healthier. But instead we found the opposite. We found that when SAMe breaks down in the body, it produces very toxic molecules, including adenine which causes gout, kidney disease and liver disease.” Fustin added that, although their study was carried out on mice, their results were relevant for humans. “We have not yet tested the supplement on men and women but we have added it to human cells in laboratory cultures and have found it had the same effect as it had on mice.”
Their study, which was funded by the Medical Research Council and the Japanese Society for the Promotion of Science, makes it clear that the health benefits of SAMe are questionable, to say the very least, Fustin added. “It is unclear what dose of it might be safe, so there is a good chance that a safe dose will be exceeded if someone takes this supplement – if a safe dose exists at all.”
This randomized, double-blind, placebo-controlled trial investigated whether homeopathic Hypericum leads to a reduction in postoperative pain and a decrease in pain medication compared with placebo. Inpatients undergoing lumbar sequestrectomy surgery were given the homeopathic treatment Hypericum C200 or a placebo in addition to usual pain management. The primary endpoint was pain relief measured with a visual analog scale. Secondary endpoints were the reduction of inpatient postoperative analgesic medication and change in sensory and affective pain perception.
The baseline characteristics were comparable between the two groups. Pain perception between baseline and day 3 did not significantly differ between the study arms. With respect to pain medication, total morphine equivalent doses did not differ significantly. However, a statistical trend and a moderate effect (d = 0.432) in the decrease of pain medication consumption in favor of the Hypericum group was observed.
The authors concluded that this is the first trial of homeopathy that evaluated the efficacy of Hypericum C200 after lumbar monosegmental spinal sequestrectomy. Although no significant differences between the groups could be shown, we found that patients who took potentiated Hypericum in addition to usual pain management showed lower consumption of analgesics. Further investigations, especially with regard to pain medication, should follow to better classify the described analgesic reduction.
I applaud the authors from the Institute of Integrative Medicine, Witten/Herdecke University, Herdecke, Germany (not an institution known for its objectivity in SCAM) to have published this negative study in a journal that is so clearly pro-SCAM that it very rarely contains anything in its pages that is not positive about SCAM. Yet, I am baffled by two things:
- The plant Hypericum is used in SCAM as a painkiller. According to the ‘like cures like’ axiom of homeopathy, it should thus INCREASE the pain of post-op patients.
- The researchers used a C 200 potency. I ask myself, how can anyone assume that such a dilution has any effect at all? C200 means that the plant tincture is diluted at a ratio of 1: 00000000000000000000 00000000000000000000 00000000000000000000 00000000000000000000 00000000000000000000 00000000000000000000 00000000000000000000 00000000000000000000 00000000000000000000 00000000000000000000 00000000000000000000 00000000000000000000 00000000000000000000 00000000000000000000 00000000000000000000 00000000000000000000 00000000000000000000 00000000000000000000 00000000000000000000 00000000000000000000. Less than one molecule of the plant per several universes!
To believe that such a dilution might work, one really needs to be a convinced disciple of Hahnemann. Yet, to disregard the ‘like cures like’ axiom, one needs to be what he called ‘a traitor’ to his true art of healing.
The Lancet is a top medical journal, no doubt. But even such journals can make mistakes, even big ones, as the Wakefield story illustrates. But sometimes, the mistakes are seemingly minor and so well hidden that the casual reader is unlikely to find them. Such mistakes can nevertheless be equally pernicious, as they might propagate untruths or misunderstandings that have far-reaching consequences.
A recent Lancet paper might be an example of this phenomenon. It is entitled “Management of common clinical problems experienced by survivors of cancer“, unquestionably an important subject. Its abstract reads as follows:
_______________________
Improvements in early detection and treatment have led to a growing prevalence of survivors of cancer worldwide.
Models of care fail to address adequately the breadth of physical, psychosocial, and supportive care needs of those who survive cancer. In this Series paper, we summarise the evidence around the management of common clinical problems experienced by survivors of adult cancers and how to cover these issues in a consultation. Reviewing the patient’s history of cancer and treatments highlights potential long-term or late effects to consider, and recommended surveillance for recurrence. Physical consequences of specific treatments to identify include cardiac dysfunction, metabolic syndrome, lymphoedema, peripheral neuropathy, and osteoporosis. Immunotherapies can cause specific immune-related effects most commonly in the gastrointestinal tract, endocrine system, skin, and liver. Pain should be screened for and requires assessment of potential causes and non-pharmacological and pharmacological approaches to management. Common psychosocial issues, for which there are effective psychological therapies, include fear of recurrence, fatigue, altered sleep and cognition, and effects on sex and intimacy, finances, and employment. Review of lifestyle factors including smoking, obesity, and alcohol is necessary to reduce the risk of recurrence and second cancers. Exercise can improve quality of life and might improve cancer survival; it can also contribute to the management of fatigue, pain, metabolic syndrome, osteoporosis, and cognitive impairment. Using a supportive care screening tool, such as the Distress Thermometer, can identify specific areas of concern and help prioritise areas to cover in a consultation.
