evidence
Max Gerson is well-known to experts in so-called alternative medicine (SCAM). After all, he invented the famous alternative cancer regimen, the Gerson therapy (previously discussed here, here, and here). Not that this treatment works – in fact, it is not just ineffective but also dangerous – but it has prominent promoters, not least King Charles III . As I say, Gerson is well known for his cancer quackery. What hardly anyone knows is that, before he dabbled in cancer, he invented an entirely different medicine.
. As I say, Gerson is well known for his cancer quackery. What hardly anyone knows is that, before he dabbled in cancer, he invented an entirely different medicine.
Max was born as the 3rd of 9 siblings into a Jewish family on October 18, 1881. They lived in Wongrowitz, a part of Poland that at the time belonged to Germany. Max went to school in his hometown and studied medicine in Breslau (Wrocław, now Poland), Wuerzburg, Berlin, and Freiburg. In 1909, he graduated from the University of Freiburg and began practicing medicine at age 28 in Breslau. During WWI, Gerson worked as a surgeon in a military hospital in Breslau and was awarded the ’Iron Cross’ for his service. In 1916, he married Gretchen Hope; the two had three daughters and stayed together until his death.
In 1918, the Gerson family moved to Bielefeld (Germany), and Max specialized in internal medicine as well as neurology. During this period, Gerson developed an anti-inflammatory drug combination and made contact with a local pharmaceutical firm, ‘ASTA Medica’. On the occasion of the firm’s recent 100th jubilee, a German newspaper reported: “The company did business with the well-known Bielefeld physician and inventor Dr. Max Gerson. At the time, he owned the prescription and trademark for a painkiller called Quadronal. Dr. Gerson became a silent partner.”[1] Remarkably, Gerson who published >50 papers (most in German) seems to have no publication on Quadronal.
In his biography of Gerson, Howard Straus (Max’s grandson), explained that Max Gerson did, in fact, develop not just Quadronal for ASTA but also another drug, Quadronox, which however was not as successful as Quadronal. Crucially, Straus makes it very clear that the drug company defrauded Gerson and “never paid a penny to him or his family, nor honored his early ownership of the shares in the company”.[2]
When I was a young clinician in Germany, Quadronal was still quite popular, and I prescribed it regularly. It had been unquestionably the main success for the multi-million firm, ASTA. Today, it is less in use or even no longer available (I am not sure, perhaps someone can fill me in). Gerson’s second drug, Quadronox, seems to have disappeared a long time ago.
I find this story interesting and potentially relevant to the history of Max Gerson. His time in Bielefeld ended when he fled the Nazis (many of his family were killed during the Holocaust). Eventually, Max, his wife, and their three daughters ended up in New York where Gerson tried to establish his anti-cancer regimen. He became fiercely anti-pharma, and many of his followers even claim that he died by being poisoned by the medico-pharmaceutical establishment which allegedly was afraid that his ‘highly successful’ cancer therapy would put them out of business. It is hard to resist the temptation of suspecting a connection between Gerson’s pharma-phobia and the unfair treatment Max received from ASTA in Bielefeld.
Obviously, my knowledge about all this is incomplete, and I would love to hear from people who know more about it.
[1] ASTA-Erfolgsgeschichte startet vor 100 Jahren (westfalen-blatt.de)
[2] Dr. Max Gerson Healing the Hopeless: Amazon.co.uk: Straus, Howard: 9780976018612: Books
The American Heart Association has issued a statement outlining research on so-called alternative medicine (SCAM) for heart failure. They found some SCAMs that work, some that don’t work, and some that are harmful.
Alternative therapies that may benefit people with heart failure include:
- Omega-3 polyunsaturated fatty acids (PUFA, fish oil) have the strongest evidence among complementary and alternative agents for clinical benefit in people with heart failure and may be used safely, in moderation, in consultation with their health care team. Omega-3 PUFA is associated with a lower risk of developing heart failure and, for those who already have heart failure, improvements in the heart’s pumping ability. There appears to be a dose-related increase in atrial fibrillation (an irregular heart rhythm), so doses of 4 grams or more should be avoided.
