education
Low back pain (LBP) affects almost all of us at some stage. It is so common that it has become one of the most important indications for most forms of so-called alternative medicine (SCAM). In the discussions about the value (or otherwise) of SCAMs for LBP, we sometimes forget that there are many conventional medical options to treat LBP. It is therefore highly relevant to ask how effective they are. This overview aimed to summarise the evidence from Cochrane Reviews of the efficacy, effectiveness, and safety of systemic pharmacological interventions for adults with non‐specific LBP.
The Cochrane Database of Systematic Reviews was searched from inception to 3 June 2021, to identify reviews of randomised controlled trials (RCTs) that investigated systemic pharmacological interventions for adults with non‐specific LBP. Two authors independently assessed eligibility, extracted data, and assessed the quality of the reviews and certainty of the evidence using the AMSTAR 2 and GRADE tools. The review focused on placebo comparisons and the main outcomes were pain intensity, function, and safety.
Seven Cochrane Reviews that included 103 studies (22,238 participants) were included. There was high confidence in the findings of five reviews, moderate confidence in one, and low confidence in the findings of another. The reviews reported data on six medicines or medicine classes: paracetamol, non‐steroidal anti‐inflammatory drugs (NSAIDs), muscle relaxants, benzodiazepines, opioids, and antidepressants. Three reviews included participants with acute or sub‐acute LBP and five reviews included participants with chronic LBP.
Acute LBP
Paracetamol
There was high‐certainty evidence for no evidence of difference between paracetamol and placebo for reducing pain intensity (MD 0.49 on a 0 to 100 scale (higher scores indicate worse pain), 95% CI ‐1.99 to 2.97), reducing disability (MD 0.05 on a 0 to 24 scale (higher scores indicate worse disability), 95% CI ‐0.50 to 0.60), and increasing the risk of adverse events (RR 1.07, 95% CI 0.86 to 1.33).
NSAIDs
There was moderate‐certainty evidence for a small between‐group difference favouring NSAIDs compared to placebo at reducing pain intensity (MD ‐7.29 on a 0 to 100 scale (higher scores indicate worse pain), 95% CI ‐10.98 to ‐3.61), high‐certainty evidence for a small between‐group difference for reducing disability (MD ‐2.02 on a 0‐24 scale (higher scores indicate worse disability), 95% CI ‐2.89 to ‐1.15), and very low‐certainty evidence for no evidence of an increased risk of adverse events (RR 0.86, 95% CI 0. 63 to 1.18).
Muscle relaxants and benzodiazepines
There was moderate‐certainty evidence for a small between‐group difference favouring muscle relaxants compared to placebo for a higher chance of pain relief (RR 0.58, 95% CI 0.45 to 0.76), and higher chance of improving physical function (RR 0.55, 95% CI 0.40 to 0.77), and increased risk of adverse events (RR 1.50, 95% CI 1. 14 to 1.98).
Opioids
None of the included Cochrane Reviews aimed to identify evidence for acute LBP.
Antidepressants
No evidence was identified by the included reviews for acute LBP.
Chronic LBP
Paracetamol
No evidence was identified by the included reviews for chronic LBP.
NSAIDs
There was low‐certainty evidence for a small between‐group difference favouring NSAIDs compared to placebo for reducing pain intensity (MD ‐6.97 on a 0 to 100 scale (higher scores indicate worse pain), 95% CI ‐10.74 to ‐3.19), reducing disability (MD ‐0.85 on a 0‐24 scale (higher scores indicate worse disability), 95% CI ‐1.30 to ‐0.40), and no evidence of an increased risk of adverse events (RR 1.04, 95% CI ‐0.92 to 1.17), all at intermediate‐term follow‐up (> 3 months and ≤ 12 months postintervention).
Muscle relaxants and benzodiazepines
There was low‐certainty evidence for a small between‐group difference favouring benzodiazepines compared to placebo for a higher chance of pain relief (RR 0.71, 95% CI 0.54 to 0.93), and low‐certainty evidence for no evidence of difference between muscle relaxants and placebo in the risk of adverse events (RR 1.02, 95% CI 0.67 to 1.57).
Opioids
There was high‐certainty evidence for a small between‐group difference favouring tapentadol compared to placebo at reducing pain intensity (MD ‐8.00 on a 0 to 100 scale (higher scores indicate worse pain), 95% CI ‐1.22 to ‐0.38), moderate‐certainty evidence for a small between‐group difference favouring strong opioids for reducing pain intensity (SMD ‐0.43, 95% CI ‐0.52 to ‐0.33), low‐certainty evidence for a medium between‐group difference favouring tramadol for reducing pain intensity (SMD ‐0.55, 95% CI ‐0.66 to ‐0.44) and very low‐certainty evidence for a small between‐group difference favouring buprenorphine for reducing pain intensity (SMD ‐0.41, 95% CI ‐0.57 to ‐0.26).
There was moderate‐certainty evidence for a small between‐group difference favouring strong opioids compared to placebo for reducing disability (SMD ‐0.26, 95% CI ‐0.37 to ‐0.15), moderate‐certainty evidence for a small between‐group difference favouring tramadol for reducing disability (SMD ‐0.18, 95% CI ‐0.29 to ‐0.07), and low‐certainty evidence for a small between‐group difference favouring buprenorphine for reducing disability (SMD ‐0.14, 95% CI ‐0.53 to ‐0.25).
There was low‐certainty evidence for a small between‐group difference for an increased risk of adverse events for opioids (all types) compared to placebo; nausea (RD 0.10, 95% CI 0.07 to 0.14), headaches (RD 0.03, 95% CI 0.01 to 0.05), constipation (RD 0.07, 95% CI 0.04 to 0.11), and dizziness (RD 0.08, 95% CI 0.05 to 0.11).
Antidepressants
There was low‐certainty evidence for no evidence of difference for antidepressants (all types) compared to placebo for reducing pain intensity (SMD ‐0.04, 95% CI ‐0.25 to 0.17) and reducing disability (SMD ‐0.06, 95% CI ‐0.40 to 0.29).
