neglect
On 19-30 April 2021 & 1-2 September, 2021 the Professional Conduct Committee of the General Chiropractic Council considered the case of Arleen Scholten, the chiropractor who treated John Lawler, the patient who died after her treatment. Details of the case can be found in the following posts:
- Former chiropractor fined after death of MS patient receiving hyperbaric oxygen therapy
- Death by chiropractic: thoughts about the sad case of Mr Lawler
- The death of Mr Lawler highlights the scandals of chiropractic
- Death by chiropractic neck manipulation? More details on the Lawler case
The Committee considered there had been breaches of the Code, those breaches occurred as a result of Mrs. Scholten’s state of mind at the time and not as a result of a deliberate intention on her part to be inaccurate or misleading. In light of those circumstances, the Committee considered other members of the profession and fully informed members of the public would not consider her failings to be morally reprehensible or deplorable, but rather would consider them regrettable but understandable in the exceptional, albeit tragic, circumstances of this case. The Committee, therefore, agreed with the GCC’s expert witness Mr Brown and did not think Mrs Scholten’s conduct fell far short of the standard required of a registered chiropractor. The Committee was not satisfied, therefore, that her behaviour amounted to unacceptable professional conduct. Accordingly, the Committee found the allegation of UPC not to be well-founded.
How can this be right?
To remind us of the case, here is what I wrote about it previously:
The tragic case of John Lawler who died after being treated by a chiropractor has been discussed on this blog before. Naturally, it generated much discussion which, however, left many questions unanswered. Today, I am able to answer some of them.
- Mr Lawler died because of a tear and dislocation of the C4/C5 intervertebral disc caused by considerable external force.
- The pathologist’s report also shows that the deceased’s ligaments holding the vertebrae of the upper spine in place were ossified.
- This is a common abnormality in elderly patients and limits the range of movement of the neck.
- There was no adequately informed consent by Mr Lawler.
- Mr Lawler seemed to have been under the impression that the chiropractor, who used the ‘Dr’ title, was a medical doctor.
- There is no reason to assume that the treatment of Mr Lawler’s neck would be effective for his pain located in his leg.
- The chiropractor used an ‘activator’ which applies only little and well-controlled force. However, she also employed a ‘drop table’ which applies a larger and not well-controlled force.
I have the permission to publish the submissions made to the coroner by the barrister representing the family of Mr Lawler. The barrister’s evidence shows that:
The chiropractor, Mrs. Scholten, had been accused by the GCC of unacceptable professional conduct. The exact text of the GCC reads as follows :
1. Between 31 July 2017 and 11 August 2017, you provided chiropractic care and
treatment to Patient A at Chiropractic 1st, 68 The Mount, North Yorkshire, YO24 1AR,
(‘the Clinic’).
2. On 11 August 2017 you provided treatment to Patient A which included:
a. a drop technique applied to the thoracic spine;
b. the use of an Activator applied to the thoracic spine;
c. the use of an Activator applied to the cervical spine.
3. Following the drop technique, Patient A indicated he was in discomfort and had lost sensation in his arms and you inappropriately continued treatment.
4. During the course of a subsequent 999 telephone call:
a. you told the call handler that Patient A had laid on the adjusting table and you had used the Activator on his midback;
b. you told the call handler that when you were using the Activator on Patient A’s midback he had said his hands had gone numb;
c. you told the call handler that as Patient A was elderly you had never used any manual adjustment on Patient A;
d. you omitted to tell the call handler that you had used a drop technique on Patient A;
e. you omitted to tell the call handler that Patient A had first expressed discomfort following the drop technique;
f. you omitted to tell the call handler that you had treated Patient A’s cervical spine.
5. When paramedics arrived at the Clinic:
a. you told them words to the effect that you had manipulated Patient A’s midback with the use of an Activator;
b. you told them words to the effect that Patient A had first complained of discomfort when you had been using the Activator on his midback;
c. you omitted to tell the paramedics you had used a drop technique on Patient A;
d. you omitted to tell the paramedics that Patient A had first expressed discomfort following the drop technique;
e. you omitted to tell the paramedics that you had treated Patient A’s cervical spine;
f. you demonstrated the force applied by an Activator on one of the paramedic’s arms.
6. In Patient A’s records for 11 August 2017:
a. you recorded that you had used the Activator on Patient A’s thoracic spine at T2/3 level;
b. you recorded that Patient A had directly said his arms felt numb;
c. you omitted to record that you had used a drop technique on Patient A;
d. you omitted to record that you had treated Patient A’s cervical spine.