_____________________________
You can see nothing wrong? Me neither! We need to dig deeper into the paper to find what concerns me.
In the actual article, the authors state that “there is good evidence of benefit for … acupuncture …”[1]; the same message was conveyed in one of the tables. In support of these categorical statements, the authors quote the current Cochrane review entitled “Acupuncture for cancer pain in adults”. Its abstract reads as follows:
Background: Forty per cent of individuals with early or intermediate stage cancer and 90% with advanced cancer have moderate to severe pain and up to 70% of patients with cancer pain do not receive adequate pain relief. It has been claimed that acupuncture has a role in management of cancer pain and guidelines exist for treatment of cancer pain with acupuncture. This is an updated version of a Cochrane Review published in Issue 1, 2011, on acupuncture for cancer pain in adults.
Objectives: To evaluate efficacy of acupuncture for relief of cancer-related pain in adults.
Search methods: For this update CENTRAL, MEDLINE, EMBASE, PsycINFO, AMED, and SPORTDiscus were searched up to July 2015 including non-English language papers.
Selection criteria: Randomised controlled trials (RCTs) that evaluated any type of invasive acupuncture for pain directly related to cancer in adults aged 18 years or over.
Data collection and analysis: We planned to pool data to provide an overall measure of effect and to calculate the number needed to treat to benefit, but this was not possible due to heterogeneity. Two review authors (CP, OT) independently extracted data adding it to data extraction sheets. Data sheets were compared and discussed with a third review author (MJ) who acted as arbiter. Data analysis was conducted by CP, OT and MJ.
Main results: We included five RCTs (285 participants). Three studies were included in the original review and two more in the update. The authors of the included studies reported benefits of acupuncture in managing pancreatic cancer pain; no difference between real and sham electroacupuncture for pain associated with ovarian cancer; benefits of acupuncture over conventional medication for late stage unspecified cancer; benefits for auricular (ear) acupuncture over placebo for chronic neuropathic pain related to cancer; and no differences between conventional analgesia and acupuncture within the first 10 days of treatment for stomach carcinoma. All studies had a high risk of bias from inadequate sample size and a low risk of bias associated with random sequence generation. Only three studies had low risk of bias associated with incomplete outcome data, while two studies had low risk of bias associated with allocation concealment and one study had low risk of bias associated with inadequate blinding. The heterogeneity of methodologies, cancer populations and techniques used in the included studies precluded pooling of data and therefore meta-analysis was not carried out. A subgroup analysis on acupuncture for cancer-induced bone pain was not conducted because none of the studies made any reference to bone pain. Studies either reported that there were no adverse events as a result of treatment, or did not report adverse events at all.
Authors’ conclusions: There is insufficient evidence to judge whether acupuncture is effective in treating cancer pain in adults.
This conclusion is undoubtedly in stark contrast to the categorical statement of the Lancet authors: “there is good evidence of benefit for … acupuncture …“
What should be done to prevent people from getting misled in this way?
- The Lancet should correct the error. It might be tempting to do this by simply exchanging the term ‘good’ with ‘some’. However, this would still be misleading, as there is some evidence for almost any type of bogus therapy.
- Authors, reviewers, and editors should do their job properly and check the original sources of their quotes.
PS
In case someone argued that the Cochrane review is just one of many, here is the conclusion of an overview of 15 systematic reviews on the subject: The … findings emphasized that acupuncture and related therapies alone did not have clinically significant effects at cancer-related pain reduction as compared with analgesic administration alone.
An article in PULSE entitled ‘ Revolutionising Chiropractic Care for Today’s Healthcare System’ deserves a comment, I think. Here I give you first the article followed by my comments. The references in square brackets refer to the latter and were inserted by me; otherwise, the article is unchanged.
___________________________
This Chiropractic Awareness Week (4th – 10th April), Catherine Quinn, President of the British Chiropractic Association (BCA), is exploring the opportunity and need for a more integrated healthcare eco-system, putting the spotlight on how chiropractors can help alleviate pressures and support improved patient outcomes.
Chiropractic treatment and its role within today’s health system often prompts questions and some debate – what treatments fit under chiropractic care? Is the profession evidence based? How can it support primary health services, with the blend of public and private practice in mind? This Chiropractic Awareness Week, I want to address these questions and share the British Chiropractic Association’s ambition for the future of the profession.
