fallacy
Advocates of so-called alternative medicine (SCAM) often sound like a broken record to me. They bring up the same ‘arguments’ over and over again, no matter whether they happen to be defending acupuncture, energy healing, homeopathy, or any other form of SCAM. Here are some of the most popular of these generic ‘arguments’:
1. It helped me
The supporters of SCAM regularly cite their own good experiences with their particular form of treatment and think that this is proof enough. However, they forget that any symptomatic improvement they may have felt can be the result of several factors that are unrelated to the SCAM in question. To mention just a few:
- Placebo
- Regression towards the mean
- Natural history of the disease
2. My SCAM is without risk
Since homeopathic remedies, for instance, are highly diluted, it makes sense to assume that they cannot cause side effects. Several other forms of SCAM are equally unlikely to cause adverse effects. So, the notion is seemingly correct. However, this ‘argument’ ignores the fact that it is not the therapy itself that can pose a risk, but the SCAM practitioner. For example, it is well documented – and, on this blog, we have discussed it often – that many of them advise against vaccination, which can undoubtedly cause serious harm.
3. SCAM has stood the test of time
It is true that many SCAMs have survived for hundreds or even thousands of years. It is also true that millions still use it even today. This, according to enthusiasts, is sufficient proof of SCAM’s efficacy. But they forget that many therapies have survived for centuries, only to be proved useless in the end. Just think of bloodletting or mercury preparations from past times.
4 The evidence is not nearly as negative as skeptics pretend
Yes, there are plenty of positive studies on some SCAMs This is not surprising. Firstly, from a purely statistical point of view, if we have, for instance, 1 000 studies of a particular SCAM, it is to be expected that, at the 5% level of statistical significance, about 50 of them will produce a significantly positive result. Secondly, this number becomes considerably larger if we factor in the fact that most of the studies are methodologically poor and were conducted by SCAM enthusiasts with a corresponding bias (see my ALTERNATIVE MEDICINE HALL OF FAME on this blog). However, if we base our judgment on the totality of the most robust studies, the bottom line is almost invariably that there is no overall convincingly positive result.
5. The pharmaceutical industry is suppressing SCAM
SCAM is said to be so amazingly effective that the pharmaceutical industry would simply go bust if this fact became common knowledge. Therefore Big Pharma is using its considerable resources to destroy SCAM. This argument is fallacious because:
- there is no evidence to support it,
- far from opposing SCAM, the pharmaceutical industry is heavily involved in SCAM (for example, by manufacturing homeopathic remedies, dietary supplements, etc.)
6 SCAM could save a lot of money
It is true that SCAMs are on average much cheaper than conventional medicines. However, one must also bear in mind that price alone can never be the decisive factor. We also need to consider other issues such as the risk/benefit balance. And a reduction in healthcare costs can never be achieved by ineffective therapies. Without effectiveness, there can be no cost-effectiveness.
7 Many conventional medicines are also not evidence-based
Sure, there are some treatments in conventional medicine that are not solidly supported by evidence. So why do we insist on solid evidence for SCAM? The answer is simple: in all areas of healthcare, intensive work is going on aimed at filling the gaps and improving the situation. As soon as a significant deficit is identified, studies are initiated to establish a reliable basis. Depending on the results, appropriate measures are eventually taken. In the case of negative findings, the appropriate measure is to exclude treatments from routine healthcare, regardless of whether the treatment in question is conventional or alternative. In other words, this is work in progress. SCAM enthusiasts should ask themselves how many treatments they have discarded so far. The answer, I think, is zero.
8 SCAM cannot be forced into the straitjacket of a clinical trial
This ‘argument’ surprisingly popular. It supposes that SCAM is so individualized, holistic, subtle, etc., that it defies science. The ‘argument’ is false, and SCAM advocates know it, not least because they regularly and enthusiastically cite those scientific papers that seemingly support their pet therapy.
9 SCAM is holistic
This may or may not be true, but the claim of holism is not a monopoly of SCAM. All good medicine is holistic, and in order to care for our patients holistically, we certainly do not need SCAM.
1o SCAM complements conventional medicine
This argument might be true: SCAM is often used as an adjunct to conventional treatments. Yet, there is no good reason why a complementary treatment should not be shown to be worth the effort and expense to add it to another therapy. If, for instance, you pay for an upgrade on a flight, you also want to make sure that it is worth the extra expenditure.
11 In Switzerland it works, too
That’s right, in Switzerland, a small range of SCAMs was included in basic health care by referendum. However, it has been reported that the consequences of this decision are far from positive. It brought no discernible benefit and only caused very considerable costs.
I am sure there are many more such ‘arguments’. Feel free to post your favorites!
My point here is this:
the ‘arguments’ used in defense of SCAM are not truly arguments; they are fallacies, misunderstandings, and sometimes even outright lies.
The ‘Münster Circle‘ is an informal association of multi-disciplinary experts who critically examine issues in and around so-called alternative medicine (SCAM). We exist since June 2016 and are the result of an initiative by Dr Bettina Schöne-Seifert, Professor and Chair of Professor and Chair of Medical Ethics at the University of Münster.
In the past, we have published several documents which have stimulated discussions on SCAM-related subjects. Yesterday, we have published our ‘MEMORANDUM INTEGRATIVE MEDICINE‘. It is a critical analysis of this subject and will hopefully make some waves in Germany and beyond.
Here is its English summary:
The merging of alternative medicine and conventional medicine has been increasingly referred to as Integrative (or Integrated) Medicine (IM) since the 1990s and has largely replaced other terms in this field. Today, IM is represented at all levels.
IM is often characterised with the thesis of the ‘best of both worlds’. However, there is no generally accepted definition of IM. Common descriptions of IM emphasise:
– the combination of conventional and complementary methods,
– the holistic understanding of medicine,
– the great importance of the doctor-patient relationship,
– the hope for optimal therapeutic success,
– the focus on the patient,
– the high value of experiential knowledge.
On closer inspection, the descriptions of IM show numerous inconsistencies. For example, medicine in the hands of doctors is stressed, but it is also emphasised that all relevant professions would be involved. Scientific evidence is emphasised, but at the same time, it is stressed that IM itself includes homeopathy as well as other unsubstantiated treatments and is only ‘guided’ by evidence, i.e. not really evidence-based. It is claimed that IM is to be understood as ‘complementary to science-based medicine’; however, this implies that IM itself is not science-based.
The ‘best of both worlds’ thesis impresses many. However, if one investigates what is meant by ‘best’, one finds that this term is not interpreted in nearly the same way as in conventional medicine. Many claims of IM are elementary components of all good medicine and thus cannot be counted among the characterising features of IM. Finally, it is hard to ignore the fact that the supporters of IM use it as a pretext to introduce unproven or disproven modalities into conventional medicine. Contrary to promises, IM has no discernible potential to improve medicine; rather, it creates confusion and entails considerable dangers. This cannot be in the interest of patients.
Against this background, it must be demanded that IM is critically scrutinised at all levels.
________________________
One of my recent posts prompted the following comment from a chiropractor: “… please don’t let me stop you…while we actually treat patients“. It was given in the context of a debate about the evidence for or against chiropractic spinal manipulations as a treatment of whiplash injuries. My position was that there is no convincing evidence, while the chiropractor argued that he has been using manipulations for this indication with good results. Here I do not want to re-visit the pros and cons of that particular debate. Since similar objections have been put to me so many times, I want rather to raise several more principal points.
Before I do this, I need to quickly get the personal stuff out of the way: the comment implies that I don’t really know what I am talking about because I don’t see patients and thus don’t understand their needs. The truth is that I started my professional life as a clinician, then I went into basic science, then I went back into clinical medicine (while also doing research), and eventually, I became a full-time clinical researcher. I have thus seen plenty of patients, certainly enough to empathize with both the needs of patients and the reasoning of clinicians. In fact, these provided the motives for my clinical research during the last decades of my professional career (more details here).
Now about the real issue that is at stake here. When offered by a clinician to a scientist, the comment “… please don’t let me stop you…while we actually treat patients” is an expression of an arrogant feeling of superiority that clinicians often harbor vis a vis professionals who are not at the ‘coal face’ of healthcare. Stripped down to its core, the argument implies that science is fairly useless because the only knowledge worth having stems from dealing with patients. In other words, it is about the tension that so often exists between clinical experience and scientific evidence.
Many clinicians feel that experience is the best guide to correct decision-making.
Many scientists feel that experience is fraught with errors, and only science can lead us towards optimal decisions.
Such arguments emerge regularly on this blog and are constant company to almost any type of healthcare. The question is, who is right and who is wrong?
As I indicated, I can empathize with both positions. I can see that, in the context of making therapeutic decisions in a busy clinic, for instance, the clinician’s argument weighs heavily and can make sense, particularly in areas where the evidence is mixed, weak, or uncertain.
However, in the context of this blog and other discussions focused on critical evaluation of the science, I am strongly on the side of the scientist. In fact, in this context, the argument “… please don’t let me stop you…while we actually treat patients” seems ridiculous and resembles an embarrassing admission of having no rational argument left for defending one’s own position.
To put my view of this in a nutshell: it is not a question of either or; for optimal healthcare, we obviously need both clinical experience AND scientific evidence (an insight that is not in the slightest original, since it is even part of Sackett’s definition of EBM).