7. Your comments and omissions as set out above at 4 and/or 5, and/or as recorded at 6 above, were;
a. inaccurate;
b. misleading;
c. dishonest in that you intended to mislead as to the precise details of the treatment you had provided Patient A
Mr Goldring, on behalf of Mrs Scholten, indicated that the following facts were admitted: Particulars 1, 2(a), 4(a), 4(b), 4(c), 4(d), 5(a), 5(b), 5(c), 5(f), 6(a), 6(b), 6(c) and 7(a) and (b), insofar as they related to the aforementioned admitted facts. The Chair therefore announced that those matters were found proved. Later in the proceedings Mr Goldring indicated that 7(a) and 7(b) were not in fact admitted in respect of 4(c) and 6(b), since it was Mrs Scholten’s case that she had not used any manual adjustment on Patient A, (Particular 4(c)) and the record that Patient A had directly said his arms felt numb was accurate, (Particular 6(b)). Accordingly, the Chair formally announced that position.
END OF QUOTES
I am totally baffled by this ruling.
- What about the fact that the chiropractor’s treatment was not even indicated?
- What about the fact that no informed consent was obtained?
- What about the fear that the chiropractor moved her patient after the injury had happened and made an attempt of ‘mouth to mouth’ resuscitation which seems to have aggravated the injury?
- What about the fact that she misled the paramedics which then caused them not to stabilise Mr. Lawlwer’s neck?
Is the GCC truly saying that, as long as a chiropractor panics, all these mistakes can be excused? I am at a complete loss trying to understand the GCC ruling and very much hope that someone can explain it to me.
Former chiropractor Malcolm Hooper, 61, and hyperbaric oxygen therapy provider Oxymed Pty Ltd have been fined following the death of a customer in 2016. They were each convicted of three work safety-related charges, all of failing to ensure a workplace is safe and without risks to health. Hooper was fined $176,750, while the company was fined $550,000. Oxymed was trading as HyperMed at its South Yarra premises in April 2016 when a long-term client with multiple sclerosis and a history of life-threatening seizures came in for treatment. He was later found unconscious in a single-person hyperbaric chamber, taken to hospital, and placed on life support, but died five days later.
The County Court heard that both the company and Hooper had an inadequate system in place for assessing the risks oxygen therapy could pose to clients, and an inadequate system too for developing plans to eliminate or reduce those risks. In her judgment, County Court judge Amanda Fox said HyperMed wasn’t a hospital nor a medical practice and had been described as an “alternative health facility”. Hooper had already been deregistered in 2013 by the national board for chiropractors for misleading and deceptive advertising about the benefits of hyperbaric treatment.
Hyperbaric oxygen therapy involves administering pure oxygen in a pressurised environment, with the heightened air pressure allowing a patients’ lungs to gather much more oxygen than would be possible under normal conditions. The therapy is not based on strong data. A systematic review failed to find good evidence for hyperbaric oxygen therapy as a treatment of multiple sclerosis:
Multiple sclerosis (MS) is a chronic, inflammatory, and degenerative neurological illness with no cure. It has been suggested that Hyperbaric Oxygen Therapy (HBO(2)T) may slow or reverse the progress of the disease. This article summarizes the clinical evidence for the use of HBO(2)T in the treatment of MS. We conducted a literature review focused on the interaction of hyperbaric oxygenation and MS. In particular, we appraised the clinical data regarding treatment and performed a meta-analysis of the randomized evidence using the methodology of the Cochrane Collaboration. We found 12 randomized studies in the area, all of which were performed between 1983 and 1987. A meta-analysis of this evidence suggests there is no clinically significant benefit from the administration of HBO(2)T. The great majority of randomized trials investigated a course of 20 treatments at pressures between 1.75ATA and 2.5ATA daily for 60-120 min over 4 weeks against a placebo regimen. None have tested the efficacy of HBO(2)T against alternative current best practice. No plausible benefit of HBO(2)T on the clinical course of MS was identified in this review. It remains possible that HBO(2)T is effective in a subgroup of individuals not clearly identified in the trials to date, but any benefit is unlikely to be of great clinical significance. There is some case for further human trials in selected subgroups and for prolonged courses of HBO(2)T at modest pressures, but the case is not strong. At this time, the routine treatment of MS with HBO(2)T is not recommended.