The role of chiropractic today
The need for effective and efficient musculoskeletal (MSK) treatment is clear – in the UK, an estimated 17.8 million people live with a MSK condition, equivalent to approximately 28.9% of the total population.1 Lower back and neck pain specifically are the greatest causes of years lost to disability in the UK, with chronic joint pain or osteoarthritis affecting more than 8.75 million people.2 In addition to this, musculoskeletal conditions also account for 30% of all GP appointments, placing immense pressure on a system which is already under stress.3 The impact of the COVID-19 pandemic is still being felt by these patients and their healthcare professionals alike. Patients with MSK conditions are still having their care impacted by issues such as having clinic appointments cancelled, difficulty in accessing face-to-face care and some unable to continue regular prescribed exercise.
With these numbers and issues in mind, there is a lot of opportunity to more closely integrate chiropractic within health and community services to help alleviate pressures on primary care [1]. This is something we’re really passionate about at the BCA. However, we recognise that there are varying perceptions of chiropractic care – not just from the public but across our health peers too. We want to address this, so every health discipline has a consistent understanding.
First and foremost, chiropractic is a registered primary healthcare profession [2] and a safe form of treatment [3], qualified individuals in this profession are working as fully regulated healthcare professionals with at least four years of Masters level training. In the UK, chiropractors are regulated by law and required to adhere to strict codes of practice [4], in exactly the same ways as dentists and doctors [5]. At the BCA we want to represent the highest quality chiropractic care, which is encapsulated by a patient centred approach, driven by evidence and science [6].
As a patient-first organisation [7], our primary goal is to equip our members to provide the best treatment possible for those who need our care [8]. We truly believe that working collaboratively with other primary care and NHS services is the way to reach this goal [9].
The benefits of collaborative healthcare
As chiropractors, we see huge potential in working more closely with primary care providers and recognise there’s mutual benefits for both parties [10]. Healthcare professionals can tap into chiropractors’ expertise in MSK conditions, leaning on them for support with patient caseloads. Equally, chiropractors can use the experience of working with other healthcare experts to grow as professionals.
At the BCA, our aim is to grow this collaborative approach, working closely with the wider health community to offer patients the best level of care that we can [11]. Looking at primary healthcare services in the UK, we understand the pressures that individual professionals, workforces, and organisations face [12]. We see the large patient rosters and longer waiting times and truly believe that chiropractors can alleviate some of those stresses by treating those with MSK concerns [13].
One way the industry is beginning to work in a more integrated way is through First Contact Practitioners (FCPs) [14]. These are healthcare professionals like chiropractors who provide the first point of contact to GP patients with MSK conditions [15]. We’ve already seen a lot of evidence showing that primary care services using FCPs have been able to improve quality of care [16]. Through this service MSK patients are also seeing much shorter wait times for treatment (as little as 2-3 days), so the benefits speak for themselves for both the patient and GP [17].
By working as part of an integrated care model, with chiropractors, GPs, physiotherapists and other medical professionals, we’re creating a system that provides patients with direct routes to the treatments that they need, with greater choice. Our role within this system is very much to contribute to the health of our country, support primary care workers and reinforce the incredible work of the NHS [18].
Overcoming integrated healthcare challenges
To continue to see the chiropractic sector develop over the coming years, it’s important for us to face some of the challenges currently impacting progress towards a more integrated healthcare service.
One example is that there is a level of uncertainty about where chiropractic sits in the public/private blend. This is something we’re ready to tackle head on by showing exactly how chiropractic care benefits different individuals, whether that’s through reducing pain, improving physical function or increasing mobility [19]. We also need to encourage more awareness amongst both chiropractors and other healthcare providers about how an integrated workforce could benefit medical professionals and patients alike [20]. For example, there’s only two FCP chiropractors to date, and that’s something we’re looking to change [14].
This is the start of a much bigger conversation and, at the BCA, we’ll continue to work on driving peer acceptance, trust and inclusion to demonstrate the value of our place within the healthcare industry [21]. We’re ready to support the wider health community and primary carers, alleviating some of the pressures already facing the NHS; we’re placed in the perfect position as we have the knowledge and experience to provide essential support [22]. My main takeaway from this year’s Chiropractic Awareness Week would be to simply start a conversation with us about how [23].
About the British Chiropractic Association:
The BCA is the largest and longest-standing association for chiropractors in the UK. As well as promoting international standards of education and exemplary conduct, the BCA supports chiropractors to progress and develop to fulfil their professional ambitions with honour and integrity, at every step [24]. This Chiropractic Awareness Week, the BCA is raising awareness about the rigour, relevance and evidence driving the profession and the association’s ambition for chiropractic to be more closely embedded within mainstream healthcare [25].
