osteopathy
I recently came across this paper by Prof. Dr. Chad E. Cook, a physical therapist, PhD, a Fellow of the American Physical Therapy Association (FAPTA), and a professor as well as director of clinical research in the Department of Orthopaedics, Department of Population Health Sciences at the Duke Clinical Research Institute at Duke University in North Carolina, USA. The paper is entitled ‘The Demonization of Manual Therapy‘.
Cook introduced the subject by stating: “In medicine, when we do not understand or when we dislike something, we demonize it. Well-known examples throughout history include the initial ridicule of antiseptic handwashing, percutaneous transluminal coronary angioplasty (i. e., balloon angioplasty), the relationships between viruses and cancer, the contribution of bacteria in the development of ulcers, and the role of heredity in the development of disease. In each example, naysayers attempted to discredit the use of each of the concepts, despite having no evidence to support their claims. The goal in each of the aforementioned topics: demonize the concept.”
Cook then discussed 8 ‘demonizations’ of manual therapy. Number 7 is entitled “Causes as Much Harm as Help“. Here is this section in full:
By definition, harms include adverse reactions (e. g., side effects of treatments), and other undesirable consequences of health care products and services. Harms can be classified as “none”, minor, moderate, serious and severe [67]. Most interventions have some harms, typically minor, which are defined as a non-life-threatening, temporary harm that may or may not require efforts to assess for a change in a patient’s condition such as monitoring [67].
There are harms associated with a manual therapy intervention, but they are generally benign (minor). Up to 20 –40 % of individuals will report adverse events after the application of manual therapy. The most common adverse events were soreness in muscles, increased pain, stiffness and tiredness [68]. There are rare occasions of several harms associated with manual therapy and these include spinal or neurological problems as well as cervical arterial strokes [9]. It is critical to emphasize how rare these events are; serious adverse event incidence estimates ranged from 1 per 2 million manipulations to 13 per 10,000 patients [69].
Cook then concludes that “manual therapy has been inappropriately demonized over the last decade and has been associated with inaccurate assumptions and false speculations that many clinicians have acquired over the last decade. This paper critically analyzed eight of the most common assumptions that have belabored manual therapy and identified notable errors in seven of the eight. It is my hope that the physiotherapy community will carefully re-evaluate its stance on manual therapy and consider a more evidence-based approach for the betterment of our patients.
REFERENCES
[9] Ernst E. Adverse effects of spinal manipulation: a systematic review. J R Soc Med 2007; 100: 330–338.doi:10.1177/014107680710000716 [68] Paanalahti K, Holm LW, Nordin M et al. Adverse events after manual therapy among patients seeking care for neck and/or back pain: a randomized controlled trial. BMC Musculoskelet Disord 2014; 15: 77. doi:10.1186/1471-2474-15-77 [69] Swait G, Finch R. What are the risks of manual treatment of the spine? A scoping review for clinicians. Chiropr Man Therap 2017; 25: 37. doi:10.1186/s12998-017-0168-5
_________________________________
Here are a few things that I find odd or wrong with Cook’s text:
- The term ‘demonizing’ seems to be a poor choice. The historical examples chosen by Cook were not cases of demonization. They were mostly instances where new discoveries did not fit into the thinking of the time and therefore took a long time to get accepted. They also show that sooner or later, sound evidence always prevails. Lastly, they suggest that speeding up this process via the concept of evidence-based medicine is a good idea.
- Cook then introduces the principle of risk/benefit balance by entitling the cited section “Causes as Much Harm as Help“. Oddly, however, he only discusses the risks of manual therapies and omits the benefit side of the equation.
- This omission is all the more puzzling since he quotes my paper (his reference [9]) states that “the effectiveness of spinal manipulation for most indications is less than convincing.5 A risk-benefit evaluation is therefore unlikely to generate positive results: with uncertain effectiveness and finite risks, the balance cannot be positive.”
- In discussing the risks, he seems to assume that all manual therapies are similar. This is clearly not true. Massage therapies have a very low risk, while this cannot be said of spinal manipulations.
- The harms mentioned by Cook seem to be those of spinal manipulation and not those of all types of manual therapy.
- Cook states that “up to 20 –40 % of individuals will report adverse events after the application of manual therapy.” Yet, the reference he uses in support of this statement is a clinical trial that reported an adverse effect rate of 51%.
