meta-analysis
This meta-analysis was conducted by researchers affiliated to the Evangelical Clinics Essen-Mitte, Department of Internal and Integrative Medicine, Faculty of Medicine, University of Duisburg-Essen, Germany. (one of its authors is an early member of my ALTERNATIVE MEDICINE HALL OF FAME). The paper assessed the safety of acupuncture in oncological patients.
The PubMed, Cochrane Central Register of Controlled Trials, and Scopus databases were searched from their inception to August 7, 2020. Randomized controlled trials in oncological patients comparing invasive acupuncture with sham acupuncture, treatment as usual (TAU), or any other active control were eligible. Two reviewers independently extracted data on study characteristics and adverse events (AEs). Risk of bias was assessed using the Cochrane Risk of Bias Tool.
Of 4590 screened articles, 65 were included in the analyses. The authors observed that acupuncture was not associated with an increased risk of intervention-related AEs, nonserious AEs, serious AEs, or dropout because of AEs compared with sham acupuncture and active control. Compared with TAU, acupuncture was not associated with an increased risk of intervention-related AEs, serious AEs, or dropout because of AEs but was associated with an increased risk for nonserious AEs (odds ratio, 3.94; 95% confidence interval, 1.16-13.35; P = .03). However, the increased risk of nonserious AEs compared with TAU was not robust against selection bias. The meta-analyses may have been biased because of the insufficient reporting of AEs in the original randomized controlled trials.
The authors concluded that the current review indicates that acupuncture is as safe as sham acupuncture and active controls in oncological patients. The authors recommend researchers heed the CONSORT (Consolidated Standards of Reporting Trials) safety and harm extension for reporting to capture the side effects and better investigate the risk profile of acupuncture in oncology.
You might think this article is not too bad. So, why do I feel that this paper is so bad?
One reason is that the authors included evidence up to August 2020. Since then, there must have been hundreds of further papers on acupuncture. The article was therefore out of date before it was published.
But that is by no means my main reason. We know from numerous investigations that acupuncture studies often fail to report AEs (and thus violate publication ethics). This means that this new analysis is merely an amplification of the under-reporting. It is, in other words, a means of perpetuating a wrong message.
Yes, you might say, but the authors acknowledge this; they even state in the abstract that “The meta-analyses may have been biased because of the insufficient reporting of AEs in the original randomized controlled trials.” True, but this fact does not erase the mistake, it merely concedes it. At the very minimum, the authors should have phrased their conclusion differently, e.g.: the current review confirms that AEs of acupuncture are under-reported in RCTs. Therefore, a meta-analysis of RCTs is unable to verify whether acupuncture is safe. From other types of research, we know that it can cause serious AEs.
An even better solution would have been to abandon or modify the research project when they first came across the mountain of evidence showing that RCTs often fail to mention AEs.
As it stands, the conclusion that acupuncture is as safe as sham acupuncture is simply not true. Since the article probably looks sound to naive readers, I feel that is a particularly good candidate for the WORST PAPER OF 2022 COMPETITION.
PS
For those who are interested, here are 4 of my own peer-reviewed articles on the safety of acupuncture (much more can, of course, be found on this blog):
- Patient safety incidents from acupuncture treatments: a review of reports to the National Patient Safety Agency – PubMed (nih.gov)
- Acupuncture–a critical analysis – PubMed (nih.gov)
- Prospective studies of the safety of acupuncture: a systematic review – PubMed (nih.gov)
- The risks of acupuncture – PubMed (nih.gov)
I know, transcutaneous electrical nerve stimulation (TENS) is not really a so-called alternative medicine (SCAM) but it is used by many SCAM practitioners and pain patients. It is, therefore, worth knowing whether it works.
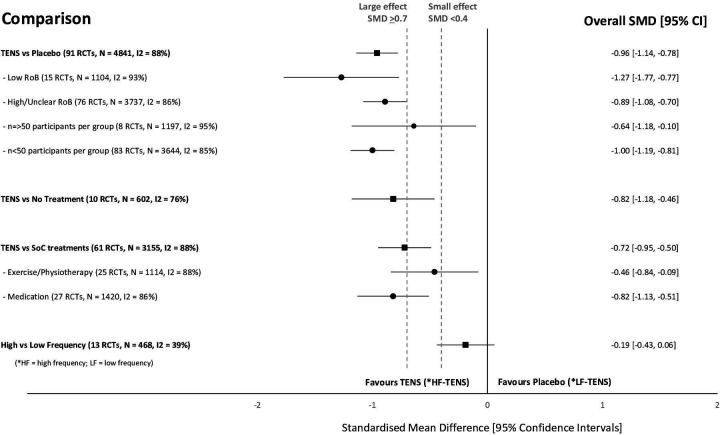
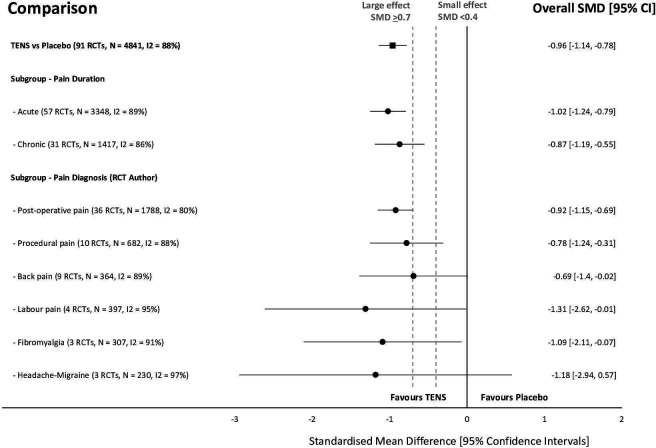
This systematic review investigated the efficacy and safety of transcutaneous electrical nerve stimulation (TENS) for the relief of pain in adults. All randomized clinical trials (RCTs) were considered which compared strong non-painful TENS at or close to the site of pain versus placebo or other treatments in adults with pain, irrespective of diagnosis.