The authors concluded as follows: we found no high‐ or moderate‐certainty evidence that any investigated pharmacological intervention provided a large or medium effect on pain intensity for acute or chronic LBP compared to placebo. For acute LBP, we found moderate‐certainty evidence that NSAIDs and muscle relaxants may provide a small effect on pain, and high‐certainty evidence for no evidence of difference between paracetamol and placebo. For safety, we found very low‐ and high‐certainty evidence for no evidence of difference with NSAIDs and paracetamol compared to placebo for the risk of adverse events, and moderate‐certainty evidence that muscle relaxants may increase the risk of adverse events. For chronic LBP, we found low‐certainty evidence that NSAIDs and very low‐ to high‐certainty evidence that opioids may provide a small effect on pain. For safety, we found low‐certainty evidence for no evidence of difference between NSAIDs and placebo for the risk of adverse events, and low‐certainty evidence that opioids may increase the risk of adverse events.
This is an important overview, in my opinion. It confirms what I and others have been stating for decades: WE CURRENTLY HAVE NO IDEAL SOLUTION TO LBP.
This is regrettable but true. It begs the question of what one should recommend to LBP sufferers. Here too, I have to repeat myself: (apart from staying as active as possible) the optimal therapy is the one that has the most favourable risk/benefit profile (and does not cost a fortune). And this option is not drugs, chiropractic, osteopathy, acupuncture, or any other SCAM – it is (physio)therapeutic exercise which is cheap, safe, and (mildly) effective.
During the coronavirus disease 2019 pandemic, Ayurvedic herbal supplements and homeopathic remedies were promoted as immune boosters (IBs) and disease-preventive agents. This happened in most parts of the world but nowhere more intensely than in India.
The present study examined the clinical outcomes among patients with chronic liver disease who presented with complications of portal hypertension or liver dysfunction temporally associated with the use of IBs in the absence of other competing causes. This Indian single-center retrospective observational cohort study included patients with chronic liver disease admitted for the evaluation and management of jaundice, ascites, or hepatic encephalopathy temporally associated with the consumption of IBs and followed up for 180 days. Chemical analysis was performed on the retrieved IBs.
From April 2020 to May 2021, 1022 patients with cirrhosis were screened, and 178 (19.8%) were found to have consumed complementary and alternative medicines. Nineteen patients with cirrhosis (10.7%), jaundice, ascites, hepatic encephalopathy, or their combination related to IBs use were included. The patients were predominantly male (89.5%). At admission, 14 (73.75%) patients had jaundice, 9 (47.4%) had ascites, 2 (10.5%) presented with acute kidney injury, and 1 (5.3%) had overt encephalopathy. Eight patients (42.1%) died at the end of the follow-up period. Hepatic necrosis and portal-based neutrophilic inflammation were the predominant features of liver biopsies.
Ten samples of IBs, including locally made ashwagandha powder, giloy juice, Indian gooseberry extracts, pure giloy tablets, multiherbal immune-boosting powder, other multiherbal tablets, and the homeopathic remedy, Arsenicum album 30C, were retrieved from our study patients. Samples were analyzed for potential hepatotoxic prescription drugs, known hepatotoxic adulterants, pesticides, and insecticides, which were not present in any of the samples. Detectable levels of arsenic (40%), lead (60%), and mercury (60%) were found in the samples analyzed. A host of other plant-derived compounds, industrial solvents, chemicals, and anticoagulants was identified using GC–MS/MS. These include glycosides, terpenoids, phytosteroids, and sterols, such as sitosterol, lupeol, trilinolein, hydroxy menthol, methoxyphenol, butyl alcohol, and coumaran derivatives.
The authors concluded that Ayurvedic and Homeopathic supplements sold as IBs potentially cause the worsening of preexisting liver disease. Responsible dissemination of scientifically validated, evidence-based medical health information from regulatory bodies and media may help ameliorate this modifiable liver health burden.
The authors comment that Ayurvedic herbal supplements and homeopathic remedies sold as IBs, potentially induce idiosyncratic liver injury in patients with preexisting liver disease. Using such untested advertised products can lead to the worsening of CLD in the form of liver failure or portal hypertension events, which are associated with a high risk of mortality compared to those with severe AH-related liver decompensation in the absence of timely liver transplantation. Severe mixed portal inflammation and varying levels of hepatic necrosis are common findings on liver histopathology in IB-related liver injury. Health regulatory authorities and print and visual media must ensure the dissemination of responsible and factual scientific evidence-based information on herbal and homeopathic “immune boosters” and health supplements to the public, specifically to the at-risk patient population.
Research by the Milner Center for Evolution at the University of Bath, U.K., along with colleagues at the Universities of Oxford and Aberdeen, found that trust in scientists has hugely increased since the COVID-19 pandemic. The study also found that people were more likely to take the COVID-19 vaccine if their trust in the science had increased.