- Cook then states that “there are rare occasions of several harms associated with manual therapy and these include spinal or neurological problems as well as cervical arterial strokes.” In support, he quotes one of my papers. In it, I emphasize that “the incidence of such events is unknown.” Cook not only ignores this fact but states in the following sentence that “it is critical to emphasize how rare these events are…”
Cook concludes that “manual therapy has been inappropriately demonized over the last decade and has been associated with inaccurate assumptions and false speculations …” He confuses, I think, demonization with critical assessment.
Cook’s defence of manual therapy is clumsy, inaccurate, ill-conceived, misleading and often borders on the ridiculous. In the age of evidence-based medicine, therapies are not ‘demonized’ but evaluated on the basis of their effectiveness and safety. Manual therapies are too diverse to do this wholesale. They range from various massage techniques, some of which have a positive risk/benefit balance, to high-velocity, low-amplitude thrusts, for which the risks do not demonstrably outweigh the benefits.
Spinal manipulation therapy (SMT) is widely used worldwide to treat musculoskeletal and many other conditions. The evidence that it works for any of them is weak, non-existent, or negative. What is worse, SMT can – as we have discussed so often on this blog – cause adverse events some of which are serious, even fatal.
Spinal epidural hematoma (SEH) caused by SMT is a rare emergency that can cause neurological dysfunction. Chinese researchers recently reported three cases of SEH after SMT. 
- The first case was a 30-year-old woman who experienced neck pain and numbness in both upper limbs immediately after SMT. Her symptoms persisted after 3 d of conservative treatment, and she was admitted to our hospital. Magnetic resonance imaging (MRI) demonstrated an SEH, extending from C6 to C7.
- The second case was a 55-year-old man with sudden back pain 1 d after SMT, numbness in both lower limbs, an inability to stand or walk, and difficulty urinating. MRI revealed an SEH, extending from T1 to T3.
- The third case was a 28-year-old man who suddenly developed symptoms of numbness in both lower limbs 4 h after SMT. He was unable to stand or walk and experienced mild back pain. MRI revealed an SEH, extending from T1 to T2.
All three patients underwent surgery after failed conservative treatment and all recovered to ASIA grade E on day 5, 1 wk, and day 10 after surgery, respectively. All patients returned to normal after 3 mo of follow-up.
The authors concluded that SEH caused by SMT is very rare, and the condition of each patient should be evaluated in full detail before operation. SEH should be diagnosed immediately and actively treated by surgery.
These cases might serve as an apt reminder of the fact that SMT (particularly SMT of the neck) is not without its dangers. The authors’ assurance that SEH is VERY RARE is a little puzzling, in my view (the paper includes a table with all 17 previously published cases). There is, as we often have mentioned, no post-marketing surveillance, surgeons only see those patients who survive such complications long enough to come to the hospital, and they publish such cases only if they feel like it. Consequently, the true incidence is anyone’s guess.
As pointed out earlier, the evidence that SMT might be effective is shaky for most indications. In view of the potential for harm, this can mean only one thing:
The risk/benefit balance for SMT is not demonstrably positive.
In turn, this leads to the conclusion that patients should think twice before having SMT and should inquire about other therapeutic options that have a more positive risk/benefit balance. Similarly, the therapists proposing SMT to a patient have the ethical and moral duty to obtain fully informed consent which includes information about the risk/benefit balance of SMT and other options.
These days, I live in France (some of my time) and I am often baffled by the number of osteopaths and the high level of acceptance of osteopathy in this country. The public seems to believe everything osteopaths claim and even most doctors have long given up to object to the idiocies they proclaim.
The website of the Institute of Osteopathy in Renne is but one of many examples. The Institute informed us as follows (my translation):
In addition to back pain, the osteopath can act on functional disorders of the digestive, neurological, cardiovascular systems or conditions related to ear, nose and throat. Osteopaths can promote recovery in athletes, relieve migraines, musculoskeletal disorders such as tendonitis, or treat sleep disorders. Less known for its preventive aspect, osteopathy also helps maintain good health. It can be effective even when everything is going well because it will prevent the appearance of pain. Osteopathy is, in fact, a manual medicine that allows the rebalancing of the major systems of the body, whatever the age of the patient and his problems. The osteopath looks for the root cause of your complaint in order to develop a curative and preventive treatment.
Who are osteopathic consultations for?