Reviewers independently screened, extracted data, and assessed the risk of bias (RoB, Cochrane tool) and certainty of evidence (Grading and Recommendations, Assessment, Development, and Evaluation). The outcome measures were the mean pain intensity and the proportions of participants achieving reductions of pain intensity (≥30% or >50%) during or immediately after TENS. Random effect models were used to calculate standardized mean differences (SMD) and risk ratios. Subgroup analyses were related to trial methodology and characteristics of pain.
The review included 381 RCTs (24 532 participants). Pain intensity was lower during or immediately after TENS compared with placebo (91 RCTs, 92 samples, n=4841, SMD=-0·96 (95% CI -1·14 to -0·78), moderate-certainty evidence). Methodological (eg, RoB, sample size) and pain characteristics (eg, acute vs chronic, diagnosis) did not modify the effect. Pain intensity was lower during or immediately after TENS compared with pharmacological and non-pharmacological treatments used as part of standard of care (61 RCTs, 61 samples, n=3155, SMD = -0·72 (95% CI -0·95 to -0·50], low-certainty evidence). Levels of evidence were downgraded because of small-sized trials contributing to imprecision in magnitude estimates. Data were limited for other outcomes including adverse events which were poorly reported, generally mild, and not different from comparators.
The authors concluded that there was moderate-certainty evidence that pain intensity is lower during or immediately after TENS compared with placebo and without serious adverse events.
This is an impressive review, not least because of its rigorous methodology and the large number of included trials. Its results are clear and convincing. In the words of the authors: “TENS should be considered in a similar manner to rubbing, cooling or warming the skin to provide symptomatic relief of pain via neuromodulation. One advantage of TENS is that users can adjust electrical characteristics to produce a wide variety of TENS sensations such as pulsate and paraesthesiae to combat the dynamic nature of pain. Consequently, patients need to learn how to use a systematic process of trial and error to select electrode positions and electrical characteristics to optimise benefits and minimise problems on a moment to moment basis.”
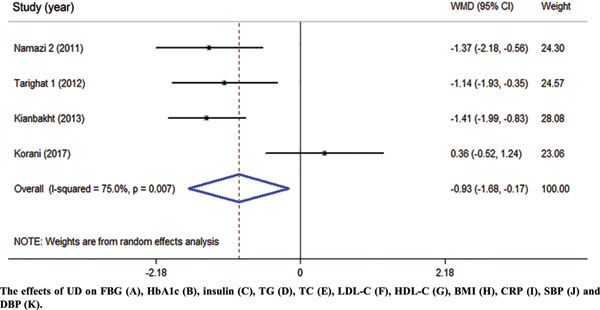
This systematic review and meta-analysis of clinical trials were performed to summarize the evidence of the effects of Urtica dioica (UD) consumption on metabolic profiles in patients with type 2 diabetes mellitus (T2DM).
Eligible studies were retrieved from searches of PubMed, Embase, Scopus, Web of Science, Cochrane Library, and Google Scholar databases until December 2019. Cochran (Q) and I-square statistics were used to examine heterogeneity across included clinical trials. Data were pooled using a fixed-effect or random-effects model and expressed as weighted mean difference (WMD) and 95% confidence interval (CI).
Among 1485 citations, thirteen clinical trials were found to be eligible for the current metaanalysis. UD consumption significantly decreased levels of fasting blood glucose (FBG) (WMD = – 17.17 mg/dl, 95% CI: -26.60, -7.73, I2 = 93.2%), hemoglobin A1c (HbA1c) (WMD = -0.93, 95% CI: – 1.66, -0.17, I2 = 75.0%), C-reactive protein (CRP) (WMD = -1.09 mg/dl, 95% CI: -1.64, -0.53, I2 = 0.0%), triglycerides (WMD = -26.94 mg/dl, 95 % CI = [-52.07, -1.82], P = 0.03, I2 = 90.0%), systolic blood pressure (SBP) (WMD = -5.03 mmHg, 95% CI = -8.15, -1.91, I2 = 0.0%) in comparison to the control groups. UD consumption did not significantly change serum levels of insulin (WMD = 1.07 μU/ml, 95% CI: -1.59, 3.73, I2 = 63.5%), total-cholesterol (WMD = -6.39 mg/dl, 95% CI: -13.84, 1.05, I2 = 0.0%), LDL-cholesterol (LDL-C) (WMD = -1.30 mg/dl, 95% CI: -9.95, 7.35, I2 = 66.1%), HDL-cholesterol (HDL-C) (WMD = 6.95 mg/dl, 95% CI: -0.14, 14.03, I2 = 95.4%), body max index (BMI) (WMD = -0.16 kg/m2, 95% CI: -1.77, 1.44, I2 = 0.0%), and diastolic blood pressure (DBP) (WMD = -1.35 mmHg, 95% CI: -2.86, 0.17, I2= 0.0%) among patients with T2DM.
