evidence
Despite considerable doubts about its effectiveness, osteopathic manipulative treatment (OMT) continues to be used for a range of pediatric conditions. Here is just one example of many osteopaths advertising their services:
I qualified as an Osteopath in 2009 after 4 years of intensive training from the British College of Osteopathic medicine, where I received a distinction for my efforts. After having two children I decided to do a 2-year Postgraduate training in Pediatric Osteopathy from the Osteopathic Centre for Children in London. Whilst at the centre I was lucky enough to meet a wide variety of children from premature babies in a Neonate Hospital ward to children with developmental issues and disabilities, children on the Autistic spectrum, to kids doing exams or experiencing high levels of stress. We also saw lots of children with normal coughs, colds, lumps and bumps.
And the ‘Institute of Osteopathy states this:
Parents visit osteopaths for a range of reasons to support their child’s health. Children, like adults, can be affected by general joint and muscle issues, which is one of the reasons people visit an osteopath. Parents will also take their children to visit an osteopath for a variety of other health reasons that may benefit from osteopathic care.
As osteopathic care is based on the individual needs of the patient, it will vary depending on your child’s age and the diagnosis. Osteopaths generally use a wide range of gentle hands-on techniques that focus on releasing tension, improving mobility and optimising function. This is often used together with exercise and helpful advice. Some osteopaths have been trained in very gentle techniques which are particularly suitable to assess and treat very young children, including new-borns. You do not need to consult your GP before you visit an osteopath, although you may wish to do so.
So, how good or bad is osteopathy for kids? Our systematic review wanted to find out. Specifically, the aim of this paper is to update our previous systematic review (SR) initially published in 2013 by critically evaluating the evidence for or against this treatment.
Eleven databases were searched (January 2012 to November 2021). Only randomized clinical trials (RCTs) of OMT in pediatric patients compared with any type of controls were considered. The Cochrane risk-of-bias tool was used. In addition, the quality of the evidence was rated using Grading of Recommendations, Assessment, Development and Evaluation (GRADE) criteria, as recommended by the Cochrane Collaboration.
Thirteen trials met the eligibility criteria, of which four could be subjected to a meta-analysis. The findings show that, in preterm infants, OMT has little or no effect on reducing the length of hospital stay (standardized mean difference (SMD) -0.03; 95% confidence interval (CI) -0.44 to 0.39; very low certainty of the evidence) when compared with usual care alone. Only one study (8.3%) was judged to have a low risk of bias and showed no effects of OMT on improving exclusive breastfeeding at one month. The methodological quality of RCTs published since 2013 has improved. However, adverse effects remain poorly reported.
We concluded that the quality of the primary trials of OMT has improved during recent years. However, the quality of the totality of the evidence remains low or very low. Therefore, the effectiveness of OMT for selected pediatric populations remains unproven.
These days, it is not often that I am the co-author of a systematic review. So, allow me to discuss one of my own papers for a change by making a few very brief points:
- Considering how many osteopaths treat children, the fact that only 13 trials exist is shameful. To me, it suggests that the osteopathic profession has little interest in research.
- The finding that adverse effects are poorly reported is even more shameful, in my view. It suggests that the few osteopaths who do some research don’t mind violating research ethics.
- The fact that overall our review fails to yield good evidence that osteopathy is effective for any pediatric condition is the most shameful finding of them all. It means that osteopaths are either not informed about the evidence for their own approach, or that they are informed but don’t give a hoot and treat kids regardless. In both cases, they behave unethically.
Cannabis use is a frequently-discussed subject, not just in the realm of so-called alternative medicine (SCAM). In general, SCAM advocates view it as an herbal medicine and recommend it for all sorts of conditions. They also often downplay the risks associated with cannabis use. Yet, these risks might be substantial.
Cannabis potency, defined as the concentration of Δ9-tetrahydrocannabinol (THC), has increased internationally, which could increase the risk of adverse health outcomes for cannabis users. The first systematic review of the association of cannabis potency with mental health and addiction was recently published in ‘The Lancet Psychiatry’.
The authors searched Embase, PsycINFO, and MEDLINE (from database inception to Jan 14, 2021). Included studies were observational studies of human participants comparing the association of high-potency cannabis (products with a higher concentration of THC) and low-potency cannabis (products with a lower concentration of THC), as defined by the studies included, with depression, anxiety, psychosis, or cannabis use disorder (CUD).