Osteopathic consultations at the Institute of Osteopathy of Rennes-Bretagne are intended for the following types of patients and pathologies
BABY / CHILD
GERD (gastric reflux), plagiocephaly (cranial deformities), recurrent ENT disorders (sinusitis, ear infections…), digestive, sleep and behavioural disorders, motor delay, following a difficult birth…
ADULT
Prevention, comfort treatment of osteoarthritis, musculoskeletal pain, functional abdominal pain, digestive disorders, headaches, dizziness, postural deficiency, facial pains…
PREGNANT WOMAN
Musculoskeletal pain (lumbago, back pain), digestive disorders, preparation for childbirth, post-partum check-up.
COMPANY
Prevention and treatment of MSDs (musculoskeletal disorders) linked to workstation ergonomics, stress, pain due to repetitive movements, poor posture at work, etc.
ADOLESCENT
Scoliosis, prevention of certain pathologies linked to growth, fatigue, stress, follow-up of orthodontic treatment.
SPORTSMAN
Musculoskeletal pain, tendonitis, osteopathic preparation for competition, osteopathic assessment according to the sport practised, repetitive injury.
In case you are not familiar with the evidence for osteopathy, let me tell you that as good as none of the many claims made in the above text is supported by anything that even resembles sound evidence.
So, how can we explain that, in France, osteopathy is allowed to thrive in a virtually evidence-free space?
In France, osteopathy started developing in the 1950s. In 2002, osteopathy received legislative recognition in France, and today, it is booming; between 2016 and 2018, 3589 osteopaths were trained in France. Osteopaths can be DO doctors, DO physiotherapists, DO nurses, DO midwives, DO chiropodists, or even DO dentists.
Thus, in 2018, and out of a total of 29,612 professionals practising osteopathy, there were 17,897 osteopaths DO and 11,715 DO health professionals. The number of professionals using the title of osteopath has roughly tripled in 8 years (11608 in 2010 for 29612 in 2018). There are currently around 30 osteopathic schools in France. About 3 out of 5 French people now consult osteopaths.
But this does not answer my question why, in France, osteopathy is allowed to thrive in a virtually evidence-free space! To be honest, I do not know its answer.
Perhaps someone else does?
If so, please enlighten me.
The aims of this bibliometric analysis are to describe the characteristics of articles published on the efficacy of osteopathic interventions and to provide an overall portrait of their impacts in the scientific literature. A bibliometric analysis approach was used. Articles were identified with searches using a combination of relevant MeSH terms and indexing keywords about osteopathy and research designs in MEDLINE and CINAHL databases. The following indicators were extracted: country of the primary author, year of publication, journals, impact factor of the journal, number of citations, research design, participants’ age group, system/body part addressed, primary outcome, indexing keywords and types of techniques.
A total of 389 articles met the inclusion criteria. The number of empirical studies doubled every 5 years, with the United States, Italy, Spain, and the United Kingdom being the most productive countries. Twenty-three articles were cited over 100 times. Articles were published in 103 different indexed journals, but more than half (53.7%) of articles were published in one of three osteopathy-focused readership journals. Randomized control trials (n = 145; 37.3%) and case reports (n = 142; 36.5%) were the most common research designs. A total of 187 (48.1%) studies examined the effects of osteopathic interventions using a combination of techniques that belonged to two or all of the classic fields of osteopathic interventions (musculoskeletal, cranial, and visceral).
The authors concluded that this bibliometric analysis shows that publications about efficacy of osteopathy are relatively recent and have increased at a rapid pace over the last three decades. More than half of these publications are published in three osteopathic journals targeting a limited, disciplinary-focused readership. Our results highlight important needs for large efficacy and effectiveness trials, as well as study designs to further understanding of the mechanisms of action of the techniques being investigated. Finally, this bibliometric analysis can assist to identify osteopathy techniques and populations where further clinical research is required.
What the authors fail to state is that their analysis discloses osteopathy to be an area of utter unimportance. Less than 400 studies in 52 years is a dismal result. The fact that they were mostly published in journals of no impact makes it even worse. Twenty-three articles were cited more than 100 times; this is dismal! To put it in perspective, I have ~250 articles that were cited more than 100 times. Does that suggest that my work has made about 10 times more impact than the entire field of osteopathy?
A substantial number of patients globally receive spinal manipulative therapy (SMT) to manage non-musculoskeletal disorders. However, the efficacy and effectiveness of these interventions to prevent or treat non-musculoskeletal disorders remain controversial.