The case reminds me of that of John Lawler. Mr. Lawlwer’s chiropractor also used a therapy that was not indicated, broke his neck (to put it crudely), and subsequently proved herself more than inept in saving his life. It suggests to me that some chiros may not be trained adequately to deal with emergencies. If that is true, they should perhaps focus less on practice-building courses and more on first aid instructions.
Two chiropractors conducted a retrospective review of publicly available data from the California Board of Chiropractic Examiners. Their aim was to determine categories of offense, experience, and gender of disciplined doctors of chiropractic (DC) in California and compare them with disciplined medical physicians in California.
Retrospective reviews of publicly available data from the California Board of Chiropractic Examiners.
The DC disciplinary categories, in descending order, were
- fraud (44%),
- sexual boundary issues (22%),
- other offences (13%),
- abuse of alcohol or drugs (10%),
- negligence or incompetence (6%),
- poor supervision (2%),
- mental impairment (.3%).
The authors concluded that the professions differ in the major reasons for disciplinary actions. Two thirds (67%) of the doctors of chiropractic were disciplined for fraud and sexual boundary issues, compared with 59% for negligence and substance misuse for medical physicians. Additional study in each profession may reveal methods to identify causes and possible intervention for those who are at high risk.
The two authors of this paper should be congratulated for their courage to publish such a review. These figures seem shocking. But I think that in reality some of them might be far higher. Take the important matter of competence, for instance. If you consider it competent that chiropractors treat conditions other than back pain, you might arrive at the above-mentioned figure of 6%. If you consider this as incompetent, as I do, the figure might be one order of magnitude higher (for more on unprofessional conduct by chiropractors see here).
The abstract of the paper does not provide comparisons to the data related to the medical profession. Here they are; relative to doctors, chiropractors are:
- 2x more likely to be involved in malpractice,
- 9x more likely to be practising fraud,
- 2x more likely to transgress sexual boundaries.
The frequency of fraud is particularly striking. Come to think of it, however, it is not all that amazing. I have said it before: chiropractic is in my view mostly about money.
RNZ reported that New Zealand doctors spreading misinformation about Covid-19 may lose their job. Medical Council chair Dr Curtis Walker said a small number of doctors were peddling conspiracies. “It’s questioning the severity of Covid, it’s questioning the safety of vaccination, it’s questioning whether the whole thing is a conspiracy theory. You know you name it, this is what’s been put out there.”
The council has received 13 complaints about medical staff from the public this year – although that included instances of multiple complaints about the same doctor. It comes after it was reported last month that dozens of heath professions, including GPs, signed an open letter opposing the Pfizer vaccine.
Dr Walker said an independent body was investigating to decide if charges should be laid with the Health Practitioners Disciplinary Tribunal. Doctors have a professional duty to provide advice based on evidence, he said. “There’s a mountain of evidence out there of how effective and safe the Covid vaccine is. And we’ve already seen the alternative of unvaccinated populations where millions have died.” Walker said doctors were particularly respected members of the community and their opinions about health carried extra weight. Any found spreading misinformation could potentially lose their jobs and the right to practice medicine.
NZ Royal College of General Practitioners president Dr Samantha Murton said while people could choose not to get vaccinated there were serious consequences if the virus breached the borders. “If those vulnerable people are being given misinformation, they may choose to do something that’s really detrimental to their health. What worries me the most is the poorer people, the people who are at higher risk. If they’re getting this … misinformation then it’s potentially putting their lives in jeopardy.”
Kate Hannah, who researches misinformation at the University of Auckland, said anyone could be sucked in – including highly educated people such as doctors. Most misinformation originated overseas – with people here adapting it to target particular demographics, she said. “And in doing so it targets people’s lived experiences of things like racism in the health system or racism more broadly, or say women’s experiences of the health system where they may have experiences of previously not being listened to.”
Ways to spot misinformation included if someone was trying to sell you something; was asking for donations; or the information was presented to elicit an emotional reaction. “If it’s written in a way that makes you feel upset or scared, or nervous or fearful, you know that’s not normally how we convey good quality public health information. Good quality public health information should provide you with information and make you feel reassured and calm and like you can make good decisions.” Other red flags included asking for personal information or to sign up to receive regular updates – ways to separate you from your current community or sources of information, Hannah said. Covid conspiracies could act as as a gateway, exposing people to online communities espousing far right ideology, misogyny, racism and transphobia, she said.