- https://bjgp.org/content/70/suppl_1/bjgp20X711497
- https://www.versusarthritis.org/about-arthritis/data-and-statistics/the-state-of-musculoskeletal-health/
- https://www.england.nhs.uk/elective-care-transformation/best-practice-solutions/musculoskeletal/#:~:text=Musculoskeletal%20(MSK)%20conditions%20account%20for,million%20people%20in%20the%20UK
__________________________________
And here are my comments:
- Non sequitur = a conclusion or statement that does not logically follow from the previous argument or statement.
- A primary healthcare profession is a profession providing primary healthcare which, according to standard definitions, is the provision of health services, including diagnosis and treatment of a health condition, and support in managing long-term healthcare, including chronic conditions like diabetes. Thus chiropractors are not in that category.
- This is just wishful thinking. Chiropractic spinal manipulation is not safe!
- “Required to adhere to strict codes of practice”. Required yes, but how often do they not comply?
- This is not true.
- Chiropractic is very far from being “driven by evidence and science”.
- Platitude = a remark or statement, especially one with a moral content, that has been used too often to be interesting or thoughtful.
- Judging from past experience, the primary goal seems to be to protect chiropractors (see, for instance, here).
- Belief is for religion, in healthcare you need evidence. Have you looked at the referral rates of chiropractors to GPs, for instance?
- For chiropractors, the benefit is usually measured in £s.
- To offer the ” best level of care” you need research and evidence, not politically correct statements.
- Platitude = a remark or statement, especially one with a moral content, that has been used too often to be interesting or thoughtful.
- Belief is for religion, in healthcare you need evidence.
- First Contact Practitioners are “regulated, advanced and autonomous health CARE PROFESSIONALS who are trained to provide expert PATIENT assessment, diagnosis and first-line treatment, self-care advice and, if required, appropriate onward referral to other SERVICES.” I doubt that many chiropractors fulfill these criteria.
- Not quite; see above.
- “A lot of evidence”? Really? Where is it?
- “The benefits speak for themselves” only if the treatments used are evidence-based.
- Platitude = a remark or statement, especially one with a moral content, that has been used too often to be interesting or thoughtful.
- Where is the evidence?
- Awareness is not needed as much as evidence?
- Platitude = a remark or statement, especially one with a moral content, that has been used too often to be interesting or thoughtful.
- Platitude = a remark or statement, especially one with a moral content, that has been used too often to be interesting or thoughtful.
- Fine, let’s start the conversation: where is your evidence?
- Judging from past experience honor and integrity seem rather thin on the ground (see, for instance here).
The article promised to ‘revolutionize chiropractic care and to answer questions like what treatments fit under chiropractic care? Is the profession evidence-based? Sadly, none of this emerged. Instead, we were offered politically correct platitudes, half-truths, and obscurations.
The revolution in chiropractic, it thus seems, is not in sight.
Today, several UK dailies report about a review of osteopathy just published in BMJ-online. The aim of this paper was to summarise the available clinical evidence on the efficacy and safety of osteopathic manipulative treatment (OMT) for different conditions. The authors conducted an overview of systematic reviews (SRs) and meta-analyses (MAs). SRs and MAs of randomised controlled trials evaluating the efficacy and safety of OMT for any condition were included.
The literature searches revealed nine SRs or MAs conducted between 2013 and 2020 with 55 primary trials involving 3740 participants. The SRs covered a wide range of conditions including
- acute and chronic non-specific low back pain (NSLBP, four SRs),
- chronic non-specific neck pain (CNSNP, one SR),
- chronic non-cancer pain (CNCP, one SR),
- paediatric (one SR),
- neurological (primary headache, one SR),
- irritable bowel syndrome (IBS, one SR).
Although with different effect sizes and quality of evidence, MAs reported that OMT is more effective than comparators in reducing pain and improving the functional status in acute/chronic NSLBP, CNSNP and CNCP. Due
to the small sample size, presence of conflicting results and high heterogeneity, questionable evidence existed on OMT efficacy for paediatric conditions, primary headaches and IBS. No adverse events were reported in most SRs. The methodological quality of the included SRs was rated low or critically low.
The authors concluded that based on the currently available SRs and MAs, promising evidence suggests the possible effectiveness of OMT for musculoskeletal disorders. Limited and inconclusive evidence occurs for paediatric conditions, primary headache and IBS. Further well-conducted SRs and MAs are needed to confirm and extend the efficacy and safety of OMT.
This paper raises several questions. Here a just the two that bothered me most:
- If the authors had truly wanted to evaluate the SAFETY of OMT (as they state in the abstract), they would have needed to look beyond SRs, MAs or RCTs. We know – and the authors of the overview confirm this – that clinical trials of so-called alternative medicine (SCAM) often fail to mention adverse effects. This means that, in order to obtain a more realistic picture, we need to look at case reports, case series and other observational studies. It also means that the positive message about safety generated here is most likely misleading.