- Yoga and Tai Chi, in addition to standard treatment, may help improve exercise tolerance and quality of life and decrease blood pressure.
Meanwhile, some therapies were found to have harmful effects, such as interactions with common heart failure medications and changes in heart contraction, blood pressure, electrolytes and fluid levels:
- While low blood levels of vitamin D are associated with worse heart failure outcomes, supplementation hasn’t shown benefit and may be harmful when taken with heart failure medications such as digoxin, calcium channel blockers and diuretics.
- The herbal supplement blue cohosh, from the root of a flowering plant found in hardwood forests, might cause a fast heart rate called tachycardia, high blood pressure, chest pain and may increase blood glucose. It may also decrease the effect of medications taken to treat high blood pressure and Type 2 diabetes.
- Lily of the valley, the root, stems and flower of which are used in supplements, has long been used in mild heart failure because it contains active chemicals similar to, but less potent than, the heart failure medicine digoxin. It may be harmful when taken with digoxin by causing very low potassium levels, a condition known as hypokalemia. Lily of the valley also may cause irregular heartbeat, confusion and tiredness.
Other therapies have been shown as ineffective based on current data, or have mixed findings, highlighting the importance of patients having a discussion with a health care professional about any non-prescribed treatments:
- Routine thiamine supplementation isn’t shown to be effective for heart failure treatment unless someone has this specific nutrient deficiency.
- Research on alcohol varies, with some data showing that drinking low-to-moderate amounts (1 to 2 drinks per day) is associated with preventing heart failure, while habitual drinking or intake of higher amounts is toxic to the heart muscle and known to contribute to heart failure.
- There are mixed findings about vitamin E. It may have some benefit in reducing the risk of heart failure with preserved ejection fraction, a type of heart failure in which the left ventricle is unable to properly fill with blood between heartbeats. However, it has also been associated with an increased risk of hospitalization in people with heart failure.
- Co-Q10, or coenzyme Q10, is an antioxidant found in small amounts in organ meats, oily fish and soybean oil, and commonly taken as a dietary supplement. Small studies show it may help improve heart failure class, symptoms and quality of life, however, it may interact with blood pressure lowering and anti-clotting medicines. Larger trials are needed to better understand its effects.
- Hawthorn, a flowering shrub, has been shown in some studies to increase exercise tolerance and improve heart failure symptoms such as fatigue. Yet it also has the potential to worsen heart failure, and there is conflicting research about whether it interacts with digoxin.
“Overall, more quality research and well-powered randomized controlled trials are needed to better understand the risks and benefits of complementary and alternative medicine therapies for people with heart failure,” said Chow. “This scientific statement provides critical information to health care professionals who treat people with heart failure and may be used as a resource for consumers about the potential benefit and harm associated with complementary and alternative medicine products.”
____________________
No doubt, this assessment is a laudable attempt to inform patients responsibly. Personally, I am always a bit skeptical about such broad statements. SCAM encompasses some 400 different therapies, and I doubt that these can all be assessed in one single overview.
It is not difficult to find SCAMs that seem to have not been considered. Take this systematic review, for instance. It included 24 RCTs (n = 1314 participants) of 9 different mind-body interventions (MBI) types: Tai Chi (n = 7), yoga (n = 4), relaxation (n = 4), meditation (n = 2), acupuncture (n = 2), biofeedback (n = 2), stress management (n = 1), Pilates (n = 1), and reflexology (n = 1). Most (n = 22, 95.8%) reported small-to-moderate improvements in quality of life (14/14 studies), exercise capacity (8/9 studies), depression (5/5 studies), anxiety and fatigue (4/4 studies), blood pressure (3/5 studies), heart rate (5/6 studies), heart rate variability (7/9 studies), and B-type natriuretic peptide (3/4 studies). Studies ranged from 4 minutes to 26 weeks and group sizes ranged from 8 to 65 patients per study arm.
The authors concluded that, although wide variability exists in the types and delivery, RCTs of MBIs have demonstrated small-to-moderate positive effects on HF patients’ objective and subjective outcomes. Future research should examine the mechanisms by which different MBIs exert their effects.
