medical ethics
Mind-body interventions (MBIs) are one of the top ten so-called alternative medicine (SCAM) approaches utilized in pediatrics, but there is limited knowledge on associated adverse events (AE). The objective of this review was to systematically review AEs reported in association with MBIs in children.
Electronic databases MEDLINE, Embase, CINAHL, CDSR, and CCRCT were searched from inception to August 2018. The authors included primary studies on participants ≤ 21 years of age that used an MBI. Experimental studies were assessed for whether AEs were reported on or not, and all other study designs were included only if they reported an AE.
A total of 441 were included as primary pediatric MBI studies. Of these, 377 (85.5%) did not explicitly report the presence/absence of AEs or a safety assessment. In total, there were 64 included studies: 43 experimental studies reported that no AE occurred, and 21 studies reported AEs. A total of 37 AEs were found, of which the most serious were grade 3. Most of the studies reporting AEs did not report on severity (81.0%) or duration of AEs (52.4%).
The authors concluded that MBIs are popularly used in children; however associated harms are often not reported and lack important information for meaningful assessment.
SCAM is far too often considered to be risk-free. This phenomenon is particularly stark if the SCAM in question does not involve physical or pharmacological treatments. Thus MBIs are seen and often waved through as especially safe. Consequently, many researchers do not even bother to monitor AEs in their clinical trials. This might be understandable, but it is nevertheless a violation of research ethics.
This new review is important in that it highlights these issues. It is high time that we stop giving researchers in SCAM the benefit of the doubt. They may or may not make honest mistakes when not reporting AEs. In any case, it is clear that they are not properly trained and supervised. All too often, we still see clinical trials run by amateurs who have little idea of methodology and even less of ethics. The harm this phenomenon does is difficult to quantify, but I fear it is huge.
“Time to say good-bye? Homeopathy, skeptics and thoughts on how to proceed” is the title of an article by two Swiss homeopaths which is almost touchingly naive. Here is its abstract:
Although homeopathy is frequently used by many health professionals, there are ongoing debates concerning its effectiveness. Currently no unifying explanation how homeopathy works exists. Homeopaths are frequently challenged by skeptics, and in public opinion, the swan song for homeopathy is frequently sung.
Content: Regarding the efficacy of homeopathy, several well-designed RCTs, observational studies, case studies, and case reports, have been published, demonstrating its clinical efficacy. Regarding its mode of action, the discovery of the working principle of homeopathy would be a major advance towards a thorough scientific recognition of homeopathy. Basic research has already discovered some milestones, e.g., significant and reproducible effects of homeopathic preparations in plants.
Summary: To overcome the distrust of skeptics and public opinion, the support of basic research is indispensable. Second, homeopaths should continue to design prospective randomized clinical studies in order to create robust clinical evidence for the efficacy of homeopathy. Third, they should continue to publish their treatment outcomes, as these publications document clinical effectiveness beyond doubts about its mode of action.
Outlook: These measures will not only support homeopaths in continuing their clinical work, but may lead to a better recognition of this treatment in both the scientific world and the public.
To this, I might add the following comments:
- “ongoing debates concerning its effectiveness”: this debate has been ongoing for 200 years but it has now come to a conclusion, namely that homeopathy is a placebo therapy.
- “no unifying explanation how homeopathy works exists”: we do know, however, that the laws of nature, as we understand them today, must be wrong if homeopathy did work.
- “Homeopaths are frequently challenged by skeptics”: the main challenges currently come not from skeptics but from health experts who rightly insist on sound evidence.
- “several well-designed RCTs, observational studies, case studies, and case reports, have been published, demonstrating its clinical efficacy”: arguably, this might be correct but misses the crucial point that the totality of the reliable evidence fails to show that homeopathy is efficacious for any condition of humans or animals.
- “the discovery of the working principle of homeopathy would be a major advance”: yes, so much so that it would require rewriting whole sections of the textbooks of physics and chemistry.