- The authors (the lead author is an osteopath) might have noticed that most – if not all – of the positive SRs were published by osteopaths. Their assessments might thus have been less than objective. The authors did not include one of our SRs (because it fell outside their inclusion period). Yet, I do believe that it is one of the few reviews of OMT for musculoskeletal problems that was not done by osteopaths. Therefore, it is worth showing you its abstract here:
The objective of this systematic review was to assess the effectiveness of osteopathy as a treatment option for musculoskeletal pain. Six databases were searched from their inception to August 2010. Only randomized clinical trials (RCTs) were considered if they tested osteopathic manipulation/mobilization against any control intervention or no therapy in human with any musculoskeletal pain in any anatomical location, and if they assessed pain as an outcome measure. The selection of studies, data extraction, and validation were performed independently by two reviewers. Studies of chiropractic manipulations were excluded. Sixteen RCTs met the inclusion criteria. Their methodological quality ranged between 1 and 4 on the Jadad scale (max = 5). Five RCTs suggested that osteopathy compared to various control interventions leads to a significantly stronger reduction of musculoskeletal pain. Eleven RCTs indicated that osteopathy compared to controls generates no change in musculoskeletal pain. Collectively, these data fail to produce compelling evidence for the effectiveness of osteopathy as a treatment of musculoskeletal pain.
It was published 11 years ago. But I have so far not seen compelling evidence that would make me change our conclusion. As I state in the newspapers:
OSTEOPATHY SHOULD BE TAKEN WITH A SIZABLE PINCH OF SALT.
This study explored the curative effects of remote home management combined with ‘Feng’s spinal manipulation’ on the treatment of elderly patients with lumbar disc herniation (LDH). (LDH is understood by the investigators to be a condition where lumbar disc degeneration or trauma causes the nucleus pulposus and annulus fibrosus to protrude towards the spinal canal and to constrict the spinal cord or nerve root.)
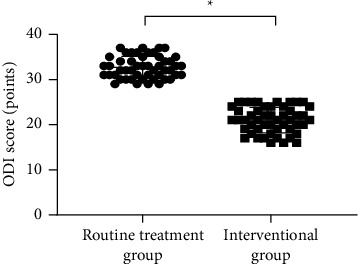
The clinical data of 100 patients with LDH were retrospectively reviewed. The 100 patients were equally divided into a routine treatment group and an interventional group according to the order of admission. The routine treatment group received conventional rehabilitation training, and the interventional group received remote home management combined with Feng’s spinal manipulation. The Oswestry disability index (ODI) and straight leg raising test were adopted for the assessment of the degrees of dysfunction and straight leg raising angles of the two groups after intervention. The curative effects of the two rehabilitation programs were evaluated.
Compared TO the routine treatment group, the interventional group had a remarkably higher excellent and good rate (P < 0.05), a significantly lower average ODI score after intervention (P < 0.001), notably higher straight leg raising angle, surface AEMG (average electromyogram) during stretching and tenderness threshold after intervention (P < 0.001), markedly lower muscular tension, surface AEMG during buckling, and flexion-extension relaxation ratio (FRR; (P < 0.001)), and much higher quality of life scores after intervention (P < 0.001).
The authors concluded that remote home management combined with Feng’s spinal manipulation, as a reliable method to improve the quality of life and the back muscular strength of the elderly patients with LDH, can substantially increase the straight leg raising angle and reduce the degree of dysfunction. Further study is conducive to establishing a better solution for the patients with LDH.
The authors state that “Feng’s spinal manipulation adopts spinal fixed-point rotation reduction to correct the vertebral displacement, and its curative effects have been confirmed in the treatment of sequestered LDH.” This is an odd statement: firstly, there is no vertebral displacement in LDH; secondly, if the treatment had been confirmed to be curative, why conduct this study?
Moreover, I don’t quite understand how the authors conducted a retrospective chart review and equally divide the 100 patients into two groups treated differently. What I do understand, however, is this:
- a retrospective review does not lend itself to conclusions about the effectiveness of any therapy;
- no type of spinal manipulation can hope to cure a lumbar disc degeneration or trauma that causes a herniation of the nucleus pulposus and annulus fibrosus.
Thus, I recommend we take this study with a sizable pinch of salt.
No 10-year follow-up study of so-called alternative medicine (SCAM) for lumbar intervertebral disc herniation (LDH) has so far been published. Therefore, the authors of this paper performed a prospective 10-year follow-up study on the integrated treatment of LDH in Korea.