__________________________
Willful misinformation about a serious health matter amounts to a violation of medical ethics. It, therefore, stands to reason that healthcare professionals who engage in such activities should be reprimanded. If that is so, it applies not just to COVID-19 but to any medical misinformation. Moreover, I should not just apply to doctors, but to all healthcare professionals.
If we do this systematically, it would mean that also providers of so-called alternative medicine (SCAM) might get struck off their professional register, if they make unsubstantiated claims in cases of serious illnesses.
Not realistic, you say?
Why not? After all, medical ethics cannot be bent to protect the interests of SCAM professionals.
WHAT DO YOU THINK?
This study describes the use of so-called alternative medicine (SCAM) among older adults who report being hampered in daily activities due to musculoskeletal pain. Cross-sectional European Social Survey (EES) Round 7 (2014) data from 21 countries were examined for participants aged 55 years and older, who reported musculoskeletal pain that hampered daily activities in the past 12months. From a total of 35,063 individuals who took part in the ESS study, 13,016 (37%) were aged 55 or older; of which 8183 (63%) reported the presence of pain, with a further 4950 (38%) reporting that this pain hampered their daily activities in any way.
Of the 4950 older adult participants reporting musculoskeletal pain that hampered daily activities, the majority (63.5%) were from the West of Europe, reported secondary education or less (78.2%), and reported at least one other health-related problem (74.6%). In total, 1657 (33.5%) reported using at least one SCAM treatment in the previous year. Manual body-based therapies (MBBTs) were most used, including massage therapy (17.9%) and osteopathy (7.0%). Alternative medicinal systems (AMSs) were also popular with 6.5% using homeopathy and 5.3% reporting herbal treatments. A general trend of higher SCAM use in younger participants was noted.
SCAM usage was associated with
- physiotherapy use,
- female gender,
- higher levels of education,
- being in employment,
- living in West Europe
- having multiple health problems.
The authors concluded that a third of older Europeans with musculoskeletal pain report SCAM use in the previous
12 months. Certain subgroups with higher rates of SCAM use could be identified. Clinicians should comprehensively and routinely assess SCAM use among older adults with musculoskeletal pain.
Such studies have the advantage of large sample sizes, and therefore one is inclined to consider their findings to be reliable and informative. Yet, they resemble big fishing operations where all sorts of important and unimportant stuff is caught in the net. When studying such papers, it is wise to remember that associations do not necessarily reveal causal relationships!
Having said this, I find very little information in these already outdated results (they originate from 2014!) that I would not have expected. Perhaps the most interesting aspect is the nature of the most popular SCAMs used for musculoskeletal problems. The relatively high usage of MBBTs had to be expected; in most of the surveyed countries, massage therapy is considered to be not SCAM but mainstream. The fact that 6.5% used homeopathy to ease their musculoskeletal pain is, however, quite remarkable. I know of no good evidence to show that homeopathy is effective for such problems (in case some homeopathy fans disagree, please show me the evidence).
In my view, this indicates that, in 2014, much needed to be done in terms of informing the public about homeopathy. Many consumers mistook homeopathy for herbal medicine (which btw may well have some potential for musculoskeletal pain), and many consumers had been misguided into believing that homeopathy works. They had little inkling that homeopathy is pure placebo therapy. This means they mistreated their conditions, continued to suffer needlessly, and caused an unnecessary financial burden to themselves and/or to society.
Since 2014, much has happened (as discussed in uncounted posts on this blog), and I would therefore assume that the 6.5% figure has come down significantly … but, as you know:
I am an optimist.
I believe in progress.
An article in the Daily Mail (I know, not my favorite newspaper either) reported about a UK court case against the father of an 11-year-old daughter who objected to her being given conventional life-saving treatments for her leukemia. The man was said to be worried about possible side effects and wanted to explore homeopathic and natural therapies, while his estranged wife favored the conventional approach.
Mr Justice Hayden decided that there is ‘no basis’ for the man’s homeopathic option and that specialists can lawfully carry out the conventional treatments. But the father said he believed that previous chemotherapy had already weakened his daughter’s immune system and that the conventional treatment proposed has further side effects. He, therefore, wanted to try homeopathic and natural therapies, including ozone therapy. ‘I am not waiting for her to deteriorate and get worse,’ he told the judge. ‘Chemotherapy is not the only way. There are so many other different therapies I am hoping to try – anything as long as it doesn’t really affect her.’
A specialist treating the girl told the judge that the treatments proposed are the best option and that they know of no homeopathic options which would help. Mr Justice Hayden approved Great Ormond Street’s plan and said doctors should start the treatments as soon as possible. ‘If she receives no treatment then her life expectancy is weeks,’ he said. ‘There is no basis for the father’s homeopathic option.’