Or take this systematic review of 38 RCTs of oral TCM remedies. The majority of the included trials were assessed to be of high clinical heterogeneity and poor methodological quality. The main results of the meta-analysis showed improvement in total MLHFQ score when oral Chinese herbal medicine plus conventional medical treatment (CMT) compared with CMT with or without placebo [MD = -5.71 (-7.07, -4.36), p < 0.01].
The authors concluded that there is some encouraging evidence of oral Chinese herbal medicine combined with CMT for the improvement of QoL in CHF patients. However, the evidence remains weak due to the small sample size, high clinical heterogeneity, and poor methodological quality of the included trials. Further, large sample size and well-designed trials are needed.
Don’t get me wrong: I am not saying that TCM remedies are a viable option – in fact, I very much doubt it – but I am saying that attempts to provide comprehensive overviews of all SCAMs are problematic, and that incomplete overviews are just that: incomplete.
Hardly a day goes by that I am not asked by someone – a friend, colleague, practitioner, journalist, etc. – about the evidence for this or that so-called alternative medicine (SCAM). I always try my best to give a truthful answer, and often it amounts to something like this: TO THE BEST OF MY KNOWLEDGE, THERE IS NO GOOD EVIDENCE TO SHOW THAT IT WORKS.
The reactions to this news vary, e.g.:
- Some ignore it and seem to think ‘what does he know?’.
- Some thank me and make their decisions accordingly.
- Some feel they better do a fact-check.
The latter reaction is perhaps the most interesting because often the person, clearly an enthusiast of that particular SCAM, later comes back to me and triumphantly shows me evidence that contradicts my statement.
This means I now must have a look at what evidence he/she has found.
It can fall into several categories:
- Opinion articles published by proponents of the SCAM in question.
- Papers that are not truly relevant to the SCAM.
- Research that provides data about the SCAM that does not relate to its effectiveness, e.g. surveys, or qualitative studies.
- Studies of the SCAM in question.
It is usually easy to explain why the three first-named categories are irrelevant. Yet, the actual studies can be a problem. Remember, I told that person that no good evidence exists, and now he (let’s assume I am dealing with a man) proudly shows me a study of it suggesting the opposite. There might be the following explanations:
- I did not know this high-quality study (e.g. because it is new) and my dismissive statement was thus questionable or wrong.
- The study draws a positive conclusion about the SCAM but this conclusion is not justified.
In the first instance, do I need to change my mind and apologize for my wrong statement? Perhaps! But I also need to explain that, even with a rigorous study, we really ought to have one (better more than one) independent replication before we start changing our clinical routine.
In the second instance, I need to explain why the conclusion is not justified. The realm of SCAM is plagued by studies with misleading conclusions (as regular readers of this blog know only too well). Therefore, this situation arises with some regularity. There are numerous reasons why a study can generate unreliable findings (as regular readers of this blog know only too well). Some of them are easy to understand others might be more difficult for non-scientists to comprehend. This means that the discussions with the man who proudly brought the ‘evidence’ to my attention can be tedious.
Often he feels that I am unfair to his favorite SCAM. He might argue that:
- I am biased;
- I lack an open mind;
- I am not qualified;
- I am changing the goalpost;
- I am applying double standards because much of the research into conventional medicine is also not flawless.
In such cases, we are likely to eventually end our discussions by agreeing to disagree. He will be convinced of his point of view and I will be convinced of mine. Essentially, we are more or less where we started, and the whole palaver was for nothing.
… a bit like this post?
I hope not!
What I have been trying to demonstrate is that:
- SCAM enthusiasts are often difficult, sometimes impossible to convince;
- research is not always easy to understand and requires a minimum of education and know-how.
Onion water seems to be all the rage these days. Advocates claim that it is a natural cold and flu remedy that can help the body heal faster and kick symptoms like coughing and congestion. And many consumers who feel threatened by flu, COVID, and various respiratory infections believe them.
But what on earth is onion water? It is precisely what it sounds like: onion immersed in water. Preparation starts with cutting up raw red or yellow onions, placing them into a bowl, and adding water. The fresh onion and water mixture should then soak for about 12 hours. After that, the onion water is ready for consumption. 
Besides being a recipe for bad breath, can onion water actually relieve any symptoms, or help the body heal from infections?
A review of the evidence concluded that “effect of onion and its constituents on oxidative stress, inflammatory and immune system were shown indicating their therapeutic value in treatment of various diseases associated with oxidative stress, inflammation, and immune-dysregulation.”
This may sound encouraging but the review was based mostly on pre-clinical evidence, and the question, therefore, remains: are there any good trial data?
Another recent review included clinical trials (where available) and concluded that “possible bronchodilatory and preventive effects of onion and Qt on asthma and other obstructive respiratory diseases. The effects of the plant and its constituents on lung cancer, lung infections, and allergic disorders were also reported both in experimental and clinical studies. However, before preparing drugs based on A. cepa and its constituents for clinical practice, further standard clinical trials are needed to be performed.”
In other words, compelling trial evidence that preparations from onion are effective against viral infections does not exist.
And what about homeopathy?
Homeopaths frequently use potentised onion as a remedy for conditions that cause eyes to water (because ‘like cures like’). Is there any sound evidence that homeopathic onion remedies are better than a placebo? You probably guessed: the answer is NO!
So, no good evidence for onion, potentised onion, onion water, or any other preparations of onion. My advice, therefore, is to continue using your onions in the kitchen rather than in the medicine cabinet.
Osteopathy is currently regulated in 12 European countries: Cyprus, Denmark, Finland, France, Iceland, Italy, Liechtenstein, Luxembourg, Malta, Portugal, Switzerland, and the UK. Other countries such as Belgium and Norway have not fully regulated it. In Austria, osteopathy is not recognized or regulated. The Osteopathic Practitioners Estimates and RAtes (OPERA) project was developed as a Europe-based survey, whereby an updated profile of osteopaths not only provides new data for Austria but also allows comparisons with other European countries.
A voluntary, online-based, closed-ended survey was distributed across Austria in the period between April and August 2020. The original English OPERA questionnaire, composed of 52 questions in seven sections, was translated into German and adapted to the Austrian situation. Recruitment was performed through social media and an e-based campaign.
The survey was completed by 338 individuals (response rate ~26%), of which 239 (71%) were female. The median age of the responders was 40–49 years. Almost all had preliminary healthcare training, mainly in physiotherapy (72%). The majority of respondents were self-employed (88%) and working as sole practitioners (54%). The median number of consultations per week was 21–25 and the majority of respondents scheduled 46–60 minutes for each consultation (69%).
The most commonly used diagnostic techniques were: palpation of position/structure, palpation of tenderness, and visual inspection. The most commonly used treatment techniques were cranial, visceral, and articulatory/mobilization techniques. The majority of patients estimated by respondents consulted an osteopath for musculoskeletal complaints mainly localized in the lumbar and cervical region. Although the majority of respondents experienced a strong osteopathic identity, only a small proportion (17%) advertise themselves exclusively as osteopaths.
The authors concluded that this study represents the first published document to determine the characteristics of the osteopathic practitioners in Austria using large, national data. It provides new information on where, how, and by whom osteopathic care is delivered. The information provided may contribute to the evidence used by stakeholders and policy makers for the future regulation of the profession in Austria.
This paper reveals several findings that are, I think, noteworthy:
- Visceral osteopathy was used often or very often by 84% of the osteopaths.
- Muscle energy techniques were used often or very often by 53% of the osteopaths.
- Techniques applied to the breasts were used by 59% of the osteopaths.
- Vaginal techniques were used by 49% of the osteopaths.
- Rectal techniques were used by 39% of the osteopaths.
- “Taping/kinesiology tape” was used by 40% of osteopaths.
- Applied kinesiology was used by 17% of osteopaths and was by far the most-used diagnostic approach.
Perhaps the most worrying finding of the entire paper is summarized in this sentence: “Informed consent for oral techniques was requested only by 10.4% of respondents, and for genital and rectal techniques by 21.0% and 18.3% respectively.”
I am lost for words!
I fail to understand what meaningful medical purpose the fingers of an osteopath are supposed to have in a patient’s vagina or rectum. Surely, putting them there is a gross violation of medical ethics.
Considering these points, I find it impossible not to conclude that far too many Austrian osteopaths practice treatments that are implausible, unproven, potentially harmful, unethical, and illegal. If patients had the courage to take action, many of these charlatans would probably spend some time in jail.
Yesterday, the post brought me a nice Christmas present. For many months, I had been working on updating and extending a book of mine. Then there were some delays at the publisher, but now it is out – what a delight!
The previous edition contained my evidence-based assessments of 150 alternative modalities (therapies and diagnostic techniques). This already was by no means an easy task. The new edition has 202 short, easy-to-understand, and fully-referenced chapters, each on a different modality. I am quite proud of the achievement. Let me just show you the foreword to the new edition:
Alternative medicine is full of surprises. For me, a big surprise was that the first edition of this book was so successful that I was invited to do a second one. I do this, of course, with great pleasure.
So, what is new? I have made two main alterations. Firstly, I updated the previous text by adding new evidence where it had emerged. Secondly, I added many more modalities—52, to be exact.
To the best of my knowledge, this renders the new edition of this book the most comprehensive reference text on alternative medicine available to date. It informs you about the nature, proven benefits, and potential risks of 202 different diagnostic methods and therapeutic interventions from the realm of so-called alternative medicine. If you use this information wisely, it could save you a lot of money. One day, it might even save your life.
I hope you enjoy using this book as much as I enjoyed writing it.
Like the first edition, the book is not about promoting so-called alternative medicine (SCAM) nor about the opposite. It is about evaluating SCAM critically but fairly. In other words, each subject had to be researched and the evidence for or against it explained such that a layperson will comprehend it. This proved to be a colossal task.
The end result will not please the many believers in SCAM, I am afraid. Yet, I hope it will suit those who realize that, in healthcare, progress is generated not through belief but through critical evaluation of the evidence.
Is acupuncture more than a theatrical placebo? Acupuncture fans are convinced that the answer to this question is YES. Perhaps this paper will make them think again.
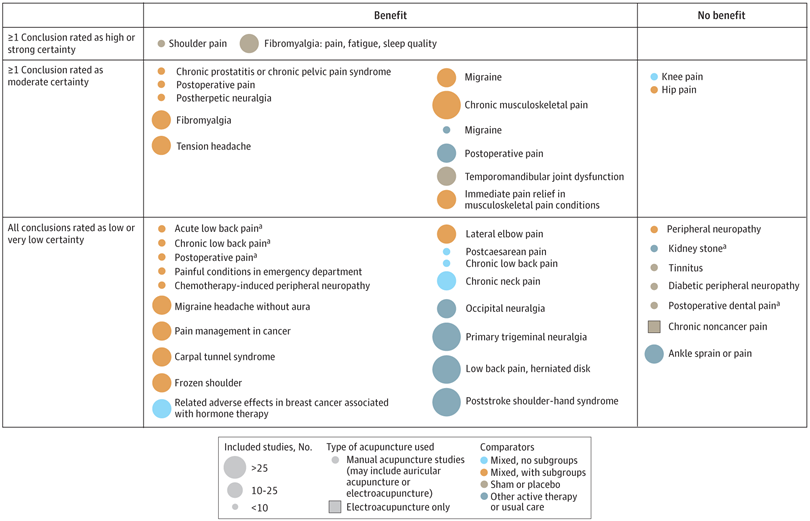
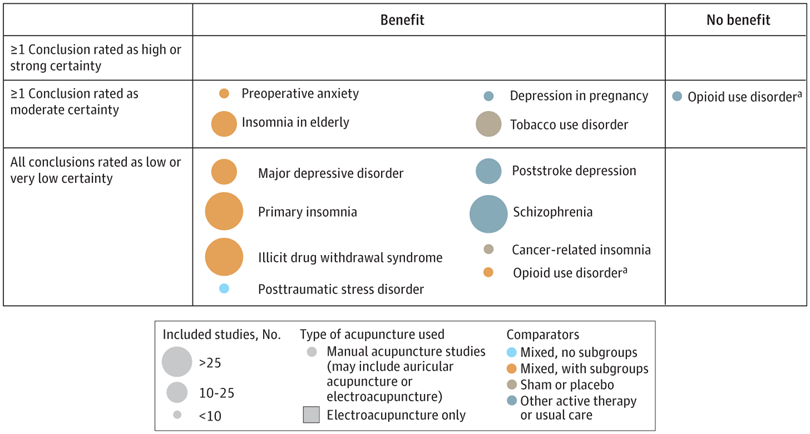
A new analysis mapped the systematic reviews, conclusions, and certainty or quality of evidence for outcomes of acupuncture as a treatment for adult health conditions. Computerized search of PubMed and 4 other databases from 2013 to 2021. Systematic reviews of acupuncture (whole body, auricular, or electroacupuncture) for adult health conditions that formally rated the certainty, quality, or strength of evidence for conclusions. Studies of acupressure, fire acupuncture, laser acupuncture, or traditional Chinese medicine without mention of acupuncture were excluded. Health condition, number of included studies, type of acupuncture, type of comparison group, conclusions, and certainty or quality of evidence. Reviews with at least 1 conclusion rated as high-certainty evidence, reviews with at least 1 conclusion rated as moderate-certainty evidence and reviews with all conclusions rated as low- or very low-certainty evidence; full list of all conclusions and certainty of evidence.
A total of 434 systematic reviews of acupuncture for adult health conditions were found; of these, 127 reviews used a formal method to rate the certainty or quality of evidence of their conclusions, and 82 reviews were mapped, covering 56 health conditions. Across these, there were 4 conclusions that were rated as high-certainty evidence and 31 conclusions that were rated as moderate-certainty evidence. All remaining conclusions (>60) were rated as low- or very low-certainty evidence. Approximately 10% of conclusions rated as high or moderate-certainty were that acupuncture was no better than the comparator treatment, and approximately 75% of high- or moderate-certainty evidence conclusions were about acupuncture compared with a sham or no treatment.
Three evidence maps (pain, mental conditions, and other conditions) are shown below
The authors concluded that despite a vast number of randomized trials, systematic reviews of acupuncture for adult health conditions have rated only a minority of conclusions as high- or moderate-certainty evidence, and most of these were about comparisons with sham treatment or had conclusions of no benefit of acupuncture. Conclusions with moderate or high-certainty evidence that acupuncture is superior to other active therapies were rare.
These findings are sobering for those who had hoped that acupuncture might be effective for a range of conditions. Despite the fact that, during recent years, there have been numerous systematic reviews, the evidence remains negative or flimsy. As 34 reviews originate from China, and as we know about the notorious unreliability of Chinese acupuncture research, this overall result is probably even more negative than the authors make it out to be.
Considering such findings, some people (including the authors of this analysis) feel that we now need more and better acupuncture trials. Yet I wonder whether this is the right approach. Would it not be better to call it a day, concede that acupuncture generates no or only relatively minor effects, and focus our efforts on more promising subjects?
An international team of researchers described retracted papers originating from paper mills, including their characteristics, visibility, and impact over time, and the journals in which they were published. The term paper mill refers to for-profit organizations that engage in the large-scale production and sale of papers to researchers, academics, and students who wish to, or have to, publish in peer-reviewed journals. Many paper mill papers included fabricated data.
All paper mill papers retracted from 1 January 2004 to 26 June 2022 were included in the study. Papers bearing an expression of concern were excluded. Descriptive statistics were used to characterize the sample and analyze the trend of retracted paper mill papers over time, and to analyze their impact and visibility by reference to the number of citations received.
In total, 1182 retracted paper mill papers were identified. The publication of the first paper mill paper was in 2004 and the first retraction was in 2016; by 2021, paper mill retractions accounted for 772 (21.8%) of the 3544 total retractions. Overall, retracted paper mill papers were mostly published in journals of the second highest Journal Citation Reports quartile for impact factor (n=529 (44.8%)) and listed four to six authors (n=602 (50.9%)). Of the 1182 papers, almost all listed authors of 1143 (96.8%) paper mill retractions came from Chinese institutions, and 909 (76.9%) listed a hospital as a primary affiliation. 15 journals accounted for 812 (68.7%) of 1182 paper mill retractions, with one journal accounting for 166 (14.0%). Nearly all (n=1083, 93.8%) paper mill retractions had received at least one citation since publication, with a median of 11 (interquartile range 5-22) citations received.
The authors concluded that papers retracted originating from paper mills are increasing in frequency, posing a problem for the research community. Retracted paper mill papers most commonly originated from China and were published in a small number of journals. Nevertheless, detected paper mill papers might be substantially different from those that are not detected. New mechanisms are needed to identify and avoid this relatively new type of misconduct.
China encourages its researchers to publish papers in return for money and career promotions. Furthermore, medical students at Chinese universities are required to produce a scientific paper in order to graduate. Paper mills openly advertise their services on the Internet and maintain a presence on university campuses. The authors of this analysis reference another recent article (authored by two Chinese researchers) that throws more light on the problem:
This study used data from the Retraction Watch website and from published reports on retractions and paper mills to summarize key features of research misconduct in China. Compared with publicized cases of falsified or fabricated data by authors from other countries of the world, the number of Chinese academics exposed for research misconduct has increased dramatically in recent years. Chinese authors do not have to generate fake data or fake peer reviews for themselves because paper mills in China will do the work for them for a price. Major retractions of articles by authors from China were all announced by international publishers. In contrast, there are few reports of retractions announced by China’s domestic publishers. China’s publication requirements for physicians seeking promotions and its leniency toward research misconduct are two major factors promoting the boom of paper mills in China.
As the authors of the new analysis point out: “Fraudulent papers have negative consequences for the scientific community and the general public, engendering distrust in science, false claims of drug or device efficacy, and unjustified academic promotion, among other problems.” On this blog, I have often warned of research originating from China (some might even think that this is becoming an obsession of mine but I do truly think that this is very important). While such fraudulent papers may have a relatively small impact in many areas of healthcare, their influence in the realm of TCM (where the majority of research comes from China) is considerable. In other words, TCM research is infested by fraud to a degree that prevents drawing meaningful conclusions about the value of TCM treatments.
I feel strongly that it is high time for us to do something about this precarious situation. Otherwise, I fear that in the near future no respectable scientist will take TCM seriously.
It has been reported that a naturopath from the US who sold fake COVID-19 immunization treatments and fraudulent vaccination cards during the height of the coronavirus pandemic has been sentenced to nearly three years in prison. Juli A. Mazi pleaded guilty last April in federal court in San Francisco to one count of wire fraud and one count of false statements related to health care matters. Now District Judge Charles R. Breyer handed down a sentence of 33 months, according to Joshua Stueve, a spokesperson for the U.S. Department of Justice. Mazi, of Napa, was ordered to surrender to the Bureau of Prisons on or before January 6, 2023.
The case is the first federal criminal fraud prosecution related to fraudulent Centers for Disease Control and Prevention vaccination cards for COVID-19, according to the U.S. Department of Justice. In August, Breyer denied Mazi’s motion to withdraw her plea agreement after she challenged the very laws that led to her prosecution. Mazi, who fired her attorneys and ended up representing herself, last week filed a letter with the court claiming sovereign immunity. Mazi said that as a Native American she is “immune to legal action.”
She provided fake CDC vaccination cards for COVID-19 to at least 200 people with instructions on how to complete the cards to make them look like they had received a Moderna vaccine, federal prosecutors said. She also sold homeopathic pellets she fraudulently claimed would provide “lifelong immunity to COVID-19.” She told customers that the pellets contained small amounts of the virus and would create an antibody response. Mazi also offered the pellets in place of childhood vaccinations required for attendance at school and sold at least 100 fake immunization cards that said the children had been vaccinated, knowing the documents would be submitted to schools, officials said. Federal officials opened an investigation against Mazi after receiving a complaint in April 2021 to the Department of Health and Human Services Office of Inspector General hotline.
_______________________
On her website, Mazi states this about herself:
Juli Mazi received her doctorate in Naturopathic Medicine from the National University of Natural Medicine in Portland, Oregon where she trained in the traditional medical sciences as well as ancient and modern modalities that rely on the restorative power of Nature to heal. Juli Mazi radiates the vibrant health she is committed to helping her patients achieve. Juli’s positive outlook inspires confidence; her deep well of calm puts people at immediate ease. The second thing they notice is that truly she listens. Dr. Mazi’s very presence is healing.
On this site, she also advocates all sorts of treatments and ideas which I would call more than a little strange, for instance, coffee enemas:
Using a coffee enema is a time-tested remedy for detoxification, but it is not without risks. If you are not careful, the process can cause internal burns. In addition, improperly brewed coffee can lead to electrolyte imbalances and dehydration, and coffee enemas are not recommended for pregnant women or young children.
To make coffee enemas safe and effective, always choose quality organic coffee. A coffee enema should be free of toxins and pesticides. Use a reusable enema kit with stainless steel or silicone hosing for safety. Moreover, do not use a soft plastic or latex enema bags. It is also essential to limit the length of time that the coffee spends in the container.
A coffee enema should be held for 12 to 15 minutes and then released in the toilet. You may repeat the process as necessary. Usually, the procedure should be done once or twice a day. However, if you are experiencing acute toxicity, you can use a coffee enema as often as needed. Make sure you have had a bowel movement before making the coffee enema. Otherwise, the process may be hindered.
Perhaps the most interesting thing on her website is her advertisement of the fact that her peers not just tolerate such eccentricities but gave Mazi an award for ‘BEST ALTERNATIVE HEALTH & BEST GENERAL PRACTITIONER’.
To me, this suggests that US ‘doctors of naturopathy’ and their professional organizations live on a different planet, a planet where evidence counts for nothing and dangerously misleading patients seems to be the norm.
I know, I have often posted nasty things about integrative medicine and those who promote it. Today, I want to make good for all my sins and look at the bright side.
Imagine you are a person convinced of the good that comes from so-called alternative medicine (SCAM). Imagine you believe it has stood the test of time, is natural, holistic, tackles the root problems of illness, etc., etc. Imagine you are such a person.
Your convictions made you support more research into SCAM because you feel that evidence is needed for it to be more generally accepted. So, you are keen to see more studies proving the efficacy of this or that SCAM in the management of this or that condition.
This, unfortunately, is where the problems start.
Not only is there not a lot of money and even fewer scientists to do this research, but the amount of studies that would need doing is monstrously big:
- There are hundreds of different types of SCAM.
- Each SCAM is advocated for hundreds of conditions.
Consequently, tens of thousands of studies are needed to only have one trial for each specific research question. This is tough for a SCAM enthusiast! It means he/she has to wait decades to see the light at the end of the tunnel.
But then it gets worse – much worse!
As the results of these studies come in, one after the other, you realize that most of them are not at all what you have been counting on. Many can be criticized for being of dismal quality and therefore inconclusive, and those that are rigorous tend to be negative.
Bloody hell! There you have been waiting patiently for decades and now you must realize that this wait did not take you anywhere near the goal that was so clear in your sight. Most reasonable people would give up at this stage; they would conclude that SCAM is a pipedream and direct their attention to something else. But not you! You are single-minded and convinced that SCAM is the future. Some people might even call you obsessed – obsessed and desperate.
It is out of this sense of desperation that the idea of integrative medicine was born. It is a brilliant coup that solves most of the insurmountable problems outlined above. All you need to do is to take the few positive findings that did emerge from the previous decades of research, find a political platform, and loudly proclaim:
SCAM does work.
Consumers like SCAM.
SCAM must be made available to all.
Consumers deserve the best of both worlds.
The future of healthcare evidently lies in integrated medicine.
Forgotten are all those irritating questions about the efficacy of this or that treatment. Now, it’s all about the big issue of wholesale integration of SCAM. Forgotten is the need for evidence – after all, we had decades of that! – now, the issue is no longer scientific, it is political.
And if anyone has the audacity to ask about evidence, he/she can be branded as a boring nit-picker. And if anyone doubts the value of integrated medicine, he/she will be identified as a politically incorrect dinosaur.
Mission accomplished!