The authors concluded that UD consumption may result in an improvement in levels of FBS, HbA1c, CRP, triglycerides, and SBP, but did not affect levels of insulin, total-, LDL-, and HDL-cholesterol, BMI, and DBP in patients with T2DM.
Several plants have been reported to affect the parameters of diabetes. Whenever I read such results, I cannot stop wondering whether this is a good or a bad thing. It seems to be positive at first glance, yet I can imagine at least two scenarios where such effects might be detrimental:
- A patient reads about the antidiabetic effects and decides to swap his medication for the herbal remedy which is far less effective. Consequently, the patient’s metabolic control is insufficient.
- A patient adds the herbal remedy to his therapy. Consequently, his blood sugar drops too far and he suffers a hypoglycemic episode.
My advice to diabetics is therefore this: if you want to try herbal antidiabetic treatments, please think twice. And if you persist, do it only under the close supervision of your doctor.
There is hardly a form of therapy under the SCAM umbrella that is not promoted for back pain. None of them is backed by convincing evidence. This might be because back problems are mostly viewed in SCAM as mechanical by nature, and psychological elements are thus often neglected.
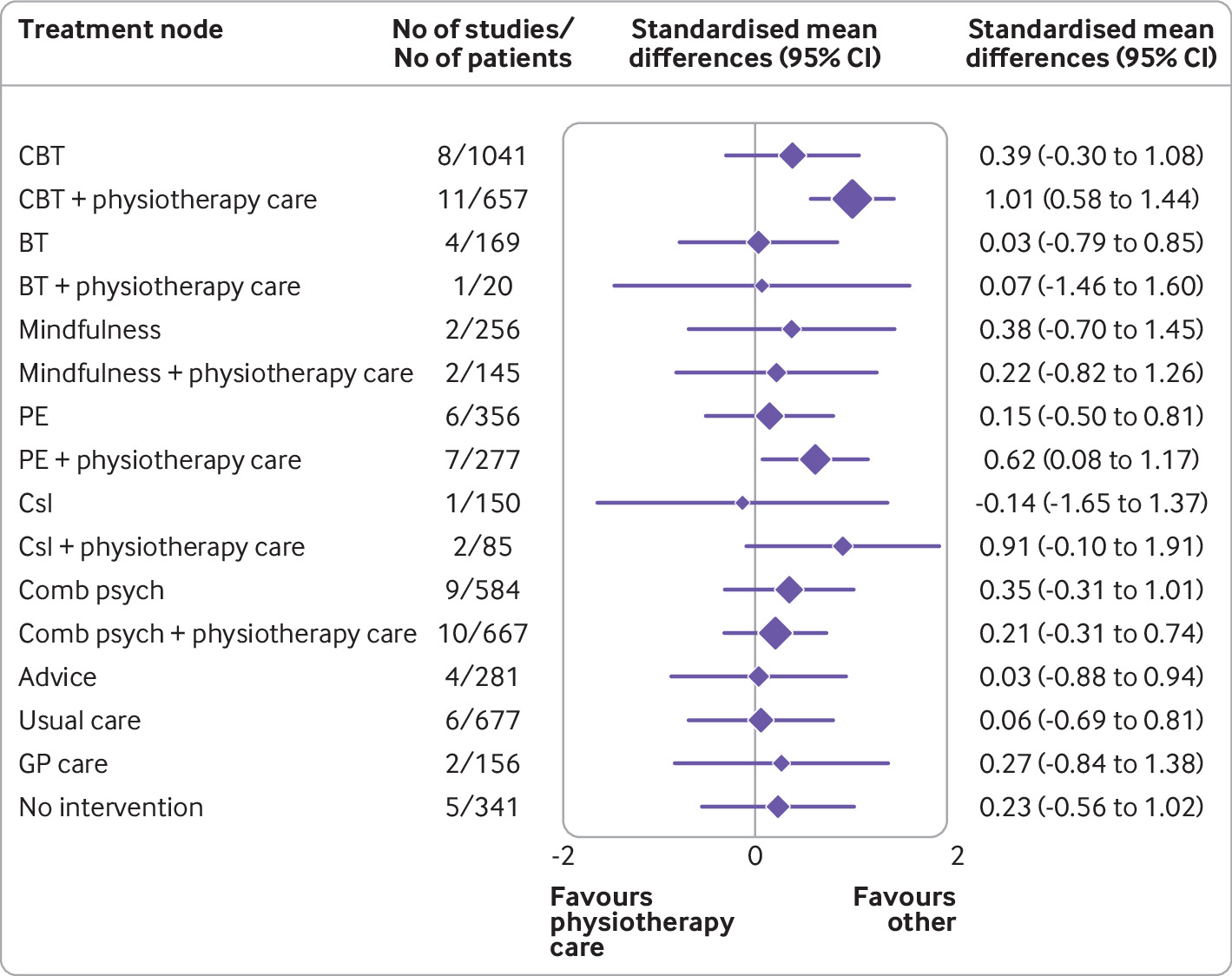
This systematic review with network meta-analysis determined the comparative effectiveness and safety of psychological interventions for chronic low back pain. Randomised controlled trials comparing psychological interventions with any comparison intervention in adults with chronic, non-specific low back pain were included.