This case highlights the indirect risks of homeopathy and similar treatments in an exemplary fashion. The therapies per se might be harmless but the therapists are clearly not. There are enough homeopaths who are deluded enough to persuade their patients that homeopathy can alter the natural history of even serious conditions such as cancer. And, as we have discussed recently, these irresponsible fools are not just from the ranks of the lay-homeopaths (homeopaths who have not been to medical school) who might not know better; they also include medically trained homeopaths and even professors at leading medical schools.
A few months ago, I started contributing to a German blog. This has been fun but only moderately successful in terms of readership. This week, I posted something about a homeopath and his strange attitude towards COVID vaccinations. This post was so far read by around 20 000 people!
As it was so unusually successful (and because there is a big conference today on the subject), I decided to translate it for my non-German readers.
Here we go:
A lot of downright silly stuff is currently being written about vaccine side effects at the moment, not least on Twitter where I recently found the following comment from a medical colleague:
I’ve been a doctor for 25 years now. I have never experienced such an amount of vaccine side effects. I can’t imagine that other colleagues feel differently.
This kind of remark naturally makes you think. So let’s think a little bit about these two sentences. In particular, I would like to ask and briefly answer the following questions:
- How reliable is this physician’s impression?
- What does the reliable evidence say?
- Is it conceivable that this doctor is mistaken?
- What might be the causes of his error?
- Who is the author?
- Why is the tweet questionable?
1. How reliable is this doctor’s impression?
A whole 25 years of professional experience! So we are dealing with a thoroughly experienced doctor. His statement about the current unusually large amount of vaccination side effects should therefore be correct. Nevertheless, one should perhaps bear in mind that the incidence of side effects cannot be determined by rough estimations, but must be precisely quantified. In addition, we also need data on the severity and duration of symptoms. For example, is it only mild pain at the injection site or venous thrombosis? Are the symptoms only temporary, long-lasting, or even permanent? In general, it must be said that the experience of a physician, while not completely insignificant, does not constitute evidence. Oscar Wilde once said, “experience is the name we give to our mistakes.”
2. What does the reliable evidence tell us?
Even if the good doctor had 100 years of professional experience and even if he could accurately characterize the side effects, his experience would be trivial compared to the hard data we have on this subject. Nearly 2 billion vaccinations have now been performed worldwide, and we are therefore in the fortunate position of having reliable statistics to guide us. And they show that side effects such as pain at the injection site, fatigue, and headaches are quite common, while serious problems are very rare.[1] A recent summary comes to the following conclusion (my translation)[2]:
The current data suggests that the currently approved mRNA-based COVID-19 vaccines are safe and effective for the vast majority of the population. Furthermore, broad-based vaccine uptake is critical for achieving herd immunity; an essential factor in decreasing future surges of COVID-19 infections. Ensuring sufficient COVID-19 vaccination adoption by the public will involve attending to the rising vaccine hesitancy among a pandemic-weary population. Evidence-based approaches at the federal, state, city, and organizational levels are necessary to improve vaccination efforts and to decrease hesitancy. Educating the general public about the safety of the current and forthcoming vaccines is of vital consequence to public health and ongoing and future large-scale vaccination initiatives.
3. Is it conceivable that this doctor is mistaken?
In answering this question, I agree with Oscar Wilde. The evidence very clearly contradicts the physician’s impression. So the doctor seems to be mistaken — at least about the incidence of side effects that are not completely normal and thus to be expected. Even if indeed ‘other colleagues feel no differently’, such a cumulative experience would still mislead us. The plural of ‘anecdote’ is ‘anecdotes’ and not ‘evidence’.
4. What might be the causes of his error?
I wonder whether our doctor perhaps did not see or did not want to see the following circumstance: It is inevitable that a physician, at a time when soon 50% of all Germans were vaccinated, also sees a lot of patients complaining about side effects. He has never seen anything like that in his 25-year career! That’s because we haven’t been hit by a pandemic in the last 25 years. For a similar reason, the colleague will treat far fewer frostbites in midsummer than during a severe winter. The only surprising thing would be not to see more patients reporting vaccine side effects during the biggest vaccination campaign ever.