A Global Summit of international chiropractors and scientists conducted a systematic review of the literature to determine the efficacy and effectiveness of SMT for the primary, secondary and tertiary prevention of non-musculoskeletal disorders. The Global Summit took place on September 14-15, 2019 in Toronto, Canada. It was attended by 50 chiropractic researchers from 8 countries and 28 observers from 18 chiropractic organizations. Participants met the following criteria: 1) chiropractor with a PhD, or a researcher with a PhD (not a chiropractor) with research expertise in chiropractic; 2) actively involved in research (defined as having published at least 5 peer-reviewed papers over the past 5 years); and 3) appointed at an academic or educational institution. In addition, a small group of researchers who did not meet these criteria were invited. These included three chiropractors with a strong publication and scientific editorial record who did not have a PhD (SMP, JW, and HS) and two early career researchers with expertise within the area of chiropractic and pseudoscience (ALM, GG). Participants were invited by the Steering Committee using purposive and snowball sampling methods. At the summit, participants critically appraised the literature and synthesized the evidence.
They searched MEDLINE, Embase, the Cochrane Central Register of Controlled Trials, the Cumulative Index to Nursing and Allied Health, and the Index to Chiropractic Literature from inception to May 15, 2019, using subject headings specific to each database and free text words relevant to manipulation/manual therapy, effectiveness, prevention, treatment, and non-musculoskeletal disorders. Eligible for review were randomized controlled trials published in English. The methodological quality of eligible studies was assessed independently by reviewers using the Scottish Intercollegiate Guidelines Network (SIGN) criteria for randomized controlled trials. The researchers synthesized the evidence from articles with high or acceptable methodological quality according to the Synthesis without Meta-Analysis (SWiM) Guideline. The final risk of bias and evidence tables were reviewed by researchers who attended the Global Summit and 75% (38/50) had to approve the content to reach consensus.
A total of 4997 citations were retrieved, and 1123 duplicates were removed, and 3874 citations were screened. Of those, the eligibility of 32 articles was evaluated at the Global Summit and 16 articles were included in the systematic review. The synthesis included 6 randomized controlled trials with acceptable or high methodological quality (reported in 7 articles). These trials investigated the efficacy or effectiveness of SMT for the management of
- infantile colic,
- childhood asthma,
- hypertension,
- primary dysmenorrhea,
- migraine.
None of the trials evaluated the effectiveness of SMT in preventing the occurrence of non-musculoskeletal disorders. A consensus was reached on the content of all risk of bias and evidence tables. All randomized controlled trials with high or acceptable quality found that SMT was not superior to sham interventions for the treatment of these non-musculoskeletal disorders.
Six of 50 participants (12%) in the Global Summit did not approve the final report.
The authors concluded that our systematic review included six randomized clinical trials (534 participants) of acceptable or high quality investigating the efficacy or effectiveness of SMT for the treatment of non-musculoskeletal disorders. We found no evidence of an effect of SMT for the management of non-musculoskeletal disorders including infantile colic, childhood asthma, hypertension, primary dysmenorrhea, and migraine. This finding challenges the validity of the theory that treating spinal dysfunctions with SMT has a physiological effect on organs and their function. Governments, payers, regulators, educators, and clinicians should consider this evidence when developing policies about the use and reimbursement of SMT for non-musculoskeletal disorders.
I would have formulated the conclusions much more succinctly:
As has already been shown repeatedly, there is no sound evidence that SMT is effective for non-musculoskeletal conditions.
Myofascial release (also known as myofascial therapy or myofascial trigger point therapy) is a type of low-load stretch therapy that is said to release tightness and pain throughout the body caused by the myofascial pain syndrome, a chronic muscle pain that is worse in certain areas known as trigger points. Various types of health professionals provide myofascial release, e.g. osteopaths, chiropractors, physical or occupational therapists, massage therapists, or sports medicine/injury specialists. The treatment is usually applied repeatedly, but there is also a belief that a single session of myofascial release is effective. This study was a crossover clinical trial aimed to test whether a single session of a specific myofascial release technique reduces pain and disability in subjects with chronic low back pain (CLBP).
A total of 41 participants were randomly enrolled into 3 situations in a balanced and crossover manner:
- experimental,
- placebo,
- control.
The subjects underwent a single session of myofascial release on thoracolumbar fascia and the results were compared with the control and placebo groups. A single trained and experienced therapist applied the technique.