A total of 97 randomised controlled trials involving 13 136 participants and 17 treatment nodes were included. Inconsistency was detected at short term and mid-term follow-up for physical function, and short term follow-up for pain intensity, and were resolved through sensitivity analyses. For physical function, cognitive behavioural therapy (standardised mean difference 1.01, 95% confidence interval 0.58 to 1.44), and pain education (0.62, 0.08 to 1.17), delivered with physiotherapy care, resulted in clinically important improvements at post-intervention (moderate-quality evidence). The most sustainable effects of treatment for improving physical function were reported with pain education delivered with physiotherapy care, at least until mid-term follow-up (0.63, 0.25 to 1.00; low-quality evidence). No studies investigated the long term effectiveness of pain education delivered with physiotherapy care. For pain intensity, behavioural therapy (1.08, 0.22 to 1.94), cognitive behavioural therapy (0.92, 0.43 to 1.42), and pain education (0.91, 0.37 to 1.45), delivered with physiotherapy care, resulted in clinically important effects at post-intervention (low to moderate-quality evidence). Only behavioural therapy delivered with physiotherapy care maintained clinically important effects on reducing pain intensity until mid-term follow-up (1.01, 0.41 to 1.60; high-quality evidence).
Forest plot of network meta-analysis results for physical function at post-intervention. *Denotes significance at p<0.05. BT=behavioural therapy; CBT=cognitive behavioural therapy; Comb psych=combined psychological approaches; Csl=counselling; GP care=general practitioner care; PE=pain education; SMD=standardised mean difference. Physiotherapy care was the reference comparison group
The authors concluded that for people with chronic, non-specific low back pain, psychological interventions are most effective when delivered in conjunction with physiotherapy care (mainly structured exercise). Pain education programmes (low to moderate-quality evidence) and behavioural therapy (low to high-quality evidence) result in the most sustainable effects of treatment; however, uncertainty remains as to their long term effectiveness. Although inconsistency was detected, potential sources were identified and resolved.
The authors’ further comment that their review has identified that pain education, behavioural therapy, and cognitive behavioural therapy are the most effective psychological interventions for people with chronic, non-specific LBP post-intervention when delivered with physiotherapy care. The most sustainable effects of treatment for physical function and fear avoidance are achieved with pain education programmes, and for pain intensity, they are achieved with behavioural therapy. Although their clinical effectiveness diminishes over time, particularly in the long term (≥12 months post-intervention), evidence supports the clinical benefits of combining physiotherapy care with these specific types of psychological interventions at the onset of treatment. The small total sample size at long term follow-up (eg, for physical function, n=6986 at post-intervention v n=2469 for long term follow-up; for pain intensity, n=6963 v n=2272) has resulted in wide confidence intervals at this time point; however, the magnitude and direction of the pooled effects seemed to consistently favour the psychological interventions delivered with physiotherapy care, compared with physiotherapy care alone.
Commenting on their paper, two of the authors, Ferriera and Ho, said they would like to see the guidelines on LBP therapy updated to provide more specific recommendations, the “whole idea” is to inform patients, so they can have conversations with their GP or physiotherapist. Patients should not come to consultations with a passive attitude of just receiving whatever people tell them because unfortunately people still receive the wrong care for chronic back pain,” Ferreira says. “Clinicians prescribe anti-inflammatories or paracetamol. We need to educate patients and clinicians about options and more effective ways of managing pain.”
Is there a lesson here for patients consulting SCAM practitioners for their back pain? Perhaps it is this: it is wise to choose the therapy that has been demonstrated to be effective while having the least potential for harm! And this is not chiropractic or any other form of SCAM. It could, however, well be a combination of physiotherapeutic exercise and psychological therapy.
The Lancet is a top medical journal, no doubt. But even such journals can make mistakes, even big ones, as the Wakefield story illustrates. But sometimes, the mistakes are seemingly minor and so well hidden that the casual reader is unlikely to find them. Such mistakes can nevertheless be equally pernicious, as they might propagate untruths or misunderstandings that have far-reaching consequences.
A recent Lancet paper might be an example of this phenomenon. It is entitled “Management of common clinical problems experienced by survivors of cancer“, unquestionably an important subject. Its abstract reads as follows:
_______________________
Improvements in early detection and treatment have led to a growing prevalence of survivors of cancer worldwide.