5. Who is the author?
At this point, we should ask, who is actually the author and author of the above tweet? Perhaps the answer to this question will provide insight into his motivation for spreading nonsense? Dr. Thomas Quak (no, I did not invent the name) is a practicing homeopath in Fürstenfeldbruck, Germany. Like many homeopaths, this Quak probably has a somewhat disturbed relationship to vaccination. In his case, this goes as far as recommending several vaccine-critical machinations on his website and even offering ‘critical vaccination advice’ as a special service.[3]
Now we can immediately put the Quak tweet in a better perspective. Dr. Quak is a vaccination opponent or critic and wants to warn the public: for heaven’s sake, don’t get vaccinated folks; side effects are more common than ever!!!! Therefore, he also conceals the fact that the side-effects are completely normal, short-term vaccination reactions, which are ultimately of no significance.
6. Why is the tweet concerning?
Perhaps you feel that the Quak and his Quack tweet are irrelevant? What harm can a single tweet do, and who cares about a homeopath from Fürstenfeldbruck? As good as none and nobody! However, the importance does not lie in a single homeopath unsettling the population; it consists in the fact that such things currently happen every day thousandfold.
In their narrow-mindedness, vaccination opponents of all shades want to make us believe that they are concerned about our well-being because they know more than we and all the experts (who are of course bought by the pharmaceutical industry). But if you scratch just a little at the surface of their superficiality, it turns out that the exact opposite is true. They are ill-informed and only interested in spreading their hare-brained, misanthropic ideology.
And why do homeopaths do this? There are certainly several reasons. Although Hahnemann himself was impressed by the success of vaccination, which was invented in his time and hailed as a breakthrough, most of his successors soon sided with vaccination critics. Many do so by warning (like our Quak) of side effects, thinking that they are thus protecting their patients. However, they ignore two very important points:
- Even if the dangers of vaccinations were much greater than they actually are (no one is claiming that they are completely harmless), the benefits would still far outweigh the potential harms.
- If the Quaks (and all the quacks) of this world succeeded in dissuading a sizable percentage of the population from vaccinating and thus save them from the ‘oh-so-dangerous side effects’, they would still be doing a real disservice to public health. With regard to COVID-19, this would mean that the pandemic would remain with us in the long term and cost many more lives.
Whatever the motives of the homeopathic anti-vax brigade, it is certain that their attitude is a threat to our health. This has repeatedly made me state:
The homeopathic pills may be harmless, but unfortunately, the homeopaths are not!
REFERENCES
- COVID-19 vaccine availability: what are the side effects? | British Journal of General Practice (bjgp.org) ︎
- Review the safety of Covid-19 mRNA vaccines: a review – PubMed (nih.gov) ︎
- Vaccination Information (doktor-quak.de) ︎
‘CLAMP DOWN ON THE BOGUS SCIENCE OF HOMEOPATHY’ is the title of a comment by Oliver Klamm in The Times today. Here is the background to his article.
In September 2020, the website of Homeopathy UK, www.homeopathy-uk.org, featured a page titled “Conditions Directory” with text that stated “Please find below a list of conditions where homeopathy can help …” followed by a list of medical conditions that included depression, diabetes, infertility, psoriasis and asthma. When consumers clicked-through the links to the conditions listed on that page, they were taken to separate pages for each that contained anecdotal descriptions from doctors detailing how they had applied homeopathic methods to the relevant conditions.
The UK Advertising Standards Authority received a complainant that challenged whether the ad discouraged essential treatment for conditions for which medical supervision should be sought, namely depression, diabetes, infertility, psoriasis and asthma.
The response of ‘Homeopathy UK’ said that, as a registered charity, they sought to share information about homeopathy for the benefit of others, rather than for commercial gain, and that they would always recommend that patients seeking homeopathic care did so under the supervision of a qualified medical practitioner…
The ASA upheld the complaint and argued as follows:
The CAP Code required that marketers must not discourage essential treatment for conditions for which medical supervision should be sought. For example, they must not offer specific advice on, diagnosis or treatment for such conditions unless that advice, diagnosis or treatment was conducted under the supervision of a suitably qualified medical professional. The ad referred to “depression”, “diabetes”, “infertility”, “psoriasis” and “asthma”, which we considered were conditions for which medical supervision should be sought. Any advice, diagnosis or treatment, therefore, must be conducted under the supervision of a suitably qualified medical professional. We acknowledged that the articles had been written by GMC-registered doctors, who we considered would be suitably qualified to offer advice, diagnosis or treatment. However, we noted that the ad and the articles to which it linked referred to homeopathy in general, rather than treatment by a specific individual. We understood that there were no minimum professional qualifications required to practice homeopathy, which could result in consumers being advised, diagnosed, or treated for the conditions listed in the ad by a practitioner with no medical qualification. We therefore considered Homeopathy UK would not be able to demonstrate that all such treatment would be conducted under the supervision of a suitably qualified health professional.