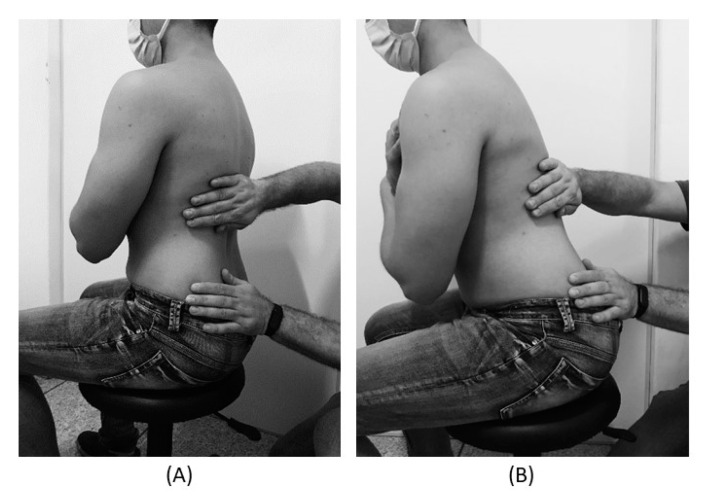
For the control treatment, the subjects were instructed to remain in the supine position for 5 minutes. For the muscle release session, the subjects were in a sitting position with feet supported and the thoracolumbar region properly undressed. The trunk flexion goniometry of each participant was performed and the value of 30° was marked with a barrier to limit the necessary movement during the technique. The trained researcher positioned their hands on all participants without sliding over the skin or forcing the tissue, with the cranial hand close to the last rib and at the T12–L1 level on the right side of the individual’s body and the caudal hand on the ipsilateral side between the iliac crest and the sacrum. Then, the researcher caused slight traction in the tissues by moving their hands away from each other in a longitudinal direction. Then, the participant was instructed to perform five repetitions of active trunk flexion-extension (30°), while the researcher followed the movement with both hands simultaneously positioned, without losing the initial tissue traction and position. The same technique and the same number of repetitions of active trunk flexion-extension were repeated with the researcher’s hands positioned on the opposite sides. This technique lasted approximately five minutes.
For the placebo treatment, the subjects were not submitted to the technique of manual thoracolumbar fascia release, but they slowly performed ten repetitions of active trunk flexion-extension (30°) in the same position as the experimental situation. Due to the fact that touch can provide not only well-recognized discriminative input to the brain, but also an affective input, there was no touch from the researcher at this stage.
The outcomes, pain, and functionality, were evaluated using the numerical pain rating scale (NPRS), pressure pain threshold (PPT), and Oswestry Disability Index (ODI).
The results showed no effects between-tests, within-tests, nor for interaction of all the outcomes, i.e., NPRS (η 2 = 0.32, F = 0.48, p = 0.61), PPT (η2 = 0.73, F = 2.80, p = 0.06), ODI (η2 = 0.02, F = 0.02, p = 0.97).
The authors concluded that a single trial of a thoracolumbar myofascial release technique was not enough to reduce pain intensity and disability in subjects with CLBP.
Surprised?
I’m not!
This systematic review assessed the effects and reliability of sham procedures in manual therapy (MT) trials in the treatment of back pain (BP) in order to provide methodological guidance for clinical trial development.
Different databases were screened up to 20 August 2020. Randomized controlled trials involving adults affected by BP (cervical and lumbar), acute or chronic, were included. Hand contact sham treatment (ST) was compared with different MT (physiotherapy, chiropractic, osteopathy, massage, kinesiology, and reflexology) and to no treatment. Primary outcomes were BP improvement, the success of blinding, and adverse effects (AE). Secondary outcomes were the number of drop-outs. Dichotomous outcomes were analyzed using risk ratio (RR), continuous using mean difference (MD), 95% CIs. The minimal clinically important difference was 30 mm changes in pain score.
A total of 24 trials were included involving 2019 participants. Most of the trials were of chiropractic manipulation. Very low evidence quality suggests clinically insignificant pain improvement in favor of MT compared with ST (MD 3.86, 95% CI 3.29 to 4.43) and no differences between ST and no treatment (MD -5.84, 95% CI -20.46 to 8.78).ST reliability shows a high percentage of correct detection by participants (ranged from 46.7% to 83.5%), spinal manipulation is the most recognized technique. Low quality of evidence suggests that AE and drop-out rates were similar between ST and MT (RR AE=0.84, 95% CI 0.55 to 1.28, RR drop-outs=0.98, 95% CI 0.77 to 1.25). A similar drop-out rate was reported for no treatment (RR=0.82, 95% 0.43 to 1.55).
