economic evaluation
We live in truly grim times! Let me therefore try to cheer you up a little. Here is a story that might make you smile.
In 1981, I moved back from London to Munich. While still in London, I had written an article on garlic for a German medical journal. It was published just as we arrived in our new home. Here is it’s English abstract:
Garlic has had a firm place in folk medicine since ancient times. More recent results are summarized here which show that extracts of the plant have an antimicrobial action, they are capable of lowering blood cholesterol and of reducing secondary vascular changes. They raise fibrinolytic activity and inhibit thrombocyte aggregation. Therefore the plant contains highly active therapeutic principles which appear to be particularly suitable for prophylaxis of arteriosclerosis.
Yes, you are quite right, this paper is nothing to write home about. So, why do I consider it ‘most consequential‘? Here is what happened:
My wife and I had barely arrived in our new home, when a man phoned (he had gone to a lot of trouble to find my number) and said: “I know you are the leading expert on garlic; I urgently need to talk to you”. Never correct a man’s mistake, if it’s in your favour, I thought, and we made an appointment for a meeting at the Munich train station hotel.
When I met him a few days later, he ordered me a coffee (which later I had to pay for) and explained that he had worked his whole life (he was about 50, I guessed) for the pharmaceutical industry and had now decided that this was enough. He thus planned to set up his own pharmaceutical company. He already had a photocopy machine in his basement, he proudly told me, and a wife who was willing to work as hard as he was. Specifically, his plan was to launch a garlic pill, and for that he needed my advice. I told him what he wanted to know, and we parted after about two hours promising to stay in contact.
The man’s name was Kuno Lichtwer.
During the weeks that followed, he often phoned me to pick my brain. One day, he told me that he had everything in place: he had found a supplier of the materials, a manufacturer to produce the pills and even registered a name for it:
KWAI

Then he popped the question that was foremost on his mind: ‘What do you think, Dr Ernst, should I risk it and go ahead with this or not?’. I had started to like that man; he was going to lose all his savings on a crazy idea, I felt. So, I told him: ‘If I were you, I would not do it. There are already plenty of garlic pills on the market. You are risking to lose everything.’ Then there was a long pause; eventually, he thanked me for my honest advice and hung up.
Weeks later he phoned again to tell me that he had truly appreciated my brutally direct advice, thought long and hard about it, but went ahead with his plan anyway. Would I now accept the position of ‘medical advisor’ to Lichwer Pharma? I was surprised, but accepted this new post. Thereafter, I advised him the best I could. We even conducted and published the very first clinical trial with his product. It was a rather flimsy study (we had no funds at all), but did suggest a positive result.
Each time Mr Lichtwer called me, he was elated; things were not just going well, they were booming! He was evidently hugely gifted in promoting KWAI. Then he invited me several times to come to Berlin where Lichtwer Pharma was based for business meetings. Proudly, he showed me that meanwhile his firm had moved out of his basement into a proper building. The next I knew was that he had a dozen employees. Lichtwer seemed unstoppable. This went on for 2 or 3 years, if I remember correctly.
During all this time, we had never talked about money, and my work for him had always been unpaid – that is, until one day just before Christmas he phoned and explained that he had moved his firm to yet a bigger building and hired yet more staff. He also realised that I deserved some renumeration for my advice; therefore, he had put a cheque in the post. When I told my wife about it, we both celebrated in anticipation of the substantial windfall. Two days later, his letter arrived. He very kindly thanked me for years of work and included a cheque of 500 DM (about 150 DM per year of work). A few months later, his firm had grown so big that a full time medical and research director was badly needed. He informed me that he had found a highly experienced expert and invited me to meet the new man, Prof Schulz.
No, I did not feel hard done by! On the contrary, I was happy that my prediction had been grossly wrong and that my friend Kuno was doing so well. In addition, I was also relieved, because my research at the University did not give me nearly enough time to look adequately after the now substantial firm of Lichtwer Pharma.
Thereafter, Lichtwer’s garlic pill went from strength to strength. Several larger studies confirmed our initial results that garlic positively influenced blood lipids (in 2000, our systematic review concluded: The available data suggest that garlic is superior to placebo in reducing total cholesterol levels. However, the size of the effect is modest, and the robustness of the effect is debatable. The use of garlic for hypercholesterolemia is therefore of questionable value). One day, I read somewhere that KWAI had become the most consumed pill in Germany (even beating Aspirin). Then Lichtwer Pharma went international and added several further herbal products to its portfolio. In 1991, Lichtwer Pharma was estimated to be worth 100 Million DM. Several years later, the firm had almost 400 employees and a yearly turnover of 353 Million DM.
To his credit, Kuno Lichtwer never entirely forgot me. When I had moved to the UK, he even came to Exeter, was entertained by my University, and made a donation of £100 000 towards a ‘Lichtwer Research Fellowship’ for my department. I am not sure whether Kuno Lichtwer is still alive. If he is, he would probably agree that, had I offered him 10 000 DM of my savings during our 1st meeting in 1981 (he did hint at that possibility), he would have gladly made me a partner in his enterprise.
But, as they say: money is not everything.
And a good story to tell is also not bad.
Today, HRH the Prince of Wales has his 72th birthday. As every year, I send him my best wishes by dedicating an entire post to a brief, updated summary of his achievements in the area of so-called alternative medicine (SCAM).