Of 4171 articles screened, 20 met the eligibility criteria:
- eight studies focused on psychosis,
- eight on anxiety,
- seven on depression,
- and six on CUD.
Overall, higher potency cannabis, relative to lower potency cannabis, was associated with an increased risk of psychosis and CUD. Evidence varied for depression and anxiety. The association of cannabis potency with CUD and psychosis highlights its relevance in healthcare settings, and for public health guidelines and policies on cannabis sales.
The authors concluded that standardisation of exposure measures and longitudinal designs are needed to strengthen the evidence of this association.
The fact that cannabis use increases the risk of psychosis has long been general knowledge. The notion that the risk increases with increased potency of cannabis seems entirely logical and is further supported by this systematic review. Perhaps it is time to educate the public and make cannabis users more aware of these risks, and perhaps it is time that SCAM proponents negate the harm cannabis can do.
Reports of serious complications of chiropractic manipulation keep on coming. Take this one, for instance:
My daughter went for a routine chiropractor appointment. Now she’s paralysed – 1:20 000 chiropractic neck manipulations result in stroke from vertebral artery dissection.
Or take a recent article by US neurosurgeons:
Cranio-cervical artery dissection (CeAD) is a common cause of cerebrovascular events in young subjects with no clear treatment strategy established. This study evaluated the incidence of major adverse cardiovascular events (MACE) in CeAD patients treated with and without stent placement. COMParative effectiveness of treatment options in cervical Artery diSSection (COMPASS) is a single high-volume center observational, retrospective longitudinal registry that enrolled consecutive CeAD patients over a 2-year period. Patients were ≥ 18 years of age with confirmed extra- or intracranial CeAD on imaging. Enrolled participants were followed for 1 year evaluating MACE as the primary endpoint.
One-hundred ten patients were enrolled (age 53 ± 15.9, 56% Caucasian, and 50% male, BMI 28.9 ± 9.2). Grade I, II, III, and IV blunt vascular injury was noted in 16%, 33%, 19%, and 32%, respectively. Predisposing factors were noted in the majority (78%), including
- sneezing,
- carrying a heavy load,
- chiropractic manipulation.
Stent was placed in 10 (10%) subjects (extracranial carotid n = 9; intracranial carotid n = 1; extracranial vertebral n = 1) at the physician’s discretion along with medical management. Reasons for stent placement were early development of high-grade stenosis or expanding pseudoaneurysm. Stented patients experienced no procedural or in-hospital complications and no MACE between discharge and 1 year follow up. CeAD patients treated with medical management only had 14% MACE at 1 year.
The authors concluded that in this single high-volume center cohort of CeAD patients, stenting was found to be beneficial, particularly with development of high-grade stenosis or expanding pseudoaneurysm. These results warrant confirmation by a randomized clinical trial.
Yes, I know: this study was not meant to investigate the link between chiropractic manipulations and CeAD. The finding that chiropractic manipulation is a predisposing factor for CeAD is entirely incidental. But it is an important finding nevertheless.
Chiropractors will laugh about the notion that manipulation is a risk factor akin to sneezing and thus try to trivialize the danger of their treatments. I would then point out that sneezing is unavoidable and fulfills a purpose. Chiropractic manipulations do neither.
Placebo effects are a fascinating subject. In so-called alternative medicine (SCAM), they are particularly important because much of SCAM seems to rely on little more than placebo effects. Therefore, I think this new paper is of some relevance to us.
The aim of this systematic review was to quantify the placebo effect of intraarticular injections for knee osteoarthritis in terms of pain, function, and objective outcomes. Factors influencing placebo effect were investigated.
Out of 2,363 records, 50 articles on 4,076 patients were included. The meta-analysis showed significant improvements up to the 6-month follow-up: Visual Analogue Scale (VAS)-pain −13.4 mean difference (MD) (95% confidence interval [CI]: −21.7/−5.1; P < 0.001), Western Ontario and McMaster Osteoarthritis Index (WOMAC)-pain −3.3 MD (95% CI: −3.9/−2.7; P < 0.001). Other significant improvements were WOMAC-stiffness −1.1 MD (95% CI: −1.6/−0.6; P < 0.001), WOMAC-function −10.1 MD (95% CI: −12.2/−8.0; P < 0.001), and Evaluator Global Assessment −21.4 MD (95% CI: −29.2/−13.6; P < 0.001). The responder rate was 52% (95% CI: 40% to 63%). Improvements were greater than the “minimal clinically important difference” for all outcomes (except 6-month VAS-pain). The level of evidence was moderate for almost all outcomes.