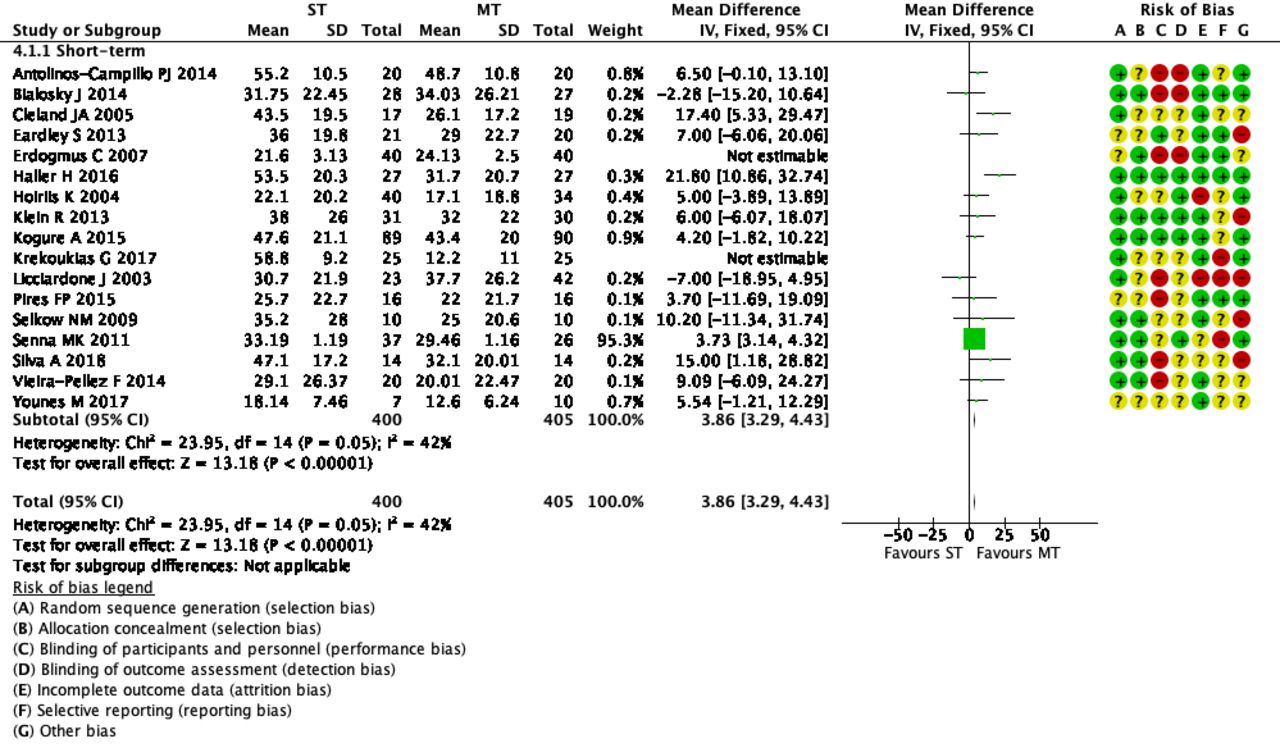 The authors concluded that MT does not seem to have clinically relevant effect compared with ST. Similar effects were found with no treatment. The heterogeneousness of sham MT studies and the very low quality of evidence render uncertain these review findings. Future trials should develop reliable kinds of ST, similar to active treatment, to ensure participant blinding and to guarantee a proper sample size for the reliable detection of clinically meaningful treatment effects.
The authors concluded that MT does not seem to have clinically relevant effect compared with ST. Similar effects were found with no treatment. The heterogeneousness of sham MT studies and the very low quality of evidence render uncertain these review findings. Future trials should develop reliable kinds of ST, similar to active treatment, to ensure participant blinding and to guarantee a proper sample size for the reliable detection of clinically meaningful treatment effects.