Furthermore, we understood that, although elsewhere on the website there were links to specific clinics, not all treatment would be conducted under the supervision of a suitably qualified health professional across those clinics. Because Homeopathy UK had not supplied evidence that treatment would always be carried out by a suitably qualified health professional. Also, because reference to the conditions listed in the ad, and discussed in the related articles, could discourage consumers from seeking essential treatment under the supervision of a suitably qualified health professional, we concluded that the ad had breached the Code.
On that point the ad breached CAP Code (Edition 12) rule 12.2 (Medicines, medical devices, health-related products and beauty products).
The ad must not appear again in the form complained about. We told Homeopathy UK to ensure their future marketing communications did not to refer to conditions for which advice should be sought from suitably qualified health professionals.
___________________________
Depression, diabetes, and asthma have few things in common. Just two characteristics stand out, in my view:
- they are potentially fatal;
- homeopathy is ineffective in changing their natural history.
- It was therefore high time that the ASA stopped this criminally dangerous nonsense of deluded homeopaths.
The article by Oliver Klamm concludes with the following wise words about homeopathy:
“For public officials and opinion formers, the time for appeasing this dangerous quackery should be long past.”
In staunch defiance of the evidence and common sense, Prince Charles has long defended homeopathy. Apparently, he not only uses it himself but also employs it for his animals. Claiming that his cattle don’t know about placebo effects, he seems convinced it works better than a placebo. Homeopaths are naturally delighted to have his royal support, not least the ones from India where homeopathy has been hugely popular for many years.
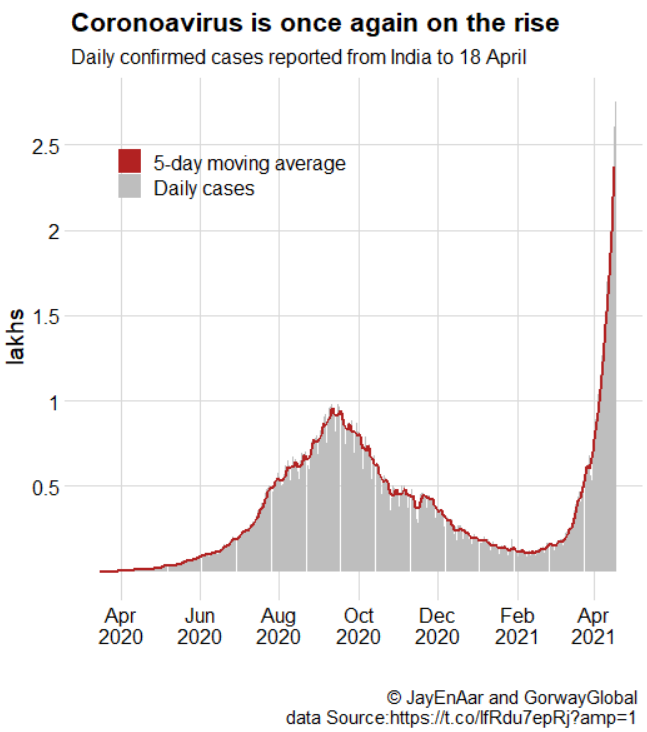
From the beginning of the pandemic, many Indian enthusiasts have claimed that homeopathy can effectively prevent and treat COVID-19 infections. In parts of India, homeopathy was thus employed on a population basis in an attempt to prevent the spread of the disease. There were voices that warned of a disaster but the Indian enthusiasm for homeopathy as an effective anti-COVID-19 therapy won the day.
When Prince Charles fell ill with COVID-19, Indian officials did not hesitate to claim that his quick recovery was due to the homeopathic treatment he had received. Charles’ officials denied this but in India, the story was reported widely and lent crucial support to the myth that homeopathy would provide a solution to the pandemic. Subsequently, Indian officials began to rely even more on the alleged power of homeopathy.
Today, the consequences of these actions are becoming tragically visible: With more than 15 million confirmed cases, India is experiencing a catastrophic tsunami of COVID-19 infections. Its healthcare system is close to collapse, and the high prevalence of the virus provides dangerously fertile grounds for the development of mutants. One does not need to be a clairvoyant to predict that, in turn, these will cause problems on a global basis.
Why am I telling you all this?
I think this depressing sequence of events shows in exemplary fashion what damage ill-informed VIP support for an ineffective therapy can do. Many people tend to feel that Charles’ passion for homeopathy might perhaps be laughable but is essentially harmless. I beg to differ. I am not saying that Charles instructed Indian officials to employ homeopathy the way they did. I am even emphasizing that Charles’ officials denied that homeopathy had anything to do with his speedy recovery after his illness. But I am saying that Charles’ life-long promotion of homeopathy combined with his quick recovery motivated Indian officials, even more, to ignore the evidence and decide to heavily rely on homeopathy.
This decision has cost uncounted lives and will cause many more in the near future. I submit that the seemingly harmless promotion of unproven or disproven treatments such as homeopathy can be a deadly dangerous game indeed.
After yesterday’s post entitled ‘What does a holistic doctor do that a traditional doctor doesn’t?‘, I thought it would only be fair to turn the question around and ask: What does a proper doctor do that a holistic healer doesn’t? The answers will upset a lot of practitioners of alternative medicine (SCAM), but so be it.
So, what does a proper doctor do that a holistic healer doesn’t?
I suggest several answers and hope that the readers of this blog will contribute to further points. Many of them center around safeguarding the public:
- Proper doctors avoid confusing or misleading the public with titles they do not have.
- They do have rigorous education and training.
- They avoid making false therapeutic claims.
- They adhere to the ethical standards of their profession.
- They resist the temptation to advertise their services to the consumer.
- They do their best to identify the cause of their patient’s symptoms.
- They treat the causes of disease whenever possible.
- They avoid pretending that they always have all the answers.
- They abide by the rules of evidence-based medicine.
- They are aware that almost any effective treatment comes with adverse effects.
- They try to keep abreast with the rapid advances in medicine.
- They know that a patient is more than a diagnostic label.
- They try to treat patients holistically.
At this stage, I can hear some readers shout in anger:
- Ahh, but that is rubbish!
- I know doctors who are not at all like that!
- You are idealizing your profession!
- This is little more than wishful thinking!
Yes, I know that many patients are disappointed and have had a bad experience with conventional medicine. That is one of the reasons many try SCAM. I know that many doctors occasionally fail to live up to the ideal that I depicted above. And I fear that some do so more often than just occasionally.
This is regrettable and occasionally it is unacceptable. Medicine is populated not by perfect people; it is run by humans like you and me. Humans are fallible. Doctors have bad days just like you and me. If that happens regularly, we need to address the problems that may the cause of the deficit. If necessary, the case has to go before a disciplinary hearing. There are thousands of experts who are dedicated to improving healthcare in the hope of generating progress.
The point I was trying to make is that there is such a thing as an ideal physician. It relies on:
- rigorous training,
- ethical codes,
- post-graduate education,
- supervision,
- governance,
- swift disciplinary procedures,
- advances brought about through colossal research efforts,
- etc., etc.
Do ‘holistic healers’ offer all of these safeguards?
The sad answer is no.
For those who disagree, let’s briefly look at a recent example.
John Lawler died in 2017 after being treated by a chiropractor (as discussed on this blog before).
- Mr. Lawler died because of a tear and dislocation of the C4/C5 intervertebral disc caused by a considerable external force.
- The pathologist’s report also showed that the deceased’s ligaments holding the vertebrae of the upper spine in place were ossified.
- This is a common abnormality in elderly patients and limits the range of movement of the neck.
- There was no adequately informed consent by Mr. Lawler.
- Mr. Lawler seemed to have been under the impression that the chiropractor, who used the ‘Dr’ title, was a medical doctor.
- There is no reason to assume that the treatment of Mr. Lawler’s neck would be effective for his pain located in his leg.
- The chiropractor used an ‘activator’ that applies only little and well-controlled force. However, she also employed a ‘drop table’ which applies a larger and not well-controlled force.
As far as I can see, most of the safeguards and standards that apply to conventional medicine were not in place to safeguard Mr. Lawler. And that includes a timely disciplinary hearing of the case. Mr. Lawler died in 2017! The CCG has been dragging its feet ever since, and, as far as I know, the chiropractor was meanwhile allowed to practise. The HEARING BEFORE THE PROFESSIONAL CONDUCT COMMITTEE OF THE GENERAL CHIROPRACTIC COUNCIL has now been scheduled to commence on 19 April 2021.
I know, it’s just an example. But it should make us think.