- “Basic research has already discovered some milestones”: these ‘milestones’ are so imposing that nobody outside the realm of homeopathy has ever recognized them.
- “the support of basic research is indispensable”: not so much indispensable as non-existent, I would say.
- “design prospective randomized clinical studies in order to create robust clinical evidence for the efficacy of homeopathy”: homeopaths believe research to be a tool for creating evidence that supports their creed; I have often tried to remind them that it is a tool for testing hypotheses – to no avail, it seems.
- “publish their treatment outcomes, as these publications document clinical effectiveness”: I have also often tried to explain to them that treatment outcomes can be due to many factors other than the specific effect of the applied therapy – again to no avail.
- “These measures will not only support homeopaths in continuing their clinical work, but may lead to a better recognition of this treatment in both the scientific world and the public”: these measures, if applied rigorously, will merely confirm what we already know, namely that homeopathy does not work beyond placebo.
The UK ‘Advertising Standards Authority‘ (ASA) received a complaint about an advertisement that stated:
“Homeopathy is used throughout the world to keep healthy … People in the UK have been using it to successfully help with migraine, anxiety, chronic pain, woman’s [sic] health issues, depression, eczema, chronic fatigue, asthma, IBS, rheumatoid arthritis, and many other conditions”.
The ‘Good Thinking Society‘ had challenged whether:
- the ad discouraged essential treatment for conditions for which medical supervision should be sought, namely migraines, chronic pain, women’s health issues, depression, asthma, rheumatoid arthritis; and
- the claim “People in the UK have been using [homeopathy] to successfully help with anxiety, chronic pain … eczema, chronic fatigue syndrome … IBS” was misleading and could be substantiated.
The response of the ASA has just been published. Here are the key excerpts from the ASA’s assessment:
1. Upheld
The CAP Code required that marketers must not discourage essential treatment for conditions for which medical supervision should be sought. For example, they must not offer specific advice on, diagnosis or treatment for such conditions unless that advice, diagnosis or treatment was conducted under the supervision of a suitably qualified medical professional. Among other conditions, the ad referred to “migraines”, “chronic pain”, “woman’s [sic] health issues”, “depression”, “asthma”, and “rheumatoid arthritis”, which we considered were conditions for which medical supervision should be sought, and therefore advice, diagnosis or treatment must be conducted under the supervision of a suitably qualified medical professional. We noted that the practice was run by a GMC-registered GP, who we considered was a suitably qualified health professional. However, the individual homeopaths were not registered and did not hold the same qualifications. Therefore, Homeopathy UK had not shown that all treatment and diagnoses conducted at the practice would be conducted under the supervision of a suitably qualified medical professional. Because Homeopathy UK had not supplied evidence that treatment would always be carried out by a suitably qualified health professional, and because reference to the conditions listed in the ad could discourage consumers from seeking essential treatment under the supervision of a suitably qualified health professional, we concluded that the ad had breached the Code.
On that point the ad breached CAP Code (Edition 12) rule 12.2 (Medicines, medical devices, health-related products and beauty products).
2. Upheld
We considered that consumers would understand the claim “People in the UK have been using [homeopathy] to successfully help with anxiety, chronic pain … eczema, chronic fatigue syndrome … IBS” to mean that homeopathy could be used to successfully treat those conditions … when we reviewed the evidence provided by Homeopathy UK, we considered that the studies provided did not meet the standard of evidence we required for the types of claims being made, both in terms of adequacy and relevance…
On that point the ad breached CAP Code (Edition) rules 3.1 (Misleading advertising), 3.7 (Substantiation) and 12.1 (Medicines, medical devices, health-related products and beauty products).
Action
The ad must not appear again in the form complained about. We told Homeopathy UK to ensure their future marketing communications did not to refer to conditions for which advice should be sought from suitably qualified health professionals. We also told them to ensure they did not make claims for homeopathy unless they were supported with robust evidence.
_____________________________
Am I reading this correctly?
The ASA seems to be saying that homeopaths are not suitably qualified health professionals and, as no therapeutic claims are supported by robust evidence, that claims for homeopathy are improper.
Qigong is a branch of Traditional Chinese Medicine using meditation, exercise, deep breathing, and other techniques with a view of strengthening the assumed life force ‘qi’ and thus improving health and prolong life. There are several distinct forms of qigong which can be categorized into two main groups, internal qigong, and external qigong. Internal qigong refers to a physical and mental training method for the cultivation of oneself to achieve optimal health in both mind and body. Internal qigong is not dissimilar to tai chi but it also employs the coordination of different breathing patterns and meditation. External qigong refers to a treatment where qigong practitioners direct their qi-energy to the patient with the intention to clear qi-blockages or balance the flow of qi within that patient. According to Taoist and Buddhist beliefs, qigong allows access to higher realms of awareness. The assumptions of qigong are not scientifically plausible and its clinical effectiveness remains unproven.
The aim of this study was to investigate the effects of internal Qigong for the management of a symptom cluster comprising fatigue, dyspnea, and anxiety in patients with lung cancer.
A total of 156 lung cancer patients participated in this trial, and they were randomized to a Qigong group (6 weeks of intervention) or a waitlist control group receiving usual care. A professional coach with 12 years of experience in teaching Qigong was employed to guide the participants’ training. The training protocol was developed according to the “Qigong Standard” enacted by the Chulalongkorn University, Thailand. The training involved a series of simple, repeated practices including body posture/movement, breathing practice, and meditation performed in synchrony. It mainly consisted of gentle movements designed to bring about a deep state of relaxation and included 7 postures. The symptom cluster was assessed at baseline, at the end of treatment (primary outcome), and at 12 weeks, alongside measures of cough and quality of life (QOL).
The results showed no significant interaction effect between group and time for the symptom cluster, the primary outcome measure of this study, overall and for fatigue and anxiety. However, a significant trend towards improvement was observed on fatigue (P = .004), dyspnea (P = .002), and anxiety (P = .049) in the Qigong group from baseline assessment to the end of intervention at the 6th week (within-group changes). Improvements in dyspnea and in the secondary outcomes of cough, global health status, functional well-being and QOL symptom scales were statistically significant between the 2 groups (P = .001, .014, .021, .001, and .002, respectively).
The authors concluded that Qigong did not alleviate the symptom cluster experience. Nevertheless, this intervention was effective in reducing dyspnea and cough, and improving QOL. More than 6 weeks were needed, however, for detecting the effect of Qigong on improving dyspnea. Furthermore, men benefited more than women. It may not be beneficial to use Qigong to manage the symptom cluster consisting of fatigue, dyspnea, and anxiety, but it may be effective in managing respiratory symptoms (secondary outcomes needing further verification in future research). Future studies targeting symptom clusters should ensure the appropriateness of the combination of symptoms.
I am getting very tired of negative trials getting published as (almost) positive ones. The primary outcome measure of this study did not yield a positive result. The fact that some other endpoints suggested a positive might provide an impetus for further study but does not demonstrate Qigong to be effective. I know the first author of this study is a fan of so-called alternative medicine (SCAM), but this should not stop him from doing proper science.
The usage of so-called alternative medicine (SCAM) in pediatric settings has been high for some time. However, the risks of pediatric SCAM use remain under-investigated. Almost 20 years ago, I published this systematic review:
Unconventional therapies have become popular in paediatric and adolescent populations. It is therefore important to define their risks. The aim of this systematic review was to summarise the recent evidence. Computerised literature searches were carried out in five databases to identify all recent reports of adverse events associated with unconventional therapies in children. The reports were summarised in narrative and tabular form. The results show that numerous case reports and several case series have been published since 1990. Investigations of a more systematic nature are, however, rare. Most of the adverse events were associated with herbal medications. Inadequately regulated herbal medicines may contain toxic plant material, be contaminated with heavy metals, or be adulterated with synthetic drugs. The adverse events included bradycardia, brain damage, cardiogenic shock, diabetic coma, encephalopathy, heart rupture, intravascular haemolysis, liver failure, respiratory failure, toxic hepatitis and death. A high degree of uncertainty regarding a causal relationship between therapy and adverse event was frequently noted. The size of the problem and its importance relative to the well-documented risks of conventional treatments are presently unknown. Several unconventional therapies may constitute a risk to the health of children and adolescents. At present, it is impossible to provide reliable incidence figures. It seems important to be vigilant and investigate this area more systematically.
Nothing much has happened since in terms of systematic investigation. But now, a 3-year survey was carried out at the Dutch Pediatric Surveillance Unit. Pediatricians were asked to register cases of adverse events associated with pediatric SCAM usage.
In 3 years, 32 unique adverse events were registered. Twenty-two of these adverse events were indirect and not related to the specific SCAM therapy but due to delaying, changing, or stopping of regular treatment, a deficient or very restrictive diet, or an incorrect diagnosis by a SCAM therapist. These events were associated with many different SCAM therapies.
Nine events were deemed direct adverse events like bodily harm or toxicity and one-third of them occurred in infants. Only supplements, manual therapies, and (Chinese) herbs were involved in these nine events. In one case, there was a risk of a serious adverse event but the harm had not yet occurred.
The authors concluded that relatively few cases of adverse events associated with pediatric SCAM usage were found, mostly due to delaying or stopping conventional treatment. Nevertheless, parents, pediatricians, and SCAM providers should be vigilant for both direct and indirect adverse events in children using SCAM, especially in infants.
The number of cases seems small indeed, but there may be many further adverse events that went unreported. Here are 4 of the documented cases of severe and life-threatening consequences:
- An 8-year-old child with autoimmune hypothyroidism had his prescribed replaced with an ineffective herbal remedy.
- A 14-year-old child developed septic shock with multiple organ failure after receiving homeopathy for acute appendicitis.
- A 14-year-old child needed colectomy after ineffective naturopathic treatments for colitis.
- A 5-year-old developed secondary adrenal insufficiency after his eczema was treated with Chinese herbal remedies adulterated with large doses of corticosteroids.
In view of the risks – even if small – I suggest that, in pediatric settings, we employ only those SCAMs that are supported by solid evidence. And those are very few indeed.
Many people believe that homeopathy is essentially plant-based – but they are mistaken! Homeopathic remedies can be made from anything: Berlin wall, X-ray, pus, excrement, dental plaque, mobile phone rays, poisons … anything you can possibly think of. So, why not from vaccines?
This is exactly what a pharmacist specialized in homeopathy thought.
It has been reported that the ‘Schloss-Apotheke’ in Koblenz, Germany offered for sale a homeopathic remedy made from the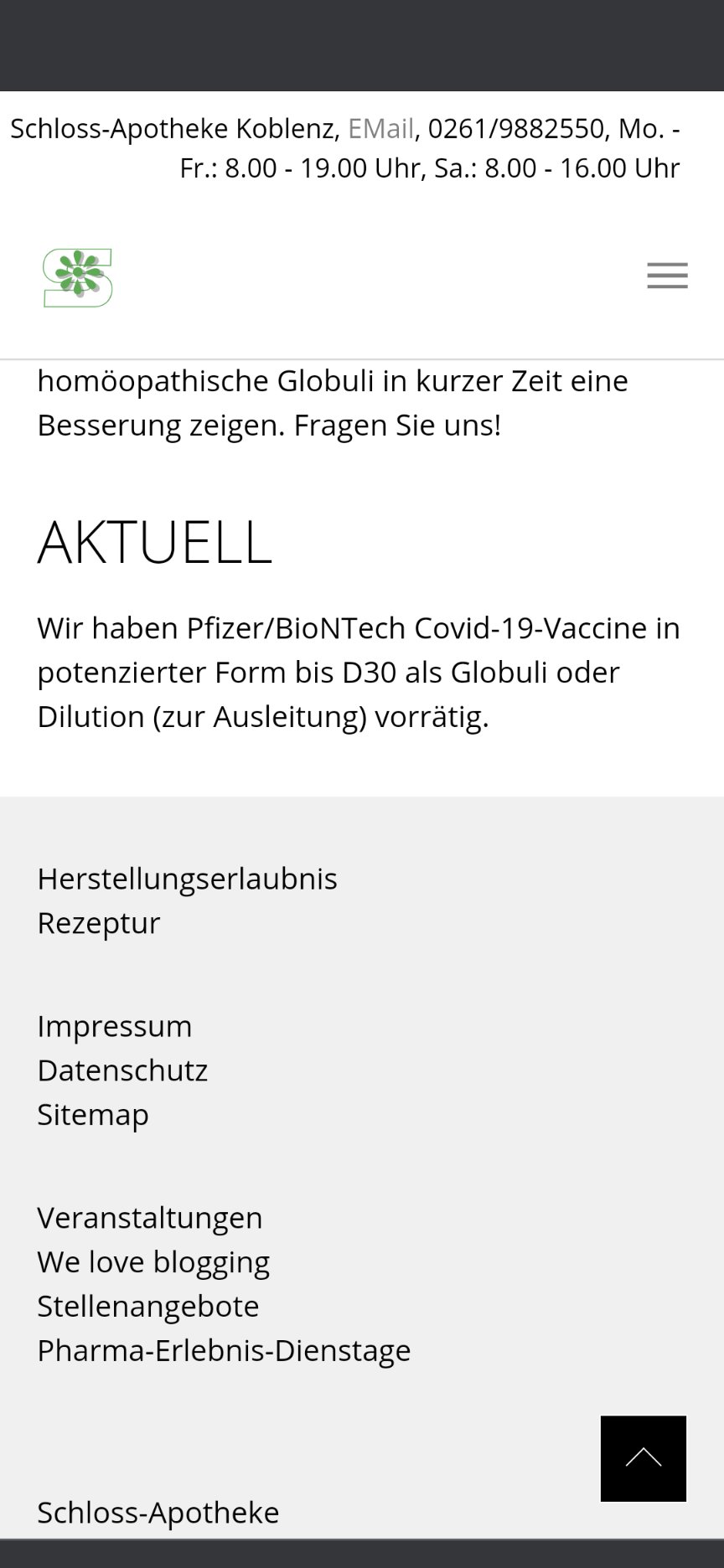 Pfizer vaccine. This has since prompted not only the Chamber of Pharmacists but also the Paul Ehrlich Institute and Pfizer to issue statements. On Friday (30/4/2021) morning, the pharmacy had advertised homeopathic remedies based on the Pfizer/Biontech vaccine. The Westphalia-Lippe Chamber of Pharmacists then issued an explicit warning against it. “We are stunned by this,” said a spokesman. The offer has since disappeared from the pharmacy’s website.
Pfizer vaccine. This has since prompted not only the Chamber of Pharmacists but also the Paul Ehrlich Institute and Pfizer to issue statements. On Friday (30/4/2021) morning, the pharmacy had advertised homeopathic remedies based on the Pfizer/Biontech vaccine. The Westphalia-Lippe Chamber of Pharmacists then issued an explicit warning against it. “We are stunned by this,” said a spokesman. The offer has since disappeared from the pharmacy’s website.
On Friday afternoon, the manufacturer of the original vaccine also intervened. The Paul Ehrlich Institute released a statement making it clear that a vaccine is only safe “if it is administered in accordance with the marketing authorization.”
The Schloss-Apotheke had advertised the product in question with the following words:
“We have Pfizer/BioNTech Covid-19-Vaccine in potentized form up to D30 as globules or dilution (for discharge) in stock.”
The chamber of pharmacists countered with a warming under the heading “Facts instead of Fake News” on Facebook and Instagram:
“Whatever they might contain: These remedies are no effective protection against Covid-19.”
Pharmacy manager, Annette Eichele, of the Schloss-Apotheke claimed she had not sold homeopathic Corona vaccines and stressed that effective vaccines of this kind do not exist. According to Eichele, only an additional “mini drop” of the original Biontech vaccine had been used and “highly potentized” and prepared homeopathically. According to Eichele, Corona vaccinations that had already been administered were thus to have a “better and more correct effect with this supplementary product, possibly without causing side effects … but this is not scientifically proven”. The homeopathic product had been produced only on customer request and had been sold less than a dozen times in the past weeks. Ten grams of the remedy were sold for about 15 Euros. On Twitter, Eichele stated: „Wir haben nichts Böses getan, wir wollten nur Menschen helfen!“ (We have done nothing evil, we only wanted to help people). I am reminded yet again of Bert Brecht who observed:
“The opposite of good is not evil but good intentions”.
Thread embedding acupuncture therapy (TEAT) involves the insertion of thread at specific points on the body surface. The claim is that TEAT provides a sustained stimulation of acupoints and is therefore superior to needle acupuncture. Initially, TEAT was used in China to treat obesity, today it is employed to treat many conditions, including musculoskeletal conditions such as ankle sprain, shoulder pain, lumbar intervertebral disc herniation, and plantar fasciitis. Its effectiveness is, however, doubtful and so is its safety.
This review evaluated the safety of thread embedding acupuncture therapy (TEAT) and discuss the prevention and treatment of some adverse events (AEs).
Databases, including China National Knowledge Infrastructure (CNKI), CBMdisc, Wanfang, VIP databases and PubMed, MEDLINE, EMBASE, and Web of Science, were searched from their inception to January 2020. Included were randomized controlled trials (RCTs) and case reports in which AEs with TEAT were reported. Cochrane Collaboration’s tool and RevMan V.5.3.3 software were used to evaluate the quality of the studies.
A total of 61 articles (45 RCTs and 16 case reports) with a total of 620 cases of AEs were included in this review. These studies were published in two countries: China and South Korea. Twenty-eight kinds of AEs were noted. The most common AEs were induration, bleeding and ecchymosis, redness and swelling, fever, and pain. They accounted for 75.35% of all AEs. Most AEs were mild.; The rarest AEs were epilepsy, irregular menstruation, skin ulcer, thread malabsorption, and fat liquefaction, with 1 case each. Not all of them had a clear causal relationship with TEAT. Most of the AEs were local reactions and systemic reactions accounted for only 1.27%. Although the included studies showed that AEs were very commonly encountered (11.09%), only 5 cases of severe AEs reported from 2013 to 2017 (0.1%) by using catgut thread, which is rarely employed nowadays with new absorbable surgical suture being more popular. All of the patients with severe AEs were recovered after symptomatic treatment with no sequelae.
The authors concluded that the evidence showed that TEAT is a relatively safe and convenient therapy especially since application of new absorbable surgical suture. Improving practitioner skills, regulating operations, and paying attention to the patients’ conditions may reduce the incidence of AEs and improve safety of TEAT.
TEAT was initially used in China only but recently it has become popular elsewhere as well. Therefore the question about its risks has become relevant. The present paper is interesting in that it demonstrates that AEs do occur with some regularity. The authors’ conclusion that TEAT is “relatively safe” is, however, not justified because:
- the total sample size was not large enough for a generalizable conclusion;
- only RCTs and case reports were included, whereas case series and case-control studies (which would provide more relevant data) were excluded or might not even exist;
- RCTs of acupuncture often fail to mention or under-report AEs;
- acupuncture papers from China are notoriously unreliable.
So, all we can conclude from the evidence presented here is that AEs after TEAT do occur and do not seem to be all that rare. As the efficacy of TEAT has not been shown beyond doubt, this must inevitably lead to the conclusion that the risk-benefit balance of TEAT is not positive. In turn, that means that TEAT cannot be recommended as a treatment for any condition.
If I search on Amazon for books on ALTERNATIVE MEDICINE, I get between 50 000 and 60 000 volumes, depending on what country I am in. As a very rough guess, I estimate that about 95% of them are rubbish – not just useless, but dangerous. Because of this lamentable situation, I am delighted each time I come across one that belongs to the other 5%. And in recent years, there have been quite a few.
No, I am not about to advertise another book of mine; I am about to commend to you
Brad McKay’s FAKE MEDICINE
(I don’t often publish book reviews here, but I feel that might change.)
The new book is advertised with the following words: “Dr Brad McKay, Australian GP and science communicator, has seen the rise of misinformation permeate our lives and watched as many of us have turned away from health experts. Too often, we place our trust in online influencers, celebrities and Dr Google when it comes to making important health decisions. Fake Medicine explores the potential dangers of wellness warriors, anti-vaxxers, fad diets, dodgy supplements, alternative practitioners and conspiracy theories. This book is an essential tool for debunking pseudoscience and protecting you and your loved ones from the health scams that surround us. Protect your mind, body and wallet by fighting fake medicine.”
They describe the book fairly accurately. McKay covers all of these subjects with considerable skill. His book is well-suited for people who are newcomers to the critical assessment of so-called alternative medicine (SCAM); the text is free of jargon or long-winded technical explanations. Instead, the author mostly tells stories of events that actually happened to him. Several happened to him in a most personal fashion, as his experience as a young gay Australian with a form of conversion therapy administered by religious zealots, or the story where he took some highly dodgy Chinese medicine to boost his energy levels.
Lots of people have done similarly foolish things, I know, but not many are doctors and can thus put their experience in a medical perspective. And crucially, not many can write as entertaining as Brad. I had thought I knew most of what there is to know about SCAM, but I did learn something new from Brad: did you know what GISH GALLOP is? Well, I didn’t!
One of the most useful parts of the book is chapter 16 where Brad tells everyone what they can and should do to stop fake medicine in its tracks. And he does mean EVERYONE! – not just skeptics or sceptics or activists or scientists. This book is truly written for laypeople. If you don’t belong to this group, buy it anyway and give it to someone from your circle of friends who needs it. I am sure there are a few.
Many chiropractors seem to view the present pandemic as a business opportunity and make no end of false claims to attract customers. This has now been outlawed in the US. Medscape reported that a US district court will decide whether a chiropractor who is charged with 10 counts of making false marketing claims related to COVID-19 will be the first person convicted under a new federal law.
On his website, chiropractor ‘Dr.’ Eric Neptune advertises his services as follows:
Have you ever been told by your medical doctor that you or a member of your family had a specific disease, syndrome, or sickness? Did your doctor then recommend a drug or surgery to fix the issue, or tell you that you would have to live with it for the rest of your life? If so, you are not alone!
Nepute Wellness Center is unlike any medical clinic you may have been to. The clinic team is focused on finding and fixing the CAUSE of your problem vs. seeking out and treating only the SYMPTOMS. Nepute Wellness Center is equipped with state-of-the-art diagnostic equipment and testing, as well as medical doctors, nurses, and chiropractors who have been uniquely trained to treat your whole body, regardless of age, and return your body to a healthy balance so that it can heal itself the way God intended.
If you are tired of trying to treat your symptoms using prescription and over-the-counter pills, or even considering surgery, then Nepute Wellness Center may be right for you! Or like many, you want to be proactive with your health and prevent sickness and disease before you begin to suffer any symptoms, allowing you to live the full life you deserve, then make Nepute Wellness Center your partner in health!
Already over a year ago, Eric Nepute, the owner of Quickwork, based in St. Louis, Missouri, managed to make headlines. He had recorded a video that racked up more than 21 million views and suggested that drinking tonic water would prevent COVID-19 infections. Now, Mr. Neptune is the first person charged by the Federal Trade Commission (FTC) under the new COVID- 19 Consumer Protection Act. His company which has several locations in St. Louis County advertised its vitamin D and zinc products on social media and the internet as drugs that could treat or prevent COVID-19 claiming that their products are “more effective than the available COVID-19 vaccines”.
The FTC warned Nepute’s company in May 2020 about making unsubstantiated claims for other products regarding efficacy against COVID-19 and advised him to immediately stop making claims that were not supported by scientific evidence. However, Nepute seemed undeterred.
The FTC is seeking to fine Nepute and Quickwork up to US$43,792 for each violation of the COVID-19 Consumer Protection Act. In addition, the FTC seeks to bar the company from making health claims unless they are true and can be substantiated by scientific evidence.
Through his attorney, Neptune told the local NBC TV news affiliate, “I feel that I have not done anything wrong. I encourage everyone to live a healthy lifestyle during this unprecedented time. My attorneys are reviewing the complaint and I have no further comments at this time.”
In 2008, the British Chiropractic Association sued Simon Singh because he disclosed that they were promoting chiropractic for infant colic. The BCA lost the case, plenty of money, and all its reputation. Ever since the issue is a very sore point for chiropractic pride. The data show that Simon was quite correct in stating that they are happily promoting bogus treatments without a jot of evidence. Here for instance is my systematic review:
Some chiropractors claim that spinal manipulation is an effective treatment for infant colic. This systematic review was aimed at evaluating the evidence for this claim. Four databases were searched and three randomised clinical trials met all the inclusion criteria. The totality of this evidence fails to demonstrate the effectiveness of this treatment. It is concluded that the above claim is not based on convincing data from rigorous clinical trials.
But chiropractors steadfastly refuse to accept defeat and keep on trying to find positive results. Now Danish chiropractors have made another attempt.
The purpose of this study is to evaluate the effect of chiropractic care on infantile colic. This multicenter, single-blind randomized controlled trial was conducted in four Danish chiropractic clinics, 2015–2019. Information was distributed in the maternity wards and by maternal and child health nurses. Children aged 2–14 weeks with unexplained excessive crying were recruited through home visits and randomized (1:1) to either chiropractic care or control group. Both groups attended the chiropractic clinic twice a week for 2 weeks. The intervention group received chiropractic care, while the control group was not treated. The parents were not present in the treatment room and unaware of their child’s allocation.
The primary outcome was change in daily hours of crying before and after treatment. Secondary outcomes were changes in hours of sleep, hours being awake and content, gastrointestinal symptoms, colic status and satisfaction. All outcomes were based on parental diaries and a final questionnaire.
Of 200 recruited children, 185 completed the trial (treatment group n = 96; control group n = 89). Duration of crying in the treatment group was reduced by 1.5 h compared with 1 h in the control group (mean difference − 0.6, 95% CI − 1.1 to − 0.1; P = 0.026), but when adjusted for baseline hours of crying, age, and chiropractic clinic, the difference was not significant (P = 0.066). The proportion obtaining a clinically important reduction of 1 h of crying was 63% in the treatment group and 47% in the control group (p = 0.037), and NNT was 6.5. We found no effect on any of the secondary outcomes.

The authors concluded that excessive crying was reduced by half an hour in favor of the group receiving chiropractic care compared with the control group, but not at a statistically significant level after adjustments. From a clinical perspective, the mean difference between the groups was small, but there were large individual differences, which emphasizes the need to investigate if subgroups of children, e.g. those with musculoskeletal problems, benefit more than others from chiropractic care.
This seems to be a rigorous trial. However, I don’t quite understand why the authors even mention that, before adjusting, the results seemed to favor chiropractic. This only makes a squarely negative study look positive! Why would anyone want to do that? Could this perhaps hint at a reason for this odd behavior? “The study was primarily funded by the Foundation for Chiropractic Research and Postgraduate Education.”