One hundred and fifty patients from the baseline study, who initially met the LDH diagnostic criteria with a chief complaint of radiating pain and received integrated treatment, were recruited for this follow-up study. The 10-year follow-up was conducted from February 2018 to March 2018 on pain, disability, satisfaction, quality of life, and changes in a herniated disc, muscles, and fat through magnetic resonance imaging.
Sixty-five patients were included in this follow-up study. Visual analogue scale score for lower back pain and radiating leg pain were maintained at a significantly lower level than the baseline level. Significant improvements in Oswestry disability index and quality of life were consistently present. MRI confirmed that disc herniation size was reduced over the 10-year follow-up. In total, 95.38% of the patients were either “satisfied” or “extremely satisfied” with the treatment outcomes and 89.23% of the patients claimed their condition “improved” or “highly improved” at the 10-year follow-up.
The authors concluded that the reduced pain and improved disability was maintained over 10 years in patients with LDH who were treated with nonsurgical Korean medical treatment 10 years ago. Nonsurgical traditional Korean medical treatment for LDH produced beneficial long-term effects, but future large-scale randomized controlled trials for LDH are needed.
This study and its conclusion beg several questions:
WHAT DID THE SCAM CONSIST OF?
The answer is not provided in the paper; instead, the authors refer to 3 previous articles where they claim to have published the treatment schedule:
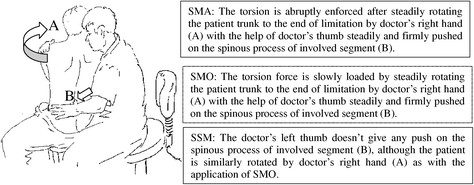
The treatment package included herbal medicine, acupuncture, bee venom pharmacopuncture and Chuna therapy (Korean spinal manipulation). Treatment was conducted once a week for 24 weeks, except herbal medication which was taken twice daily for 24 weeks; (1) Acupuncture: frequently used acupoints (BL23, BL24, BL25, BL31, BL32, BL33, BL34, BL40, BL60, GB30, GV3 and GV4)10 ,11 and the site of pain were selected and the needles were left in situ for 20 min. Sterilised disposable needles (stainless steel, 0.30×40 mm, Dong Bang Acupuncture Co., Korea) were used; (2) Chuna therapy12 ,13: Chuna is a Korean spinal manipulation that includes high-velocity, low-amplitude thrusts to spinal joints slightly beyond the passive range of motion for spinal mobilisation, and manual force to joints within the passive range; (3) Bee venom pharmacopuncture14: 0.5–1 cc of diluted bee venom solution (saline: bee venom ratio, 1000:1) was injected into 4–5 acupoints around the lumbar spine area to a total amount of 1 cc using disposable injection needles (CPL, 1 cc, 26G×1.5 syringe, Shinchang medical Co., Korea); (4) Herbal medicine was taken twice a day in dry powder (2 g) and water extracted decoction form (120 mL) (Ostericum koreanum, Eucommia ulmoides, Acanthopanax sessiliflorus, Achyranthes bidentata, Psoralea corylifolia, Peucedanum japonicum, Cibotium barometz, Lycium chinense, Boschniakia rossica, Cuscuta chinensis and Atractylodes japonica). These herbs were selected from herbs frequently prescribed for LBP (or nerve root pain) treatment in Korean medicine and traditional Chinese medicine,15 and the prescription was further developed through clinical practice at Jaseng Hospital of Korean Medicine.9 In addition, recent investigations report that compounds of C. barometz inhibit osteoclast formation in vitro16 and A. japonica extracts protect osteoblast cells from oxidative stress.17 E. ulmoides has been reported to have osteoclast inhibitive,18 osteoblast-like cell proliferative and bone mineral density enhancing effects.19 Patients were given instructions by their physician at treatment sessions to remain active and continue with daily activities while not aggravating pre-existing symptoms. Also, ample information about the favourable prognosis and encouragement for non-surgical treatment was given.
The traditional Korean spinal manipulations used (‘Chuna therapy’ – the references provided for it do NOT refer to this specific way of manipulation) seemed interesting, I thought. Here is an explanation from an unrelated paper:
Chuna, which is a traditional manual therapy practiced by Korean medicine doctors, has been applied to various diseases in Korea. Chuna manual therapy (CMT) is a technique that uses the hand, other parts of the doctor’s body or other supplementary devices such as a table to restore the normal function and structure of pathological somatic tissues by mobilization and manipulation. CMT includes various techniques such as thrust, mobilization, distraction of the spine and joints, and soft tissue release. These techniques were developed by combining aspects of Chinese Tuina, chiropratic, and osteopathic medicine.[13] It has been actively growing in Korea, academically and clinically, since the establishment of the Chuna Society (the Korean Society of Chuna Manual Medicine for Spine and Nerves, KSCMM) in 1991.[14] Recently, Chuna has had its effects nationally recognized and was included in the Korean national health insurance in March 2019.[15]
This almost answers the other questions I had. Almost, but not quite. Here are two more:
- The authors conclude that the SCAM produced beneficial long-term effects. But isn’t it much more likely that the outcomes their uncontrolled observations describe are purely or at least mostly a reflection of the natural history of lumbar disc herniation?