The optimal therapy for back pain does not exist or has not yet been identified; there are dozens of different approaches but none has been found to be truly and dramatically effective. Manual therapies like chiropractic and osteopathy are often used, and some data suggest that they are as good (or as bad) as most other options. This review confirms what we have discussed many times previously (e.g. here), namely that the small positive effect of MT, or specifically spinal manipulation, is largely due to placebo.
Considering this information, what is the best treatment for back pain sufferers? The answer seems obvious: it is a therapy that is as (in)effective as all the others but causes the least harm or expense. In other words, it is not chiropractic nor osteopathy but exercise.
My conclusion:
avoid therapists who use spinal manipulation for back pain.
Absurd claims about spinal manipulative therapy (SMT) improving immune function have increased substantially during the COVID-19 pandemic. Is there any basis at all for such notions?
The objective of this systematic review was to identify, appraise, and synthesize the scientific literature on the efficacy and effectiveness of SMT in preventing the development of infectious disease or improving disease-specific outcomes in patients with infectious disease and to examine the association between SMT and selected immunological, endocrine, and other physiological biomarkers.
A literature search of MEDLINE, the Cumulative Index to Nursing and Allied Health Literature, the Index to Chiropractic Literature, the Cochrane Central Register of Controlled Trials, and Embase was conducted. Randomized clinical trials and cohort studies were included. Eligible studies were critically appraised, and evidence with high and acceptable quality was synthesized using the Synthesis Without Meta-Analysis guideline.
A total of 2593 records were retrieved; after exclusions, 50 full-text articles were screened, and 16 articles reporting the findings of 13 studies comprising 795 participants were critically appraised. No clinical studies were located that investigated the efficacy or effectiveness of SMT in preventing the development of infectious disease or improving disease-specific outcomes among patients with infectious disease. Eight articles reporting the results of 6 high- and acceptable-quality RCTs comprising 529 participants investigated the effect of SMT on biomarkers. Spinal manipulative therapy was not associated with changes in lymphocyte levels or physiological markers among patients with low back pain or participants who were asymptomatic compared with sham manipulation, a lecture series, and venipuncture control groups. Spinal manipulative therapy was associated with short-term changes in selected immunological biomarkers among asymptomatic participants compared with sham manipulation, a lecture series, and venipuncture control groups.
The authors concluded that no clinical evidence was found to support or refute claims that SMT was efficacious or effective in changing immune system outcomes. Although there were limited preliminary data from basic scientific studies suggesting that SMT may be associated with short-term changes in immunological and endocrine biomarkers, the clinical relevance of these findings is unknown. Given the lack of evidence that SMT is associated with the prevention of infectious diseases or improvements in immune function, further studies should be completed before claims of efficacy or effectiveness are made.
I fully agree with the data as summarised in this paper. Yet, I find the conclusions a bit odd. The authors of this paper are chiropractors who declare the following conflicts of interest: Dr Côté reported receiving grants from the College of Chiropractors of British Columbia during the conduct of the study and grants from the Canadian Chiropractic Research Foundation, travel expenses from the World Federation of Chiropractic, and personal fees from the Canadian Chiropractic Protective Association outside the submitted work. Dr Cancelliere reported receiving grants from the Canadian Chiropractic Research Foundation outside the submitted work. Dr Mior reported receiving grants from the College of Chiropractors of British Columbia during the conduct of the study and grants from the Canadian Chiropractic Association and the Ontario Chiropractic Association outside the submitted work. Dr Hogg-Johnson reported receiving grants from the College of Chiropractors of British Columbia during the conduct of the study and grants from the Canadian Chiropractic Research Foundation outside the submitted work. No other disclosures were reported. The research was supported by funding from the College of Chiropractors of British Columbia to Ontario Tech University, the Canada Research Chairs program (Dr Côté), and the Canadian Chiropractic Research Foundation (Dr Cancelliere).
Would authors independent of chiropractic influence have drawn the same conclusions? I doubt it! While I do appreciate that chiropractors published these negative findings prominently, I feel the conclusions could easily be put much clearer:
There is no clinical evidence to support claims that SMT is efficacious or effective in changing immune system outcomes. Further studies in this area are not warranted.
Osteopathic manipulative treatment (OMT) is frequently recommended by osteopaths for improving breastfeeding. But does it work?
This double-blind randomised clinical trial tested whether OMT was effective for facilitating breastfeeding. Breastfed term infants were eligible if one of the following criteria was met:
- suboptimal breastfeeding behaviour,
- maternal cracked nipples,
- maternal pain.