Models of care fail to address adequately the breadth of physical, psychosocial, and supportive care needs of those who survive cancer. In this Series paper, we summarise the evidence around the management of common clinical problems experienced by survivors of adult cancers and how to cover these issues in a consultation. Reviewing the patient’s history of cancer and treatments highlights potential long-term or late effects to consider, and recommended surveillance for recurrence. Physical consequences of specific treatments to identify include cardiac dysfunction, metabolic syndrome, lymphoedema, peripheral neuropathy, and osteoporosis. Immunotherapies can cause specific immune-related effects most commonly in the gastrointestinal tract, endocrine system, skin, and liver. Pain should be screened for and requires assessment of potential causes and non-pharmacological and pharmacological approaches to management. Common psychosocial issues, for which there are effective psychological therapies, include fear of recurrence, fatigue, altered sleep and cognition, and effects on sex and intimacy, finances, and employment. Review of lifestyle factors including smoking, obesity, and alcohol is necessary to reduce the risk of recurrence and second cancers. Exercise can improve quality of life and might improve cancer survival; it can also contribute to the management of fatigue, pain, metabolic syndrome, osteoporosis, and cognitive impairment. Using a supportive care screening tool, such as the Distress Thermometer, can identify specific areas of concern and help prioritise areas to cover in a consultation.
_____________________________
You can see nothing wrong? Me neither! We need to dig deeper into the paper to find what concerns me.
In the actual article, the authors state that “there is good evidence of benefit for … acupuncture …”[1]; the same message was conveyed in one of the tables. In support of these categorical statements, the authors quote the current Cochrane review entitled “Acupuncture for cancer pain in adults”. Its abstract reads as follows:
Background: Forty per cent of individuals with early or intermediate stage cancer and 90% with advanced cancer have moderate to severe pain and up to 70% of patients with cancer pain do not receive adequate pain relief. It has been claimed that acupuncture has a role in management of cancer pain and guidelines exist for treatment of cancer pain with acupuncture. This is an updated version of a Cochrane Review published in Issue 1, 2011, on acupuncture for cancer pain in adults.
Objectives: To evaluate efficacy of acupuncture for relief of cancer-related pain in adults.
Search methods: For this update CENTRAL, MEDLINE, EMBASE, PsycINFO, AMED, and SPORTDiscus were searched up to July 2015 including non-English language papers.
Selection criteria: Randomised controlled trials (RCTs) that evaluated any type of invasive acupuncture for pain directly related to cancer in adults aged 18 years or over.
Data collection and analysis: We planned to pool data to provide an overall measure of effect and to calculate the number needed to treat to benefit, but this was not possible due to heterogeneity. Two review authors (CP, OT) independently extracted data adding it to data extraction sheets. Data sheets were compared and discussed with a third review author (MJ) who acted as arbiter. Data analysis was conducted by CP, OT and MJ.
Main results: We included five RCTs (285 participants). Three studies were included in the original review and two more in the update. The authors of the included studies reported benefits of acupuncture in managing pancreatic cancer pain; no difference between real and sham electroacupuncture for pain associated with ovarian cancer; benefits of acupuncture over conventional medication for late stage unspecified cancer; benefits for auricular (ear) acupuncture over placebo for chronic neuropathic pain related to cancer; and no differences between conventional analgesia and acupuncture within the first 10 days of treatment for stomach carcinoma. All studies had a high risk of bias from inadequate sample size and a low risk of bias associated with random sequence generation. Only three studies had low risk of bias associated with incomplete outcome data, while two studies had low risk of bias associated with allocation concealment and one study had low risk of bias associated with inadequate blinding. The heterogeneity of methodologies, cancer populations and techniques used in the included studies precluded pooling of data and therefore meta-analysis was not carried out. A subgroup analysis on acupuncture for cancer-induced bone pain was not conducted because none of the studies made any reference to bone pain. Studies either reported that there were no adverse events as a result of treatment, or did not report adverse events at all.
Authors’ conclusions: There is insufficient evidence to judge whether acupuncture is effective in treating cancer pain in adults.
This conclusion is undoubtedly in stark contrast to the categorical statement of the Lancet authors: “there is good evidence of benefit for … acupuncture …“
What should be done to prevent people from getting misled in this way?
- The Lancet should correct the error. It might be tempting to do this by simply exchanging the term ‘good’ with ‘some’. However, this would still be misleading, as there is some evidence for almost any type of bogus therapy.
- Authors, reviewers, and editors should do their job properly and check the original sources of their quotes.
PS
In case someone argued that the Cochrane review is just one of many, here is the conclusion of an overview of 15 systematic reviews on the subject: The … findings emphasized that acupuncture and related therapies alone did not have clinically significant effects at cancer-related pain reduction as compared with analgesic administration alone.
Today, several UK dailies report about a review of osteopathy just published in BMJ-online. The aim of this paper was to summarise the available clinical evidence on the efficacy and safety of osteopathic manipulative treatment (OMT) for different conditions. The authors conducted an overview of systematic reviews (SRs) and meta-analyses (MAs). SRs and MAs of randomised controlled trials evaluating the efficacy and safety of OMT for any condition were included.
The literature searches revealed nine SRs or MAs conducted between 2013 and 2020 with 55 primary trials involving 3740 participants. The SRs covered a wide range of conditions including
- acute and chronic non-specific low back pain (NSLBP, four SRs),
- chronic non-specific neck pain (CNSNP, one SR),
- chronic non-cancer pain (CNCP, one SR),
- paediatric (one SR),
- neurological (primary headache, one SR),
- irritable bowel syndrome (IBS, one SR).
Although with different effect sizes and quality of evidence, MAs reported that OMT is more effective than comparators in reducing pain and improving the functional status in acute/chronic NSLBP, CNSNP and CNCP. Due
to the small sample size, presence of conflicting results and high heterogeneity, questionable evidence existed on OMT efficacy for paediatric conditions, primary headaches and IBS. No adverse events were reported in most SRs. The methodological quality of the included SRs was rated low or critically low.