- If I remember correctly, I learned a long time ago in medical school that spinal manipulation is contraindicated in lumbar disc herniation. If that is so, the results might have been better, if the patients of this study had not received any SCAM at all. In other words, are the results perhaps due to firstly the natural history of the condition and secondly to the detrimental effects of the SCAM the investigators applied?
If I am correct, this would then be the 4th article reporting the findings of a SCAM intervention that aggravated lumbar disc herniation.
PS
I know that this is a mere hypothesis but it is at least as plausible as the conclusion drawn by the authors.
Low back pain (LBP) is influenced by interrelated biological, psychological, and social factors, however current back pain management is largely dominated by one-size fits all unimodal treatments. Team based models with multiple provider types from complementary professional disciplines is one way of integrating therapies to address patients’ needs more comprehensively.
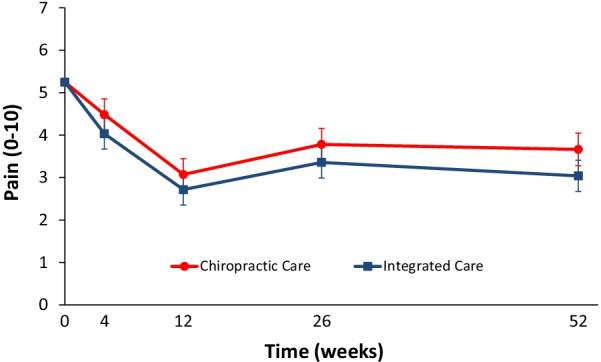
This parallel-group randomized clinical trial conducted from May 2007 to August 2010 aimed to evaluate the relative clinical effectiveness of 12 weeks of monodisciplinary chiropractic care (CC), versus multidisciplinary integrative care (IC), for adults with sub-acute and chronic LBP. The primary outcome was pain intensity and secondary outcomes were disability, improvement, medication use, quality of life, satisfaction, frequency of symptoms, missed work or reduced activities days, fear-avoidance beliefs, self-efficacy, pain coping strategies, and kinesiophobia measured at baseline and 4, 12, 26 and 52 weeks. Linear mixed models were used to analyze outcomes.
In total, 201 participants were enrolled. The largest reductions in pain intensity occurred at the end of treatment and were 43% for CC and 47% for IC. The primary analysis found IC to be significantly superior to CC over the 1-year period (P = 0.02). The long-term profile for pain intensity which included data from weeks 4 through 52, showed a significant advantage of 0.5 for IC over CC (95% CI 0.1 to 0.9; P = 0.02; 0 to 10 scale). The short-term profile (weeks 4 to 12) favored IC by 0.4, but was not statistically significant (95% CI – 0.02 to 0.9; P = 0.06). There was also a significant advantage over the long term for IC in some secondary measures (disability, improvement, satisfaction, and low back symptom frequency), but not for others (medication use, quality of life, leg symptom frequency, fear-avoidance beliefs, self-efficacy, active pain coping, and kinesiophobia). No serious adverse events resulted from either of the interventions.
The authors concluded that participants in the IC group tended to have better outcomes than the CC group, however, the magnitude of the group differences was relatively small. Given the resources required to successfully implement multidisciplinary integrative care teams, they may not be worthwhile, compared to monodisciplinary approaches like chiropractic care, for treating LBP.