One of my previous posts was about a press release announcing a ‘WORLDWIDE DECLARATION’, and I promised to comment about the actual declaration. This post firstly reproduces this document and secondly provides a few comments on it. Here is the document:
DEFINITIONS
Traditional, complementary and integrative healthcare (TCIH) refers to the respectful collaboration between various systems of healthcare and their health professionals with the aim of offering a person-centred and holistic approach to health.
ABOUT US
We represent a worldwide community of users and health professionals of TCIH with a large diversity of backgrounds and experiences with a common commitment to the advancement and
promotion of TCIH.
THE HEALTHCARE WE DESIRE
• Focuses on the whole person, including physical, mental, social and spiritual dimensions
• Is patient-centred and supports self-healing and health creation
• Is participative and respects individual choices
• Is evidence-based by integrating clinical experience and patient values with the best available research information
• Respects cultural diversity and regional differences
• Is an integral part of community and planetary health
• Uses natural and sustainable resources that are respectful of the health of our planet
• Integrates traditional, complementary and biomedical practices in a supportive and collaborative manner
We appreciate the benefits of conventional / biomedicine. At the same time we recognize its limitations, including:
• The insufficient therapeutic options that biomedicine provides, especially for chronic / non-communicable diseases (NCDs)
• Frequent side effects of biomedical treatments and rising antimicrobial resistance
• Fragmentation of care from increased specialization and the limits of a disease-based model
We are inspired by countries that are successfully integrating TCIH into their healthcare systems. However, we are concerned about:
• Countries that prevent, limit or undervalue the practice of TCIH
• Uninformed or unbalanced media reporting of TCIH
• Insufficient public funding of TCIH research
• Risk of reduced availability of TCIH and unregulated practices in some countries
OUR CALL TO ACTION
All countries
• Ensure full access to TCIH as part of the right to health for all
• Include TCIH into national health systems
• Provide accreditation of TCIH healthcare professionals in accordance with international training standards to ensure high quality care
• Ensure access and safety of TCIH medicines through specific regulatory pathways
• Fund research on TCIH and disseminate reliable information on TCIH to the public
All healthcare professionals
• Foster respectful collaboration between all healthcare professions towards achieving a person-centred and holistic approach to healthcare
_____________________________
And here are my comments.
- “TCIH”: in the realm of so-called alternative medicine it seems popular to create a new name for the subject at hand; this one is yet another one in a long line of innovations – sadly, it is as nonsensical as most of the previous ones.
- Person-centred and holistic approach to health: all good healthcare has these qualities.
- We represent a worldwide community: really? Who exactly are you then, and what is your ligitimization?
- Whole person, including physical, mental, social and spiritual dimensions: all good healthcare has these qualities.
- Patient-centred and supports self-healing and health creation: all good healthcare has these qualities.
- Respects individual choices: all good healthcare has these qualities.
- Evidence-based: either they do not know what this term means or they are deliberately misleading the public.
- Integral part of community and planetary health: all good healthcare has these qualities.
- Natural and sustainable resources that are respectful of the health of our planet: like Rhino horn and similar ingredients of TCM products?
- Insufficient therapeutic options that biomedicine provides: yes, conventional medicine is far from perfect, but adding something even less perfect to it cannot improve it.
- Frequent side effects of biomedical treatments and rising antimicrobial resistance: yes, conventional medicine is far from perfect, but adding something even less perfect to it cannot improve it.
- Full access to TCIH as part of the right to health for all: the ‘right to health for all’ means the right to the most effective therapies not the right to the most bizarre quackery.
- Accreditation of TCIH healthcare professionals: giving respectability to every quack would not render healthcare better or safer but worse and more dangerous.
- Access and safety of TCIH medicines through specific regulatory pathways: regulating access to unproven treatments is nothing less than a recipe for disaster.
- Research on TCIH: yes in some areas, research might be worthwhile, but it must be rigorously testing TCIH and not promoting it uncritically.
- Disseminate reliable information on TCIH to the public: thank you! This is my main aim in writing the ~2500 posts on this blog. Yet I do often get the impression that this gets disappointingly little support – and frequently the exact opposite – from enthusiasts of TCIH.
I reported about the activities of Eurocam before (see here) and I was distinctly underwhelmed with this quackery lobby group. Now they have published a press release about a ‘worldwide declaration’ in favor of integrated medicine. Here is my translation of the press release (I will comment on the actual declaration at a later stage):
With a declaration, Eurocam and the European Federation of Homeopathic Patient’s Association, among others, call for an open scientific discourse, more research funds, and more promotion of young researchers in the field of integrative medicine. The declaration is supported by the German Central Association of Homeopathic Physicians and the Homeopathy Research Institute (HRI), among others. Integrative medicine combines conventional and complementary elements in health care for the benefit of patients. The goal is patient-centred and holistic health care. Already 130 organisations have committed themselves to these goals in the medical care of the population in the Declaration.
Integrative medicine integrates complementary and conventional methods
In addition, the Declaration advocates health care that takes the whole person into account in its psychological, mental, social and spiritual dimensions. Integrative medicine in the sense of the Declaration is patient-centred and supports the body’s own regulatory abilities. In addition, it is participatory and respects individual decisions with regard to medical care. It is committed to the evidence of medical procedures, which is based on experience, patient preferences and research findings. It incorporates cultural diversity and regional differences as well as the concepts of community health and planetary health. Integrative medicine uses natural and sustainable resources and integrates complementary and conventional medical procedures.
Integrative medicine: Opportunities especially for chronic diseases and side effects
The supporters of the Declaration see opportunities for integrative medicine above all in chronic and non-communicable diseases, as well as in the frequent side effects of conventional therapies and increasing antibiotic resistance. Conventional medicine is characterised by fragmentation and divisional thinking within medical care, as well as by the increasing specialisation of the health professions. The holistic view of the patient is thus left out. Against this backdrop, the Declaration advocates anchoring integrative medicine as a legal entitlement in health care and integrating it into national health care systems. International training standards should be adapted with integrative medicine in mind, and research projects should be promoted. At the same time, balanced and high-quality patient information is needed.
________________________________
This press release requires a few short comments, in my view:
- “Integrative medicine combines conventional and complementary elements in health care for the benefit of patients.” Anyone who cares to research for longer than 10 minutes will find that very often the complementary elements are unproven and disproven treatments.
- “The goal is patient-centred and holistic health care.” By integrating unproven and disproven treatments into routine care, medicine cannot become more patient-centred but must get less effective and more expensive.
- “The Declaration advocates health care that takes the whole person into account in its psychological, mental, social and spiritual dimensions.” Any good healthcare aims at doing this.
- “Individual decisions with regard to medical care” are respected in all forms of healthcare.
- “Side effects of conventional therapies and increasing antibiotic resistance” are regrettable phenomena and much research is going on to minimize them. So-called alternative medicine (SCAM) has not yet been shown to offer a single solution to these problems.
- “The holistic view of the patient is left out” in conventional medicine. One of the most popular fallacies with SCAM advocates is the strawman fallacy.
I find the text almost comical. It reveals thought processes that lack even the most fundamental rules of logic. One really does get the impression that it had been written by people who are deplorably naive, misinformed, and quite frankly stupid.
It is not often that I publish a paper with a philosopher in a leading journal of philosophy. In fact, it is the first time, and I am rather proud of it – so much so that I must show my readers (the article is freely available via the link below and I encourage everyone to read the full text) the abstract of our article entitled WHY HOMOEOPATHY IS PSEUDOSCIENCE (Synthese (2022) 200:394):
Homoeopathy is commonly recognised as pseudoscience. However, there is, to date, no systematic discussion that seeks to establish this view. In this paper, we try to fill this gap. We explain the nature of homoeopathy, discuss the notion of pseudoscience, and provide illustrative examples from the literature indicating why homoeopathy fits the
bill. Our argument contains a conceptual and an empirical part.
In the conceptual part, we introduce the premise that a doctrine qualifies as a pseudoscience if, firstly, its proponents claim scientific standing for it and, secondly, if they produce bullshit to defend it, such that, unlike science, it cannot be viewed as the most reliable knowledge on its topic. In the empirical part, we provide evidence that homoeopathy fulfils both criteria. The first is quickly established since homoeopaths often explicitly claim scientificity.
To establish the second, we dive into the pseudo-academic literature on homoeopathy to provide evidence of bullshit in the arguments of homoeopaths. Specifically, we show that they make bizarre ontological claims incompatible with natural science, illegitimately shift the burden of proof to sceptics, and mischaracterise, cherry-pick, and misreport the evidence. Furthermore, we demonstrate that they reject essential parts of established scientific methodology and use epistemically unfair strategies to immunise their doctrine against recalcitrant evidence.
And here is our conclusion:
At the beginning of the paper, we noted that homoeopathy is commonly named one of the prototypical pseudosciences. However, there has been, to date, no comprehensive discussion as to what makes it a pseudoscience. Moreover, the problem is not trivial since the most well-known and influential demarcation criteria, such as Popper’s falsifiability criterion and Kuhn’s problem-solving criterion, cannot account for it, as we have shown. We have tried to fill this research gap using a novel bullshitology-based approach to the demarcation problem. Following this approach, we have argued that homoeopathy should be regarded as pseudoscience because its proponents claim scientific standing for it and produce argumentative bullshit to defend it, thus violating important epistemic standards central to science.
A study by an international team of researchers estimated the proportion of healthcare interventions tested within Cochrane Reviews that are effective according to high-quality evidence.
They selected a random sample of 2428 (35%) of all Cochrane Reviews published between 1 January 2008 and 5 March 2021 and extracted data about interventions within these reviews that were compared with placebo, or no treatment, and whose outcome quality was rated using Grading of Recommendations Assessment, Development and Evaluation (GRADE). They then calculated the proportion of interventions whose effectiveness was based on high-quality evidence according to GRADE, had statistically significant positive effects and were judged as beneficial by the review authors. They also calculated the proportion of interventions that suggested harm.
Of 1567 eligible interventions, 87 (5.6%) had high-quality evidence on first-listed primary outcomes, positive, statistically significant results, and were rated by review authors as beneficial. Harms were measured for 577 (36.8%) interventions, 127 of which (8.1%) had statistically significant evidence of harm. Our dependence on the reliability of Cochrane author assessments (including their GRADE assessments) was a potential limitation of our study. 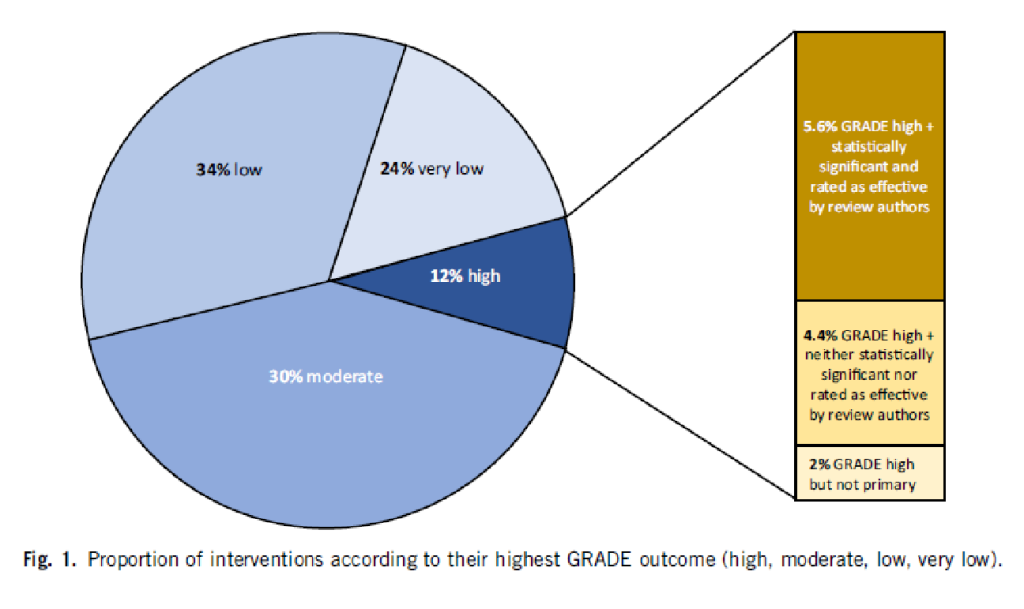
The authors drew the following conclusions: While many healthcare interventions may be beneficial, very few have high-quality evidence to support their effectiveness and safety. This problem can be remedied by high-quality studies in priority areas. These studies should measure harms more frequently and more rigorously. Practitioners and the public should be aware that many frequently used interventions are not supported by high-quality evidence.
Proponents of so-called alternative medicine (SCAM) are fond of the ‘strawman’ fallacy; meaning they like to present a picture of conventional medicine that is overtly negative in order for SCAM to appear more convincing (Prince Charles, for instance, uses this trick every single time he speaks about SCAM). Therefore I am amazed that this paper has not been exploited in that way by them. I was expecting headlines such as
Evidence-based medicine is not supported by evidence
or
Less than 6% of all conventional treatments are supported by sound evidence.
etc.
Why did they not have a field day with this new paper then?
As the article is behind a paywall, it took me a while to get the full paper (thanks Paul). Now that I have read it, I think I understand the reason.
In the article, the authors provide figures for specific types of treatments. Let me show you some of the percentages of interventions that met the primary outcome (high quality, statistically significant effect, and authors interpret as effective):
- pharmacological 73.8%
- surgical 4.6%
- exercise 5.8%
- diet 1.2%
- alternative 0.0%
- manual therapies 0.0%
So, maybe the headlines should not be any of the above but:
No good evidence to support SCAM?
or
SCAM is destroying the evidence base of medicine.
In a previous post, I reported about the ‘biggest ever’, ‘history-making’ conference on integrative medicine. It turns out that it was opened by none other than Prince Charles. Here is what the EXPRESS reported about his opening speech:
Opening the conference, Charles said:
“I know a few people have seen this integrated approach as being in some way opposed to modern medicine. It isn’t. But we need to combine this with a personal approach that also takes account of our beliefs, hopes, culture and history. It builds upon the abilities of our minds and bodies to heal, and to live healthy lives by improving diet and lifestyle.”
Dr. Michael Dixon, Chair of the College of Medicine, said:
“Medicine, as we know it, is no longer affordable or sustainable. Nor is it able to curb the increase in obesity, mental health problems and most long-term diseases. A new medical mindset is needed, which goes to the heart of true healthcare. The advantages and possibilities of social prescription are limitless. An adjustment to the system now will provide a long-term, sustainable solution for the NHS to meet the ever-increasing demand for funding and healthcare professionals.”
_______________________
Charles very kindly acknowledges that not everyone is convinced about his concept of integrated/integrative medicine. Good point your royal highness! But I fear Charles did not quite understand our objections. In a nutshell: it is not possible to cure the many ills of conventional medicine by adding unproven and disproven therapies to it. In fact, it distracts from our duty to constantly improve conventional medicine. And pretending it is all about diet and lifestyle is simply not true (see below). Moreover, it is disingenuous to pretend that diet and lifestyle do not belong to conventional healthcare.
Dr. Dixon’s concern about the affordability of medicine is, of course, justified. But the notion that “the advantages and possibilities of social prescription are limitless” is a case of severe proctophasia, and so is Dixon’s platitude about ‘adjusting the system’. His promotion of treatments like Acupuncture, Alexander Technique, Aromatherapy, Herbal Medicine, Homeopathy, Hypnotherapy, Massage, Naturopathy, Reflexology, Reiki, Tai Chi, Yoga Therapy will not adjust anything, it will only make healthcare less efficient.
I do not doubt for a minute that doctors are prescribing too many drugs and that we could save huge amounts by reminding patients that they are responsible for their own health while teaching them how to improve it without pills. This is what we learn in medical school! All we need to do is remind everyone concerned. In fact, Charles and his advisor, Michael, could be most helpful in achieving this – but not by promoting a weird branch of healthcare (integrative/integrated medicine or whatever other names they choose to give it) that can only distract from the important task at hand.
I was alerted to the following conference announcement:
The MEP Interest Group on Integrative Medicine and Health is delighted to invite you to the event ‘Integrative Medicine and Health in prevention and management of COVID-19 and long COVID’ on Thursday 2 June 16.00–18.00 CEST.
This event will give you in-depth information about:
Expert speakers will share their knowledge and insights about how:
• Complementary and Integrative Medicine and Health interventions can improve resilience to COVID-19 infection.
• Promoting resilience and health restoration can reduce the risk of severe COVID-19 or development of Long COVID.
• These interventions can improve the recovery from Long COVID.
Key speakers and topics:
Therapeutic strategies of complementary medicines in the COVID 19 pandemic and Long COVID in addition to conventional medicine
Dr Joanna Dietzel, MD Neurologist, Acupuncturist. Department for integrative & complementary medicine, Institute of social medicine, epidemiology and health economics, Charité – Universitätsmedizin Berlin, Germany.
Chinese herbal medicine treatment in cases of infections with SARS-CoV-2 – therapeutic strategies for COVID-19 and Long COVID
Dr Christian Thede, MD, General practitioner, specialised in Acupuncture and Chinese Medicine. Former lecturer in Chinese medicine, University of Witten-Herdecke, Germany
Instructor for Acupuncture and Chinese Medicine at International Society of Chinese Medicine (SMS).
Traditional and Complementary Medicine contributions to health system resilience during COVID-19 – the WHO perspective
Dr Geetha Kopalakrishna, MD, Bachelor of Ayurvedic Medicine & Surgery
Technical Officer at Traditional, Complementary & Integrative Medicine, Department of Service Delivery and Safety, World Health Organization, Geneva, Switzerland
Key member of the AYUSH-based COVID-19 response Task Force for the Government of India.
Research programme into integrative medicine’s contribution to improving resilience to COVID-19 infection and reducing the risk of severe COVID-19 or development of Long COVID
Dr Helene M. Langevin, Director at National Center for Complementary and Integrative Health, National Institutes of Health, Bethesda, Maryland (MD), USA. Previously, Director of the Harvard Osher Center for Integrative Medicine and professor of medicine at Harvard Medical School, Boston (MA) and professor of neurological sciences at the Larner College of Medicine at the University of Vermont (VT).
Q&A sessions after the presentations.
Resilience to infections: a solution for COVID-19 and other infectious illnesses
Studies show that certain common medical conditions put people at higher risk for severe illness and death from COVID-19. Nearly two-thirds of COVID-19 hospitalizations could be attributed to obesity, diabetes, hypertension, and heart failure. There is increasing awareness that a health system that focuses on improving health could prevent all these conditions to a large extent.
Long COVID
More than 40% of people who have or had COVID-19 get long COVID, and among people who needed hospitalization, the statistics go up to 57%. The recovery from such post viral syndromes will be greatly helped by offering patients access to complementary and integrative medicine interventions that aim at restoring their health balance.
MEP Interest Group on Integrative Medicine and Health
The event is hosted by the members of the MEP Interest Group on Integrative Medicine & Health:
Michèle Rivasi, Greens/EFA, France
Sirpa Pietikäinen, EPP, Finland
Tilly Metz, Greens/EFA, Luxembourg
Margrete Auken, Greens/EFA, Denmark
Romana Jerković, S&D, Croatia
Manuela Ripa, Greens/EFA, Germany
I had not been aware of the ‘MEP Interest Group on Integrative Medicine & Health‘. Therefore, I looked it up and found this:
The newly established Interest Group on Integrative Medicine & Health continues the work of the former MEP Interest Group on CAM. This group brings together MEPs who work collectively to promote the inclusion of CAM as part of Integrative Medicine & Health in all possible European Parliament public health policy.
Why an Interest Group in the European Parliament?
One in two EU citizens uses complementary medicine either alongside or as an alternative to conventional biomedical care. This high demand is not yet reflected in EU or national health policy or provision. In addition, there is diversity in complementary medicine regulation across the EU. There are differences in who can practice complementary medicine, what qualifications are required and how services are offered and financed. These discrepancies mean that citizens experience practical and attitudinal barriers that limit their access to and use of TCIM.
The health sector in the EU Member States is facing considerable challenges, such as antimicrobial resistance (AMR), increasing prevalence of Non-Communicable Diseases (NCDs) and soaring costs. Complementary medicine can offer a significant contribution to meet these challenges. These modalities are “integrative”, offering patient-centered healthcare, based on evidence-informed integration of conventional biomedicine and complementary medicine. Integrative Medicine and Health focuses on the whole person and considers the individual in its physical, psychological, spiritual, social and environmental context. It is inclusive of all professions and practices that use this approach and meets the demand of EU citizens for a more holistic, patient-centered approach in medicine. At the same time, TCIM is at the center of political and scientific debate. In this context, a forum for discussion on Integrative and Complementary Medicine’s contribution to EU health systems will bring clarity and rationality to this debate.
Aims and objectives of the Interest Group on Integrative Medicine & Health
- Establish and maintain a forum for discussion and action with all stakeholders regarding Integrative Medicine and Health.
- Raise awareness of Integrative Medicine and its contribution to more sustainable healthcare systems in the EU and a more holistic approach to health.
- Focus on the integration of complementary modalities into the health systems of the EU Member States.
- Protect and promote citizens’ right to choose their own healthcare while providing access to Integrative Medicine and Health information.
- Advocate for EU involvement in setting unified standards to regulation of Integrative Medicine and Health.
__________________________________
Unified standards? But what about high or perhaps just scientific standards? What about first doing the research and then making claims about CAM or TCIM or however you decide to call it? Has common sense gone out of fashion?
Yes, you guessed it: I am seriously underwhelmed by all this. To show you why, let me list just a few claims from the above two statements that are based purely on wishful thinking:
- Complementary and Integrative Medicine and Health interventions can improve resilience to COVID-19 infection.
- These interventions can improve the recovery from Long COVID.
- Studies show that certain common medical conditions put people at higher risk for severe illness and death from COVID-19.
- The recovery from such post viral syndromes will be greatly helped by offering patients access to complementary and integrative medicine interventions that aim at restoring their health balance.
- One in two EU citizens uses complementary medicine either alongside or as an alternative to conventional biomedical care.
- The health sector in the EU Member States is facing considerable challenges, such as antimicrobial resistance (AMR), increasing prevalence of Non-Communicable Diseases (NCDs) and soaring costs. Complementary medicine can offer a significant contribution to meet these challenges.
- These modalities are “integrative”, offering patient-centered healthcare, based on evidence-informed integration of conventional biomedicine and complementary medicine.
- Integrative medicine … meets the demand of EU citizens for a more holistic, patient-centered approach in medicine.
I find all this confusing and concerning in equal measure. I also seriously doubt that the forum for discussion on Integrative and Complementary Medicine will bring clarity and rationality to this debate. If they really wanted a debate, they would need to include a few critical thinkers; can anyone recognize one on the list of speakers? I cannot!
I fear the aim of the group and their meeting is to mislead us all into thinking that CAM, TCIM, etc. generate more good than harm without ever delivering the evidence for that assumption. Therefore, I suggest they rename both the conference as well as their group:
‘Wishful thinking in prevention and management of COVID-19 and long COVID’
and
MEP Interest Group on Wishful Thinking and Promotion of Quackery
PS
As an antidote to wishful thinking, I recommend reading some proper science papers on the subject. Here are the conclusions of an up-to-date and wishful-thinking-free review on the subject of post-acute infection syndrome:
Unexplained post-acute infection syndromes (PAISs) appear to be an under-recognized feature of a spectrum of infectious diseases in a minority of patients. At present, our understanding of the underlying pathophysiologic mechanisms and etiologic factors is poor and there are no known objective markers or effective therapeutic options. More basic biomedical research is needed. The overlap of symptoms, signs, and general features of the individual PAISs suggests the involvement of shared pathological pathways and the possibility that common diagnostic markers, or even a unified etiological model, might be established.
However, some symptoms or clinical characteristics seem to be trigger-specific or more prevalent in one PAIS than in others, emphasizing the need for cohorts with a well-documented infectious trigger. The overall clinical picture of many PAISs often overlaps with the presentation of post-infectious ME/CFS or fibromyalgia, or resembles other fatiguing, neurological, or rheumatic disorders. Exploiting existing knowledge of these conditions might help guide future scientific discovery and progress in clinical care.
The SARS-CoV-2 pandemic uncovered a significant gap in knowledge about post-acute sequelae of infectious diseases and identified the need for better diagnostic care and clinical infrastructure for patients experiencing these long-term effects. In addition to basic biomedical research, more needs to be done to refine diagnostic criteria and obtain more reliable estimates of the prevalence and societal burden of these disorders to help shape health-policy decisions. Moreover, we call for unified nomenclature and better conceptualization of post-acute infection symptoms.
There is much to be done, but the unprecedented amount of attention and resources that have recently been allocated to the study of COVID-19-related pathology brings a promise of much-needed progress in the wider field of unexplained infection-associated chronic disability.
Anyone who has followed this blog for a while will know that advocates of so-called alternative medicine (SCAM) are either in complete denial about the risks of SCAM or they do anything to trivialize them. Here is a dialogue between a SCAM proponent (P) and a scientist (S) that is aimed at depicting this situation. The conversation is fictitious, of course, but it is nevertheless based on years of experience in discussing these issues with practitioners of various types of SCAM. As we shall see, the arguments turn out to be perfectly circular.
P: My therapy is virtually free of risks.
S: How can you be so sure?
P: I am practicing it for decades and have never seen a single problem.
S: That could have several reasons; perhaps the patients who experience problems did simply not come back.
P: I find this unlikely.
S: I don’t, and I know of reports where patients had serious complications after the type of SCAM you practice.
P: These are isolated case reports. They do not amount to evidence.
S: How do you know they are isolated?
P: They must be isolated because, in the many clinical trials of my therapy available to date, you will not find any evidence of serious adverse effects.
S: That is true, but it has been repeatedly shown that these trials regularly fail to mention side effects altogether.
P: That’s because there aren’t any.
S: Not quite, clinical trials should always mention adverse effects, and if there were none, they should mention this too.
P: So, you admit that you have no evidence that my therapy causes adverse effects.
S: The thing is, I don’t need such evidence. It is you, the practitioners of this therapy, who should provide evidence that your treatments are safe.
P: We did! The complete absence of reports of side effects constitutes that evidence.
S: Except, there is some evidence. I already told you that there are several case reports of serious problems.
P: But case reports are anecdotes; they are no evidence.
S: Look, here is a systematic review of all the case reports. You cannot possibly deny that this is a concern.
P: It’s still merely a bunch of anecdotes, nothing more.
S: Only because your profession does nothing about it.
P: What do you think we need to do about it?
S: Like other professions, you need to systematically record adverse effects.
P: How would that help?
S: It would give us a rough indication of the size and severity of the problem.
P: This sounds expensive and complicated to organize.
S: Perhaps, but it is necessary if you want to be sure that your therapy is safe.
P: But we are sure already!
S: No, you believe it, but you don’t know it.
P: You are getting on my nerves with your obsession. Don’t you know that the true danger in healthcare is the adverse effects of pharmaceutical drugs?
S: But these drugs are also effective.
P: Are you saying my therapy isn’t?
S: What I am saying is that the drugs you claim to be dangerous do more good than harm, while this is not at all clear with your SCAM.
P: To me, that is very clear. My therapy helps many and harms nobody!
S: How do you know that it harms nobody?
… At this point, we have gone full circle and we can re-start this conversation from its beginning.
