evidence
Turnera diffusa, known as damiana is a shrub native to southern Texas in the United States, Central America, Mexico, South America, and the Caribbean that produces small, aromatic flowers. Damiana is an ingredient in a traditional Mexican liqueur, which is sometimes used in lieu of triple sec in margaritas. Damiana was included in several 19th-century patent medicines, such as Pemberton’s French Wine Coca. The leaves were omitted from that product’s non-alcoholic counterpart, Coca-Cola.
In folklore, the plant was believed to be an aphrodisiac. I looked for evidence from clinical trials but was unable to find any. However, that does not seem to bother PharmaSGP GmbH which produces a drug called Neradin.
The German advertisement of Neradin tells us that:
Bei sexueller Schwäche wie Erektionsstörungen können auch traditionelle Mittel helfen – ohne die Nebenwirkungen mancher chemischer Potenzmittel. Das pflanzliche Arzneimittel Neradin® nutzt dazu erfolgreich Wirkstoffe der mexikanischen Heilpflanze Damiana (Turnera Diffusa).
Die Vorteile von Neradin® auf einen Blick: Fördert die Potenz des Mannes bei sexueller Schwäche
I translated this into English:
Traditional remedies can also help with sexual weakness such as erectile dysfunction – without the side effects of some chemical sexual enhancers. The herbal medicine Neradin® successfully uses active ingredients from the Mexican medicinal plant Damiana (Turnera Diffusa).
The advantages of Neradin® at a glance: Promotes male potency in case of sexual weakness
The patient information leaflet states that “Niradin is a homeopathic drug” and “one tablet Niradin contains 100mg Turnera Diffusa Trit. D4”.
English language sites concur:
Neradin is a homeopathic medicine. Homeopathy is understood as a regulatory therapy for acute and chronic diseases. The areas of application are derived from the homeopathic drug pictures. The following indications are authorised for this medicinal product: Discomfort caused by sexual weakness
So, what we seem to have here is the following:
- A pharma firm that advertises a homeopathic product as a herbal drug.
- A homeopathic remedy that is based on a plant for which there is not a jot of evidence.
- If there were evidence that the plant helps against erectile dysfunction, its homeopathic dilution would, according to the homeopathic ‘like cures like’ axiom, bring about erectile dysfunction.
- A dilution (1:10000) that is too low to have any effect, even if it were made of Viagra.
Am I the only one to think that something is not quite right here?
But don’t let it spoil your HAPPY VALENTINE!
Remember the Bavarian Homeopathy Study? I reported about it only a few days ago. Now the ‘German Homeopathic Doctors Association’ has published an interview with someone who allegedly knows more about it. Here is my translation:
Dr. Springer, what does it actually mean politically that this study came about at all?
First of all, it means that the work of several years was worthwhile and that we were able to convince those responsible with a carefully elaborated study design. It also shows how enormously important it is to have solid political contacts with parties, MPs, parliamentary groups, and spokespersons in health committees. In addition to persuasion, personal credibility and professional competence are indispensable for the growth of such contacts. This is also shown by the fact that LIMed (List of Integrative Medicine) in Bavaria (as in some other federal states) has succeeded in sending committed colleagues to the representations of the State Medical Association and the Medical District and County Association.
What is special about this study?
As far as I know, it is the first study worldwide to be carried out with hand-shaken high potencies (C 200 and C 1000). If the results were positive, the mechanism of action of homeopathy would not be clarified, but it would be proven that highly potentised medicinal substances have a healing effect that can be objectified scientifically.
Who is the sponsor of this study?
The Bavarian Parliament voted with an absolute majority to scientifically investigate the role of complementary medicine in the fight against increasing antibiotic resistance. Several study designs were submitted on this question, and our study approach won the bid in the end. The Bavarian State Ministry of Health and Care is financing the study and has won the Technical University of Munich as a partner – after all, it is one of Germany’s universities of excellence. This removes all doubts about the correct scientific conduct of the study.
What is to be investigated in the study?
It relates to a diagnosis with great relevance to healthcare: Women often suffer from recurrent urinary tract infections, which are often treated with antibiotics. This is always associated with the risk of causative bacteria developing resistance to antibiotics. As homeopathically qualified doctors, we know from decades of experience that we can reduce and even end the frequency of recurrent urinary tract infections and their occurrence with our homeopathic remedies. We want to put this experience to the test scientifically with this study.
How do you see the chances for a positive study result?
As doctors, we know what we do and what we can do. We will do everything in our power to show that we can do it! I would also like to take this opportunity to thank all those who have made this study possible and who are providing us with professional and scientific support!-
The interview was conducted by Ulf Riker, MD.
___________________________
The interview raises several questions:
- Dr. Springer confirms that the existence of the study and its financial support is mostly due to political influence. Is this how good science should be generated?
- Is it true that the study is the first to investigate potency homeopathy? Considering that the bestselling homeopathic, Oscillococcinum, is sold in the C200 potency, this seems to be a very questionable statement.
- If the results were to come out positive, would we really re-write the textbooks of physics and chemistry which state that the absence of an active molecule cannot have an effect?
- Does the involvement of the Technical University truly remove all doubts about the correct scientific conduct of the study?
- If the homeopathically qualified doctors conducting the study already claim to know from decades of experience that they can reduce and even end the frequency of recurrent urinary tract infections with homeopathic remedies, are they not going to be too biased in conducting such a study?
- If the trialists are determined to do everything in their power to show that homeopathy works, will the study generate a reliable result?
- My last question is, how reliable is Dr. Springer? I found another interview of him dated 2021. In it he stated about the homeopathic treatment of COVID patients: ” [There is a} group of Covid-19 patients … [to] whose successful treatment we as homeopathic physicians can certainly contribute. The symptomatology of these patients is considerable, sometimes severe, but not life-threatening. They suffer from headaches and pain in the limbs, dizziness, fever, have the often-quoted “dry cough”, sweat, and usually feel very weak. But they have not yet developed clinical symptoms of pneumonia. These patients – and they are by no means few – can be helped by medical homeopathy, I am firmly convinced, curatively. Provided, of course, that a very precise, individual homeopathic anamnesis is carried out, the patient is closely followed, the course of the disease is closely observed and the remedy administered is adjusted if necessary. By preventing an acute condition and hospitalization in these patients homeopathy could make a not inconsiderable contribution to overcoming these greatest health and social challenges in one hundred years.” That, I think might answer my question.
As I pointed out before, the study design looks rigorous. After reading this interview, I have my doubts that its execution will be rigorous as well.
I recently came across a truly baffling article. As it is in German, I translated it for you:
Supply shortages have kept pharmacies on tenterhooks for months, with more than 400 common medicines missing. The German Central Association of Homeopathic Doctors (DZVhÄ) suggests switching to alternative medicine as a solution: “We have homeopathic medicines that have been tried and tested in practice for more than 200 years and can replace many medicines that are currently not available,” says the president of the DZVhÄ , Dr Michaela Geiger.
The DZVhÄ is convinced that homeopathic medical practices can replace fever-reducing medicines, but in many cases also antibiotics and much more. However, Geiger qualifies: “Due to our medical training, we also know that cancer drugs such as the often cited Tamoxifen cannot be replaced by homeopathy”.
The homeopathic doctors respond directly to the sharpest argument of their critics: “But let’s assume that homeopathy only works via the placebo effect, as is being rumored, even then it would be an option, especially if other options are lacking,” says DZVhÄ vice-president Dr. Ulf Riker. Since homeopathically trained doctors can judge the general course of a disease, they can also distinguish a placebo effect from a medicinal effect.
…
If fever medication for children is lacking, parents should not be deprived of another “therapy option”, Riker said. “If you do not get your conventional fever medication in the coming weeks, visit a specialist pharmacy for naturopathy and homeopathy. If you are due for a medical consultation, experienced homeopathic doctors can prescribe a suitable homeopathic medicine for you,” he says.
Why do I find this so intriguing?
Essentially, what we have learned from the article is the following:
- “Tried and tested in practice for more than 200 years” is ‘homeopathy speak’ for “effective”, even if the evidence tells us otherwise.
- Homeopathic remedies can replace many evidence-based conventional medications such as fever-reducing medicines, antibiotics, and much more, even if the evidence tells us otherwise.
- Homeopaths know that cancer drugs cannot be replaced by homeopathy – except for those homeopaths who seem to have forgotten this simple lesson.
- Homeopathic placebos are a realistic option when there is a supply problem with effective drugs, even if the evidence tells us otherwise.
- Homeopathically trained doctors can distinguish a placebo effect from a medicinal effect, even if there is no evidence that any clinician can reliably do this.
- Homeopathic doctors prescribe suitable homeopathic medicine. Suitable for whom? As it is ineffective, it is unsuitable for the patient. Therefore, Riker is probably talking about the homeopath.
So, what have we really learned from this article? I don’t know about you, but I got the impression that the president and the vice president of the DZVhÄ do not seem to mind putting patients in danger, as long as they can promote homeopathy.
Homeopathic remedies are highly diluted formulations without proven clinical benefits, traditionally believed not to cause adverse events. Nonetheless, published literature reveals severe local and non-liver-related systemic side effects. This paper presents the first series on homeopathy-related severe drug-induced liver injury (DILI) from a single center.
A retrospective review of records from January 2019 to February 2022 identified 9 patients with liver injury attributed to homeopathic formulations. Competing causes were comprehensively excluded. Chemical analysis was performed on retrieved formulations using triple quadrupole gas chromatography-mass spectrometry and inductively coupled plasma atomic emission spectroscopy.
Males predominated with a median age of 54 years. The most typical clinical presentation was acute hepatitis, followed by acute on chronic liver failure. All patients developed jaundice, and ascites were notable in one-third of the patients. Five patients had underlying chronic liver disease. COVID-19 prevention was the most common indication for homeopathic use. Probable DILI was seen in 77.8%, and hepatocellular injury predominated (66.7%). Four (44.4%) patients died (3 with chronic liver disease) at a median follow-up of 194 days. Liver histopathology showed necrosis, portal and lobular neutrophilic inflammation, and eosinophilic infiltration with cholestasis. A total of 29 remedies were consumed between 9 patients, and 15 formulations were analyzed. Toxicology revealed industrial solvents, corticosteroids, antibiotics, sedatives, synthetic opioids, heavy metals, and toxic phyto-compounds, even in ‘supposed’ ultra-dilute formulations.
The authors concluded that homeopathic remedies potentially result in severe liver injury, leading to death in those with underlying liver disease. The use of mother tinctures, insufficient dilution, poor manufacturing practices, adulteration and contamination, and the presence of direct hepatotoxic herbals were the reasons for toxicity. Physicians, the public, and patients must realize that Homeopathic drugs are not ‘gentle placebos.’
Over a decade ago, we published a systematic review entitled “Adverse effects of homeopathy: a systematic review of published case reports and case series”:
Aim: The aim of this systematic review was to critically evaluate the evidence regarding the adverse effects (AEs) of homeopathy.
Method: Five electronic databases were searched to identify all relevant case reports and case series.
Results: In total, 38 primary reports met our inclusion criteria. Of those, 30 pertained to direct AEs of homeopathic remedies; and eight were related to AEs caused by the substitution of conventional medicine with homeopathy. The total number of patients who experienced AEs of homeopathy amounted to 1159. Overall, AEs ranged from mild-to-severe and included four fatalities. The most common AEs were allergic reactions and intoxications. Rhus toxidendron was the most frequently implicated homeopathic remedy.
Conclusion: Homeopathy has the potential to harm patients and consumers in both direct and indirect ways. Clinicians should be aware of its risks and advise their patients accordingly.
It caused an outcry from fans of homeopathy who claimed that one cannot insist that homeopathic remedies are ineffective because they contain no active ingredient, while also arguing that they cause severe adverse effects. In a way, they were correct: homeopathic remedies are useless even at causing adverse effects. But this applies only to remedies that are manufactured correctly and that are highly dilute. The trouble is that quality control in homeopathy often seems to be less than adequate. And this is how adverse effects can happen!
The new article from India is an important addition to the literature providing more valuable information about the risks of homeopathy. Its authors were able to do chemical analyses of some of the remedies and could thus show what the reasons for the liver injuries were. The article provides an essential caution for those who delude themselves by assuming that homeopathy is harmless. In fact, the remedies can cause severe problems. But, as we have discussed regularly on this blog, the far greater risk in homeopathy is not the remedy but the homeopath and his/her all too often incompetent advice to patients.
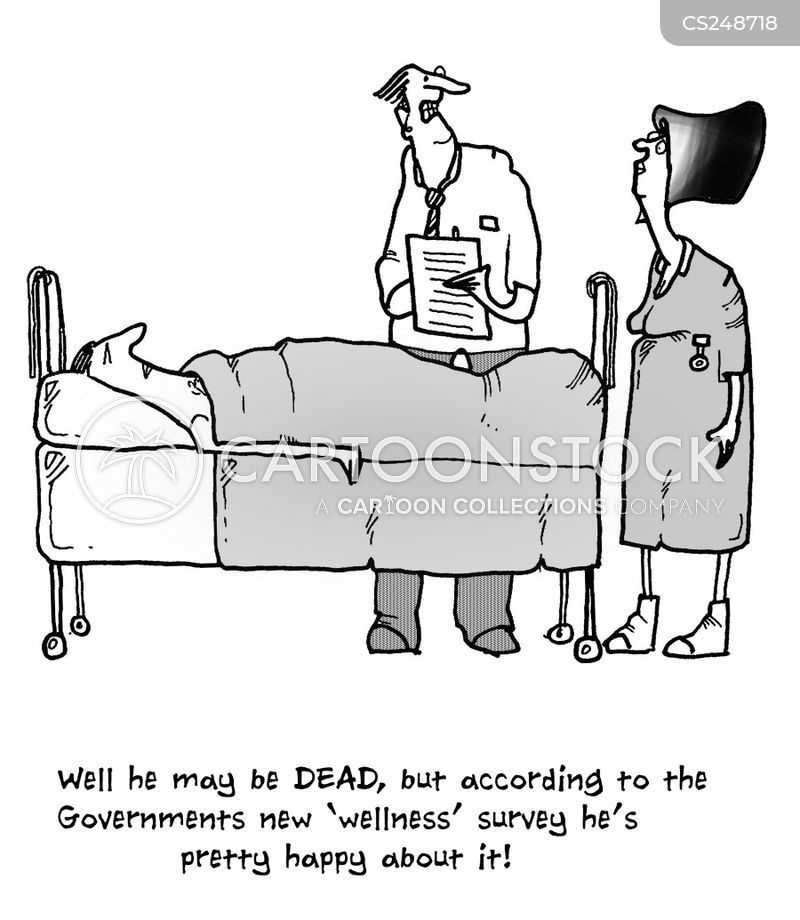
Wellness seems to be everywhere these days – I mean of course the term, not the state or condition. On Medline, we find in excess of 500 000 articles on wellness, just for the year 2022! Wellness is en vogue, sexy, politically correct, etc. It looks good to talk and write about it. Most importantly it is good business. A report by the Global Wellness Institute stated that in 2020 the wellness industry was valued at $4.5 trillion and continues to grow at a frightening rate.
Having studied some of the recent literature on the subject, I get the impression that, for many, wellness is foremost an excuse for waffling utter nonsense. Let me, therefore, today ask just 5 simple questions about wellness that are likely to reduce the wellness of the ‘wellness brigade’:
1.What is wellness?
It is quite evidently a sector that is unable to define itself. Here are just a few of the definitions that have been suggested. Wellness is:
- the active pursuit of activities, choices and lifestyles that lead to a state of holistic health
- the result of personal initiative, seeking a more optimal, holistic and balanced state of health and well-being across multiple dimensions
- an active process of becoming aware of and making choices towards a healthy and fulfilling life
- the state of being in good health, especially as an actively pursued goal
- a state beyond absence of illness but rather aims to optimize well-being
- the act of practicing healthy habits on a daily basis to attain better physical and mental health outcomes
- an active process through which people become aware of, and make choices toward, a more successful existence
- the optimal state of health of individuals and groups
A 2018 review revealed that there is a lack of a uniform definition of wellness and showed that there is insufficient evidence to support the clinical utility of a single particular wellness instrument.
2. How do we measure wellness?
The short answer to this question is: nobody is quite sure. There simply is no generally accepted, well-validated measure. A few domains come to mind:
- physical functioning,
- somatic symptoms, e.g. pain,
- psychological symptoms,
- social functioning,
- needs and satisfaction.
But there is no simple means to quantify wellness. If you think that I am exaggerating, consider this recent review: 79 mental wellness instruments were identified. Most studies did not provide a definition for mental wellness. We identified thirteen mental wellness concepts from 97 studies, namely: life satisfaction, mental wellbeing [general], resilience, self-efficacy, self- esteem, connectedness, coping, self-control, mindfulness/spiritual, hope, sense of coherence, happiness, and life purpose.
3. What affects wellness?
The short answer is: potentially everything. My very own wellness, for instance, deteriorates sharply, if I have to read yet another nonsensical article about it.
4. Which interventions improve wellness?
As we have seen in my previous post, this is where so-called alternative medicine (SCAM) comes in. Since there is no measure to quantify wellness, we just have to take the word of SCAM proponents for it: SCAM improves wellness!!!
Which specific SCAM?
Can I see the evidence?
Sorry, no questions allowed!
And if you dare to insist on evidence, the ‘wellness brigade’ would just give you a pitiful smile and say: wellness has to be experienced, not measured.
5. Are there risks?
Yes, of course! Here are just some of them:
- The treatments advocated for wellness almost invariably cost money.
- The treatments advocated for wellness almost invariably cause direct and indirect harm, as discussed in many of my previous posts.
- Wellness treatments tend to give the impression that one can buy wellness like an expensive piece of clothing without putting in any real effort oneself.
Considering all this, I’d like to offer my very own definition of the sector:
Wellness is a fashionable paradise for charlatans in which they are protected from scientific scrutiny and feel at liberty to bullshit to their hearts’ content.
The All-Party Parliamentary Group (APPG) on Beauty and Wellbeing, UK, has undertaken an investigation into the ‘complementary therapies sector’, to consider how the sector can support everyone’s physical health, mental health, and well-being and take pressure off the NHS. In their recent document, they state:
The complementary therapies industry is an integral part of the Personal Care sector, which includes beauty, wellbeing, and alternative therapies. These therapies can be key to supporting everyone’s health and mental wellbeing…
To ensure complementary therapies can adequately support the NHS, we need to attract more talent into the sector and ensure all therapists receive the right training to become highly skilled professionals.
We also need to enhance the perception of the professionalism within the sector, so that it is no longer seen as ‘frivolous and fluffy’ and non-essential. Building awareness and understanding of its value in supporting our nation’s health is one step. However, it also important to crack down on any bad practice and the ‘underground market’ of poor treatment…
The committee makes the following recommendations:
1. The Government must work with NHS England to better promote the benefits of social prescribing with GPs, nurses and other health and care professionals, and how they can refer people to non-clinical complementary therapy services.
2. The Personal Care sector team in the Department for Business, Energy, Industry and Strategy must work with officials within the Department for Health and Social Care responsible for social prescribing to better integrate complementary therapy services into the NHS, and produce guidance to support health professionals and therapists in doing so.
3. The Department for Health and Social Care must undertake or fund research studies to demonstrate the value of integrating complementary therapy services into the NHS through social prescribing.
4. The Department for Education must revisit the gap between the apprentice wage and minimum wage for apprentices aged 19+, and provide financial incentives for employers to take on learners on any ‘job ready ‘qualification.
5. The Government must give Environmental health officers (EHOs) greater powers to act quickly to deal with bad practice and lead a crack-down on tax evading businesses that are driving down prices and undermining legitimate businesses under pressure.
…
…
…
Conclusions
The evidence that we have received during this investigation clearly demonstrate that greater support
and recognition is needed for the complementary therapies sector to ensure that they are able support
everyone’s physical health, mental health and wellbeing and take pressure off the NHS.
We hope the Government will review our recommendations in order to support the complementary
therapies sector and ensure they have adequate funding and acknowledgement.
In case you are wondering what therapies they refer to, here is their complete list of the treatments (including links to what they seem to think about them):
This could have made me laugh, had it not been so serious. The committee is composed of MPs who might be full of goodwill. Yet, they seem utterly clueless regarding the ‘complementary therapies sector’. For instance, they seem to be unaware of the evidence for some of the treatments they want to promote, e.g. craniosacral therapy, aromatherapy, Reiki, shiatsu, energy healing, or reflexology (which is far less positive than they seem to assume); and they aim at enhancing the “perception of the professionalism” instead of improving the PROFESSIONALISM of the therapists (which obviously would include adherence to evidence-based practice). And perhaps the committee might have given some thought to the question of whether it is ethical to push dubious therapies onto the unsuspecting public.
I could go on, but the perplexing wooliness of the document speaks for itself, I think.
And in case you are wondering who the MP members of the committee are, here is the list of its members:
• Carolyn Harris MP – Co-Chair
• Judith Cummins MP – Co-Chair
• Jessica Morden MP – Vice-Chair
• Jackie Doyle-Price MP – Vice-Chair
• Peter Dowd MP – Treasurer
• Nick Smith MP – Secretary
• Caroline Nokes MP – Member
• Sarah Champion MP – Member
• Alex Davies-Jones MP – Member
• Kate Osamor MP – Member
• John McNally MP – Member
• Kevan Jones MP – Member
• Gagan Mohindra MP- Member
The Secretariat for this APPG is Dentons Global Advisors with support from the National Hair and Beauty Federation, the Federation of Holistic Therapists and spabreaks.com.
PS
Two hours after having posted this, I begin to feel bad about being so dismissive. Let me thus try to do something constructive: I herewith offer to give one or more lectures to the committee about the evidence as it pertains to the therapies they included in their report.
In one of my last posts, I was rather dismissive of veterinary chiropractic.
Was I too harsh?
I did ask readers who disagree with my judgment to send me their evidence.
Sadly, none arrived!
Therefore, I did several further literature searches and found a recent review of the topic. It included 14 studies; 13 were equine and one was a canine study. Seven of these were cohort studies and seven were randomized controlled clinical trials. . Study quality was low (n = 4), moderate (n = 7), and high (n = 3) and included a wide array of outcome parameters with varying levels of efficacy and duration of therapeutic effects, which prevented further meta-analysis. The authors concluded that it was difficult to draw firm conclusions despite all studies reporting positive effects. Optimal technique indications and dosages need to be determined to improve the standardization of these treatment options.
This, I think, can hardly be called good evidence. But I also found this more recent paper:
Chiropractic care is a common treatment modality used in equine practice to manage back pain and stiffness but has limited evidence for treating lameness. The objective of this blinded, controlled clinical trial was to evaluate the effect of chiropractic treatment on chronic lameness and concurrent axial skeleton pain and dysfunction. Two groups of horses with multiple limb lameness (polo) or isolated hind limb lameness (Quarter Horses) were enrolled. Outcome measures included subjective and objective measures of lameness, spinal pain and stiffness, epaxial muscle hypertonicity, and mechanical nociceptive thresholds collected on days 0, 14, and 28. Chiropractic treatment was applied on days 0, 7, 14, and 21. No treatment was applied to control horses. Data was analyzed by a mixed model fit separately for each response variable (p < 0.05) and was examined within each group of horses individually. Significant treatment effects were noted in subjective measures of hind limb and whole-body lameness scores and vertebral stiffness. Limited or inconsistent therapeutic effects were noted in objective lameness scores and other measures of axial skeleton pain and dysfunction. The lack of pathoanatomical diagnoses, multilimb lameness, and lack of validated outcome measures likely had negative impacts on the results.
Great! So, we finally have an RCT of chiropractic for horses. Unfortunately, the study is less than convincing:
- It included just 20 polo horses plus 18 horses active in ridden or competitive work all suffering from lameness.
- The authors state that ‘horses were numerically randomized to treatment and control groups’; yet I am not sure what this means.
- Treatment consisted of high-velocity, low-amplitude, manually applied thrusts to sites of perceived pain or stiffness with the axial and appendicular articulations. Treatment was applied on days 0, 7, 14, and 21 by a single examiner. The control group received no treatment and was restrained quietly for 15 min to simulate the time required for chiropractic treatment. In other words, no placebo controls were used.
- The validity of the many outcome measures is unknown.
- The statistical analyses seem odd to me.
- No correction for multiple statistical tests was done.
- Most of the outcomes show no significant effect.
- Overall, there were some small positive treatment effects based on subjective assessment of lameness, but no measurable treatment effects on objective measures of limb lameness.
- The polo horses began their competition season at the beginning of the study which would have confounded the outcomes.
What does all this tell us about veterinary chiropractic?
Not a lot.
All we can safely say, I think, is that veterinary chiropractic is not evidence-based and that claims to the contrary are certainly ill-informed and most probably of a promotional nature.
Konjac glucomannan (KGM), also just called ‘glucomannan’, is a dietary fiber hydro colloidal polysaccharide isolated from the tubers of Amorphophallus konjac. It is used as a food, a food additive, as well as a dietary supplement in many countries. KGM is claimed to reduce the levels of glucose, cholesterol, triglycerides, and blood pressure.
The objective of this study was to evaluate the effect of the consumption of gummy candy enriched with KGM on appetite and to evaluate anthropometric data, biochemical, and oxidative stress markers in overweight individuals. Forty-two participants aged 18 to 45 years completed this randomized, double-blind, placebo-controlled clinical trial. Participants were randomly assigned to consume for 14 days, 2 candies per day, containing 250 mg of KGM or identical-looking placebo candy with 250 mg of flaxseed meal, shortly after breakfast and dinner. As a result, we observed that there was a reduction in waist circumference and in the intensity of hunger of the participants who consumed KGM. The authors believe that a longer consumption time as well as an increased dose of KGM would contribute to even more satisfactory body results.
These findings seem promising, yet somehow I am not convinced. The study was small and short-term; moreover, the authors seem uncritical and, instead of a conclusion, they offer speculations.
Our own review of 2014 included 9 clinical studies. There was a variation in the reporting quality of the included RCTs. A meta-analysis (random effect model) of 8 RCTs revealed no significant difference in weight loss between glucomannan and placebo (mean difference [MD]: -0.22 kg; 95% confidence interval [CI], -0.62, 0.19; I(2) = 65%). Adverse events included abdominal discomfort, diarrhea, and constipation. We concluded that the evidence from available RCTs does not show that glucomannan intake generates statistically significant weight loss. Future trials should be more rigorous and better reported.
Rigorous trials are required to change my mind, and I am not sure that the new study falls into this category.
The concept of ultra-processed food (UPF) was initially developed and the term coined by the Brazilian nutrition researcher Carlos Monteiro, with his team at the Center for Epidemiological Research in Nutrition and Health (NUPENS) at the University of São Paulo, Brazil. They argue that “the issue is not food, nor nutrients, so much as processing,” and “from the point of view of human health, at present, the most salient division of food and drinks is in terms of their type, degree, and purpose of processing.”
Examples of UPF include:
- Carbonated soft drinks,
- Sweet, fatty or salty packaged snacks,
- Candies (confectionery),
- Mass-produced packaged breads and buns,
- Cookies (biscuits),
- Pastries,
- Cakes and cake mixes,
- Margarine and other spreads,
- Sweetened breakfast cereals,
- Sweetened fruit yoghurt and energy drinks,
- Powdered and packaged instant soups, noodles, and desserts,
- Pre-prepared meat, cheese, pasta and pizza dishes,
- Poultry and fish nuggets and sticks,
- Sausages, burgers, hot dogs, and other reconstituted meat products,
Ultra-processed food is bad for our health! This message is clear and has been voiced so many times – not least by proponents of so-called alternative medicine (SCAM) – that most people should now understand it.
But how bad?
And what diseases does UPF promote?
How strong is the evidence?
I did a quick Medline search and was overwhelmed by the amount of research on this subject. In 2022 alone, there were more than 2000 publications! Here are the conclusions from just a few recent studies on the subject:
- Higher intake of UPFs was associated with higher incidence of Crohn’s disease, but not ulcerative colitis. In individuals with a pre-existing diagnosis of inflammatory bowel disease, consumption of UPFs was significantly higher compared to controls, and was associated with an increased need for IBD-related surgery. Further studies are needed to address the impact of UPF intake on disease pathogenesis, and outcomes.
- In this prospective cohort study, higher consumption of UPF was associated with higher risk of dementia, while substituting unpr2ocessed or minimally processed foods for UPF was associated lower risk of dementia.
- In almost all countries and age groups, increases in the dietary share of ultraprocessed foods were associated with increases in energy density and free sugars and decreases in fiber, suggesting that ultraprocessed food consumption is a potential determinant of obesity in children and adolescents.
- Higher ultraprocessed foods consumption was independently associated with a higher risk of incident chronic kidney disease in a general population.
- These data suggest that a consistent intake of ultra-processed foods over time is needed to impact nutritional status and body composition of children and adolescents.
- This meta-analysis suggests that high consumption of UPF, sugar-sweetened beverages, artificially sweetened beverages, processed meat, and processed red meat might increase all-cause mortality, while breakfast cereals might decrease it.
- The consumption of ultraprocessed foods represents a significant cause of premature death in Brazil.
- Available evidence suggests that UPFs may increase cancer risk via their obesogenic properties as well as through exposure to potentially carcinogenic compounds such as certain food additives and neoformed processing contaminants.
- The high consumption of UPF, almost more than 10% of the diet proportion, could increase the risk of developing type 2 diabetes in adult individuals.
Don’t get me wrong: this is not a systematic review of the subject. I am merely trying to give a rough impression of the research that is emerging. A few thoughts seem nonetheless appropriate.
- The research on this subject is intense.
- Even though most studies disclose associations and not causal links, there is in my view no question that UPF aggravates many diseases.
- The findings of the current research are highly consistent and point to harm done to most organs.
- Even though this is a subject on which advocates of SCAM are exceedingly keen, none of the research I saw was conducted by SCAM researchers.
- The view of many SCAM proponents that conventional medicine does not care about nutrition is clearly not correct.
- Considering how unhealthy UPF is, there seems to be a lack of effective education and action aimed at preventing the harm UPF does to us.
The UK medical doctor, Sarah Myhill, has a website where she tells us:
Everyone should follow the general approach to maintaining and restoring good health, which involves eating a paleo ketogenic diet, taking a basic package of nutritional supplements, ensuring a good night’s sleep on a regular basis and getting the right balance between work, exercise and rest. Because we live in an increasingly polluted world, we should probably all be doing some sort of detox regime.
She also happens to sell dietary supplements of all kinds which must surely be handy for all who want to follow her advice. Dr. Myhill boosted her income even further by putting false claims about Covid-19 treatments online. And that got her banned from practicing for nine months after a medical tribunal.
She posted videos and articles advocating taking vitamins and other substances in high doses, without evidence they worked. The General Medical Council (GMC) found her recommendations “undermined public health” and found some of her recommendations had the potential to cause “serious harm” and “potentially fatal toxicity”. The tribunal was told she uploaded a series of videos and articles between March and May 2020, describing substances as “safe nutritional interventions” which she said meant vaccinations were “rendered irrelevant”. But the substances she promoted were not universally safe and have potentially serious health risks associated with them, the panel was told. The tribunal found Dr. Myhill “does not practice evidence-based medicine and may encourage false reassurance in her patients who may believe that they will not catch Covid-19 or other infections if they follow her advice”.
Dr. Myhill previously had a year-long ban lifted after a General Medical Council investigation into her claims of being a “pioneer” in the treatment of chronic fatigue syndrome. In fact, the hearing was told there had been 30 previous GMC investigations into Dr. Myhill, but none had resulted in findings of misconduct.
Dr. Myhill is also a vocal critic of the PACE trial and biopsychosocial model of ME/CFS. Dr. Myhill’s GMC complaint regarding a number of PACE trial authors was first rejected without investigation by the GMC, after Dr. Myhill appealed the GMC stated they would reconsider. Dr. Myhill’s action against the GMC for failing to provide reasoning for not investigating the PACE trial authors is still continuing and began a number of months before the most recent GMC instigation of her practice started.
The recent tribunal concluded: “Given the circumstances of this case, it is necessary to protect members of the public and in the public interest to make an order suspending Dr. Myhill’s registration with immediate effect, to uphold and maintain professional standards and maintain public confidence in the profession.”