The obvious question is: what were the exact treatments used in both groups? The authors provide the following explanations:
All participants in the study received 12 weeks of either monodisciplinary chiropractic care (CC) or multidisciplinary team-based integrative care (IC). CC was delivered by a team of chiropractors allowed to utilize any non-proprietary treatment under their scope of practice not shown to be ineffective or harmful including manual spinal manipulation (i.e., high velocity, low amplitude thrust techniques, with or without the assistance of a drop table) and mobilization (i.e., low velocity, low amplitude thrust techniques, with or without the assistance of a flexion-distraction table). Chiropractors also used hot and cold packs, soft tissue massage, teach and supervise exercise, and administer exercise and self-care education materials at their discretion. IC was delivered by a team of six different provider types: acupuncturists, chiropractors, psychologists, exercise therapists, massage therapists, and primary care physicians, with case managers coordinating care delivery. Interventions included acupuncture and Oriental medicine (AOM), spinal manipulation or mobilization (SMT), cognitive behavioral therapy (CBT), exercise therapy (ET), massage therapy (MT), medication (Med), and self-care education (SCE), provided either alone or in combination and delivered by their respective profession. Participants were asked not to seek any additional treatment for their back pain during the intervention period. Standardized forms were used to document the details of treatment, as well as adverse events. It was not possible to blind patients or providers to treatment due to the nature of the study interventions. Patients in both groups received individualized care developed by clinical care teams unique to each intervention arm. Care team training was conducted to develop and support group dynamics and shared clinical decision making. A clinical care pathway, designed to standardize the process of developing recommendations, guided team-based practitioner in both intervention arms. Evidence based treatment plans were based on patient biopsychosocial profiles derived from the history and clinical examination, as well as baseline patient rated outcomes. The pathway has been fully described elsewhere [23]. Case managers facilitated patient care team meetings, held weekly for each intervention group, to discuss enrolled participants and achieve treatment plan recommendation consensus. Participants in both intervention groups were presented individualized treatment plan options generated by the patient care teams, from which they could choose based on their preferences.
This is undoubtedly an interesting study. It begs many questions. The two that puzzle me most are:
- Why publish the results only 12 years after the trial was concluded? The authors provide a weak explanation, but I would argue that it is unethical to sit on a publicly funded study for so long.
- Why did the researchers not include a third group of patients who were treated by their GP like in normal routine?
The 2nd question is, I think, important because the findings could mostly be a reflection of the natural history of LBP. We can probably all agree that, at present, the optimal treatment for LBP has not been found. To me, the results look as though they indicate that it hardly matters how we treat LBP, the outcome is always very similar. If we throw the maximum amount of care at it, the results tend to be marginally better. But, as the authors admit, there comes a point where we have to ask, is it worth the investment?
Perhaps the old wisdom is not entirely wrong (old because I learned it at medical school some 50 years ago): make sure LBP patients keep as active as they can while trying to ignore their pain as best as they can. It’s not a notion that would make many practitioners of so-called alternative medicine (SCAM) happy – LBP is their No 1 cash cow! – but it would surely save huge amounts of public expenditure.
A multi-disciplinary research team assessed the effectiveness of interventions for acute and subacute non-specific low back pain (NS-LBP) based on pain and disability outcomes. For this purpose, they conducted a systematic review of the literature with network meta-analysis.
They included all 46 randomized clinical trials (RCTs) involving adults with NS-LBP who experienced pain for less than 6 weeks (acute) or between 6 and 12 weeks (subacute). Non-pharmacological treatments (eg, manual therapy) including acupuncture and dry needling or pharmacological treatments for improving pain and/or reducing disability considering any delivery parameters were included. The comparator had to be an inert treatment encompassing sham/placebo treatment or no treatment. The risk of bias was
- low in 9 trials (19.6%),
- unclear in 20 (43.5%),
- high in 17 (36.9%).
At immediate-term follow-up, for pain decrease, the most efficacious treatments against an inert therapy were:
- exercise (standardised mean difference (SMD) -1.40; 95% confidence interval (CI) -2.41 to -0.40),
- heat wrap (SMD -1.38; 95% CI -2.60 to -0.17),
- opioids (SMD -0.86; 95% CI -1.62 to -0.10),
- manual therapy (SMD -0.72; 95% CI -1.40 to -0.04).
- non-steroidal anti-inflammatory drugs (NSAIDs) (SMD -0.53; 95% CI -0.97 to -0.09).
Similar findings were confirmed for disability reduction in non-pharmacological and pharmacological networks, including muscle relaxants (SMD -0.24; 95% CI -0.43 to -0.04). Mild or moderate adverse events were reported in the opioids (65.7%), NSAIDs (54.3%), and steroids (46.9%) trial arms.
The authors concluded that NS-LBP should be managed with non-pharmacological treatments which seem to mitigate pain and disability at immediate-term. Among pharmacological interventions, NSAIDs and muscle relaxants appear to offer the best harm-benefit balance.
The authors point out that previous published systematic reviews on spinal manipulation, exercise, and heat wrap did overlap with theirs: exercise (eg, motor control exercise, McKenzie exercise), heat wrap, and manual therapy (eg, spinal manipulation, mobilization, trigger points or any other technique) were found to reduce pain intensity and disability in adults with acute and subacute phases of NS-LBP.
I would add (as I have done so many times before) that the best approach must be the one that has the most favorable risk/benefit balance. Since spinal manipulation is burdened with considerable harm (as discussed so many times before), exercise and heat wraps seem to be preferable. Or, to put it bluntly: