evidence
It has been reported that a recent inspection from the Care Quality Commission (CQC) found that the diagnostic imaging service at AECC University College in Parkwood Road, Bournemouth, requires improvement in three out of four areas – including patient safety. This is surprising not least because the AECC prides itself on being “a leading higher education institution in healthcare disciplines, nationally and internationally recognised for quality and excellence.” 
The unannounced inspection in May this year resulted in several demands for the service to improve upon. For example, the CQC report said staff “did not receive all of the training they needed to keep patients safe” and that patient chaperones “did not receive chaperone training”. Moreover, managers were reported as not always ensuring staff were competent to operate certain equipment. In fact, there was no record of staff competencies which meant inspectors “could not tell if staff had been trained to use equipment”. General cleanliness was also found lacking in relation to certain procedures, namely no sink in any of the site’s nine ultrasound rooms (including those for transvaginal scans) – meaning staff carrying out ultrasound scanning did not have access to a clinical handwashing facility.
The CQC states on its website that it “is the independent regulator of health and adult social care in England. We make sure health and social care services provide people with safe, effective, compassionate, high-quality care and we encourage care services to improve. We monitor, inspect and regulate services. Then we publish what we find, including performance ratings, to help people choose care. Where we find poor care, we will use our powers to take action.”
No doubt, these are laudable aims. What I find, however, disappointing is that the CQC’s inspection of the AECC did not question the nature of some of the courses taught by the AECC. Earlier this year, I reported in a blog post that the AECC has announced a new MSc ‘Musculoskeletal Paediatric Health‘. This motivated me to look into the evidence for such a course. This is what I found with several Medline searches (date of the review on chiropractic for any pediatric conditions, followed by its conclusion + link [so that the reader can look up the evidence]):
2008
I am unable to find convincing evidence for any of the above-named conditions.
2009
Previous research has shown that professional chiropractic organisations ‘make claims for the clinical art of chiropractic that are not currently available scientific evidence…’. The claim to effectively treat otitis seems to
be one of them. It is time now, I think, that chiropractors either produce the evidence or abandon the claim.
2009
The … evidence is neither complete nor, in my view, “substantial.”
2010
2018
What seems to emerge is rather disappointing:
- There are no really new reviews.
- Most of the existing reviews are not on musculoskeletal conditions.
- All of the reviews cast considerable doubt on the notion that chiropractors should go anywhere near children.
But perhaps I was too ambitious. Perhaps there are some new rigorous clinical trials of chiropractic for musculoskeletal conditions. A few further searches found this (again year and conclusion):
2019
2018
I might have missed one or two trials because I only conducted rather ‘rough and ready’ searches, but even if I did: would this amount to convincing evidence? Would it be good science?
No! and No!
So, why does the AECC offer a Master of Science in ‘Musculoskeletal Paediatric Health’?
____________________
Isn’t that a question the CQC should have asked?
Warning: Exceptionally, this post is not on so-called alternative medicine but on a different scam.
The current issue of the BMJ carries an editorial that is worth quoting on my blog, I think. I have never made a secret of the fact that I am against Brexit. In fact, I re-took German nationality because of it. Therefore, I am in agreement with Kamran Abbasi, the BMJ editor and author of the editorial. Here are what I consider the two most important paragraphs from his article:
… In the absence of public debate and meaningful data six years after the UK’s Brexit referendum, we asked Richard Vize to examine the effects of Brexit on health and care (doi:10.1136/bmj.o1870).20 The news isn’t all bad, although there isn’t much good. Brexit hasn’t brought about a cut in NHS funding but did fail to deliver the £350m weekly windfall that Boris Johnson and others promised. The European Working Time Directive remains in place, and the predicted “stampede” of European doctors leaving the NHS hasn’t happened. But the impacts on social care and lower paid staff are harming delivery of care in an increasingly multidisciplinary service.
Health technology, life science industries, and research, where integration with Europe was greatest and benefits most obvious, are being damaged. Promises to cut red tape have created new complexities and been tarnished by suspect procurement practices at the height of the pandemic (doi:10.1136/bmj.o1893).21 Perhaps the most damning legacy of Brexit, however, is the state of unreadiness it created for a pandemic that required utmost readiness. Whether or not you agree Brexit was the right decision, you should at least agree that it is a decision worthy of question, analysis, and redoubled effort if the signs are good and possibly even reversal if the damage is too great.
This quote probably makes more sense if one also reads the paper referenced in its 2nd link. So, please allow me to quote from this article as well:
… In a highly critical report, the Commons Public Account Committee accuses the Department of Health and Social Care of “woefully inadequate record keeping” and failing to meet basic requirements to publicly report ministers’ external meetings or deal with potential conflicts of interest when awarding testing contracts to the company.