The infants were randomly assigned to the intervention or the control group. The intervention consisted of two sessions of early OMT, while in the control group, the manipulations were performed on a doll behind a screen. The primary outcome was the exclusive breastfeeding rate at 1 month, which was assessed in an intention-to-treat analysis. Randomisation was computer generated and only accessible to the osteopath practitioner. The parents, research assistants and paediatricians were masked to group assignment.
One hundred twenty-eight mother-infant dyads were randomised, with 64 assigned to each group. In each group, five infants were lost to follow-up. In the intervention group, 31 of 59 (53%) of infants were still exclusively breastfed at 1 month vs 39 of 59 (66%) in the control group. After adjustment for suboptimal breastfeeding behaviour, caesarean section, use of supplements and breast shields, the adjusted OR was 0.44. No adverse effects were reported in either group.
The authors concluded dryly that OMT did not improve exclusive breastfeeding at 1 month.
This is a rigorous trial with clear and expected results. It was conducted in cooperation with a group of 7 French osteopaths, and the study was sponsored by the ‘Société Européenne de Recherche en Osthéopathie Périnatale et Pédiatrique’, the ‘Fonds pour la Recherche en Ostéopathie’ and ‘Formation et Recherche Ostéopathie et Prévention’. The researchers need to be congratulated on publishing this trial and expressing the results so clearly despite the fact that the findings were not what the osteopaths had hoped for.
Three questions come to my mind:
- Is any of the many therapeutic recommendations of osteopaths valid?
- Why was it ever assumed that OMT would be effective?
- Do we really have to test every weird assumption before we can dismiss it?
The authors of this study claim that, in the aging brain, reduction in the pulsation of cerebral vasculature and fluid circulation causes impairment in the fluid exchange between different compartments and lays a foundation for the neuroinflammation that results in Alzheimer disease (AD). The knowledge that lymphatic vessels in the central nervous system play a role in the clearance of brain-derived metabolic waste products opens an unprecedented capability to increase the clearance of macromolecules such as amyloid β proteins. However, currently, there is no pharmacologic mechanism available to increase fluid circulation in the aging brain.
Based on these considerations, the authors conducted a study to demonstrate the influence of an osteopathic cranial manipulative medicine (OCMM) technique, specifically, compression of the fourth ventricle, on spatial memory and changes in substrates associated with mechanisms of metabolic waste clearance in the central nervous system using the naturally aged rat model of AD.
The rats in the OCMM group received the CV4 technique every day for 7 days for 4 to 7 minutes at each session. Rats were anesthetized with 1.5% to 3% isoflurane throughout the procedure. Rats in the UT group were also anesthetized to nullify any influence of isoflurane in spatial learning. During the CV4 procedure, the operator applied mechanical pressure over the rat’s occiput, medial to the junction of the occiput and temporal bone and inferior to the lambdoid suture to place tension on the dural membrane around the fourth ventricle. This gentle pressure was applied to resist cranial flexion with the aim of improving symmetry in the cranial rhythmic impulse (CRI), initiating a rhythmic fluctuation of the CSF, and improving mobility of the cranial bones and dural membranes. This rhythmic fluctuation is thought to be primarily due to flexion and extension that takes place at the synchondrosis between the sphenoid and basiocciput. The treatment end point was achieved when the operator identified that the tissues relaxed, a still point was reached, and improved symmetry or fullness of the CRI was felt. Currently, there is no quantitative measure for the pressure used in this treatment.
The results showed a significant improvement in spatial memory in 6 rats after 7 days of OCMM sessions. Live animal positron emission tomographic imaging and immunoassays revealed that OCMM reduced amyloid β levels, activated astrocytes, and improved neurotransmission in the aged rat brains.
The authors concluded that these findings demonstrate the molecular mechanism of OCMM in aged rats. This study and further investigations will help physicians promote OCMM as an evidence-based adjunctive treatment for patients with AD.
If there ever was an adventurous, over-optimistic extrapolation, this must be it!
Even assuming that all of the findings can be confirmed and replicated, they would be a very far shot from rendering OCMM an evidence-based treatment for AD:
- Rats are not humans.
- Aged rats do not have AD.
- OCMM is not a plausible treatment.
- An animal study is not a clinical trial.
I am at a complete loss to see how the findings of this bizarre animal experiment might help physicians promote OCMM as an evidence-based adjunctive treatment for patients with AD.