The authors concluded that based on the currently available SRs and MAs, promising evidence suggests the possible effectiveness of OMT for musculoskeletal disorders. Limited and inconclusive evidence occurs for paediatric conditions, primary headache and IBS. Further well-conducted SRs and MAs are needed to confirm and extend the efficacy and safety of OMT.
This paper raises several questions. Here a just the two that bothered me most:
- If the authors had truly wanted to evaluate the SAFETY of OMT (as they state in the abstract), they would have needed to look beyond SRs, MAs or RCTs. We know – and the authors of the overview confirm this – that clinical trials of so-called alternative medicine (SCAM) often fail to mention adverse effects. This means that, in order to obtain a more realistic picture, we need to look at case reports, case series and other observational studies. It also means that the positive message about safety generated here is most likely misleading.
- The authors (the lead author is an osteopath) might have noticed that most – if not all – of the positive SRs were published by osteopaths. Their assessments might thus have been less than objective. The authors did not include one of our SRs (because it fell outside their inclusion period). Yet, I do believe that it is one of the few reviews of OMT for musculoskeletal problems that was not done by osteopaths. Therefore, it is worth showing you its abstract here:
The objective of this systematic review was to assess the effectiveness of osteopathy as a treatment option for musculoskeletal pain. Six databases were searched from their inception to August 2010. Only randomized clinical trials (RCTs) were considered if they tested osteopathic manipulation/mobilization against any control intervention or no therapy in human with any musculoskeletal pain in any anatomical location, and if they assessed pain as an outcome measure. The selection of studies, data extraction, and validation were performed independently by two reviewers. Studies of chiropractic manipulations were excluded. Sixteen RCTs met the inclusion criteria. Their methodological quality ranged between 1 and 4 on the Jadad scale (max = 5). Five RCTs suggested that osteopathy compared to various control interventions leads to a significantly stronger reduction of musculoskeletal pain. Eleven RCTs indicated that osteopathy compared to controls generates no change in musculoskeletal pain. Collectively, these data fail to produce compelling evidence for the effectiveness of osteopathy as a treatment of musculoskeletal pain.
It was published 11 years ago. But I have so far not seen compelling evidence that would make me change our conclusion. As I state in the newspapers:
OSTEOPATHY SHOULD BE TAKEN WITH A SIZABLE PINCH OF SALT.
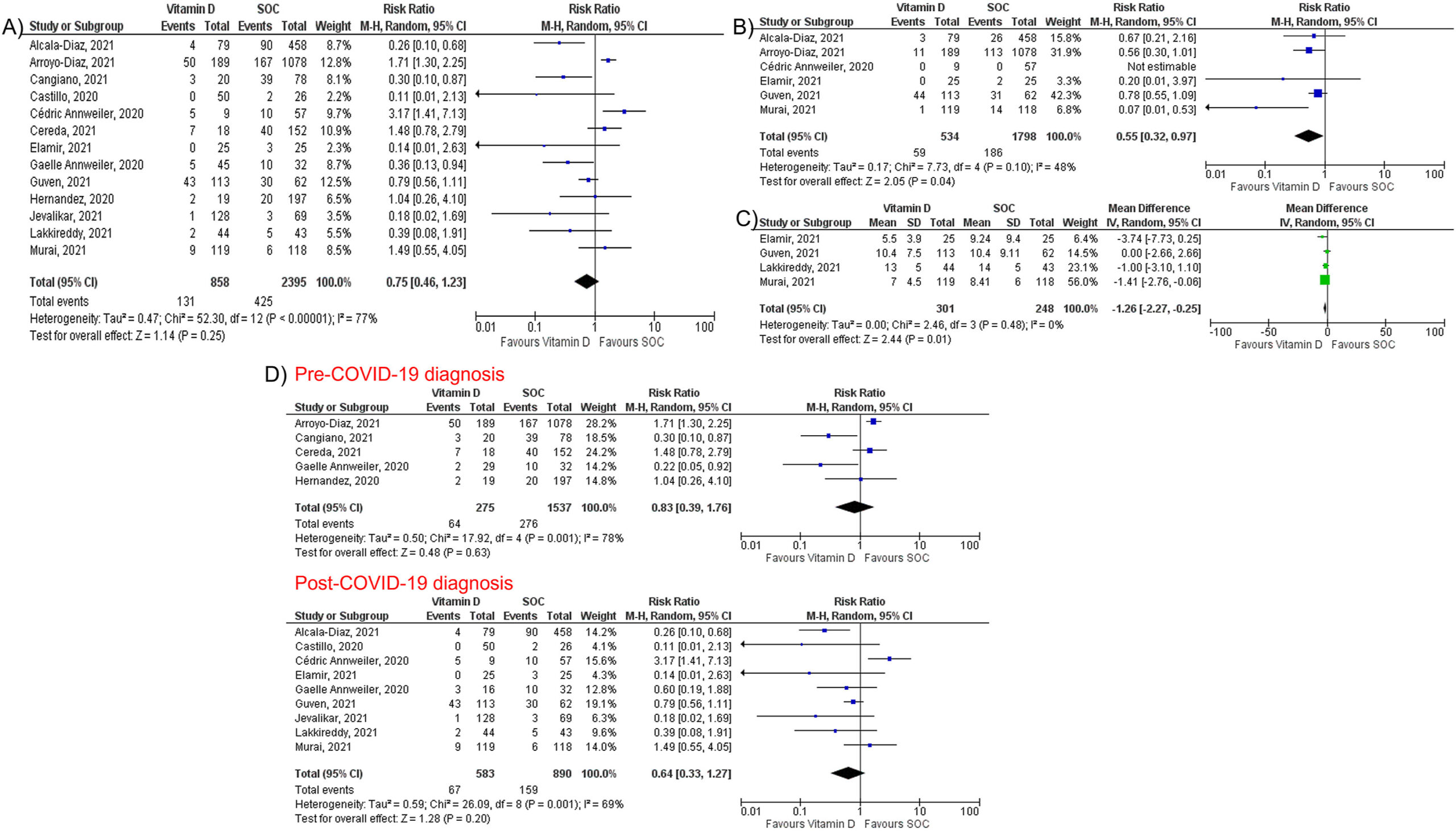
Micronutrient supplements such as vitamin D, vitamin C, and zinc have been used in managing viral illnesses. However, the clinical significance of these individual micronutrients in patients with Coronavirus disease 2019 (COVID-19) remains unclear. A team of researchers conducted this meta-analysis to provide a quantitative assessment of the clinical significance of these individual micronutrients in COVID-19.