The committee said that large gaps in the document trail meant it was impossible to say the contracts were awarded properly in the way that would be expected, even allowing for the exceptional circumstances and accelerated processes in place at the time. The first contract, for £132m, was awarded at the height of the covid pandemic in March 2020, when the department had suspended the normal requirements for competition between suppliers in the award of government contracts.
The report noted that officials were aware of contacts between Matt Hancock, the then health and social care secretary, and Owen Paterson, a Conservative MP and paid consultant for Randox, and of hospitality that Hancock received from Randox’s founder Peter Fitzgerald in 2019, but failed to identify any conflicts of interest before awarding the first contract.
The department set up a “VIP lane,” through which suppliers put forward by officials, MPs, ministers, or Number 10 would be given priority. Suppliers coming through priority routes were awarded £6bn out of the total £7.9bn of testing contracts awarded between May 2020 and March 2021, the committee noted…
This is by no means all, and I do encourage you to read these articles in full. Once you have, you might ask yourself as I do:
Has Britain become a banana republic?
I have often called out unreliable or fraudulent research in the realm of Traditional Chinese Medicine (TCM). I think it is important to do so because the abundance of scientific misconduct is such that it has become a danger to public health. Today, I present yet another example:
This recent review claimed to summarize the evidence on TCM in treating MI, the clinical evaluations of TCM in treating male infertility (MI), and the molecular mechanisms of TCM effects. I was alerted to the fact that the authors cite a paper on acupuncture that I had co-authored. Here is the section in question from the review:
Acupuncture is one of the therapeutic techniques that are part of TCM. Acupuncture is a non-invasive technique and is regarded as free of risk if performed by trained personnel [35]. One of the advantages of acupuncture was that the incidence of adverse effects was substantially lower than that of many drugs or other accepted [35]. Acupuncture has been used in the treatment of male and female infertility and in assisted reproductive technology treatments for many years. A total of 100 patients with MI who met the diagnostic criteria were randomly divided into two groups [7]. Half of the patients received acupuncture treatment, and the other half received placebo acupuncture. After 10 weeks treatment, acupuncture successfully improved the indicators of the semen, including the spermatozoa survival rate, b-level activity rate, sperm density, sperm activity rate. A total of 28 infertile patients with severe oligoasthenozoospermia received acupuncture according to the principles of acupuncture and 29 infertile patients received placebo acupuncture. A significantly higher percentage of motile sperm (World Health Organization categories A-C), but no effect on sperm concentration, was found after acupuncture compared with placebo acupuncture [36]. Of the 279 cases of male sterility treated by the combination of acupuncture, pilose antler essence injection to acupoints and oral administration of Chinese materia medica, 142 cases (47.8%) were cured, 81 cases (27.3%) markedly effective, 53 cases (17.8%) effective and 21 cases (7.1%) ineffective [37]. The therapeutic effect of the combination of these three treatments was satisfactory.
Ref 7
Emerging evidence has shown that cell-cell interactions between testicular cells, in particular at the Sertoli cell-cell and Sertoli-germ cell interface, are crucial to support spermatogenesis. The unique ultrastructures that support cell-cell interactions in the testis are the basal ES (ectoplasmic specialization) and the apical ES. The basal ES is found between adjacent Sertoli cells near the basement membrane that also constitute the blood-testis barrier (BTB). The apical ES is restrictively expressed at the Sertoli-spermatid contact site in the apical (adluminal) compartment of the seminiferous epithelium. These ultrastructures are present in both rodent and human testes, but the majority of studies found in the literature were done in rodent testes. As such, our discussion herein, unless otherwise specified, is focused on studies in testes of adult rats. Studies have shown that the testicular cell-cell interactions crucial to support spermatogenesis are mediated through distinctive signaling proteins and pathways, most notably involving FAK, Akt1/2 and Cdc42 GTPase. Thus, manipulation of some of these signaling proteins, such as FAK, through the use of phosphomimetic mutants for overexpression in Sertoli cell epithelium in vitro or in the testis in vivo, making FAK either constitutively active or inactive, we can modify the outcome of spermatogenesis. For instance, using the toxicant-induced Sertoli cell or testis injury in rats as study models, we can either block or rescue toxicant-induced infertility through overexpression of p-FAK-Y397 or p-FAK-Y407 (and their mutants), including the use of specific activator(s) of the involved signaling proteins against pAkt1/2. These findings thus illustrate that a potential therapeutic approach can be developed to manage toxicant-induced male reproductive dysfunction. In this review, we critically evaluate these recent findings, highlighting the direction for future investigations by bringing the laboratory-based research through a translation path to clinical investigations.
This paper does not relate to the statement it is meant to support by the review authors.
Ref 35
The review by Qin et al (1) includes 5 trials none of which should have been included in a quality metaanalysis as the methodology was unconvincing: In the trial by Alraek et al., patients were randomised to receive either acupuncture or no treatment. This means that no attempt was made to control for the effects of placebo or extra attention. Therefore, this study does not demonstrate an effect of acupuncture as the outcome could be due to non-specific effects unrelated with this therapy. By contrast, the trial by Aune et al. did attempt to control for placebo effects by using a sham control group. Sham acupuncture was given using six needles superficially inserted in the calves, thighs or abdomen outside known acupuncture points or meridians. Needles were not manipulated in the sham group. Sham or placebo controls have the purpose of rendering patients unaware of whether they receive the real or the sham treatment. The method used here cannot achieve this aim; patients would be easily able to tell which intervention they received. In other words, this study also did not adequately control for placebo effects. The remaining three trials are all not Medline-listed, authored by Chinese investigators and published in inaccessible journals. This should disqualify them from inclusion as they were unverifiable by the peer review process. According to the published table, they were equivalence trials of acupuncture versus antibiotics with a sample size around 30. This means they are grossly underpowered and thus unable to generate reliable results. Unless BJOG peer reviewers could see the primary articles, or be provided with translations from Chinese, the systematic review should not have been accepted. The “many eyes of science” requires transparency, testing, challenge and verification. Although in the past, inconclusive results of acupuncture have not been thought to be due to Chinese influence (2), it has been noted that virtually all recent published acupuncture trials are “positive” (3), raising questions of publication and other biases. Our colleagues are under tremendous pressure to publish, but we do them no favours by effectively lowering the standard of scientific peer review. Elite journals too have an obligation to train and reiterate about publication ethics and sound scientific writing (4). As none of the primary studies convincingly demonstrated that acupuncture is an effective therapy for recurrent urinary tract infections, no positive conclusion was warranted. Although Qin et al. did state that the risk of bias of the included trials was generally high or unclear (1), the BJOG nevertheless allowed them to turn massive uncertainty into relatively firm, positive conclusions in the abstract (“Acupuncture appeared to be beneficial for treatment and prophylaxis of rUTIs”) and tweetable abstract (“This review found that acupuncture may improve treatment and prevent recurrence of urinary tract infection in women”), thus leading to excited media headlines that inevitably mislead the public. ‘May’ is a weasel word which should be avoided as it is unfalsifiable (for example, pigs do not fly but they ‘may’ fly in the future). The definite, straightforward conclusion must be “There is no good evidence to support the use of acupuncture for the treatment and prophylaxis of recurrent UTIs”. It is not acceptable to give international credibility to an implausible modality that no objective, independent high-quality review has found effective beyond placebo (5). The dampening accompanying mini-commentary (6) does not undo the damage.
The review should be withdrawn while the primary papers are translated for peer reviewers to examine, the above limitations discussed in the text, and the positive ‘spin’ in conclusions corrected. These improvements would consolidate the researchers’ probity and justify the accolade of BJOG publication.
Our letter to the editor does not bear any relation to the statement it is meant to support by the review authors.
Ref 36
In this first prospective, randomized, single-blind, placebo-controlled study, 28 infertile patients with severe oligoasthenozoospermia received acupuncture according to the principles of traditional Chinese medicine (TCM) and 29 infertile patients received placebo acupuncture. A significantly higher percentage of motile sperm (World Health Organization categories A–C), but no effect on sperm concentration, was found after acupuncture compared with placebo acupuncture.
This small study is far from convincing and does not lend itself to far-reaching conclusions
Ref 37
Of the 279 cases of male sterility treated by the combination of acupuncture, pilose antler
essence injection to acupoints and oral administration of Chinese materia medica, 142
cases (47.8%) were cured, 81 cases (27.3%) markedly effective, 53 cases (17.8%) effective
and 21 cases (7.1%) ineffective. The therapeutic effect of the combination of these three
treatments was satisfactory.
This study had no control group and used two different therapies. Therefore, it does not allow any conclusion about the effectiveness of acupuncture.
____________________
Perhaps you feel that these errors are trivial. But I would disagree. The review authors’ praise of acupuncture for MI is misplaced and will mislead the public. There are plenty of reviews on the subject, and those that are not overtly biased arrive at conclusions like these:
- The current evidence on acupuncture for oligoasthenozoospermia is inadequate to draw a solid conclusion due to the poor methodological quality. Rigorous full-scale RCTs are needed to validate the therapeutic efficacy and safety of acupuncture in treating oligoasthenozoospermia.
- The current evidence showing that acupuncture might improve poor semen quality is insufficient because of the small number of studies, inadequacy of procedures and/or insufficient information for semen analysis, high levels of heterogeneity, high risk of bias, and poor quality of reporting. Further large, well-designed RCTs are required.
So, how did this sloppy review come about?
Its authors are affiliated to the TCM Regulating Metabolic Diseases Key Laboratory of Sichuan Province, Hospital of Chengdu University of Traditional Chinese Medicine, Chengdu 610072, China, and the Tea Research Institute, Sichuan Academy of Agricultural Sciences, Chengdu 610066, China. A footnote tells us that their review was supported by the National Natural Science Foundation of China [No. 81973647] and the Xinglin scholar discipline promotion talent program of Chengdu University of traditional Chinese medicine [No. BSH2021018]. This sounds respectable enough.
The journal that published the review is ‘Pharmacological Research – Modern Chinese Medicine‘. Its stated aims are as follows: The journal publishes articles reporting on advances in our comprehension of mechanism and safety in experimental pharmacology and clinical efficacy and safety of pharmacologically active substances, including compound prescriptions, utilized in Traditional Chinese Medicine applying modern scientific research methods. Studies reporting also on the mechanisms of actions of the active substance(s) investigated are encouraged.
The editors in chief of the journal are Guan-Hua Du, PhD, China Academy of Chinese Medical Sciences Institute of Chinese Materia Medica, Beijing, China and Emilio Clementi, M.Mus, MD, PhD, University of Milan, Milan, Italy. No doubt, these are respectable scientists. And because they are, they should make sure that what they publish is correct – a criterion this recent review clearly does not meet.
I had totally forgotten this amusing little episode: According to THE GUARDIAN, Jacob Rees-Mogg (JRM) once tweeted that I should be locked up in the Tower of London!
If you are not from the UK, you may not know this Member of Parliament. So, let me explain.
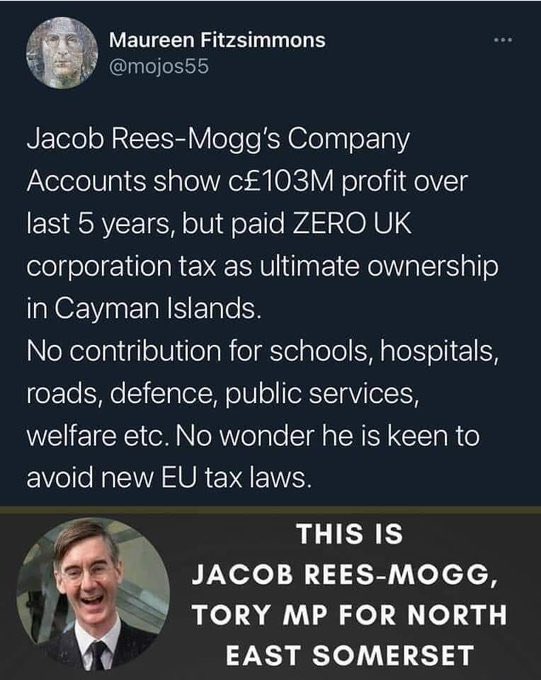
JRM is the MP for North East Somerset and currently the ‘Minister for Brexit Opportunities and Government Efficiency’. His personal net worth is estimated to be well over £100 million. I probably don’t need to add much more about JRM; there is plenty about him on the Internet and on social media, for instance, this little gem:
Some of JRM’s medically relevant voting records are revealing:
- He voted against raising welfare benefits five times in 2013.
- He voted against higher benefits over long periods for those unable to work as a result of an illness or disability: 14 votes over 5 years.
- Between 2012-2016, he voted 52 times to reduce the spending on welfare benefits.
- He voted to exempt pubs and clubs where food is not served from the smoking ban in October 2010.
- He voted against a law to make private vehicles smoke-free if a child is present.
- He voted against allowing terminally ill people to be given assistance in ending their lives.
Wikipedia mentions that Rees-Mogg is against abortion in all circumstances, stating: “life begins at the point of conception. With same-sex marriage, that is something that people are doing for themselves. With abortion, that is what people are doing to the unborn child.” In September 2017, he expressed “a great sadness” on hearing about how online retailers had reduced pricing of emergency contraception.
In October 2017, it was reported that Somerset Capital Management, of which Rees-Mogg was a partner, had invested £5m in Kalbe Farma, a company that produces and markets misoprostol pills designed to treat stomach ulcers but widely used in illegal abortions in Indonesia. Rees-Mogg defended the investment by arguing that the company in question “obeys Indonesian law so it’s a legitimate investment and there’s no hypocrisy. The law in Indonesia would satisfy the Vatican”. Several days later, it was reported that the same company also held shares in FDC, a company that sold drugs used as part of legal abortions in India. Somerset Capital Management subsequently sold the shares it had held in FDC. Rees-Mogg said: “I am glad to say it’s a stock that we no longer hold. I would not try to defend investing in companies that did things I believe are morally wrong”.
In a nutshell, JRM seems to stand for pretty much everything that I am against. But that is no reason to send me to the Tower of London. So, what exactly was JRM referring to when he wanted me locked up?
The Guardian article explains: At a press conference to mark his retirement [Ernst] agreed with a Daily Mail reporter’s suggestion that the Prince of Wales is a “snake-oil salesman”. In the living room of his house in Suffolk he unpacks the label with the precision on which he prides himself. “He’s a man, he owns a firm that sells this stuff, and I have no qualms at all defending the notion that a tincture of dandelion and artichoke [Duchy Herbals detox remedy] doesn’t do anything to detoxify your body and therefore it is a snake oil.” Far from regretting the choice of words and the controversy it has generated, he appears to relish it.
Looking back at all this bizarre story, I am surprised that JRM did not advocate chopping my head off in the Tower of London. He must have been in a benevolent mood that day!
The interest in the medicinal properties of honey is lively. A recent review, for instance, concluded that honey is a safe natural substance, effective in the inhibition of bacterial growth and the treatment of a broad range of wound types, including burns, scratches, diabetic boils (Skin abscesses associated with diabetic), malignancies, leprosy, fistulas, leg ulcers, traumatic boils, cervical and varicose ulcers, amputation, burst abdominal wounds, septic and surgical wounds, cracked nipples, and wounds in the abdominal wall. Honey comprises a wide variety of active compounds, including flavonoids, phenolic acid, organic acids, enzymes, and vitamins, that may act to improve the wound healing process. Tissue-engineered scaffolds have recently attracted a great deal of attention, and various scaffold fabrication techniques are being researched. 
But there is also reason to be cautious. The U.S. Food and Drug Administration (FDA) posted warning letters to four companies for illegally selling honey-based products that may pose a significant health risk to consumers. The FDA’s laboratory testing found that product samples contained active drug ingredients not listed on the product labels, including the active drug ingredients found in Cialis (tadalafil) and Viagra (sildenafil), which are FDA approved drugs used to treat men with erectile dysfunction. Sildenafil and tadalafil are restricted to use under the supervision of a licensed health care professional. These undeclared ingredients may interact with nitrates found in some prescription drugs, such as nitroglycerin, and may lower blood pressure to dangerous levels. People with diabetes, high blood pressure, high cholesterol, or heart disease often take nitrates.
“Tainted honey-based products like these are dangerous because consumers are likely unaware of the risks associated with the hidden prescription drug ingredients in these products and how they may interact with other drugs and supplements they may take,” said FDA Associate Commissioner for Regulatory Affairs Judy McMeekin, Pharm.D., “Products marketed with unidentified ingredients may be dangerous and, in some cases, deadly to consumers. We encourage consumers to remain vigilant when shopping online or in stores to avoid purchasing products that put their health at risk, and instead seek effective, FDA-approved treatments.”
Today’s warning letters outline how companies violated federal law by selling active drug ingredients in products marketed as foods, like honey, and by making unauthorized claims that their products treat disease or improve health. These products are promoted and sold for sexual enhancement on various websites and online marketplaces, and possibly in some retail stores.
The warning letters were issued to:
- Thirstyrun LLC (also known as US Royal Honey LLC),
- MKS Enterprise LLC,
- Shopaax.com,
- 1am USA Incorporated dba Pleasure Products USA
Companies marketing food products containing tadalafil and/or sildenafil violate federal law. Some of the products cited in the warning letters are also unapproved new drugs because they are intended for use in the cure, mitigation, treatment, or prevention of disease and they lack FDA approval. In some cases, product claims reference diseases that can only be diagnosed or treated under medical supervision. Additionally, some products cited in the warning letters are represented as dietary supplements even though tadalafil and sildenafil products are excluded from the dietary supplement definition.
The FDA has requested responses from the companies within 15 working days stating how they will address these issues or providing their reasoning and supporting information as to why they think the products are not in violation of the law. Failure to promptly address the violations may result in legal action, including product seizure and/or injunction.
Consumers using or considering using any over-the-counter product marketed for sexual enhancement should talk to a health care professional first, as some ingredients may interact with medications or dietary supplements. The FDA’s health fraud products database can help consumers identify nearly 1,000 of these potentially dangerous products.
The FDA previously warned consumers about more than 10 honey-based products containing hidden drug ingredients. The FDA’s laboratory testing found that product samples contained undeclared active ingredients, including sildenafil and tadalafil. The agency also previously warned consumers to avoid products with hidden drug ingredients sold through Amazon, eBay, Walmart and other retailers. The FDA is committed to protecting consumers by identifying and removing these potentially dangerous products from the market and urges stores, websites, and online marketplaces to stop selling these products.
If a consumer thinks that a product might have caused a reaction or an illness, they should immediately stop using the product and contact their health care provider. The FDA also encourages health care providers and consumers to report adverse reactions associated with FDA-regulated products to the agency using MedWatch or the Safety Reporting Portal.
Look what I found on Facebook:
Learn how to offer the healing energy of Reiki to yourself, people, and animals while enhancing your animal connection skills!
From daily support for health or challenges during times of crisis, Reiki helps restore balance on physical, emotional, spiritual, and mental levels for all living beings, enabling the body to do what it does best—heal itself. These benefits extend to other people, animals, trees/plants, and self-healing.
Reiki offers so many benefits for animals and for their human caregivers that I call it the gift that keeps on giving!
Reiki also enables students to connect and communicate more deeply with animals. If you think animals like you now, wait until they discover you’ve got Reiki—you’ll become an animal magnet!
For 25+ years Reiki has blessed me, my animal companions, students, and as a teacher I love sharing those benefits with as many people and animals as possible.
AVAILABLE WORLDWIDE
For many years I’ve taught a LIVE personally-mentored 6-week audio class where students learn all the basic skills needed by a beginning Reiki practitioner in addition to foundational principles of energy healing. And you don’t even need to leave the comfort of your home!
TAKEN REIKI BEFORE but don’t feel confident? Students who have retaken Reiki with me share that the weekly calls, opportunities to practice, online community, and opportunity to ask questions and receive guidance have helped them make Reiki a part of their daily lives and feel confident in offering it to loved ones.
REIKI LEVEL 1 CLASS SERIES
August 3 – September 7, 2022
LIVE WEEKLY CALLS and PERSONAL MENTORING
Every Wednesday at 6:00 p.m. Pacific for six weeks. Each call will be recorded and available for replay for students, including those in other time zones/countries. You do not have to attend live to take this class.
In addition to the 60-90 minute weekly calls, each student receives handouts and personal guidance for practice sessions.
When the class concludes, and all requirements have been fulfilled, each student receives a Reiki Level 1 certificate.
To learn more or register:

AND NOW FOR THE IMPORTANT BIT:
Choose one payment for all six classes. Payment is available with Visa, MC, or PayPal (choose PayPal credit card option for payment with Amex or Discover). PayPal also offers a payment plan option. Confirmation will be sent after registration along with instructions on how to join the first call. If you were unable to register in time to attend the first class live you can very easily catch up with the replay. Final deadline for registration is the day of the second class.
Single Pay Plan: $249.00
____________________________
This seems like a good little earner to me!
Congratulations to whoever invented it.
Yet I do feel that something has been forgotten:
the evidence.
If you search for Reiki on Pubmed, you find a baffling array of papers many of which arrive at positive conclusions. If you then check out the primary studies, you realize that most of them are of extremely poor quality, published by members of the Reiki cult (often in 3rd class journals for the nursing professions). If you search for independent systematic reviews that adequately account for the quality of the primary studies, you discover that, in fact, the evidence does not support the notion that Reiki is effective for anything. Here are a few examples:
- There is insufficient evidence to say whether or not Reiki is useful for people over 16 years of age with anxiety or depression or both.
- The serious methodological and reporting limitations of limited existing Reiki studies preclude a definitive conclusion on its effectiveness.
- In total, the trial data for any one condition are scarce and independent replications are not available for each condition. Most trials suffered from methodological flaws such as small sample size, inadequate study design and poor reporting.
And what about Reiki for animals?
As far as I can see, there is no good evidence at all.
So, does this render the above and similar courses fraudulent?
I let you answer this question for yourselves.
The UK Chiropractic Council is inviting you to help them re-formulate their educational standards. It is an occasion, some of my readers might find interesting. I, therefore, copy the relevant part of their announcement:
… Following a scoping review in 2021, which determined that the existing Education Standards, published in 2017, required development and updating, the GCC began revising the Education Standards in January 2022.
The revision will ensure that the Education Standards:
- Provide a realistic and comprehensive set of outcomes to be met by graduates on approved qualifications, demonstrating an ability to practise in accordance with the GCC Code.
- Take into account developments within the profession, increase focus on multi-disciplinary learning and different professions working more closely together across the UK, ensuring that graduates are well placed to meet the opportunities to care for patients in different contexts.
- Remain consistent, as appropriate, with the outcomes set by other UK healthcare frameworks and standards.
Purpose: why we are consulting
This consultation sets out our draft Education Standards for providers and Learning Outcomes for students, which reflect and build on the evidence and feedback we have obtained through our scoping review.
We seek stakeholders’ views on these draft Education Standards to ensure our final proposals are future-proof and fit for purpose.
We welcome all responses to the consultation.
Documents
The draft Education Standards on which we invite comments.
The equality impact assessment of the Education Standards, with comments invited within the consultation.
The GCC Education Standards consultation document in Word format.
Ways to respond
Submissions to this consultation can be made online (see below) or by email at [email protected] (click here to download the consultation document).
It is advisable to make a copy of your submission to prevent the loss of information due to internet, portal or connectivity issues. This should be done before pressing the submit button.
Information in responses, including personal information, may need to be published or disclosed under the access to information regimes (mainly the Freedom of Information Act 2000, the General Data Protection Regulation, the Data Protection Act 2018, and the Environmental Information Regulations 2004).
The GCC is a data controller registered with the Information Commissioner’s Office. We use personal data to support our work as the regulatory body for chiropractors. We may share data with third parties to meet our statutory aims and objectives, and when using our powers and meeting our responsibilities.
Closing date
The deadline for responses to this consultation on the draft Education Standards is 16 September 2022 at noon. The consultation will be publicised and stakeholders will be invited to comment…
_________________
Personally, I think the GCC desperately needs to improve its educational (and other) standards. They claim that, “as the regulator for chiropractors, our role is to protect the public”. The case of the late John Lawler is one of many examples to show how unfit for this purpose the GCC truly is.
So, perhaps you might want to contribute to the consultation with a view to making UK chiropractors less of a danger to the public?
HISC (HOMEOPATHY IN THE SUSSEX COMMUNITY) was formed in 2011 and has established effective partnerships with organisations that support those in need. Projects include working with domestic and sexual violence charities as well as supporting people recovering from long-term and enduring mental health illness issues. They enable vulnerable and marginalised members of the Sussex community to access low cost treatment with highly experienced homeopaths.
On 22 July, HISC made the following announcement:
Homeopathy in the Sussex Community (HISC) has been awarded a grant from The National Lottery Community Fund to provide homeopathy to survivors of domestic abuse and sexual violence.
HISC works in partnership with Sussex-based organisations; RISE, and Survivors Network, offering long-term and low-cost homeopathic support to women who have experienced abuse and sexual violence.
This grant will fund these projects for the next year, allowing HISC to build on the valuable work already being done and reaching even more vulnerable women who want access to homeopathic support.
Society Fellow Caroline Jurdon and Registered members Michael Bird, Therese Eriksen, Tara Lavelle and Jo Magowan have all worked on the project with colleagues from the wider community. HISC received one of the Society of Homeopath’s Community Clinic awards in 2018.
HISC also offer volunteering and sitting in opportunities for students.
_________________________
The ‘National Lottery Community Fund’ make the following points on their website:
- “Our funding is public money. This means that it cannot be used to give organisations an unlawful advantage.”
- “We fund projects that support people and communities across the UK to thrive.”
I would argue that, for the following reasons, the award is misplaced:
- Public money should not be wasted. It must be invested in projects that have a reasonable chance to do more good than harm.
- A broad consensus exists today that homeopathy has no effect beyond placebo. In fact, the NHS has stopped funding homeopathy and states that “there’s been extensive investigation of the effectiveness of homeopathy. There’s no good-quality evidence that homeopathy is effective as a treatment for any health condition.”
- Homeopathy can endanger lives. If people are misled into believing that it is effective and thus treat serious conditions with homeopathy, they needlessly prolong their suffering or, in the worst case scenario, hasten their death. Awards of the above nature can undoubtedly have this effect.
In my view, this means that the award given to HISC by the National Lottery Community Fund gives an unlawful advantage to an organisation promoting a bogus therapy. At best, it is a waste of public funds, at worst it causes serious harm.
Surely, women who have experienced abuse and sexual violence deserve better!
I have been warning the public about the indirect dangers of so-called alternative medicine (SCAM) for a very long time. It is now 25 years ago, for instance, that I published an article in the ‘European Journal of Pediatrics’ entitled “The attitude against immunisation within some branches of complementary medicine“. Here is the discussion section of this paper:
… certain groupings within COMPLEMENTARY MEDICINE (CM) may advise their patients against immunisation. Within these groupings, there is, of course, a considerable diversity of attitudes towards immunisation. Therefore
generalisations are difficult and more detailed investigations are required to clarify the issue.
The question arises whether the level of advice against immunisation as it exists today represents a real or only a potential risk. One study from the U.K. demonstrates homoeopathy to be the most prevalent reason for non-compliance with immunisation [30]. The problem may not be confined to naturopathy, chiropractic and homoeopathy. Books relating to CM in general [e.g. 19] also strongly advise against immunisation: “Vaccination may provoke the illness which it is supposed to prevent. People who are vaccinated can transmit the illness, even if they are not ill themselves. The vaccine can make the person more susceptible to the illness … The vaccinated child is a contaminated child”.
At present, our data is insufficient to de®ne which proportion of which complementary practitioners share this
attitude. The origin of this stance against vaccination is largely unknown. For instance, there is nothing in Hahnemann’s writings against immunisation [14]. It may therefore stem from a general antipathy toward modern medicine which seems to be prevalent within CM [7, 19, 23]. A more specific reason is that immunisation is viewed as detrimental, burdened with long-term side effects. It is also felt that it is not fully effective and unnecessary because
better methods of protection exist within CM [16].
Anti-immunisation activists are often unable to argue their case rationally, yet they place advertisements in the daily press warning about immunisation. In Britain, one tragic case has recently been publicised. A physician advised parents against measles vaccination for their child who was suspected of suffering from convulsions. Five years later, the child suffered severe brain damage after contracting measles. The doctor was sued by the parents and found guilty of negligence and ordered to pay £825,000 in damages [1].
In medicine we must, of course, always be vigilant about the risks of our interventions. Each form of immunisation should therefore be continuously scrutinised for its possible risks and benefits. Most forms of immunisation are clearly not entirely free of risk [e.g. 22] – in fact, no effective intervention will ever be entirely risk-free. Therefore the risks have to be discounted against the benefits. It follows that any blanket rejection of immunisation, in general, must be misleading. It endangers not only the individual patient but (if prevalent) also the herd immunity of the community at large. Such unreflected rejection of immunisation, in general, will inevitably do more harm than good.
It is concluded that the advice of some, by no means all complementary practitioners in relation to immunisation represents an area for concern, which requires further research. Complementary practitioners and patients alike should be educated about the risks and benefits of immunisation. Paediatricians should be informed about the present negative attitude of some complementary practitioners and discuss the issue openly with their patients.
_____________________________
I suspect that, had we heeded my caution, researched the subject more thoroughly, and taken appropriate action, the current pandemic might have produced fewer and less vocal anti-vaxxers, and fewer patients might have died.
The US Food and Drug Administration (FDA) state that dietary supplements can help people improve or maintain their overall health. But they may also come with health risks. Whether you’re a consumer of dietary supplements or it’s your job to inform and educate, it’s important to know the facts before deciding to take any dietary supplement.
Therefore, they launched the initiative, “Supplement Your Knowledge”. It aims to help inform health care professionals, consumers, and educators about dietary supplements.
“Dietary supplements can be valuable to your health but taking some supplements can also involve health risks,” Douglas Stearn, JD, deputy director for regulatory affairs in the FDA’s Center for Food Safety and Applied Nutrition, said in a statement. “These Supplement Your Knowledge resources will help provide consumers and health care professionals with facts to make informed decisions when determining if they want to use or recommend dietary supplements.”
In collaboration with the American Medical Association, publisher of JAMA, the FDA has developed a free continuing medical education program for physicians and other health care professionals about the regulation of dietary supplements, informing patients about their use, and reporting adverse events to the agency. The program includes 3 videos and accompanying educational materials. It is available on the FDA website and the AMA Ed Hub.
________________________
The objectives of the program are:
1. Define dietary supplements
2. Describe how dietary supplements are regulated
3. Describe how dietary supplements are labelled and the types of claims permitted
4. Review potential interactions of dietary supplements with other supplements, medications, and laboratory tests
5. Identify adverse events and how to report them to FDA
Even though some parts of the program are quite specific to the US, I think that the initiative is most laudable and an excellent resource for physicians, SCAM practitioners, consumers, and decision-makers to learn more about this important subject.