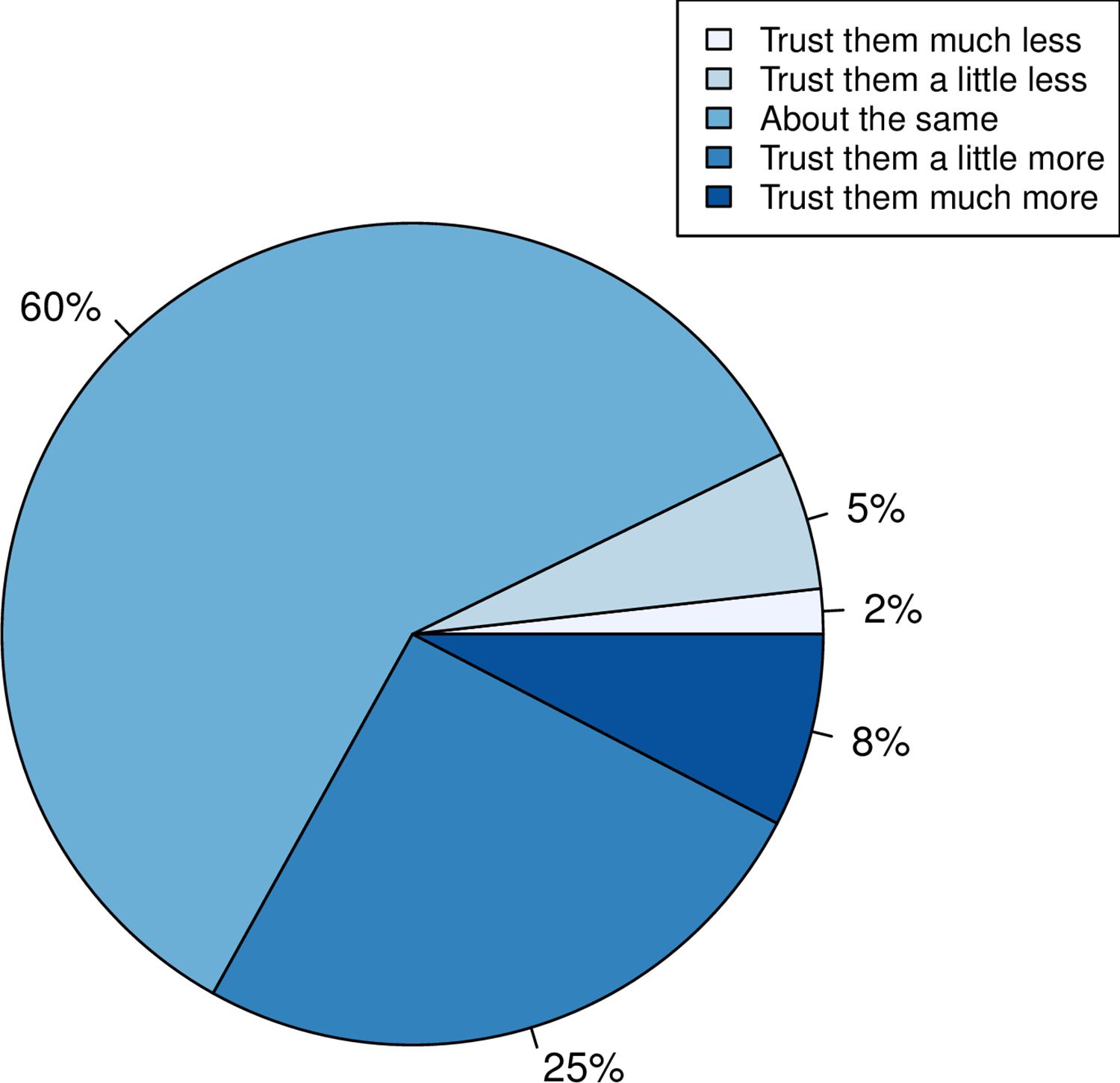
Using data from a survey of more than 2,000 U.K. adults commissioned by the Genetics Society, the team asked individuals whether their trust in scientists had gone up, down, or stayed the same.
- A third of people reported that their trust in scientists had gone up.
- When Pfizer, a company that made COVID-19 vaccines, was used as an example of the pharma industry, more people reported a positive response than when GlaxoSmithKline, a company not associated with the COVID-19 vaccine, was mentioned.
- The researchers also found that people who reported holding a negative view of science before the pandemic had become even more negative.
- People reporting increased trust were most likely to take the COVID-19 vaccine.
- Those preferring not to do so reported a decline in trust.
This is an interesting study with relevance to many discussions we had on this blog. I recommend reading it in full. Here are the abstract and link to the paper:
While attempts to promote acceptance of well-evidenced science have historically focused on increasing scientific knowledge, it is now thought that for acceptance of science, trust in, rather than simply knowledge of, science is foundational. Here we employ the COVID-19 pandemic as a natural experiment on trust modulation as it has enabled unprecedented exposure of science. We ask whether trust in science has on the average altered, whether trust has changed the same way for all and, if people have responded differently, what predicts these differences? We 1) categorize the nature of self-reported change in trust in “scientists” in a random sample of over 2000 UK adults after the introduction of the first COVID vaccines, 2) ask whether any reported change is likely to be real through consideration of both a negative control and through experiment, and 3) address what predicts change in trust considering sex, educational attainment, religiosity, political attitude, age and pre-pandemic reported trust. We find that many more (33%) report increased trust towards “scientists” than report decreased trust (7%), effects of this magnitude not being seen in negative controls. Only age and prior degree of trust predict change in trust, the older population increasing trust more. The prior degree of trust effect is such that those who say they did not trust science prior to the pandemic are more likely to report becoming less trusting, indicative of both trust polarization and a backfire effect. Since change in trust is predictive of willingness to have a COVID-19 vaccine, it is likely that these changes have public health consequences.
Sure, the LP is dangerous nonsense, but this begs the question of whether so-called alternative medicine (SCAM) has anything to offer for patients suffering from ME/CFS. If the LP story tells us anything, then it must be this: we should not trust single trials, particularly if they seem dodgy. In other words, we should look at systematic reviews that synthesize ALL clinical trials and evaluate them critically.
To locate this type of evidence I conducted several Medline searches and found several recent systematic reviews that address the issue:
Context: A variety of interventions have been used in the treatment and management of chronic fatigue syndrome (CFS). Currently, debate exists among health care professionals and patients about appropriate strategies for management.
Objective: To assess the effectiveness of all interventions that have been evaluated for use in the treatment or management of CFS in adults or children.
Data sources: Nineteen specialist databases were searched from inception to either January or July 2000 for published or unpublished studies in any language. The search was updated through October 2000 using PubMed. Other sources included scanning citations, Internet searching, contacting experts, and online requests for articles.
Study selection: Controlled trials (randomized or nonrandomized) that evaluated interventions in patients diagnosed as having CFS according to any criteria were included. Study inclusion was assessed independently by 2 reviewers. Of 350 studies initially identified, 44 met inclusion criteria, including 36 randomized controlled trials and 8 controlled trials.
Data extraction: Data extraction was conducted by 1 reviewer and checked by a second. Validity assessment was carried out by 2 reviewers with disagreements resolved by consensus. A qualitative synthesis was carried out and studies were grouped according to type of intervention and outcomes assessed.
Data synthesis: The number of participants included in each trial ranged from 12 to 326, with a total of 2801 participants included in the 44 trials combined. Across the studies, 38 different outcomes were evaluated using about 130 different scales or types of measurement. Studies were grouped into 6 different categories. In the behavioral category, graded exercise therapy and cognitive behavioral therapy showed positive results and also scored highly on the validity assessment. In the immunological category, both immunoglobulin and hydrocortisone showed some limited effects but, overall, the evidence was inconclusive. There was insufficient evidence about effectiveness in the other 4 categories (pharmacological, supplements, complementary/alternative, and other interventions).
Conclusions: Overall, the interventions demonstrated mixed results in terms of effectiveness. All conclusions about effectiveness should be considered together with the methodological inadequacies of the studies. Interventions which have shown promising results include cognitive behavioral therapy and graded exercise therapy. Further research into these and other treatments is required using standardized outcome measures.
Introduction: Chronic fatigue syndrome (CFS) affects between 0.006% and 3% of the population depending on the criteria of definition used, with women being at higher risk than men.
Methods and outcomes: We conducted a systematic review and aimed to answer the following clinical question: What are the effects of treatments for chronic fatigue syndrome? We searched: Medline, Embase, The Cochrane Library, and other important databases up to March 2010 (Clinical Evidence reviews are updated periodically; please check our website for the most up-to-date version of this review). We included harms alerts from relevant organisations such as the US Food and Drug Administration (FDA) and the UK Medicines and Healthcare products Regulatory Agency (MHRA).
Results: We found 46 systematic reviews, RCTs, or observational studies that met our inclusion criteria. We performed a GRADE evaluation of the quality of evidence for interventions.
Conclusions: In this systematic review we present information relating to the effectiveness and safety of the following interventions: antidepressants, cognitive behavioural therapy (CBT), corticosteroids, dietary supplements, evening primrose oil, galantamine, graded exercise therapy, homeopathy, immunotherapy, intramuscular magnesium, oral nicotinamide adenine dinucleotide, and prolonged rest.
Background: Throughout the world, patients with chronic diseases/illnesses use complementary and alternative medicines (CAM). The use of CAM is also substantial among patients with diseases/illnesses of unknown aetiology. Chronic fatigue syndrome (CFS), also termed myalgic encephalomyelitis (ME), is no exception. Hence, a systematic review of randomised controlled trials of CAM treatments in patients with CFS/ME was undertaken to summarise the existing evidence from RCTs of CAM treatments in this patient population.
Methods: Seventeen data sources were searched up to 13th August 2011. All randomised controlled trials (RCTs) of any type of CAM therapy used for treating CFS were included, with the exception of acupuncture and complex herbal medicines; studies were included regardless of blinding. Controlled clinical trials, uncontrolled observational studies, and case studies were excluded.
Results: A total of 26 RCTs, which included 3,273 participants, met our inclusion criteria. The CAM therapy from the RCTs included the following: mind-body medicine, distant healing, massage, tuina and tai chi, homeopathy, ginseng, and dietary supplementation. Studies of qigong, massage and tuina were demonstrated to have positive effects, whereas distant healing failed to do so. Compared with placebo, homeopathy also had insufficient evidence of symptom improvement in CFS. Seventeen studies tested supplements for CFS. Most of the supplements failed to show beneficial effects for CFS, with the exception of NADH and magnesium.
Conclusions: The results of our systematic review provide limited evidence for the effectiveness of CAM therapy in relieving symptoms of CFS. However, we are not able to draw firm conclusions concerning CAM therapy for CFS due to the limited number of RCTs for each therapy, the small sample size of each study and the high risk of bias in these trials. Further rigorous RCTs that focus on promising CAM therapies are warranted.
Background: There is no curative treatment for chronic fatigue syndrome (CFS). Traditional Chinese medicine (TCM) is widely used in the treatment of CFS in China.
Objective: To evaluate the effectiveness and safety of TCM for CFS.
Methods: The protocol of this review is registered at PROSPERO. We searched six main databases for randomized clinical trials (RCTs) on TCM for CFS from their inception to September 2013. The Cochrane risk of bias tool was used to assess the methodological quality. We used RevMan 5.1 to synthesize the results.
Results: 23 RCTs involving 1776 participants were identified. The risk of bias of the included studies was high. The types of TCM interventions varied, including Chinese herbal medicine, acupuncture, qigong, moxibustion, and acupoint application. The results of meta-analyses and several individual studies showed that TCM alone or in combination with other interventions significantly alleviated fatigue symptoms as measured by Chalder’s fatigue scale, fatigue severity scale, fatigue assessment instrument by Joseph E. Schwartz, Bell’s fatigue scale, and guiding principle of clinical research on new drugs of TCM for fatigue symptom. There was no enough evidence that TCM could improve the quality of life for CFS patients. The included studies did not report serious adverse events.
Conclusions: TCM appears to be effective to alleviate the fatigue symptom for people with CFS. However, due to the high risk of bias of the included studies, larger, well-designed studies are needed to confirm the potential benefit in the future.
Background: As the etiology of chronic fatigue syndrome (CFS) is unclear and the treatment is still a big issue. There exists a wide range of literature about acupuncture and moxibustion (AM) for CFS in traditional Chinese medicine (TCM). But there are certain doubts as well in the effectiveness of its treatment due to the lack of a comprehensive and evidence-based medical proof to dispel the misgivings. Current study evaluated systematically the effectiveness of acupuncture and moxibustion treatments on CFS, and clarified the difference among them and Chinese herbal medicine, western medicine and sham-acupuncture.
Methods: We comprehensively reviewed literature including PubMed, EMBASE, Cochrane library, CBM (Chinese Biomedical Literature Database) and CNKI (China National Knowledge Infrastructure) up to May 2016, for RCT clinical research on CFS treated by acupuncture and moxibustion. Traditional direct meta-analysis was adopted to analyze the difference between AM and other treatments. Analysis was performed based on the treatment in experiment and control groups. Network meta-analysis was adopted to make comprehensive comparisons between any two kinds of treatments. The primary outcome was total effective rate, while relative risks (RR) and 95% confidence intervals (CI) were used as the final pooled statistics.
Results: A total of 31 randomized controlled trials (RCTs) were enrolled in analyses. In traditional direct meta-analysis, we found that in comparison to Chinese herbal medicine, CbAM (combined acupuncture and moxibustion, which meant two or more types of acupuncture and moxibustion were adopted) had a higher total effective rate (RR (95% CI), 1.17 (1.09 ~ 1.25)). Compared with Chinese herbal medicine, western medicine and sham-acupuncture, SAM (single acupuncture or single moxibustion) had a higher total effective rate, with RR (95% CI) of 1.22 (1.14 ~ 1.30), 1.51 (1.31-1.74), 5.90 (3.64-9.56). In addition, compared with SAM, CbAM had a higher total effective rate (RR (95% CI), 1.23 (1.12 ~ 1.36)). In network meta-analyses, similar results were recorded. Subsequently, we ranked all treatments from high to low effective rate and the order was CbAM, SAM, Chinese herbal medicine, western medicine and sham-acupuncture.
Conclusions: In the treatment of CFS, CbAM and SAM may have better effect than other treatments. However, the included trials have relatively poor quality, hence high quality studies are needed to confirm our finding.
Objectives: This meta-analysis aimed to assess the effectiveness and safety of Chinese herbal medicine (CHM) in treating chronic fatigue syndrome (CFS). Methods: Nine electronic databases were searched from inception to May 2022. Two reviewers screened studies, extracted the data, and assessed the risk of bias independently. The meta-analysis was performed using the Stata 12.0 software. Results: Eighty-four RCTs that explored the efficacy of 69 kinds of Chinese herbal formulas with various dosage forms (decoction, granule, oral liquid, pill, ointment, capsule, and herbal porridge), involving 6,944 participants were identified. This meta-analysis showed that the application of CHM for CFS can decrease Fatigue Scale scores (WMD: -1.77; 95%CI: -1.96 to -1.57; p < 0.001), Fatigue Assessment Instrument scores (WMD: -15.75; 95%CI: -26.89 to -4.61; p < 0.01), Self-Rating Scale of mental state scores (WMD: -9.72; 95%CI:-12.26 to -7.18; p < 0.001), Self-Rating Anxiety Scale scores (WMD: -7.07; 95%CI: -9.96 to -4.19; p < 0.001), Self-Rating Depression Scale scores (WMD: -5.45; 95%CI: -6.82 to -4.08; p < 0.001), and clinical symptom scores (WMD: -5.37; 95%CI: -6.13 to -4.60; p < 0.001) and improve IGA (WMD: 0.30; 95%CI: 0.20-0.41; p < 0.001), IGG (WMD: 1.74; 95%CI: 0.87-2.62; p < 0.001), IGM (WMD: 0.21; 95%CI: 0.14-0.29; p < 0.001), and the effective rate (RR = 1.41; 95%CI: 1.33-1.49; p < 0.001). However, natural killer cell levels did not change significantly. The included studies did not report any serious adverse events. In addition, the methodology quality of the included RCTs was generally not high. Conclusion: Our study showed that CHM seems to be effective and safe in the treatment of CFS. However, given the poor quality of reports from these studies, the results should be interpreted cautiously. More international multi-centered, double-blinded, well-designed, randomized controlled trials are needed in future research.
What does all that tell us?
Disappointingly, it tells me that SCAM has preciously little to offer for ME/CFS patients.
But what about the TCM treatments? Aren’t the above reviews quite positive TCM?
Yes, they are but I nevertheless recommend taking them with a healthy pinch of salt.
Why?
Because we have seen many times before that, for a range of reasons, Chinese researchers of TCM draw false positive conclusions. That may sound unfair, harsh, or even racist, but I think it’s true. If you disagree, please show me a couple of systematic reviews of TCM for any human disease by Chinese researchers that have drawn negative conclusions.
And what is my advice to patients suffering from ME/CSF?
I think the best I can offer is this: be very cautious about the many claims made by SCAM enthusiasts; if it sounds too good to be true, it probably is!
It has been reported that the PLASTIC SURGERY INSTITUTE OF ·UTAH, INC.; MICHAEL KIRK MOORE JR.; KARI DEE BURGOYNE; KRISTIN JACKSON ANDERSEN; AND SANDRA FLORES, stand accused of running a scheme out of the Plastic Surgery Institute of Utah, Inc. to defraud the United States and the Centers for Disease Control and Prevention.
Dr. Michael Kirk Moore, Jr. and his co-defendants at the Plastic Surgery Institute of Utah have allegedly given falsified vaccine cards to people in exchange for their donating $50 to an unnamed organization, one which exists to “liberate the medical profession from government and industry conflicts of interest.” As part of the scheme, Moore and his co-defendants are accused of giving children saline injections so that they would believe they were really being vaccinated.
The co-defendants are Kari Dee Burgoyne, an office manager at the Plastic Surgery Institute of Utah; Sandra Flores, the office’s receptionist; and, strangest of all, a woman named Kristin Jackson Andersen, who according to the indictment is Moore’s neighbor. Andersen has posted copious and increasingly conspiratorial anti-vaccine content on Facebook and Instagram; Dr. Moore himself was a signatory on a letter expressing support for a group of COVID-skeptical doctors whose certification was under review by their respective medical boards. The letter expresses support for ivermectin, a bogus treatment for COVID.
According to the indictment, the Plastic Surgery Center of Utah was certified as a real vaccine provider and signed a standard agreement with the CDC, which among other things requires doctor’s offices not to “sell or seek reimbursement” for vaccines.
Prosecutors allege that, when people seeking falsified vaccine cards contacted the office, Burgoyne, the office manager, referred them to Andersen, Dr. Moore’s neighbor. Andersen, according to the indictment, would ask for the name of someone who’d referred them—it had to be someone who’d previously received a fraudulent vaccine card, per the indictment—then direct people to make a $50 donation to a charitable organization, referred to in the indictment only as “Organization 1.” Each vaccine card seeker was required to put an orange emoji in the memo line of their donation.
After making a donation to the unnamed charitable organization, prosecutors allege, Andersen would send a link to vaccine card seekers to enable them to make an appointment at the Plastic Surgery Institute. With adult patients, Moore would allegedly use a real COVID vaccine dose in a syringe, but squirt it down the drain. Flores, the office’s receptionist, gave an undercover agent a note, reading “with 18 & younger, we do a saline shot,” meaning that kids were injected with saline instead of a vaccine. Prosecutors allege the team thus disposed of at least 1,937 doses of COVID vaccines.
All four people are charged with conspiracy to defraud the United States; conspiracy to convert, sell, convey, and dispose of government property; and conversion, sale, conveyance, and disposal of government property and aiding and abetting.
Throughout the scheme, the group reported the names of all the vaccine seekers to the Utah Statewide Immunization Information System, indicating that the practice had administered 1,937 doses of COVID-19 vaccines, which included 391 pediatric doses. The value of all the doses totaled roughly $28,000. With the money from the $50 vaccination cards totaling nearly $97,000, the scheme was valued at nearly $125,000, federal prosecutors calculated.
“By allegedly falsifying vaccine cards and administering saline shots to children instead of COVID-19 vaccines, not only did this provider endanger the health and well-being of a vulnerable population, but also undermined public trust and the integrity of federal health care programs,” Curt Muller, special agent in charge with the Department of Health and Human Services for the Office of the Inspector General, said in a statement.
_________________________________
I am already baffled by anti-vax attitudes when they originate from practitioners of so-called alternative medicine (SCAM). When they come from real physicians and are followed by real actions, I am just speechless. As I stated many times before: studying medicine does unfortunately not protect you from recklessness, greed, or stupidity.
Two years ago, I published a blog about the research activity in SCAM. To demonstrate the volume of SCAM research I looked into Medline to find the number of papers published in 2020 for the SCAMs listed below. Now I repeated the exercise for the year 2022. The respective 1st numbers below are those of 2020, and the second ones refer to 2022 (in bold):
- acupuncture 2 752 – 3,565
- anthroposophic medicine 29 – 28
- aromatherapy 173 – 205
- Ayurvedic medicine 183 – 249
- chiropractic 426 – 498
- dietary supplement 5 739 – 8,915
- essential oil 2 439 – 3,340
- herbal medicine 5 081 – 16,207
- homeopathy 154 – 212
- iridology 0 – 0
- Kampo medicine 132 – 176
- massage 824 – 996
- meditation 780 – 1,016
- mind-body therapies 968 – 1,616
- music therapy 539 – 716
- naturopathy 68 – 92
- osteopathic manipulation 71 – 85
- Pilates 97 – 152
- qigong 97 – 121
- reiki 133 – 158
- tai chi 397 – 470
- Traditional Chinese Medicine 15 277 – 22,586
- yoga 698 – 837
These data suggest the following:
- As before, the research activity in SCAM seems relatively low.
- Most numbers are pretty stable with a slight overall increase.
- The meager numbers for anthroposophic medicine, homeopathy, iridology, Kampo, and naturopathy are remarkable.
- In absolute terms, only acupuncture, dietary supplements, essential oil, herbal medicine, and TCM are impressive; by and large, these are areas where commercial interest and sponsors exist.
- The ‘big winners’ in terms of increase over time are acupuncture, supplements, essential oil, herbal medicine, and TCM; I suspect that much of this is due to the fast-growing (and repeatedly mentioned) influence that China is gaining in SCAM.
Cervical radiculopathy is a common condition that is usually due to compression or injury to a nerve root by a herniated disc or other degenerative changes of the upper spine. The C5 to T1 levels are the most commonly affected. In such cases local and radiating pains, often with neurological deficits, are the most prominent symptoms. Treatment of this condition is often difficult.
The purpose of this systematic review was to assess the effectiveness and safety of conservative interventions compared with other interventions, placebo/sham interventions, or no intervention on disability, pain, function, quality of life, and psychological impact in adults with cervical radiculopathy (CR).
MEDLINE, CENTRAL, CINAHL, Embase, and PsycINFO were searched from inception to June 15, 2022, to identify studies that were randomized clinical trials, had at least one conservative treatment arm, and diagnosed participants with CR through confirmatory clinical examination and/or diagnostic tests. Studies were appraised using the Cochrane Risk of Bias 2 tool and the quality of the evidence was rated using the Grades of Recommendations, Assessment, Development, and Evaluation approach.
Of the 2561 records identified, 59 trials met our inclusion criteria (n = 4108 participants). Due to clinical and statistical heterogeneity, the findings were synthesized narratively. The results show very-low certainty evidence supporting the use of
- acupuncture,
- prednisolone,
- cervical manipulation,
- low-level laser therapy
for pain and disability in the immediate to short-term, and thoracic manipulation and low-level laser therapy for improvements in cervical range of motion in the immediate term.
There is low to very-low certainty evidence for multimodal interventions, providing inconclusive evidence for pain, disability, and range of motion. There is inconclusive evidence for pain reduction after conservative management compared with surgery, rated as very-low certainty.
The authors concluded that there is a lack of high-quality evidence, limiting our ability to make any meaningful conclusions. As the number of people with CR is expected to increase, there is an urgent need for future research to help address these gaps.
The fact that we cannot offer a truly effective therapy for CR has long been known – except, of course, to chiropractors, acupuncturists, osteopaths, and other SCAM providers who offer their services as though they are a sure solution. Sometimes, their treatments seem to work; but this could be just because the symptoms of CR can improve spontaneously, unrelated to any intervention.
The question thus arises what should these often badly suffering patients do if spontaneous remission does not occur? As an answer, let me quote from another recent systematic review of the subject: The 6 included studies that had low risk of bias, providing high-quality evidence for the surgical efficacy of Cervical Spondylotic Radiculopathy. The evidence indicates that surgical treatment is better than conservative treatment … and superior to conservative treatment in less than one year.
I have been informed by the publisher, that my book has been published yesterday. This is about two months earlier than it was announced on Amazon. It is in German – yes, I have started writing in German again. But not to worry, I translated the preface for you:
Anyone who falls ill in Germany and therefore needs professional assistance has the choice, either to consult a doctor or a non-medical practitioner (Heilpraktiker).
– The doctor has studied and is licensed to practice medicine; the Heilpraktiker is state-recognized and has passed an official medical examination.
– The doctor is usually in a hurry, while the Heilpraktiker takes his time and empathizes with his patient.
– The doctor usually prescribes a drug burdened with side effects, while the Heilpraktiker prefers the gentle methods of alternative medicine.
So who should the sick person turn to? Heilpraktiker or doctor? Many people are confused by the existence of these parallel medical worlds. Quite a few finally decide in favor of the supposedly natural, empathetic, time-tested medicine of the Heilpraktiker. The state recognition gives them the necessary confidence to be in good hands there. The far-reaching freedoms the Heilpraktiker has by law, as well as the coverage of costs by many health insurances, are conducive to further strengthening this trust. “We Heilpraktiker are recognized and respected in politics and society,” writes Elvira Bierbach self-confidently, the publisher of a standard textbook for Heilpraktiker.
The first consultation of our model patient with the Heilpraktiker of his choice is promising. The Heilpraktiker responds to the patient with understanding, usually takes a whole hour for the initial consultation, gives explanations that seem plausible, is determined to get to the root of the problem, promises to stimulate the patient’s self-healing powers naturally, and invokes a colossal body of experience. It almost seems as if our patient’s decision to consult a Heilpraktiker was correct.
However, I have quite significant reservations about this. Heilpraktiker are perhaps recognized in politics and society, but from a medical, scientific, or ethical perspective, they are highly problematic. In this book, I will show in detail and with facts why.
The claim of government recognition undoubtedly gives the appearance that Heilpraktiker are adequately trained and medically competent. In reality, there is no regulated training, and the competence is not high. The official medical examination, which all Heilpraktiker must pass is nothing more than a test to ensure that there is no danger to the general public. The ideas of many Heilpraktiker regarding the function of the human body are often in stark contradiction with the known facts. The majority of Heilpraktiker-typical diagnostics is pure nonsense. The conditions that they diagnose are often based on little more than naive wishful thinking. The treatments that Heilpraktiker use are either disproven or not proven to be effective.
There is no question in my mind that Heilpraktiker are a danger to anyone who is seriously ill. And even if Heilpraktiker do not cause obvious harm, they almost never offer what is optimally possible. In my opinion, patients have the right to receive the most effective treatment for their condition. Consumers should not be misled about health-related issues. Only those who are well-informed will make the right decisions about their health.
My book provides this information in plain language and without mincing words. It is intended to save you from a dangerous misconception of the Heilpraktiker profession. Medical parallel worlds with the radically divergent quality standard – doctor/Heilpraktiker – are not in the interest of the patient and are simply unacceptable for an enlightened society.
I had come across them so often that I had almost stopped noticing them: the ‘little extras‘ that make ineffective so-called alternative medicines (SCAMs) seem effective. Then, recently, during an interview about detox diets, the interviewer responded to my explanation of the ineffectiveness of these treatments by saying: “but these diets include stopping the consumption of alcohol, cigarettes, and other harmful stuff; therefore they must be good.” This seemingly convincing argument reminded me of a phenomenon – I call it here the ‘little extra‘ – that applies to so many (if not most) SCAMs.
Let me schematically summarise it as follows:
- A practitioner applies an ineffective SCAM to a patient.
- Because it is ineffective, it has little effect other than a small placebo response.
- The ineffective SCAM comes with a ‘little extra‘ which is unrelated to the SCAM.
- The ‘little extra‘ is effective.
- The end result is that the ineffective SCAM appears to be effective.
The above example makes it quite clear: the detox diet is utter nonsense but, as it goes hand in hand with effective lifestyle changes, it appears to be effective. A classic case. But SCAM offers no end of similar examples:
- Acupuncture is useless but it involves touch, time, attention, and empathy all of which are effective in making a patient feel better.
- Chiropractic is useless but it involves touch, time, attention, and empathy all of which are effective in making a patient feel better.
- Homeopathy is useless but it involves a long, empathic consultation and attention which are effective in making a patient feel better.
- Osteopathy is useless but it involves touch, time, attention, and empathy all of which are effective in making a patient feel better.
- Reflexology is useless but it involves touch, time, attention, and empathy all of which are effective in making a patient feel better.
Do I need to continue?
Probably not!
The ‘little extras‘ are often forgotten or subsumed under the heading ‘placebo’. Yet, they are not part of the placebo effect. Strictly speaking, they are concomitant treatments comparable to a pain patient using SCAM and also taking a few paracetamols. In the end, she forgets about the painkillers and thinks that her SCAM worked wonders.
Even ardent SCAM proponents have long realized this phenomenon. Here, for example, is a paper entitled ‘Acupuncture as a complex intervention: a holistic model’ by ex-colleagues of mine at Exeter looking at it but coming up with a very different perspective:
Objectives: Our understanding of acupuncture and Chinese medicine is limited by a lack of inquiry into the dynamics of the process. We used a longitudinal research design to investigate how the experience, and the effects, of a course of acupuncture evolved over time.
Design and outcome measures: This was a longitudinal qualitative study, using a constant comparative method, informed by grounded theory. Each person was interviewed three times over 6 months. Semistructured interviews explored people’s experiences of illness and treatment. Across-case and within-case analysis resulted in themes and individual vignettes.
Subjects and settings: Eight (8) professional acupuncturists in seven different settings informed their patients about the study. We interviewed a consecutive sample of 23 people with chronic illness, who were having acupuncture for the first time.
Results: People described their experience of acupuncture in terms of the acupuncturist’s diagnostic and needling skills; the therapeutic relationship; and a new understanding of the body and self as a whole being. All three of these components were imbued with holistic ideology. Treatment effects were perceived as changes in symptoms, changes in energy, and changes in personal and social identity. The vignettes showed the complexity and the individuality of the experience of acupuncture treatment. The process and outcome components were distinct but not divisible, because they were linked by complex connections. The paper depicts these results as a diagrammatic model that illustrates the components and their interconnections and the cyclical reinforcement, both positive and negative, that can occur over time.
Conclusions: The holistic model of acupuncture treatment, in which “the whole being greater than the sum of the parts,” has implications for service provision and for research trial design. Research trials that evaluate the needling technique, isolated from other aspects of process, will interfere with treatment outcomes. The model requires testing in different service and research settings.
I think the perspective of viewing SCAMs as complex interventions is needlessly confusing and deeply unhelpful. The truth is that there is no treatment that is not complex. Take a surgical treatment, for instance, it involves dozens of ‘little extras‘ that are known to be effective. Should we, therefore, try to use this fact for justifying useless surgical interventions? Or take a simple prescription of medication from a doctor. It involves time, empathy, attention, explanations, etc. all of which will affect the patient’s symptoms. Should we thus use this to justify a useless drug? Certainly not!
And for the same reason, it is nonsense to use the ‘little extras‘ that come with all the numerous ineffective SCAMs as a smokescreen that makes them look effective.
Homeopathy is touted as a panacea, we all know that. It is thus hardly surprising that it is also claimed to be an effective detox option. Here is a German article on the subject that I translated for you:
It was published on the independent health portal Lifeline. It claims that it “offers comprehensive, high-quality and understandably written information on health topics, diseases, nutrition, and fitness. Our editorial team is supported by doctors and freelance medical authors in the continuous creation and quality assurance of our content. Much of our information is multimedia-based with videos and informative image galleries. Numerous self-tests encourage interaction. In our expert advice and forums on various topics, Lifeline users can discuss topics with experts or exchange information with other users. Our information is in no way intended to be a substitute for a visit to the doctor. Rather, our aim is to qualitatively improve and support the relationship between doctor and patient through the information provided. Therefore, our contents do not serve the purpose of arbitrary diagnosis or treatment.”
And here is the article in question:
Environmental toxins, medications, nicotine, alcohol, unhealthy food – the human body is burdened daily by many substances, waste products and toxins. It is therefore sensible and beneficial to detoxify the liver regularly – preferably naturally. With these homeopathic remedies, this can be done gently.
To stay healthy or to prevent acute diseases from becoming chronic: The reasons to regularly rid the body of accumulated toxins are many. Toxins and waste products weaken the organism or can even cause illness themselves. Especially after drug treatments with antibiotics or cortisone, with frequently recurring colds and flu-like infections, it can be useful to detoxify the body naturally – with homeopathy.
In the body, the liver is the central organ where toxins are broken down. The kidneys, as organs of elimination, also play an important role in detoxification. To support the liver and kidneys in natural detoxification, various medicines are available. In homeopathy, detoxification is also called elimination.
Homeopathic medicines particularly suitable for the detoxification cure:
Sulfur: This classic homeopathic medicine has a strong detoxifying effect on connective tissue and mucous membranes, as well as a cleansing effect on the entire organism. In homeopathy, sulfur is mainly used for natural detoxification after drug treatments with antibiotics and cortisone. If the body is so heavily burdened with waste products that other homeopathic medicines have no effect, Sulfur can be used for natural detoxification.
Nux vomica: A very versatile homeopathic medicine is Nux vomica. It is particularly suitable for detoxifying the body naturally when one has consumed too many stimulants such as coffee or alcohol. It can also be used to eliminate harmful substances caused by medication. Nux vomica has proven particularly useful for the accompanying treatment of side effects after chemotherapy.
Pulsatilla: In homeopathy, Pulsatilla is considered an important natural remedy for detoxification, acting primarily on the mucous membranes and the stomach and intestines. Pulsatilla helps alleviate physical discomfort caused by eating too fatty, unhealthy foods, drinks that irritate the stomach such as coffee and alcohol, and taking medications. Pulsatilla works similarly to the detoxification classic sulfur, only the natural detoxification of liver and kidneys as well as connective tissue proceeds even more gently.
Arsenicum album: Within homeopathy, the remedy Arsenicum album is considered a universal remedy for poisoning, for example by heavy metals. It is mainly used for physical signs of exhaustion and weakness and can compensate for negative consequences of unhealthy nutrition. In addition, Arsenicum album is also said to have an anxiety-relieving effect.
Okoubaka: Okoubaba is also considered a medicine with a strong detoxifying effect, acting mainly on the gastrointestinal tract and used for abdominal cramps, flatulence, constipation, as well as acute diarrhea. Especially after a treatment with antibiotics or after having gone through an illness with norovirus, rotavirus or salmonella, Okoubaba can help to detoxify naturally and restore the intestinal flora.
Magnesium fluoratum: When cold symptoms such as cough and cold flare up again and again after administration of fever-reducing medications and other cold preparations, recovery is protracted and the body is weakened, natural detoxification with magnesium fluoratum can help.
Echinacea: Echinacea is known to increase the body’s defenses. As a homeopathic medicine, it can also help to naturally detoxify underlying conditions that have not been cured.
Detoxify naturally: Typical potencies and their dosage
Low potencies from D3 to D12 are commonly used for self-treatment in natural detoxification. However, choosing the right homeopathic remedy is not always easy. If there are uncertainties, an experienced homeopath should be asked for advice, if possible, in order to determine the drug, potency and dosage on the basis of a detailed anamnesis.
___________________________
Impressed?
No?
But I am – though not in a positive sense.
The article contains far too many unsubstantiated statements to mention. In fact, they are not just unsubstantiated, they are false! As the author does not even attempt to provide evidence for them, one cannot even dispute it. Suffice to say that ‘detox’ is BS and homeopathy too. And in healthcare ‘minus X minus’ does sadly not give ‘plus’.
What renders this otherwise trivial article rather important, in my view, is this: such web-based information is not the exception; quite the opposite: German consumers are bombarded with BS of this type.
Ever wondered why Germany is such a huge market for health fraud?
Now you know the answer!