They performed a literature search using MEDLINE, Embase, and Cochrane databases through December 5th, 2021. All individual micronutrients reported by ≥ 3 studies and compared with standard-of-care (SOC) were included. The primary outcome was mortality. The secondary outcomes were intubation rate and length of hospital stay (LOS). Pooled risk ratios (RR) and mean difference (MD) with corresponding 95% confidence intervals (CI) were calculated using the random-effects model.
The authors identified 26 studies (10 randomized controlled trials and 16 observational studies) involving 5633 COVID-19 patients that compared three individual micronutrient supplements (vitamin C, vitamin D, and zinc) with SOC.
Vitamin C
Nine studies evaluated vitamin C in 1488 patients (605 in vitamin C and 883 in SOC). Vitamin C supplementation had no significant effect on mortality (RR 1.00, 95% CI 0.62–1.62, P = 1.00), intubation rate (RR 1.77, 95% CI 0.56–5.56, P = 0.33), or LOS (MD 0.64; 95% CI -1.70, 2.99; P = 0.59).
Vitamin D
Fourteen studies assessed the impact of vitamin D on mortality among 3497 patients (927 in vitamin D and 2570 in SOC). Vitamin D did not reduce mortality (RR 0.75, 95% CI 0.49–1.17, P = 0.21) but reduced intubation rate (RR 0.55, 95% CI 0.32–0.97, P = 0.04) and LOS (MD -1.26; 95% CI -2.27, −0.25; P = 0.01). Subgroup analysis showed that vitamin D supplementation was not associated with a mortality benefit in patients receiving vitamin D pre or post COVID-19 diagnosis.
Zinc
Five studies, including 738 patients, compared zinc intake with SOC (447 in zinc and 291 in SOC). Zinc supplementation was not associated with a significant reduction of mortality (RR 0.79, 95% CI 0.60–1.03, P = 0.08).
The authors concluded that individual micronutrient supplementations, including vitamin C, vitamin D, and zinc, were not associated with a mortality benefit in COVID-19. Vitamin D may be associated with lower intubation rate and shorter LOS, but vitamin C did not reduce intubation rate or LOS. Further research is needed to validate our findings.
A multi-disciplinary research team assessed the effectiveness of interventions for acute and subacute non-specific low back pain (NS-LBP) based on pain and disability outcomes. For this purpose, they conducted a systematic review of the literature with network meta-analysis.
They included all 46 randomized clinical trials (RCTs) involving adults with NS-LBP who experienced pain for less than 6 weeks (acute) or between 6 and 12 weeks (subacute). Non-pharmacological treatments (eg, manual therapy) including acupuncture and dry needling or pharmacological treatments for improving pain and/or reducing disability considering any delivery parameters were included. The comparator had to be an inert treatment encompassing sham/placebo treatment or no treatment. The risk of bias was
- low in 9 trials (19.6%),
- unclear in 20 (43.5%),
- high in 17 (36.9%).
At immediate-term follow-up, for pain decrease, the most efficacious treatments against an inert therapy were:
- exercise (standardised mean difference (SMD) -1.40; 95% confidence interval (CI) -2.41 to -0.40),
- heat wrap (SMD -1.38; 95% CI -2.60 to -0.17),
- opioids (SMD -0.86; 95% CI -1.62 to -0.10),
- manual therapy (SMD -0.72; 95% CI -1.40 to -0.04).
- non-steroidal anti-inflammatory drugs (NSAIDs) (SMD -0.53; 95% CI -0.97 to -0.09).
Similar findings were confirmed for disability reduction in non-pharmacological and pharmacological networks, including muscle relaxants (SMD -0.24; 95% CI -0.43 to -0.04). Mild or moderate adverse events were reported in the opioids (65.7%), NSAIDs (54.3%), and steroids (46.9%) trial arms.
The authors concluded that NS-LBP should be managed with non-pharmacological treatments which seem to mitigate pain and disability at immediate-term. Among pharmacological interventions, NSAIDs and muscle relaxants appear to offer the best harm-benefit balance.
The authors point out that previous published systematic reviews on spinal manipulation, exercise, and heat wrap did overlap with theirs: exercise (eg, motor control exercise, McKenzie exercise), heat wrap, and manual therapy (eg, spinal manipulation, mobilization, trigger points or any other technique) were found to reduce pain intensity and disability in adults with acute and subacute phases of NS-LBP.
I would add (as I have done so many times before) that the best approach must be the one that has the most favorable risk/benefit balance. Since spinal manipulation is burdened with considerable harm (as discussed so many times before), exercise and heat wraps seem to be preferable. Or, to put it bluntly:
if you suffer from NS-LBP, see a physio and not osteos or chiros!
Yes, Today is ‘WORLD SLEEP DAY‘ and you are probably in bed hoping this post will put you back to sleep.
This study aimed to synthesise the best available evidence on the safety and efficacy of using moxibustion and/or acupuncture to manage cancer-related insomnia (CRI).
The PRISMA framework guided the review. Nine databases were searched from its inception to July 2020, published in English or Chinese. Randomised clinical trials (RCTs) of moxibustion and or acupuncture for the treatment of CRI were selected for inclusion. The methodological quality was assessed using the method suggested by the Cochrane collaboration. The Cochrane Review Manager was used to conduct a meta-analysis.
Fourteen RCTs met the eligibility criteria; 7 came from China. Twelve RCTs used the Pittsburgh Sleep Quality Index (PSQI) score as continuous data and a meta-analysis showed positive effects of moxibustion and or acupuncture (n = 997, mean difference (MD) = -1.84, 95% confidence interval (CI) = -2.75 to -0.94, p < 0.01). Five RCTs using continuous data and a meta-analysis in these studies also showed significant difference between two groups (n = 358, risk ratio (RR) = 0.45, 95% CI = 0.26-0.80, I 2 = 39%).
The authors concluded that the meta-analyses demonstrated that moxibustion and or acupuncture showed a positive effect in managing CRI. Such modalities could be considered an add-on option in the current CRI management regimen.
Even at the risk of endangering your sleep, I disagree with this conclusion. Here are some of my reasons:
- Chinese acupuncture trials invariably are positive which means they are as reliable as a 4£ note.
- Most trials were of poor methodological quality.
- Only one made an attempt to control for placebo effects.
- Many followed the A+B versus B design which invariably produces (false-) positive results.
- Only 4 out of 14 studies mentioned adverse events which means that 10 violated research ethics.
Sorry to have disturbed your sleep!
This review assessed the magnitude of reporting bias in trials assessing homeopathic treatments and its impact on evidence syntheses.
A cross-sectional study and meta-analysis. Two persons independently searched Clinicaltrials.gov, the EU Clinical Trials Register and the International Clinical Trials Registry Platform up to April 2019 to identify registered homeopathy trials. To determine whether registered trials were published and to detect published but unregistered trials, two persons independently searched PubMed, Allied and Complementary Medicine Database, Embase and Google Scholar up to April 2021. For meta-analyses, the authors used random effects models to determine the impact of unregistered studies on meta-analytic results.
The investigators reported the proportion of registered but unpublished trials and the proportion of published but unregistered trials. They also assessed whether primary outcomes were consistent between registration and publication
Since 2002, almost 38% of registered homeopathy trials have remained unpublished, and 53% of published randomised controlled trials (RCTs) have not been registered. Retrospective registration was more common than prospective registration. Furthermore, 25% of primary outcomes were altered or changed compared with the registry. Although we could detect a statistically significant trend toward an increase of registrations of homeopathy trials (p=0.001), almost 30% of RCTs published during the past 5 years had not been registered.
A meta-analysis stratified by registration status of RCTs revealed substantially larger treatment effects of unregistered RCTs (SMD: −0.53, 95% CI −0.87 to −0.20) than registered RCTs (SMD: −0.14, 95% CI −0.35 to 0.07).
The authors concluded that registration of published trials was infrequent, many registered trials were not published and primary outcomes were often altered or changed. This likely affects the validity of the body of evidence of homeopathic literature and may overestimate the true treatment effect of homeopathic remedies.
An obvious investigation to do (why did I not have this idea?)!
And a finding that will surprise few (except fans of homeopathy who will, of course, dispute it).
The authors also mention that reporting biases are likely to have a substantial impact on the estimated treatment effect of homeopathy. Using data from a highly cited meta-analysis of homeopathy RCTs, our example showed that unregistered trials yielded substantially larger treatment effects than registered trials. They also caution that, because of the reporting biases identified in their analysis, effect estimates of meta-analyses of homeopathy trials might substantially overestimate the true treatment effect of homeopathic remedies and need to be interpreted cautiously.
In other words, the few reviews suggesting that homeopathy works beyond placebo (and are thus celebrated by homeopaths) are most likely false-positive. And the many reviews showing that homeopathy does not work would demonstrate this fact even clearer if the reporting bias had been accounted for.
Or, to put it bluntly: