integrative medicine
What motivates a doctor to work as an integrative medical practitioner? This is a question I asked myself often. Despite trying to find answers through several methods, I was not very successful. The question does not seem well-researched at all. Here is what I found so far:
Our own 1996 survey of GPs participating in a course at Exeter that was aimed at familiarizing them with so-called alternative medicine (SCAM) found that the main perceived advantage of SCAM, apart from the potential intrinsic value of the techniques themselves, was the time available for establishing a good therapeutic relationship with the patient.
A UK survey from 2001 suggested that doctors are motivated by issues ranging from feeling a responsibility to respond to their patients’ interests and needs to developing “another string to their bow.” Some are attracted to its study in its own right, others by a wish to focus some of their energy away from conventional medical practice, which they may find stressful and unfulfilling. Doctors studying complementary and alternative medicine often call on different personality traits and report a variety of positive benefits from training, including welcoming the opportunity to engage their feelings, trust their intuition, and enjoy therapeutic touch. Comments from attendees at one homoeopathic course were “I started to enjoy seeing patients again,” “Training had improved my conventional history taking,” and “Having another approach made treating heart-sink patients easier.”
A German focus group in 2008 with 17 GP suggested that scientific evidence and patient preference were the main criteria used by these doctors in deciding whether to apply a SCAM or not.
An interview study published in 2011 with Australian doctors provided some details. The researchers invited 43 doctors to participate. Twenty-three agreed to take part in either a face-to-face (n = 7) or telephone (n = 16) interviews. Here is the passage entitled “Motivations to work as an integrative medical practitioner” from their paper:
‘Family of origin health beliefs and practices’ were an important influence on the doctors’ philosophical approach and their decisions to work as an integrative medical practitioner.
…When I grew up it was not uncommon that I would see my aunties and uncles preparing all sorts of things. My auntie laying me on her lap and putting breast milk in my ear and drinking chamomile tea for a sore belly…there was lots of things that influenced me. (Female, 23 years in practice)
…There is a long tradition in [country of origin] of using a herbalist. I heard things from my mum and my grandma and those ideas were there. (Male, 16 years in practice)
The ‘personal or close family illness experiences’ reported by doctors were also influential in motivating them to practice integrative medicine. These experiences included non-conventional approaches to health and illness and the use of CAM as treatment modalities.
…I had my own illness – depression and a very bad back. I’d been on medication for years and I got sick of taking medications and I was given a prognosis of chronic illness with relapses and I really didn’t like it. So I started to look elsewhere and that took me in to the world of mind-body medicine. (Female, 24 years in practice)
Other doctors cited ‘professional experiences’, often early in their careers, of different theoretical approaches to medicine as being a powerful stimulus to practice integrative medicine. These included being inspired by a medical lecturer, an interesting, usually non-conventional experience during a placement as a medical student, and professional experiences of CAM modalities during their residency or early medical career.
…We had this subject Medical Studies 3, where there was a discussion of the French fur trapper in the Yukon who had shot himself in the stomach and the local doctor who was experimenting with various emotional states. There was just that sort of moment, of thinking, that’s the sort of area that I want to work in. (Male, 26 years in practice)
…I found myself doing a clinical attachment at a hospital in Switzerland that used integrated medicine, they had a course and I thought I’ll just do this for interest. I came in contact with an Indian person who did homeopathy and I found his stories quite interesting. (Male, 22 years in practice)
‘Dissatisfaction with the conventional approach to medicine’, which was perceived to be too illness focused or commercialized, was also cited by some doctors as a precursor to adopting an integrative approach to medical practice.
…More and more I’m realising that medicine is a personalised thing. We need to learn the art of treating people individually rather than en masse as a sick lung or a sick toe or a sick whatever because it doesn’t work like that. (Male, 22 years in practice)
…Medicine was hijacked by the market; i.e.: big pharmaceutical companies. And they have seduced the government, the colleges, the universities, general practice, everybody. GPs, in my opinion, have been deskilled. (Female, 19 years in practice).
An Australian survey from 2021 suggested that GPs were attracted to SCAM because they thought it to be relatively safe and effective, offering additional, holistic benefits to patients.
___________________________
Collectively these investigations suggest that doctors’ motivation to work as integrated medical practitioners vary greatly. They seem to include:
- positive evidence for SCAM’s safety and efficacy,
- having the time to establish a good therapeutic relationship,
- wanting to use all therapeutic options,
- dissatisfaction with conventional medicine,
- patient preferences,
- wanting to practice in a more human and holistic way,
- personal and professional experiences.
But surely, there are other factors as well (from my personal experience in dealing with doctors of integrative medicine, I could list a few that are less than flattering). In any case, I would be most interested to hear your thought and read more published evidence that you might know about.
This systematic review and meta-analysis of clinical trials were performed to summarize the evidence of the effects of Urtica dioica (UD) consumption on metabolic profiles in patients with type 2 diabetes mellitus (T2DM).
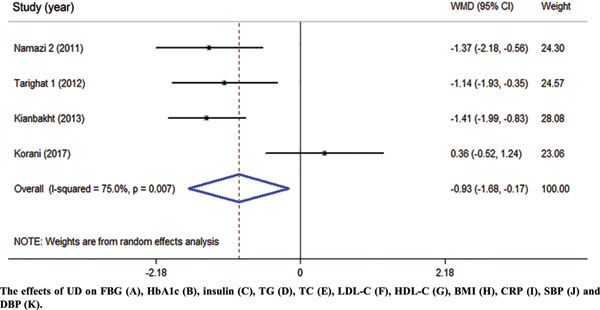
Eligible studies were retrieved from searches of PubMed, Embase, Scopus, Web of Science, Cochrane Library, and Google Scholar databases until December 2019. Cochran (Q) and I-square statistics were used to examine heterogeneity across included clinical trials. Data were pooled using a fixed-effect or random-effects model and expressed as weighted mean difference (WMD) and 95% confidence interval (CI).
Among 1485 citations, thirteen clinical trials were found to be eligible for the current metaanalysis. UD consumption significantly decreased levels of fasting blood glucose (FBG) (WMD = – 17.17 mg/dl, 95% CI: -26.60, -7.73, I2 = 93.2%), hemoglobin A1c (HbA1c) (WMD = -0.93, 95% CI: – 1.66, -0.17, I2 = 75.0%), C-reactive protein (CRP) (WMD = -1.09 mg/dl, 95% CI: -1.64, -0.53, I2 = 0.0%), triglycerides (WMD = -26.94 mg/dl, 95 % CI = [-52.07, -1.82], P = 0.03, I2 = 90.0%), systolic blood pressure (SBP) (WMD = -5.03 mmHg, 95% CI = -8.15, -1.91, I2 = 0.0%) in comparison to the control groups. UD consumption did not significantly change serum levels of insulin (WMD = 1.07 μU/ml, 95% CI: -1.59, 3.73, I2 = 63.5%), total-cholesterol (WMD = -6.39 mg/dl, 95% CI: -13.84, 1.05, I2 = 0.0%), LDL-cholesterol (LDL-C) (WMD = -1.30 mg/dl, 95% CI: -9.95, 7.35, I2 = 66.1%), HDL-cholesterol (HDL-C) (WMD = 6.95 mg/dl, 95% CI: -0.14, 14.03, I2 = 95.4%), body max index (BMI) (WMD = -0.16 kg/m2, 95% CI: -1.77, 1.44, I2 = 0.0%), and diastolic blood pressure (DBP) (WMD = -1.35 mmHg, 95% CI: -2.86, 0.17, I2= 0.0%) among patients with T2DM.
The authors concluded that UD consumption may result in an improvement in levels of FBS, HbA1c, CRP, triglycerides, and SBP, but did not affect levels of insulin, total-, LDL-, and HDL-cholesterol, BMI, and DBP in patients with T2DM.
Several plants have been reported to affect the parameters of diabetes. Whenever I read such results, I cannot stop wondering whether this is a good or a bad thing. It seems to be positive at first glance, yet I can imagine at least two scenarios where such effects might be detrimental:
- A patient reads about the antidiabetic effects and decides to swap his medication for the herbal remedy which is far less effective. Consequently, the patient’s metabolic control is insufficient.
- A patient adds the herbal remedy to his therapy. Consequently, his blood sugar drops too far and he suffers a hypoglycemic episode.
My advice to diabetics is therefore this: if you want to try herbal antidiabetic treatments, please think twice. And if you persist, do it only under the close supervision of your doctor.
A press release informs us that the World Health Organization (WHO) and the Government of India recently signed an agreement to establish the ‘WHO Global Centre for Traditional Medicine’. This global knowledge centre for traditional medicine, supported by an investment of USD 250 million from the Government of India, aims to harness the potential of traditional medicine from across the world through modern science and technology to improve the health of people and the planet.
“For many millions of people around the world, traditional medicine is the first port of call to treat many diseases,” said Dr Tedros Adhanom Ghebreyesus, WHO Director-General. “Ensuring all people have access to safe and effective treatment is an essential part of WHO’s mission, and this new center will help to harness the power of science to strengthen the evidence base for traditional medicine. I’m grateful to the Government of India for its support, and we look forward to making it a success.”
The term traditional medicine describes the total sum of the knowledge, skills and practices indigenous and different cultures have used over time to maintain health and prevent, diagnose and treat physical and mental illness. Its reach encompasses ancient practices such as acupuncture, ayurvedic medicine and herbal mixtures as well as modern medicines.
“It is heartening to learn about the signing of the Host Country Agreement for the establishment of Global Centre for Traditional Medicine (GCTM). The agreement between Ministry of Ayush and World Health Organization (WHO) to establish the WHO-GCTM at Jamnagar, Gujarat, is a commendable initiative,” said Narendra Modi, Prime Minister of India. “Through various initiatives, our government has been tireless in its endeavour to make preventive and curative healthcare, affordable and accessible to all. May the global centre at Jamnagar help in providing the best healthcare solutions to the world.”
The new WHO centre will concentrate on building a solid evidence base for policies and standards on traditional medicine practices and products and help countries integrate it as appropriate into their health systems and regulate its quality and safety for optimal and sustainable impact.
The new centre focuses on four main strategic areas: evidence and learning; data and analytics; sustainability and equity; and innovation and technology to optimize the contribution of traditional medicine to global health and sustainable development.
The onsite launch of the new WHO global centre for traditional medicine in Jamnagar, Gujarat, India will take place on April 21, 2022.
__________________________
Of course, one must wait and see who will direct the unit and what work the new centre produces. But I cannot help feeling a little anxious. The press release is full of hot air and platitudes and the track record of the Indian Ministry of Ayush is quite frankly abominable. Here are a few of my previous posts that, I think, justify this statement:
- Mucormycosis (black fungus): is the Indian AYUSH ministry trying to decimate the population?
- The ‘AYUSH COVID-19 Helpline’: have they gone bonkers?
- Individualized Homeopathic Medicines for Cutaneous Warts – the dishonesty of homeopaths continues
- Ever wondered what a homeopathic egg on the face looks like?
- An RCT on the efficacy of ayurvedic treatment on asymptomatic COVID-19 patients
- Has homeopathy caused the dramatic decline of COVID-19 cases in India?
- Eight new products aimed at mitigating COVID-19. But do they really work?
- Siddha doctors have joined those claiming to have found a cure for COVID-19
- COVID-19: homeopathy gone berserk in Mumbai
- Brazil and India collaborate in the promotion of quackery
- Hard to believe: dangerous GOVERNMENTAL advice regarding SCAM for the corona virus pandemic
WATCH THIS SPACE!
No 10-year follow-up study of so-called alternative medicine (SCAM) for lumbar intervertebral disc herniation (LDH) has so far been published. Therefore, the authors of this paper performed a prospective 10-year follow-up study on the integrated treatment of LDH in Korea.
One hundred and fifty patients from the baseline study, who initially met the LDH diagnostic criteria with a chief complaint of radiating pain and received integrated treatment, were recruited for this follow-up study. The 10-year follow-up was conducted from February 2018 to March 2018 on pain, disability, satisfaction, quality of life, and changes in a herniated disc, muscles, and fat through magnetic resonance imaging.
Sixty-five patients were included in this follow-up study. Visual analogue scale score for lower back pain and radiating leg pain were maintained at a significantly lower level than the baseline level. Significant improvements in Oswestry disability index and quality of life were consistently present. MRI confirmed that disc herniation size was reduced over the 10-year follow-up. In total, 95.38% of the patients were either “satisfied” or “extremely satisfied” with the treatment outcomes and 89.23% of the patients claimed their condition “improved” or “highly improved” at the 10-year follow-up.
The authors concluded that the reduced pain and improved disability was maintained over 10 years in patients with LDH who were treated with nonsurgical Korean medical treatment 10 years ago. Nonsurgical traditional Korean medical treatment for LDH produced beneficial long-term effects, but future large-scale randomized controlled trials for LDH are needed.
This study and its conclusion beg several questions:
WHAT DID THE SCAM CONSIST OF?
The answer is not provided in the paper; instead, the authors refer to 3 previous articles where they claim to have published the treatment schedule:
The treatment package included herbal medicine, acupuncture, bee venom pharmacopuncture and Chuna therapy (Korean spinal manipulation). Treatment was conducted once a week for 24 weeks, except herbal medication which was taken twice daily for 24 weeks; (1) Acupuncture: frequently used acupoints (BL23, BL24, BL25, BL31, BL32, BL33, BL34, BL40, BL60, GB30, GV3 and GV4)10 ,11 and the site of pain were selected and the needles were left in situ for 20 min. Sterilised disposable needles (stainless steel, 0.30×40 mm, Dong Bang Acupuncture Co., Korea) were used; (2) Chuna therapy12 ,13: Chuna is a Korean spinal manipulation that includes high-velocity, low-amplitude thrusts to spinal joints slightly beyond the passive range of motion for spinal mobilisation, and manual force to joints within the passive range; (3) Bee venom pharmacopuncture14: 0.5–1 cc of diluted bee venom solution (saline: bee venom ratio, 1000:1) was injected into 4–5 acupoints around the lumbar spine area to a total amount of 1 cc using disposable injection needles (CPL, 1 cc, 26G×1.5 syringe, Shinchang medical Co., Korea); (4) Herbal medicine was taken twice a day in dry powder (2 g) and water extracted decoction form (120 mL) (Ostericum koreanum, Eucommia ulmoides, Acanthopanax sessiliflorus, Achyranthes bidentata, Psoralea corylifolia, Peucedanum japonicum, Cibotium barometz, Lycium chinense, Boschniakia rossica, Cuscuta chinensis and Atractylodes japonica). These herbs were selected from herbs frequently prescribed for LBP (or nerve root pain) treatment in Korean medicine and traditional Chinese medicine,15 and the prescription was further developed through clinical practice at Jaseng Hospital of Korean Medicine.9 In addition, recent investigations report that compounds of C. barometz inhibit osteoclast formation in vitro16 and A. japonica extracts protect osteoblast cells from oxidative stress.17 E. ulmoides has been reported to have osteoclast inhibitive,18 osteoblast-like cell proliferative and bone mineral density enhancing effects.19 Patients were given instructions by their physician at treatment sessions to remain active and continue with daily activities while not aggravating pre-existing symptoms. Also, ample information about the favourable prognosis and encouragement for non-surgical treatment was given.
The traditional Korean spinal manipulations used (‘Chuna therapy’ – the references provided for it do NOT refer to this specific way of manipulation) seemed interesting, I thought. Here is an explanation from an unrelated paper:
Chuna, which is a traditional manual therapy practiced by Korean medicine doctors, has been applied to various diseases in Korea. Chuna manual therapy (CMT) is a technique that uses the hand, other parts of the doctor’s body or other supplementary devices such as a table to restore the normal function and structure of pathological somatic tissues by mobilization and manipulation. CMT includes various techniques such as thrust, mobilization, distraction of the spine and joints, and soft tissue release. These techniques were developed by combining aspects of Chinese Tuina, chiropratic, and osteopathic medicine.[13] It has been actively growing in Korea, academically and clinically, since the establishment of the Chuna Society (the Korean Society of Chuna Manual Medicine for Spine and Nerves, KSCMM) in 1991.[14] Recently, Chuna has had its effects nationally recognized and was included in the Korean national health insurance in March 2019.[15]
This almost answers the other questions I had. Almost, but not quite. Here are two more:
- The authors conclude that the SCAM produced beneficial long-term effects. But isn’t it much more likely that the outcomes their uncontrolled observations describe are purely or at least mostly a reflection of the natural history of lumbar disc herniation?
- If I remember correctly, I learned a long time ago in medical school that spinal manipulation is contraindicated in lumbar disc herniation. If that is so, the results might have been better, if the patients of this study had not received any SCAM at all. In other words, are the results perhaps due to firstly the natural history of the condition and secondly to the detrimental effects of the SCAM the investigators applied?
If I am correct, this would then be the 4th article reporting the findings of a SCAM intervention that aggravated lumbar disc herniation.
PS
I know that this is a mere hypothesis but it is at least as plausible as the conclusion drawn by the authors.
Since about two years, I am regularly trying to warn people of charlatans of all types who mislead the public on COVID-related subjects. In this context, a recent paper in JAMA is noteworthy. Allow me to quote just a few passages from it:
COVID-19 misinformation and disinformation flood the public discourse; physicians are not the only source. But their words and actions “may well be the most egregious of all because they undermine the trust at the center of the patient-physician relationship, and because they are directly responsible for people’s health,” Pawleys Island, South Carolina, family medicine physician Gerald E. Harmon, MD, president of the American Medical Association (AMA), (which publishes JAMA), wrote recently. In November, the AMA House of Delegates adopted a new policy to counteract disinformation by health care professionals.
… Few physicians have been disciplined so far, even though the Federation of State Medical Boards (FSMB), representing the state and territorial boards that license and discipline physicians, and, in some cases, other health care professionals, and the American Board of Medical Specialties (ABMS), consisting of the boards that determine whether physicians can be board-certified, have issued statements cautioning against spreading false COVID-19 claims.
In July 2021, the FSMB warned that spreading COVID-19 misinformation could put a physician’s license at risk. The organization said it was responding “to a dramatic increase in the dissemination of COVID-19 vaccine misinformation and disinformation by physicians and other health care professionals.”
The ABMS released a statement in September 2021. “The spread of misinformation and the misapplication of medical science by physicians and other medical professionals is especially harmful as it threatens the health and well being of our communities and at the same time undermines public trust in the profession and established best practices in care,” the ABMS said.
In an annual survey of its 70 member boards conducted in fall 2021, the FSMB asked about complaints and disciplinary actions related to COVID-19. Of the 58 boards that responded, 67% said they had seen an uptick in complaints about licensees spreading false or misleading COVID-19 misinformation, according to results released in December 2021. But only 12 (21%) of the 58 boards said they’d taken disciplinary action against a physician for that reason…
- What percentage of lay-homeopaths misinform their patients?
- What percentage of chiropractors misinform their patients?
- What percentage of energy healers misinform their patients?
- What percentage of naturopaths misinform their patients?
- What percentage of acupuncturists misinform their patients?
- etc., etc.
As the total number of SCAM practitioners might, in some parts of the world, easily outnumber doctors, these questions are highly relevant. Yet, I am not aware of any reliable data on these issues. Judging from what I have observed (and written about) during the pandemic, I guess that the percentages are likely to be substantial and way higher than those for doctors. To me, this suggests that we ought to focus much more on SCAM practitioners if, in future health crises, we want to prevent the confusion and harm that misinformation inevitably causes.
Gullibility can be described as a failure of social intelligence in which a person is easily tricked or manipulated into a course of action for which there is no plausible evidence. To express it positively, gullible people are naively trusting and thus fall for nonsensical propositions. This renders them easy prey for exploiters. 
On this blog, we see our fair share of this phenomenon, e.g.:
- people who are easily persuaded by anecdotes,
- who disregard evidence
- who fall for pseudoscience,
- who have irrational belief systems,
- who thrive on fallacies,
- who cherry-pick the evidence that fits their belief,
- who are unable to change their views in the face of evidence,
- who interpret even contradictory facts such that they confirm their belief,
- who have no ability to think critically,
- who would do just about anything to avoid cognitive dissonance.
Let me give you just three well-known examples from the realm of so-called alternative medicine (SCAM).
- Advocates of SCAM believe that natural means safe. Yet the therapies used in SCAM are neither natural nor devoid of risks.
- Advocates of SCAM believe that treatments that have a long tradition of usage must be fine. Yet a long history might just signify that the therapy in question is based on obsolete principles.
- Advocates of integrative medicine believe that, by adding unproven therapies to our medicine bag, we might improve healthcare. Yet it is clear that such a move can only make it less effective.
If I look back on 30 years of research into SCAM, I have to say that it very much looks as though a sucker is indeed born every minute.
It was reported yesterday that the district court of Schönau in Germany has issued an order to arrest Dr. Mathias Poland, a family doctor who used to practice in Zell. He is accused of issuing certificates of favor to opponents of wearing masks during the pandemic. The order of arrest was “against a doctor from the district of Lörrach” for “issuing false certificates”.
The fact, that some German doctors have issued false exemptions from wearing masks has been known for some time. Similar things have also been reported from other countries. Often, these physicians in question seem to be practitioners of so-called alternative medicine (SCAM). To the best of my knowledge, this is the first time that a doctor has been arrested for such a crime.
So, what do we know about Mathias Poland?
His is what Dr. Poland tells us about himself (my translation):
I was born in 1958 and grew up in Stuttgart. From 1976 I studied medicine in Ulm, where I came into intensive contact with anthroposophy, which has accompanied me ever since. Further stations of my studies were Münster/Westphalia (D) and Poitiers (F). Doctorate in 1983 in Münster on a pediatric oncological topic. This was followed by further training as a specialist in general medicine in several clinics in northern Germany, acquisition of the additional qualification in homeopathy. Further training in anthroposophical medicine through numerous seminars. In 1990 I set up as a general practitioner and family doctor in Wehr/Baden (Germany) – in the following years I gained additional qualifications in Traditional Chinese Medicine and acupuncture at the University of Freiburg (Germany).
Recognition as an anthroposophical doctor by the GAÄD.
I became the doctor in charge of the Kaspar Hauser School Schopfheim 1999 – 2006. From 2009, I took over a GP practice in Zell im Wiesental (D) with an additional focus on proctology.
… Since 1.9.2019, I have been the senior physician in general medicine at the Arlesheim Clinic …
Anthroposophic medicine is a form of healthcare developed in the 1920s by Rudolf Steiner (1861–1925) in collaboration with the physician Ita Wegman (1876–1943). It is based on Steiner’s mystical ideas of anthroposophy. Why do anthroposophical doctors issue such false certificates? As far as I understand it (and to explain it very simply), anthroposophical medicine teaches that infections should not be fought against but accepted and experienced. Why? Because they are important milestones that make us better and more whole as human beings.
And why do doctors believe in anthroposophical medicine?
Search me!
This review summarized the available evidence on so-called alternative medicine (SCAM) used with radiotherapy. Systematic literature searches identified studies on the use of SCAM during radiotherapy. Inclusion required the following criteria: the study was interventional, SCAM was for human patients with cancer, and SCAM was administered concurrently with radiotherapy. Data points of interest were collected from included studies. A subset was identified as high-quality using the Jadad scale. Fisher’s exact test was used to assess the association between study results, outcome measured, and type of SCAM.
Overall, 163 articles met inclusion. Of these, 68 (41.7%) were considered high-quality trials. Articles published per year increased over time. Frequently identified therapies were biologically based therapies (47.9%), mind-body therapies (23.3%), and alternative medical systems (13.5%). Within the subset of high-quality trials, 60.0% of studies reported a favorable change with SCAM while 40.0% reported no change. No studies reported an unfavorable change. Commonly assessed outcome types were patient-reported (41.1%) and provider-reported (21.5%). The rate of favorable change did not differ based on the type of SCAM or outcome measured.
The authors concluded that concurrent SCAM may reduce radiotherapy-induced toxicities and improve quality of life, suggesting that physicians should discuss SCAM with patients receiving radiotherapy. This review provides a broad overview of investigations on SCAM use during radiotherapy and can inform how radiation oncologists advise their patients about SCAM.
In my recent book, I have reviewed the somewhat broader issue of SCAM for palliative and supportive care. My conclusions are broadly in agreement with the above review:
… some forms of SCAM—by no means all— benefit cancer patients in multiple ways… four important points:
• The volume of the evidence for SCAM in palliative and supportive cancer care is currently by no means large.
• The primary studies are often methodologically weak and their findings are contradictory.
• Several forms of SCAM have the potential to be useful in palliative and supportive cancer care.
• Therefore, generalisations are problematic, and it is wise to go by the current best evidence …
One particular finding of the new review struck me as intriguing: The rate of favorable change did not differ based on the type of SCAM. Combined with the fact that most studies are less than rigorous and fail to control for non-specific effects, this indicates to me that, in cancer palliation (and perhaps in other areas as well), SCAM works mostly via non-specific effects. In other words, patients feel better not because the treatment per se was effective but because they needed the extra care, attention, and empathy.
If this is true, it carries an important reminder for oncology: cancer patients are very vulnerable and need all the empathy and compassion they can get. Seen from this perspective, the popularity of SCAM would be a criticism of conventional medicine for not providing enough of it.
‘Survive Cancer’ is a UK charity that promotes and researches orthomolecular medicine in the treatment of cancer, septic shock, mental health, and other illnesses. They claim to provide information about research and trials and a multi-pronged treatment approach for sufferers of cancer. Specifically for cancer, they recommend the following ‘top ten‘ so-called alternative medicines (SCAMs):
- Gerson
- Vitamin C therapy
- Anti-angiogenic therapy
- Immunotherapy
- Photodynamic-/Photo-therapy
- Melatonin
- Bisphosphonates (for bone cancer)
- Coley’s toxins
- Salvestrols
- Pain management
Interesting?
Yes, because it is misleading to the extreme. Here, for example, is what they say about an old favorite of mine (and of Prince Charles):
Gerson Therapy
Max Gerson was a German doctor who in the early twentieth century devised an anti-cancer diet and regime based on radically altering the sodium/potassium ratio in the body for the better, thus allowing optimal cellular functions, and nutrition, coupled with intensive detoxification through the use of coffee enemas.
Coffee enemas (see Detox, in First Steps, 5 Rs of Cancer Survival,) are a scientifically established, and medically accepted, way of stimulating the production of glutathione-s-transferases, a major liver detoxifying enzyme family. The diet is vegetarian, low in protein, with fresh organic fruit and vegetable juices daily, and certain specified supplements, such as potassium, niacin and vitamin C. At the end of his life Gerson testified before Congress with the details of 50 cases he had cured. His daughter, Charlotte, has continued Gerson’s work in the U.S. However, she has not made an attempt to integrate modern nutritional state-of-the-art knowledge into the therapy. This is being done by Gar Hildebrand. A retrospective study showed that the Gerson therapy is much more effective than chemotherapy for ovarian cancer and melanoma, both particularly aggressive forms of cancer. Gerson himself had notable successes with various kinds of brain tumour, even after some neurological damage had occurred. Orthomolecular Oncology suggests combining Immunopower with Gerson as an update. We can also cite a remarkable case of a 11 year remission in Multiple Myeloma, another fast-moving, relentless cancer without conventional cure, otherwise conventionally untreated, achieved through a combination of Gerson and modern orthomolecular approaches. Gerson is a powerful, comprehensive therapy, still capable of producing cures, even in its unmodulated form. However, it requires great discipline, time, and extra assistance. Read Gerson’s book and/or contact the Gerson Institute for further details.
One does not need to be a genius to predict that cancer patients following this sort of advice, will significantly shorten their lives, diminish their quality of life and empty their bank account. One does, however, need to be a genius to predict when the UK charity commission is finally going to do something about the many UK charities that prey on vulnerable cancer patients.
PS
I almost forgot: the patrons of this charity are:
- HRH Princess Michael of Kent
- The Earl Baldwin of Bewdley
(Co-Chairman of the Parliamentary Committee for Alternative and Complementary Medicine) - Dr Damien Downing, MBBS, (Editor of The Journal of Nutritional and Environmental Medicine)
- Mr Peter J Gravett, MB, MRCS, FRCPath.
- Dr P J Kingsley, MB, BS, MRCS, LRCP, FAAEM, DA, D.Obst. RCOG
The 13th European Congress for Integrative Medicine is about to take place online between 4 and 7 November 2021. It will host 125+ speakers presenting from around the world. The programme will cover the following topics.
- Anthroposophic Medicine
- Arts in Healthcare
- Acupuncture
- Antimicrobial Resistance
- Ayurveda
- Covid Research
- Diabetes
- Homeopathy
- Immunology
- Integrative Oncology
- Lifestyle Medicine
- Medical Education
- Mental Health & Stress Management
- Mind and Body Connection
- Mistletoe Therapy
- Nutrition, Gut Health & Microbiome
- Pain Management
- Patient Activation & Self-Management
- Planetary & Environmental Health
- Research and Evaluation
- Social Prescribing
- Traditional Health
- Yoga
Even looking at the more detailed list of lectures, I did not find a single contribution on conventional medicine (“Integrative medicine combines conventional medicine with…” [see below]) or a lecture that is remotely critical of integrative medicine. The definition of INTEGRATED MEDICINE (IM) adopted here seems similar to the US definition we recently discussed. Here is the European definition:
Integrative medicine combines conventional medicine with evidence-informed complementary medicine and therapies to achieve the optimum health and wellbeing of the patient. Focusing on a holistic, patient-centred approach to healthcare, it takes into consideration the patient’s physical and psychological wellbeing and treats the whole person rather than just the disease.
Allow me to do a quick analysis of this definition by looking at its key elements:
- Evidence-informed: While proper medicine is BASED on evidence, IM is merely INFORMED by it. The difference is fundamental. It allows IM clinicians to use any un- or disproven so-called alternative medicine (SCAM) they can think of or invent. The evidence for homeopathy fails to show that it is effective? Never mind, IM does not need to be evidence-based, it is evidence-informed. IM physicians know homeopathy is a placebo therapy (if not they would be ill-informed which would make them unethical), but they nevertheless use homeopathy (try to find an IM clinic that does not offer homeopathy!), because IM is not EBM. IM is evidence-informed!
- Therapies that achieve optimum health and wellbeing. This is odd because the website also states that “therapies can include anything from acupuncture, yoga, massage, aromatherapy, herbal medicine, nutrition, exercise along with many more approaches, tailored to the needs of the individual” indicating that virtually anything can be included. Anyway, “optimum health and wellbeing” seems a strange and unachievable criterion. In fact, it is nothing but a ‘bait and switch‘ salesmen’s trick.
- Holistic: This is a little trick that IM proponents love. With it, they imply that normal medicine is not holistic. However, this implication is demonstrably wrong. Any good medicine is holistic, and if a sector of healthcare fails to account for the whole person, we need to reform it. (Here are the conclusions of an editorial I published in 2007 entitled ‘Holistic heath care?‘: good health care is likely to be holistic but holistic health care, as it is marketed at present, is not necessarily good. The term ‘holistic’ may even be a ‘red herring’ which misleads patients. What matters most is whether or not any given approach optimally benefits the patient. This goal is best achieved with effective and safe interventions administered humanely — regardless of what label we put on them.) Creating a branch of medicine that, like IM, pretends to have a monopoly on holism is grossly misleading and can only hinder this process.
- Patient-centred: This is the same mean little trick in a different guise. They imply that conventional medicine is not patient-centred. Yet, all good medicine is, of course, patient-centred. To imply otherwise is just daft.
- Consideration of the patient’s physical and psychological wellbeing and treating the whole person rather than just the disease: Same trick yet again! The implication is that physical and psychological wellbeing and the whole person are not all that relevant in conventional medicine where only disease labels are being treated.
Altogether, this definition of IM is unworthy of anyone with the slightest ability to think critically. I find it much worse than the latest US definition (which already is fairly awful). In fact, it turns out to be a poorly disguised bonanza of strawman fallacies combined with ‘bait and switch’ deception.
How can this be?
How can a professional organisation engage in such mean trickery?
Perhaps a look at the list of speakers will go some way towards answering the question. Have a good look, you might recognize many individuals as members of our ALTERNATIVE MEDICINE HALL OF FAME.
PS
Registration costs £ 249 (standard rate)
PPS
Perhaps I should also mention at least 4 of the many commercial sponsors of the conference:
- Boiron
- Helixor
- Iscador
- Weleda