education
In Austria, even some of the most blatant quackery continues to be supported by the country’s medical association. This has been notorious for a very long time, and many rational doctors have opposed this nonsense. Now my friends and colleagues have courageously sent an open letter to the President of the Austrian Medical Association. In order to support their efforts, I have taken the liberty of translating it:
Dr. Johannes Steinhart
President of the Austrian Medical Association
Weihburggasse 10-12
1010 Vienna
Dear President Steinhart,
In 2014 we founded the “Initiative for Scientific Medicine” with the aim of counteracting the support of pseudo-medicine by medical associations and the Ministry of Health.
We (www.initiative-wissenschaftliche-medizin.at) have been demanding for years that the Austrian Medical Association distance itself from irrational, predominantly esoteric pseudo-medicine and refrain from awarding diplomas in them. We also made these demands on behalf of the supporters of the initiative (currently 1142 supporters, of which 495 are female doctors and 230 natural scientists) during a discussion with the former president Wechselberger in 2015 (unfortunately unsuccessful at the time).
We would like to draw your attention to a resolution of the German Medical Congress 2022 on homeopathy and a court ruling in the first instance in Germany on the subject of bioresonance, which show that our neighbours have obviously begun to treat pseudomedicine for what it is, namely sham medicine.
The 126th German Medical Congress 2022 in Bremen has, among other things, passed a long overdue resolution. The additional title “homeopathy” was deleted from the (model) further training regulations. Prior to this decision, 12 of 17 state medical associations had already taken this decision themselves.
In May 2022 in Reutlingen, two managing directors of a company producing and selling bioresonance devices were sentenced to 2 and 3 years in prison and a fine of 2.5 million euros, and the former sales director to 90 days’ imprisonment for commercial fraud and violation of the Therapeutic Products Advertising Act. The verdict is not yet legally binding. Unfortunately, many Austrian doctors also practice this pseudo-medicine method.
The fact that many colleagues offer esoteric, pseudo-medical “therapies” without proven benefits to their patients and can refer to diplomas and accredited further training courses of the Medical Association/Academy of Physicians is difficult for us to understand, especially in view of the fact that the majority of the accredited further training courses are of high scientific quality. A medical association that argues that such pseudo-medical practices “should better remain in the hands of doctors (as “healers”)” contradicts the principles of evidence-based medicine to which the medical association always refers. The corona pandemic has shown us all the damage potential of science denial.
We believe that the time has also come for the Austrian Medical Association to come clean. We call on the Austrian Medical Association to unreservedly declare its support for scientific medicine, to clearly distance itself from pseudo-medicine, to suspend the awarding of diplomas in pseudo-medicine methods that are far removed from science, and to end the accreditation of pseudo-medicine training courses by the Medical Academy.
We are publishing this open letter on our website and will also publish your reply if you so wish.
With collegial greetings
Dr. Theodor Much, Specialist in Dermatology and Venereology, Baden near Vienna
DDr. Viktor Weisshäupl, retired specialist in anaesthesiology and intensive care medicine, Vienna
Despite considerable doubts about its effectiveness, osteopathic manipulative treatment (OMT) continues to be used for a range of pediatric conditions. Here is just one example of many osteopaths advertising their services:
I qualified as an Osteopath in 2009 after 4 years of intensive training from the British College of Osteopathic medicine, where I received a distinction for my efforts. After having two children I decided to do a 2-year Postgraduate training in Pediatric Osteopathy from the Osteopathic Centre for Children in London. Whilst at the centre I was lucky enough to meet a wide variety of children from premature babies in a Neonate Hospital ward to children with developmental issues and disabilities, children on the Autistic spectrum, to kids doing exams or experiencing high levels of stress. We also saw lots of children with normal coughs, colds, lumps and bumps.
And the ‘Institute of Osteopathy states this:
Parents visit osteopaths for a range of reasons to support their child’s health. Children, like adults, can be affected by general joint and muscle issues, which is one of the reasons people visit an osteopath. Parents will also take their children to visit an osteopath for a variety of other health reasons that may benefit from osteopathic care.
As osteopathic care is based on the individual needs of the patient, it will vary depending on your child’s age and the diagnosis. Osteopaths generally use a wide range of gentle hands-on techniques that focus on releasing tension, improving mobility and optimising function. This is often used together with exercise and helpful advice. Some osteopaths have been trained in very gentle techniques which are particularly suitable to assess and treat very young children, including new-borns. You do not need to consult your GP before you visit an osteopath, although you may wish to do so.
So, how good or bad is osteopathy for kids? Our systematic review wanted to find out. Specifically, the aim of this paper is to update our previous systematic review (SR) initially published in 2013 by critically evaluating the evidence for or against this treatment.
Eleven databases were searched (January 2012 to November 2021). Only randomized clinical trials (RCTs) of OMT in pediatric patients compared with any type of controls were considered. The Cochrane risk-of-bias tool was used. In addition, the quality of the evidence was rated using Grading of Recommendations, Assessment, Development and Evaluation (GRADE) criteria, as recommended by the Cochrane Collaboration.
Thirteen trials met the eligibility criteria, of which four could be subjected to a meta-analysis. The findings show that, in preterm infants, OMT has little or no effect on reducing the length of hospital stay (standardized mean difference (SMD) -0.03; 95% confidence interval (CI) -0.44 to 0.39; very low certainty of the evidence) when compared with usual care alone. Only one study (8.3%) was judged to have a low risk of bias and showed no effects of OMT on improving exclusive breastfeeding at one month. The methodological quality of RCTs published since 2013 has improved. However, adverse effects remain poorly reported.
We concluded that the quality of the primary trials of OMT has improved during recent years. However, the quality of the totality of the evidence remains low or very low. Therefore, the effectiveness of OMT for selected pediatric populations remains unproven.
These days, it is not often that I am the co-author of a systematic review. So, allow me to discuss one of my own papers for a change by making a few very brief points:
- Considering how many osteopaths treat children, the fact that only 13 trials exist is shameful. To me, it suggests that the osteopathic profession has little interest in research.
- The finding that adverse effects are poorly reported is even more shameful, in my view. It suggests that the few osteopaths who do some research don’t mind violating research ethics.
- The fact that overall our review fails to yield good evidence that osteopathy is effective for any pediatric condition is the most shameful finding of them all. It means that osteopaths are either not informed about the evidence for their own approach, or that they are informed but don’t give a hoot and treat kids regardless. In both cases, they behave unethically.
Cannabis use is a frequently-discussed subject, not just in the realm of so-called alternative medicine (SCAM). In general, SCAM advocates view it as an herbal medicine and recommend it for all sorts of conditions. They also often downplay the risks associated with cannabis use. Yet, these risks might be substantial.
Cannabis potency, defined as the concentration of Δ9-tetrahydrocannabinol (THC), has increased internationally, which could increase the risk of adverse health outcomes for cannabis users. The first systematic review of the association of cannabis potency with mental health and addiction was recently published in ‘The Lancet Psychiatry’.
The authors searched Embase, PsycINFO, and MEDLINE (from database inception to Jan 14, 2021). Included studies were observational studies of human participants comparing the association of high-potency cannabis (products with a higher concentration of THC) and low-potency cannabis (products with a lower concentration of THC), as defined by the studies included, with depression, anxiety, psychosis, or cannabis use disorder (CUD).
Of 4171 articles screened, 20 met the eligibility criteria:
- eight studies focused on psychosis,
- eight on anxiety,
- seven on depression,
- and six on CUD.
Overall, higher potency cannabis, relative to lower potency cannabis, was associated with an increased risk of psychosis and CUD. Evidence varied for depression and anxiety. The association of cannabis potency with CUD and psychosis highlights its relevance in healthcare settings, and for public health guidelines and policies on cannabis sales.
The authors concluded that standardisation of exposure measures and longitudinal designs are needed to strengthen the evidence of this association.
The fact that cannabis use increases the risk of psychosis has long been general knowledge. The notion that the risk increases with increased potency of cannabis seems entirely logical and is further supported by this systematic review. Perhaps it is time to educate the public and make cannabis users more aware of these risks, and perhaps it is time that SCAM proponents negate the harm cannabis can do.
Reports of serious complications of chiropractic manipulation keep on coming. Take this one, for instance:
My daughter went for a routine chiropractor appointment. Now she’s paralysed – 1:20 000 chiropractic neck manipulations result in stroke from vertebral artery dissection.
Or take a recent article by US neurosurgeons:
Cranio-cervical artery dissection (CeAD) is a common cause of cerebrovascular events in young subjects with no clear treatment strategy established. This study evaluated the incidence of major adverse cardiovascular events (MACE) in CeAD patients treated with and without stent placement. COMParative effectiveness of treatment options in cervical Artery diSSection (COMPASS) is a single high-volume center observational, retrospective longitudinal registry that enrolled consecutive CeAD patients over a 2-year period. Patients were ≥ 18 years of age with confirmed extra- or intracranial CeAD on imaging. Enrolled participants were followed for 1 year evaluating MACE as the primary endpoint.
One-hundred ten patients were enrolled (age 53 ± 15.9, 56% Caucasian, and 50% male, BMI 28.9 ± 9.2). Grade I, II, III, and IV blunt vascular injury was noted in 16%, 33%, 19%, and 32%, respectively. Predisposing factors were noted in the majority (78%), including
- sneezing,
- carrying a heavy load,
- chiropractic manipulation.
Stent was placed in 10 (10%) subjects (extracranial carotid n = 9; intracranial carotid n = 1; extracranial vertebral n = 1) at the physician’s discretion along with medical management. Reasons for stent placement were early development of high-grade stenosis or expanding pseudoaneurysm. Stented patients experienced no procedural or in-hospital complications and no MACE between discharge and 1 year follow up. CeAD patients treated with medical management only had 14% MACE at 1 year.
The authors concluded that in this single high-volume center cohort of CeAD patients, stenting was found to be beneficial, particularly with development of high-grade stenosis or expanding pseudoaneurysm. These results warrant confirmation by a randomized clinical trial.
Yes, I know: this study was not meant to investigate the link between chiropractic manipulations and CeAD. The finding that chiropractic manipulation is a predisposing factor for CeAD is entirely incidental. But it is an important finding nevertheless.
Chiropractors will laugh about the notion that manipulation is a risk factor akin to sneezing and thus try to trivialize the danger of their treatments. I would then point out that sneezing is unavoidable and fulfills a purpose. Chiropractic manipulations do neither.
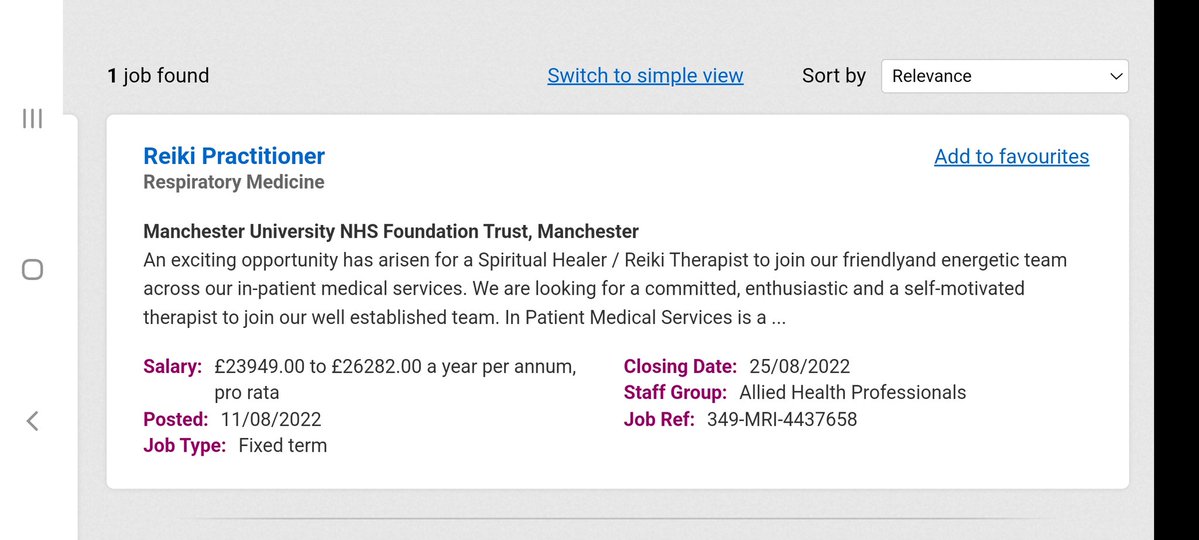
It has been reported by several sources that the NHS is advertising for a Reiki healer.
The NHS stated that “the responsibilities of a reiki healer include treating clients using energy principles … and activating the healing process.” The post is paid for by the Sam Buxton Sunflower Healing Trust (SBSHT) which states on its website:
The SBSHT healing therapists, who work within the NHS and other health areas, are proud to be part of a multi-disciplinary team of professionals to provide vital support cancer patients, their relatives and staff. Since 2006, the SBSHT has funded healers to work in NHS, and other health related areas to support cancer patients and their families. A key role of the SBSHT is to increase awareness within the UK of the importance of providing healing support to cancer patients and families. Another vital role is to generate the crucial funds needed to place more healers in NHS, and other health related areas, throughout the country. Complementary therapy (CT) is increasingly demanded and expected by patients undergoing cancer treatments. An increasing amount of research clearly demonstrates that CT is important to support patients through their conventional treatments. SBSHT is committed to providing funds to NHS hospitals and cancer centers to engage the services of a Reiki practitioner or Healer for cancer patients and their families
As a charity we are or have funded healer posts within the centres below.
- University College Hospital, London
- Addenbrookes Hospital, Cambridge
- Princess Alexandra Hospital, Epping
- Queen Elizabeth Hospital, Welwyn Garden City
- Derriford Hospital, Plymouth
- Wigan NHS Trust, Wigan
- St Josephs Hospice, London
- Eden Valley Hospice and Jigsaw Children’s Hospice, Carlisle
- St Mary’s Hospice, Ulverston and Barrow in Furness NHS Trust
- St Johns Hospice, Lancaster
- Kent and Canterbury Hospital, Canterbury
- Bristol Haematology and Oncology Centre, Bristol
- Rowcroft Hospice, Torquay
- The Lister Hospital, Stevenage
- Barnstaple NHS Trust
- Treliske Hospital, Cornwall
- Poole NHS Trust
- St Michaels Hospice, Herefordshire
The SBSHT was co-founded by Angie Buxton-King in memory of her son Sam, who died of Acute Myeloid Leukaemia in 1998 aged 10. She is a member of the ‘College of Psychic Studies’ which is “committed to serving the evolution of consciousness”. The College website states this:
We were founded in 1884 to support and encourage empirical research into the esoteric. Our programme has since broadened and diversified to meet rising demand and increasingly global interests.
However, our core values remain the same. We continue to shine a light on key themes including consciousness, intuition, self-development and meditation. Our courses, workshops, talks and special events provide a safe and inclusive space in which to explore the full spectrum of human potential under the careful guidance of our expert tutors.
The College offers all sorts of courses; I was particularly fascinated by this one: “Alchemise Your Energy Through Dowsing“.
__________________
Now, one could easily claim that there is nothing wrong with reiki healers invading the NHS; after all, they are funded by a charitable trust at no cost to the taxpayer.
Yet, I disagree!
Reiki healing is implausible and ineffective nonsense. As such it is by no means harmless. Employing such healers in the NHS sends out a strong signal that undermines the principles of rational thinking and evidence-based medicine. If the NHS truly does not value these principles, I suggest they also fill the chronic gaps in ambulance services by flying carpets.
Trevor Zierke is a D.C. who published several videos that have gone viral after saying that “literally 99% of my profession” is a scam. “When I say almost all the usual lines chiropractors tell you are lies, I mean almost all of them,” he stated. Zierke then went on to give examples of issues chiropractors allegedly make up, including someone’s spine being “misaligned,” tension on nerves causing health problems, and someone having back pain because their hips are off-center. “Almost all of these aren’t true,” he concluded.
In a follow-up video, he claimed that the reasons most people are told they need to go to a chiropractor are “overblown or just flat out lies proven wrong by research.” He also noted that, while there are many scams, that “doesn’t mean you can’t get help from a chiropractor.”
In a third TikTok video, Zierke offered some valid reasons to see a chiropractor. He said that one can seek help from a chiropractor if one has musculoskeletal pain that has been ongoing for more than one to two days, and that’s about it. He stated that issues that a chiropractor couldn’t really fix include “GI pain, hormonal issues, nutrition,” among others.
In comments, users were largely supportive of Zierke’s message.
One said: “As a physiotherapist, I’ve been trying to tell this but I don’t want to like offend any chiropractor in doing so,” a commenter shared.
“Working in a chiropractic office, this is fair,” a further user wrote. “I have issues that I know an adjustment will help & other pain that would be better stretched/released.”
In an email, Zierke reiterated the intention of his videos: “I would just like to clarify that chiropractors, in general, are not a scam or are inherently scammers (I myself am a practicing chiropractor), but rather a lot of very popular sales tactics, phrases, and wording used to imply patients need treatment, and methods of treatment, have never been proven to be true,” he explained. “When chiropractors say & use these methods stating things that are not factually true—I believe it’s scammy behavior and practices. There are still a lot of very good, honest, and integral chiropractors out there,” he concluded. “They can provide a lot of help and relief to patients. But that’s unfortunately not the majority, and I’ve heard too many stories of people falling victim to some of these scam-like tactics from bad apple chiropractors.”
None of what DC Zierke said can surprise those who have been following my blog. On the contrary, I could add a few recent posts to his criticism of chiropractic, for example:
- Pediatric chiropractic seems to be on the rise
- Catastrophic injuries after chiropractic treatment
- Chiropractic: “a safe form of treatment”?
- Malpractice Litigation Involving Chiropractic Spinal Manipulation
- Best Practices for the Chiropractic Care of Children
- No effect from adding chiropractic manipulations to exercises for neck pain
- Hurray! The new professional standard by the General Chiropractic Council protects UK chiropractors
- Manual therapy (mainly chiropractic and osteopathy) does not have clinically relevant effects on back pain compared with sham treatment
- Chiropractic Paediatric Courses … it is high time to stop this dangerous nonsense
- Chiropractic ‘subluxation’ is by no means a notion of the past
- Another indirect risk of chiropractic
- And again: chiropractic for infant colic
- Chiropractic misinformation during the COVID-19 pandemic
- The lack of chiropractic ethics: “valid consent was not obtained in a single case”
I rest my case.
About a year ago, I reported last on the situation of homeopathy in France. Now it might be time for another update. The end of the reimbursement of homeopathy was, of course, a heavy blow for the laboratories concerned, especially Boiron and Weleda.
Are these firms now going bust?
Is the French public missing homeopathy?
The cessation of reimbursement took place in two steps: in 2020, the reimbursement rate was reduced to 15 % and expired completely in 2021. The new director of Weleda France, Ludovic Rassat, explains that, in 2020, when the reimbursement was reduced to 15 %, the impact on sales was just 20 %. The decrease was limited because of the supplementary health insurance which 80 % of French people have still supplemented the reimbursement up to 100 %. In 2021, this generosity stopped and the reimbursement fell from 100 to 0 %. This led to a 60 % drop in sales and to losses of 13 million Euros for Weleda France.
According to an Ipsos survey commissioned by Boiron Laboratories in October 2018, 70 % of all French used homeopathy to relieve their first symptoms, 74 % thought homeopathic remedies were effective and 71 % thought homeopathy was a good complement to conventional treatments. One might, therefore, have assumed that French consumers would continue using their beloved remedies despite the cessation of reimbursement. However, this was not the case. The most obvious explanation for this phenomenon, I think, is that the above-mentioned survey had generated false-positive results and that people correctly judged homeopathic remedies to be superfluous.
Faced with unsustainable losses, the French manufacturers of homeopathic products are now forced to react. A press release by Weleda France from 4 July 2022 stated that “This project would result in the discontinuation of pharmaceutical production and medical information in France and the closure of the Weleda division. This would result in the cessation of production activities at the Huningue site and an adjustment of the organisation of activities at headquarters. In total, 127 jobs could be cut at Weleda France.” If this step is taken as planned, Weleda France will have to earn its money purely on its cosmetic and anthroposophical products, according to the director.
In 2019, Laboratoires Boiron owned 4 production laboratories and 28 distribution facilities in France. In March 2020, the company announced that it had decided to cut 646 jobs in France and close 13 of its 31 sites, due to the poor economic results that followed the cessation of reimbursement of its products by the social security system. Following the decision by the Minister of Health, Agnès Buzyn, to stop the reimbursement of homeopathic preparations by the social security system, Boiron announced that the Montrichard site in the Loir-et-Cher region had not managed to find a buyer. As a result, the site, which employed around 80 people, closed on 31 December 2021.
And the French consumers?
Are they missing homeopathy?
Are they suffering from homeopathy withdrawal?
Are they more frequently ill without homeopathy?
Are they switching to more expensive conventional drugs?
I currently spend much of my time in France and cannot say that I have noticed any of this. On the contrary, most people I talk to are delighted that homeopathy is no longer reimbursed. But this is no evidence, of course. I am unable to find any reliable data to answer the above questions.
When the French health minister decided against homeopathy two years ago, she said: “It’s possible to leave the doctor’s office without a prescription! Let’s take advantage of this debate on homeopathy to reflect more broadly on our use of medicine. The ultimate goal is to consume less.” She was correct, it seems.
It has been reported that a recent inspection from the Care Quality Commission (CQC) found that the diagnostic imaging service at AECC University College in Parkwood Road, Bournemouth, requires improvement in three out of four areas – including patient safety. This is surprising not least because the AECC prides itself on being “a leading higher education institution in healthcare disciplines, nationally and internationally recognised for quality and excellence.” 
The unannounced inspection in May this year resulted in several demands for the service to improve upon. For example, the CQC report said staff “did not receive all of the training they needed to keep patients safe” and that patient chaperones “did not receive chaperone training”. Moreover, managers were reported as not always ensuring staff were competent to operate certain equipment. In fact, there was no record of staff competencies which meant inspectors “could not tell if staff had been trained to use equipment”. General cleanliness was also found lacking in relation to certain procedures, namely no sink in any of the site’s nine ultrasound rooms (including those for transvaginal scans) – meaning staff carrying out ultrasound scanning did not have access to a clinical handwashing facility.
The CQC states on its website that it “is the independent regulator of health and adult social care in England. We make sure health and social care services provide people with safe, effective, compassionate, high-quality care and we encourage care services to improve. We monitor, inspect and regulate services. Then we publish what we find, including performance ratings, to help people choose care. Where we find poor care, we will use our powers to take action.”
No doubt, these are laudable aims. What I find, however, disappointing is that the CQC’s inspection of the AECC did not question the nature of some of the courses taught by the AECC. Earlier this year, I reported in a blog post that the AECC has announced a new MSc ‘Musculoskeletal Paediatric Health‘. This motivated me to look into the evidence for such a course. This is what I found with several Medline searches (date of the review on chiropractic for any pediatric conditions, followed by its conclusion + link [so that the reader can look up the evidence]):
2008
I am unable to find convincing evidence for any of the above-named conditions.
2009
Previous research has shown that professional chiropractic organisations ‘make claims for the clinical art of chiropractic that are not currently available scientific evidence…’. The claim to effectively treat otitis seems to
be one of them. It is time now, I think, that chiropractors either produce the evidence or abandon the claim.
2009
The … evidence is neither complete nor, in my view, “substantial.”
2010
2018
What seems to emerge is rather disappointing:
- There are no really new reviews.
- Most of the existing reviews are not on musculoskeletal conditions.
- All of the reviews cast considerable doubt on the notion that chiropractors should go anywhere near children.
But perhaps I was too ambitious. Perhaps there are some new rigorous clinical trials of chiropractic for musculoskeletal conditions. A few further searches found this (again year and conclusion):
2019
2018
I might have missed one or two trials because I only conducted rather ‘rough and ready’ searches, but even if I did: would this amount to convincing evidence? Would it be good science?
No! and No!
So, why does the AECC offer a Master of Science in ‘Musculoskeletal Paediatric Health’?
____________________
Isn’t that a question the CQC should have asked?
The ‘My Resilience in Adolescence (MYRIAD) Trial’evaluated the effectiveness and cost-effectiveness of SBMT compared with teaching-as-usual (TAU).
MYRIAD was a parallel group, cluster-randomised controlled trial. Eighty-five eligible schools consented and were randomized 1:1 to TAU (43 schools, 4232 students) or SBMT (42 schools, 4144 students), stratified by school size, quality, type, deprivation, and region. Schools and students (mean (SD); age range=12.2 (0.6); 11–14 years) were broadly UK population-representative. Forty-three schools (n=3678 pupils; 86.9%) delivering SBMT, and 41 schools (n=3572; 86.2%) delivering TAU, provided primary end-point data. SBMT comprised 10 lessons of psychoeducation and mindfulness practices. TAU comprised standard social-emotional teaching. Participant-level risk for depression, social-emotional-behavioural functioning and well-being at 1 year follow-up were the co-primary outcomes. Secondary and economic outcomes were included.
 An analysis of the data from 84 schools (n=8376 participants) found no evidence that SBMT was superior to TAU at 1 year. Standardised mean differences (intervention minus control) were: 0.005 (95% CI −0.05 to 0.06) for risk for depression; 0.02 (−0.02 to 0.07) for social-emotional-behavioural functioning; and 0.02 (−0.03 to 0.07) for well-being. SBMT had a high probability of cost-effectiveness (83%) at a willingness-to-pay threshold of £20 000 per quality-adjusted life year. No intervention-related adverse events were observed.
An analysis of the data from 84 schools (n=8376 participants) found no evidence that SBMT was superior to TAU at 1 year. Standardised mean differences (intervention minus control) were: 0.005 (95% CI −0.05 to 0.06) for risk for depression; 0.02 (−0.02 to 0.07) for social-emotional-behavioural functioning; and 0.02 (−0.03 to 0.07) for well-being. SBMT had a high probability of cost-effectiveness (83%) at a willingness-to-pay threshold of £20 000 per quality-adjusted life year. No intervention-related adverse events were observed.
The authors concluded that the findings do not support the superiority of SBMT over TAU in promoting mental health in adolescence.
Even though the results are negative, MYRIAD must be praised for its scale and rigor, and for highlighting the importance of large, well-designed studies before implementing measures of this kind on a population basis. Co-author Tim Dalgliesh, director of the Cambridge Centre for Affective Disorders, said: “For policymakers, it’s not just about coming up with a great intervention to teach young people skills to deal with their stress. You also have to think about where that stress is coming from in the first place.”
“There had been some hope for an easy solution, especially for those who might develop depression,” says Til Wykes, head of the School of Mental Health and Psychological Sciences at the Institute of Psychiatry, Psychology, and Neuroscience, King’s College London. “There may be lots of reasons for developing depression, and these are probably not helped by mindfulness,” she says. “We need more research on other potential factors that might be modified, and perhaps this would provide a more targeted solution to this problem.”
Personally, I feel that mindfulness has been hyped in recent years. Much of the research that seemed to support it was less than rigorous. What is now needed is a realistic approach based on sound evidence and critical thinking.
For many years, Dr. Natalie Grams-Nobmann provided evidence-based medical information on social media – including on homeopathy, other forms of so-called alternative medicine, and more recently the COVID pandemic. These activities deservedly earned her plenty of praise but sadly they also made her the target of intolerant, occasionally aggressive people who disagree with the evidence. As I mentioned in yesterday’s post, Natalie has recently deleted her Twitter account. To explain her decision, she gave an interview to Marc Zimmer, MDR AKTUELL. With Natalie’s permission, I have translated sections of it and re-publish them here:
Q: What do you think about the case of your Austrian colleague?
A: The case has affected and frightened me terribly. I followed Kellermayr’s work and everything that came afterward. It is simply a terrible example of how little protection one has as a doctor or vaccination educator on social media. It also is a terrible example of how this “hate” does not stay in the realm of social media but spills over into real life. And that we have nothing to counter this “hate”.
Q: You yourself have also drawn consequences and deleted your Twitter account. Can you explain this step?
A: After seven years of vaccination education and medical education on social media, I thought I couldn’t take it anymore. I can’t stand looking into this hell where people celebrate the death of another human being, the suicide of another human being – and see that as an admission of guilt of this really threatened and persecuted doctor and rise above it like that. I think that when even the death of a human being is no longer free of gloating and hatred, then ideology is above everything. I didn’t know how to deal with it anymore. And, of course, it also scared me. I think my death would be celebrated in the same way, and I find that terribly frightening in human terms.
Q: To what extent have you experienced threats so far?
A: … I’ve experienced an incredible amount of different forms of hate – be it threats, insults, slander, or persecution. This has also spilled over into real life for me. I have sometimes given lectures under police protection. I am very glad that it is still sensible to wear a mask in public spaces… I think that in some cases it really is a life-threatening fear that you have to endure when you speak out on social or other media about vaccination protection or about protective measures. A lot of what you hear has to be reported and followed up. It is not the case that the internet is a lawless space or that my inbox simply has to swallow every insult in the world…
Q: You mentioned the platforms. What about politics? Do you feel supported enough by it and by the authorities?
A: No, not at all and that was certainly the case with the Austrian colleague. In desperation and panic, people turn to the police, and of course, there are individual female officers who react in an excellent way. But I have also heard things like: “Well, then don’t go out in public. Why do you do that? You’re doing it voluntarily, so you have to put up with it”. Or they say that it’s freedom of expression, that everyone is allowed to say anything… If no more discourse is possible, what am I supposed to do? I would like to be able to ensure that I remain objective, that I provide information and do not insult anyone. At the moment I simply don’t see myself in a position to do that because of the many threats.
Q: What do you wish from politics?
A: I would like politicians to draw the right conclusions from this: not just those who shout the loudest must be listened to. The ones who are silenced should be heard as well.
This “silencing” that I have been following throughout the pandemic is a terrible thing. The best and most factual discussants are disappearing more and more from the platforms. I haven’t insulted or threatened or unobjectively excoriated anyone in all my time on social media. Of course, you are allowed to make a joke or use satire. But you’re not allowed to put another person down. And the very people who have always managed to remain objective – despite the well-known strains during the pandemic – are now leaving and this should alarm us all.
____________________
I do, of course, understand and respect Natalie’s decisions. Nevertheless, I am sad that she is partly withdrawing from public life. I feel that, in these difficult times, we need everyone who can contribute to more responsible information for the public. We must try to balance irrationality with rationality. Natalie is particularly gifted in doing just that (she is much more gentle and empathetic in the face of adversity than I, for instance). My hope, therefore, is that things improve, hatred recedes, and she is able to return to public life soon. Regardless of what she decides, I wish her well.