The authors concluded that the placebo effect of knee injections is significant, with functional improvements lasting even longer than those reported for pain perception. The high, long-lasting, and heterogeneous effects on the scales commonly used in clinical trials further highlight that the impact of placebo should not be overlooked in the research on and management of knee osteoarthritis.
The authors furthermore confirmed that “the main finding of this meta-analysis is that placebo is an important component of the effect of injective treatments for patients with KOA, with saline injections being able to provide relevant and long-lasting results not only in terms of pain relief but also with respect to stiffness resolution and function improvement. These results are both statistically and clinically significant and can be perceived by patients up to 6 months.”
I would dispute that!
To explain why it might help to read our 1995 BMJ paper on the subject:
We often and wrongly equate the response seen in the placebo arm of a clinical trial with the placebo effect. In order to obtain the true placebo effect, other non-specific effects can be identified by including an untreated control group in clinical trials. A review of the literature shows that most authors confuse the perceived placebo effect with the true placebo effect. The true placebo effect is highly variable, depending on several factors that are not fully understood. A distinction between the perceived and the true placebo effects would be helpful in understanding the complex phenomena involved in a placebo response.
In other words, what the authors picked up in their analysis (i.e. the changes that occurred in the placebo groups between the start of a trial and after placebo application) is not just the placebo response; it is, in fact, a combination of a placebo effect, concomitant interventions/care, regression towards the mean, natural history of the condition and possibly other factors.
Does it matter?
Yes, it does!
Placebo effects are not nearly as powerful and long-lasting as the authors conclude. And this means virtually all their implications for clinical practice are incorrect.
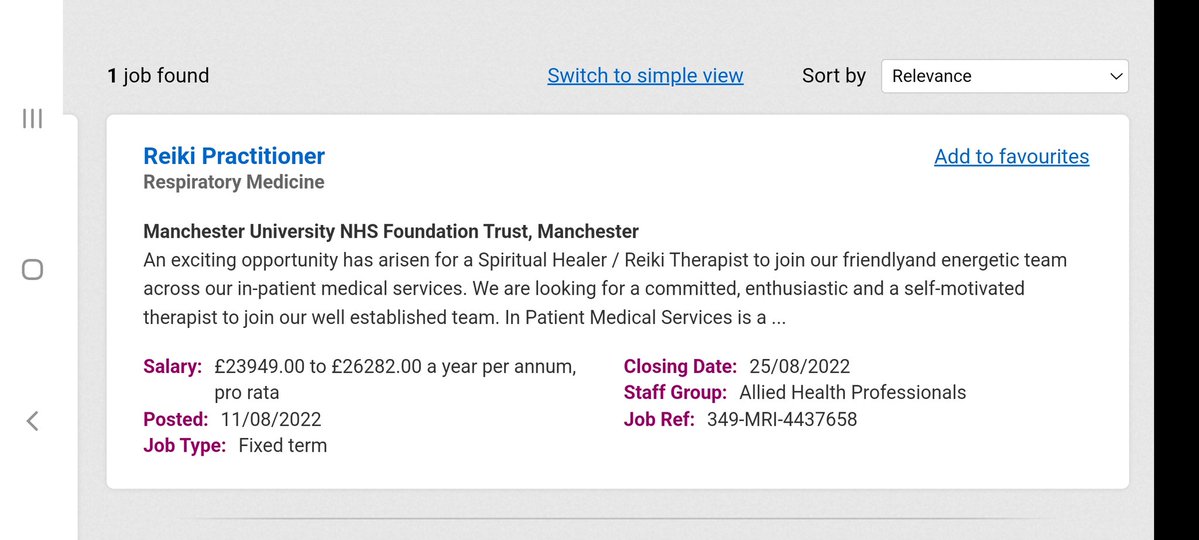
It has been reported by several sources that the NHS is advertising for a Reiki healer.
The NHS stated that “the responsibilities of a reiki healer include treating clients using energy principles … and activating the healing process.” The post is paid for by the Sam Buxton Sunflower Healing Trust (SBSHT) which states on its website:
The SBSHT healing therapists, who work within the NHS and other health areas, are proud to be part of a multi-disciplinary team of professionals to provide vital support cancer patients, their relatives and staff. Since 2006, the SBSHT has funded healers to work in NHS, and other health related areas to support cancer patients and their families. A key role of the SBSHT is to increase awareness within the UK of the importance of providing healing support to cancer patients and families. Another vital role is to generate the crucial funds needed to place more healers in NHS, and other health related areas, throughout the country. Complementary therapy (CT) is increasingly demanded and expected by patients undergoing cancer treatments. An increasing amount of research clearly demonstrates that CT is important to support patients through their conventional treatments. SBSHT is committed to providing funds to NHS hospitals and cancer centers to engage the services of a Reiki practitioner or Healer for cancer patients and their families
As a charity we are or have funded healer posts within the centres below.
- University College Hospital, London
- Addenbrookes Hospital, Cambridge
- Princess Alexandra Hospital, Epping
- Queen Elizabeth Hospital, Welwyn Garden City
- Derriford Hospital, Plymouth
- Wigan NHS Trust, Wigan
- St Josephs Hospice, London
- Eden Valley Hospice and Jigsaw Children’s Hospice, Carlisle
- St Mary’s Hospice, Ulverston and Barrow in Furness NHS Trust
- St Johns Hospice, Lancaster
- Kent and Canterbury Hospital, Canterbury
- Bristol Haematology and Oncology Centre, Bristol
- Rowcroft Hospice, Torquay
- The Lister Hospital, Stevenage
- Barnstaple NHS Trust
- Treliske Hospital, Cornwall
- Poole NHS Trust
- St Michaels Hospice, Herefordshire
The SBSHT was co-founded by Angie Buxton-King in memory of her son Sam, who died of Acute Myeloid Leukaemia in 1998 aged 10. She is a member of the ‘College of Psychic Studies’ which is “committed to serving the evolution of consciousness”. The College website states this:
We were founded in 1884 to support and encourage empirical research into the esoteric. Our programme has since broadened and diversified to meet rising demand and increasingly global interests.
However, our core values remain the same. We continue to shine a light on key themes including consciousness, intuition, self-development and meditation. Our courses, workshops, talks and special events provide a safe and inclusive space in which to explore the full spectrum of human potential under the careful guidance of our expert tutors.
The College offers all sorts of courses; I was particularly fascinated by this one: “Alchemise Your Energy Through Dowsing“.
__________________
Now, one could easily claim that there is nothing wrong with reiki healers invading the NHS; after all, they are funded by a charitable trust at no cost to the taxpayer.
Yet, I disagree!
Reiki healing is implausible and ineffective nonsense. As such it is by no means harmless. Employing such healers in the NHS sends out a strong signal that undermines the principles of rational thinking and evidence-based medicine. If the NHS truly does not value these principles, I suggest they also fill the chronic gaps in ambulance services by flying carpets.
DIARALIA is a homeopathic remedy for the symptomatic treatment of acute transient diarrhea. It is produced by Boiron, the world’s largest manufacturer of homeopathic remedies. This is how it is currently advertised:
Instructions DIARALIA
Dosage DIARALIA
Adults and children from 6 years
Lozenge 1, 4 to 6 times a day, for a maximum of three days of treatment.
Discontinue treatment as soon as symptoms disappear.
Method and route of administration DIARALIA
Sublingual (tablet to dissolve under the tongue)
In children 18 months to 6 years: dissolve the tablet in a little water before use, because of the risk of aspiration. As soon as the permitted age, dissolve the tablets under the tongue.
Duration of treatment DIARALIA
The duration of treatment should not exceed one week.
In case of overdose DIARALIA
If you have taken more DIARALIA orodispersible tablets that you don” should have:
Consult your doctor or pharmacist immediately.
In case of failure of one or more doses of DIARALIA
If you miss a dose of DIARALIA orodispersible tablets:
Do not take a double dose to make up for the dose that you forgot to take
Pregnancy and lactation with DIARALIA
Ask your doctor or pharmacist before taking any medicine.
In the absence of experimental and clinical data, and as a precautionary measure, the use of this drug should be avoided during pregnancy and lactation.
Composition DIARALIA
Excipients with known effect: This medicinal product contains lactose,
Active substances:
For a 300 mg tablet
Arsenicum album 9CH 1mg
China rubra 5CH 1mg
Podophyllum peltatum 9 CH 1mg
Excipients: sucrose, lactose monohydrate, magnesium stearate
Cons-indication DIARALIA
N” Never use DIARALIA orodispersible tablets:
· In children under 18 months.
· If you are allergic (hypersensitive) to the active substances or to any of the ingredients in CORYZALIA orodispersible tablets.
Possible interactions with DIARALIA
If you are taking or have recently taken any other medicines, including medicines obtained without a prescription, talk to your doctor or pharmacist.
This medication is to be taken between meals.
Adverse DIARALIA
Like all medicines, DIARALIA orodispersible tablets may cause side effects, although not everybody will not matter.
If you notice any side effects not listed in this leaflet, or if the side effects gets serious, please tell your doctor or pharmacist.
Storage conditions DIARALIA
Store at a temperature not exceeding 30 ° C
Precautions and warnings DIARALIA
This medication should not be used in case of vomiting, high fever, blood in the stool.
Any significant diarrhea exposed to the risk of dehydration requiring appropriate rehydration.
If diarrhea persists beyond 3 days, a medical consultation is necessary.
If your doctor has told you have an intolerance to some sugars, contact your doctor before taking this medicine
Use of this medicine is not recommended in patients with galactose intolerance, a Lapp lactase deficiency or malabsorption syndrome glucose or galactose (rare hereditary diseases).
But is there any evidence that DIARALIA works?
I’m glad you asked!
I looked far and wide but found none (if a reader knows of a clinical trial, please let me know).
Jenifer Jacobs (JJ) published a review of 3 studies – all her own! – and concluded that the results from these studies confirm that individualized homeopathic treatment decreases the duration of acute childhood diarrhea and suggest that larger sample sizes be used in future homeopathic research to ensure adequate statistical power. Homeopathy should be considered for use as an adjunct to oral rehydration for this illness. So, some homeopathy fans might claim there is good evidence. But I dispute that.
- Firstly, there are good reasons to distrust these conclusions.
- Secondly, there are good reasons to doubt that JJ is a reliable researcher.
- Thirdly, JJ used INDIVIDUALIZED homeopathy and not DIARALIA.
We all know, of course, that diarrhea can be a symptom of a range of serious conditions. Thus, one should not joke about it. On the contrary, one should diagnose the reason for the symptom and treat it adequately. And one should certainly not advertise unproven treatments for it; one could even go one step further and claim that anyone who does that is fraudulently endangering the health of the often all too gullible consumer.
Trevor Zierke is a D.C. who published several videos that have gone viral after saying that “literally 99% of my profession” is a scam. “When I say almost all the usual lines chiropractors tell you are lies, I mean almost all of them,” he stated. Zierke then went on to give examples of issues chiropractors allegedly make up, including someone’s spine being “misaligned,” tension on nerves causing health problems, and someone having back pain because their hips are off-center. “Almost all of these aren’t true,” he concluded.
In a follow-up video, he claimed that the reasons most people are told they need to go to a chiropractor are “overblown or just flat out lies proven wrong by research.” He also noted that, while there are many scams, that “doesn’t mean you can’t get help from a chiropractor.”
In a third TikTok video, Zierke offered some valid reasons to see a chiropractor. He said that one can seek help from a chiropractor if one has musculoskeletal pain that has been ongoing for more than one to two days, and that’s about it. He stated that issues that a chiropractor couldn’t really fix include “GI pain, hormonal issues, nutrition,” among others.
In comments, users were largely supportive of Zierke’s message.
One said: “As a physiotherapist, I’ve been trying to tell this but I don’t want to like offend any chiropractor in doing so,” a commenter shared.
“Working in a chiropractic office, this is fair,” a further user wrote. “I have issues that I know an adjustment will help & other pain that would be better stretched/released.”
In an email, Zierke reiterated the intention of his videos: “I would just like to clarify that chiropractors, in general, are not a scam or are inherently scammers (I myself am a practicing chiropractor), but rather a lot of very popular sales tactics, phrases, and wording used to imply patients need treatment, and methods of treatment, have never been proven to be true,” he explained. “When chiropractors say & use these methods stating things that are not factually true—I believe it’s scammy behavior and practices. There are still a lot of very good, honest, and integral chiropractors out there,” he concluded. “They can provide a lot of help and relief to patients. But that’s unfortunately not the majority, and I’ve heard too many stories of people falling victim to some of these scam-like tactics from bad apple chiropractors.”
None of what DC Zierke said can surprise those who have been following my blog. On the contrary, I could add a few recent posts to his criticism of chiropractic, for example:
- Pediatric chiropractic seems to be on the rise
- Catastrophic injuries after chiropractic treatment
- Chiropractic: “a safe form of treatment”?
- Malpractice Litigation Involving Chiropractic Spinal Manipulation
- Best Practices for the Chiropractic Care of Children
- No effect from adding chiropractic manipulations to exercises for neck pain
- Hurray! The new professional standard by the General Chiropractic Council protects UK chiropractors
- Manual therapy (mainly chiropractic and osteopathy) does not have clinically relevant effects on back pain compared with sham treatment
- Chiropractic Paediatric Courses … it is high time to stop this dangerous nonsense
- Chiropractic ‘subluxation’ is by no means a notion of the past
- Another indirect risk of chiropractic
- And again: chiropractic for infant colic
- Chiropractic misinformation during the COVID-19 pandemic
- The lack of chiropractic ethics: “valid consent was not obtained in a single case”
I rest my case.
About a year ago, I reported last on the situation of homeopathy in France. Now it might be time for another update. The end of the reimbursement of homeopathy was, of course, a heavy blow for the laboratories concerned, especially Boiron and Weleda.
Are these firms now going bust?
Is the French public missing homeopathy?
The cessation of reimbursement took place in two steps: in 2020, the reimbursement rate was reduced to 15 % and expired completely in 2021. The new director of Weleda France, Ludovic Rassat, explains that, in 2020, when the reimbursement was reduced to 15 %, the impact on sales was just 20 %. The decrease was limited because of the supplementary health insurance which 80 % of French people have still supplemented the reimbursement up to 100 %. In 2021, this generosity stopped and the reimbursement fell from 100 to 0 %. This led to a 60 % drop in sales and to losses of 13 million Euros for Weleda France.
According to an Ipsos survey commissioned by Boiron Laboratories in October 2018, 70 % of all French used homeopathy to relieve their first symptoms, 74 % thought homeopathic remedies were effective and 71 % thought homeopathy was a good complement to conventional treatments. One might, therefore, have assumed that French consumers would continue using their beloved remedies despite the cessation of reimbursement. However, this was not the case. The most obvious explanation for this phenomenon, I think, is that the above-mentioned survey had generated false-positive results and that people correctly judged homeopathic remedies to be superfluous.
Faced with unsustainable losses, the French manufacturers of homeopathic products are now forced to react. A press release by Weleda France from 4 July 2022 stated that “This project would result in the discontinuation of pharmaceutical production and medical information in France and the closure of the Weleda division. This would result in the cessation of production activities at the Huningue site and an adjustment of the organisation of activities at headquarters. In total, 127 jobs could be cut at Weleda France.” If this step is taken as planned, Weleda France will have to earn its money purely on its cosmetic and anthroposophical products, according to the director.
In 2019, Laboratoires Boiron owned 4 production laboratories and 28 distribution facilities in France. In March 2020, the company announced that it had decided to cut 646 jobs in France and close 13 of its 31 sites, due to the poor economic results that followed the cessation of reimbursement of its products by the social security system. Following the decision by the Minister of Health, Agnès Buzyn, to stop the reimbursement of homeopathic preparations by the social security system, Boiron announced that the Montrichard site in the Loir-et-Cher region had not managed to find a buyer. As a result, the site, which employed around 80 people, closed on 31 December 2021.
And the French consumers?
Are they missing homeopathy?
Are they suffering from homeopathy withdrawal?
Are they more frequently ill without homeopathy?
Are they switching to more expensive conventional drugs?
I currently spend much of my time in France and cannot say that I have noticed any of this. On the contrary, most people I talk to are delighted that homeopathy is no longer reimbursed. But this is no evidence, of course. I am unable to find any reliable data to answer the above questions.
When the French health minister decided against homeopathy two years ago, she said: “It’s possible to leave the doctor’s office without a prescription! Let’s take advantage of this debate on homeopathy to reflect more broadly on our use of medicine. The ultimate goal is to consume less.” She was correct, it seems.
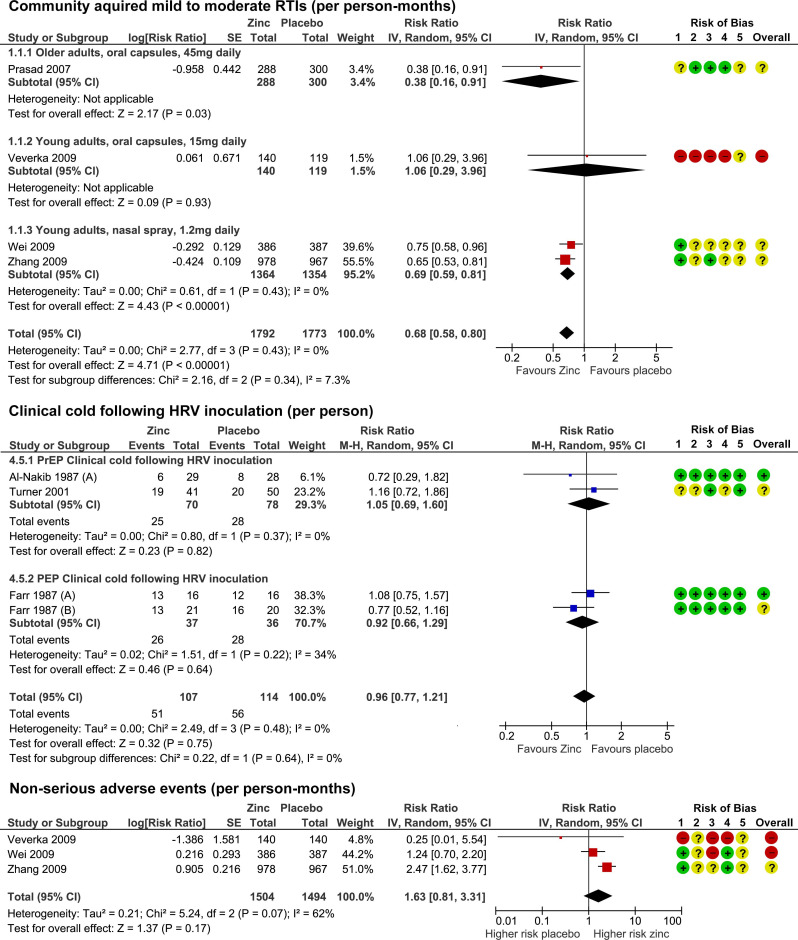
Zinc has been in the limelight recently. The reason is that it has been recommended as a preventative and/or treatment of COVID infections. The basis for such recommendations has been some trial evidence suggesting it is effective for viral respiratory tract infections (RTIs). But the evidence has been full of contradictions which means, we need a systematic review that critically evaluated the totality of the available data.
This systematic review was aimed at evaluating the benefits and risks of zinc formulations compared with controls for the prevention or treatment of acute RTIs in adults.
Seventeen English and Chinese databases were searched in April/May 2020 for randomized clinical trials (RCTs), and from April/May 2020 to August 2020 for SARS-CoV-2 RCTs. Cochrane rapid review methods were applied. Quality appraisals used the Risk of Bias 2.0 and Grading of Recommendations, Assessment, Development and Evaluation (GRADE) approach.
Twenty-eight RCTs with 5446 participants were identified. None were specific to SARS-CoV-2. Compared with placebo, oral or intranasal zinc prevented 5 RTIs per 100 person-months (95% CI 1 to 8, numbers needed to treat (NNT)=20, moderate-certainty/quality). Sublingual zinc did not prevent clinical colds following human rhinovirus inoculations (relative risk, RR 0.96, 95% CI 0.77 to 1.21, moderate-certainty/quality). On average, symptoms resolved 2 days earlier with sublingual or intranasal zinc compared with placebo (95% CI 0.61 to 3.50, very low-certainty/quality) and 19 more adults per 100 were likely to remain symptomatic on day 7 without zinc (95% CI 2 to 38, NNT=5, low-certainty/quality). There were clinically significant reductions in day 3 symptom severity scores (mean difference, MD -1.20 points, 95% CI -0.66 to -1.74, low-certainty/quality), but not average daily symptom severity scores (standardised MD -0.15, 95% CI -0.43 to 0.13, low-certainty/quality). Non-serious adverse events (AEs) (eg, nausea, mouth/nasal irritation) were higher (RR 1.41, 95% CI 1.17 to 1.69, NNHarm=7, moderate-certainty/quality). Compared with active controls, there were no differences in illness duration or AEs (low-certainty/quality). No serious AEs were reported in the 25 RCTs that monitored them (low-certainty/quality).
The authors concluded that in adult populations unlikely to be zinc deficient, there was some evidence suggesting zinc might prevent RTIs symptoms and shorten duration. Non-serious AEs may limit tolerability for some. The comparative efficacy/effectiveness of different zinc formulations and doses were unclear. The GRADE-certainty/quality of the evidence was limited by a high risk of bias, small sample sizes and/or heterogeneity. Further research, including SARS-CoV-2 clinical trials is warranted.
The authors provide a short comment on the assumed mode of action of zinc. The rationale for topical intranasal and sublingual zinc is based on the in vitro effects of zinc ions that can inhibit viral replication, stabilize cell membranes and reduce mucosal inflammation. Other conceivable mechanisms include the activation of T lymphocytes, monocytes, and granulocytes.
The authors also remind us to be cautious: clinicians and consumers need to be aware that considerable uncertainty remains regarding the clinical efficacy of different zinc formulations, doses, and administration routes, and the extent to which efficacy might be influenced by the ever changing epidemiology of the viruses that cause RTIs. The largest body of evidence comes from sublingual lozenges and zinc gluconate and acetate salts, suggesting these are suitable choices. Yet, this does not mean that other administration routes and zinc salts are less effective. The new evidence on the prophylactic effects of low-dose nasal sprays adds weight to the otherwise inconclusive findings from the handful of RCTs evaluating zinc nasal sprays or gels for acute treatment. A minimum therapeutic dose for zinc is also yet to be determined. An earlier review suggested the minimum dose for sublingual lozenges is 75 mg. However, the present analysis does not support this conclusion. Furthermore, a daily oral dose of 15 mg has been shown to upregulate lymphocytes within days, so it is plausible that much lower doses might also be effective.
It has been reported that a recent inspection from the Care Quality Commission (CQC) found that the diagnostic imaging service at AECC University College in Parkwood Road, Bournemouth, requires improvement in three out of four areas – including patient safety. This is surprising not least because the AECC prides itself on being “a leading higher education institution in healthcare disciplines, nationally and internationally recognised for quality and excellence.” 
The unannounced inspection in May this year resulted in several demands for the service to improve upon. For example, the CQC report said staff “did not receive all of the training they needed to keep patients safe” and that patient chaperones “did not receive chaperone training”. Moreover, managers were reported as not always ensuring staff were competent to operate certain equipment. In fact, there was no record of staff competencies which meant inspectors “could not tell if staff had been trained to use equipment”. General cleanliness was also found lacking in relation to certain procedures, namely no sink in any of the site’s nine ultrasound rooms (including those for transvaginal scans) – meaning staff carrying out ultrasound scanning did not have access to a clinical handwashing facility.
The CQC states on its website that it “is the independent regulator of health and adult social care in England. We make sure health and social care services provide people with safe, effective, compassionate, high-quality care and we encourage care services to improve. We monitor, inspect and regulate services. Then we publish what we find, including performance ratings, to help people choose care. Where we find poor care, we will use our powers to take action.”
No doubt, these are laudable aims. What I find, however, disappointing is that the CQC’s inspection of the AECC did not question the nature of some of the courses taught by the AECC. Earlier this year, I reported in a blog post that the AECC has announced a new MSc ‘Musculoskeletal Paediatric Health‘. This motivated me to look into the evidence for such a course. This is what I found with several Medline searches (date of the review on chiropractic for any pediatric conditions, followed by its conclusion + link [so that the reader can look up the evidence]):
2008
I am unable to find convincing evidence for any of the above-named conditions.
2009
Previous research has shown that professional chiropractic organisations ‘make claims for the clinical art of chiropractic that are not currently available scientific evidence…’. The claim to effectively treat otitis seems to
be one of them. It is time now, I think, that chiropractors either produce the evidence or abandon the claim.
2009
The … evidence is neither complete nor, in my view, “substantial.”
2010
2018
What seems to emerge is rather disappointing:
- There are no really new reviews.
- Most of the existing reviews are not on musculoskeletal conditions.
- All of the reviews cast considerable doubt on the notion that chiropractors should go anywhere near children.
But perhaps I was too ambitious. Perhaps there are some new rigorous clinical trials of chiropractic for musculoskeletal conditions. A few further searches found this (again year and conclusion):
2019
2018
I might have missed one or two trials because I only conducted rather ‘rough and ready’ searches, but even if I did: would this amount to convincing evidence? Would it be good science?
No! and No!
So, why does the AECC offer a Master of Science in ‘Musculoskeletal Paediatric Health’?
____________________