EARLY INFLUENCE OF LAURENCE VAN DER POST
Aged 18, Charles went on a journey of ‘spiritual discovery’ into the Kalahari desert. His guide was Laurens van der Post (later discovered to be a fraud and compulsive fantasist and to have fathered a child with a 14-year old girl entrusted to him during a sea voyage). Van der Post wanted to awake Charles’ mind and attune it to the ideas of Carl Jung’s ‘collective unconscious’, and it is this belief in vitalism that provides the crucial link to SCAM: virtually every form of SCAM is based on the assumption that some sort of vital force exists. Charles was impressed with van der Post that he made him the godfather of Prince William. After Post’s death, he established an annual lecture in his honour (the lecture series was quickly discontinued after van der Post was discovered to be a fraud).
CHIROPRACTIC and OSTEOPATHY
Throughout the 1980s, Charles lobbied for the statutory regulation of chiropractors and osteopaths in the UK. In 1993, this finally became reality. To this day, these two SCAM professions are the only ones regulated by statute in the UK.
THE BRITISH MEDICAL ASSOCIATION
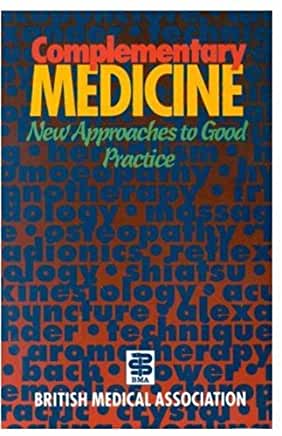
In 1982, Prince Charles was elected as President of the British Medical Association (BMA) and promptly challenged the medical orthodoxy by advocating SCAM. In a speech at his inaugural dinner as President, the Prince lectured the medics: ‘Through the centuries healing has been practised by folk healers who are guided by traditional wisdom which sees illness as a disorder of the whole person, involving not only the patient’s body, but his mind, his self-image, his dependence on the physical and social environment, as well as his relation to the cosmos.’ The BMA-officials ordered a full report on alternative medicine which promptly condemned this area as implausible nonsense.
Six years later, a second report, entitled ‘Complementary Medicine – New Approaches to Good Practice’, heralded U-turn stating that: “the demand for non-conventional therapies had become so pressing that organised medicine in Britain could no longer ignore its contribution“. At the same time, however, the BMA set in motion a further chapter in the history of SCAM by insisting that it was “unacceptable” to allow the unrestricted practice of non-conventional therapies, irrespective of training or experience.
THE FOUNDATION OF INTEGRATED HEALTH
In 1993, Charles founded his lobby group which, after being re-named several times, ended up being called the ‘Foundation for Integrated Health’ (FIH). It was closed down in 2010 amidst allegations of money laundering and fraud. Its chief executive, George Gray, was later convicted and went to jail.
MOSARAF ALI
In 2001, Charles worked on plans to help build a model hospital of integrated medicine. It was to train doctors to combine conventional medicine and SCAMs, such as homeopathy, Ayurvedic medicine and acupuncture, and was to have around 100 beds. The prince’s intervention marked the culmination of years of campaigning by him for the NHS to assign a greater role to SCAM.
INTEGRATIVE MEDICINE
In 2001, Charles published an editorial in the BMJ promoting his ideas around integrative medicine. Its title: THE BEST OF BOTH WORLDS. Ever since, Charles has been internationally recognised as one of the world’s most vociferous champions of integrated medicine.
GERSON DIET
In 2004, Charles publicly supported the Gerson diet as a treatment for cancer. Prof Baum, an eminent oncologists, was invited to respond in an open letter to the British Medical Journal: ” …Over the past 20 years I have treated thousands of patients with cancer and lost some dear friends and relatives to this dreaded disease…The power of my authority comes with knowledge built on 40 years of study and 25 years of active involvement in cancer research. Your power and authority rest on an accident of birth. I don’t begrudge you that authority but I do beg you to exercise your power with extreme caution when advising patients with life-threatening diseases to embrace unproven therapies.”
THE SMALLWOOD REPORT
In 2005, the ‘Smallwood-Report’ was published; it had been commissioned by Charles and paid for by Dame Shirley Porter to inform health ministers. It stated that up to 480 million pounds could be saved, if one in 10 family doctors offered homeopathy as an “alternative” to standard drugs for asthma. Savings of up to 3.5 billion pounds could be achieved by offering spinal manipulation rather than drugs to people with back pain. Because I had commented on this report, Prince Charles’ first private secretary asked my vice chancellor to investigate the alleged indiscretion; even though I was found to be not guilty of any wrong-doing, all local support at Exeter stopped which eventually led to my early retirement.
WORLD HEALTH ORGANISATION
In a 2006 speech, Prince Charles told the World Health Organisation in Geneva that SCAM should have a more prominent place in health care and urged every country to come up with a plan to integrate conventional and alternative medicine into the mainstream. Anticipating Prince Charles’s sermon in Geneva, 13 of Britain’s most eminent physicians and scientists wrote an “Open Letter” which expressed concern over “ways in which unproven or disproved treatments are being encouraged for general use in Britain’s National Health Service.” The signatories argued that “it would be highly irresponsible to embrace any medicine as though it were a matter of principle.”
TRADITIONAL CHINESE MEDICINE (TCM)
In 2007, the People’s Republic of China recorded the visit of Fu Ying, its ambassador in London at the time, to Clarence House, and announced that the Charles had praised TCM. “He hoped that it could be included in the modern medical system . . . and was willing to make a contribution to it.”
HERBAL MEDICINE
In 2009, the Prince held talks with the health Secretary to persuade him to introduce safeguards amid a crackdown by the EU that could prevent anyone who is not a registered health practitioner from selling remedies.
In the same year, Charles urged the government to protect SCAM because “we fear that we will see a black market in herbal products”, as Dr Michael Dixon, medical director of the FIH and Charles’ advisor in SCAM, put it.
UK HEALTH POLITICS
In 2009, the health secretary wrote to the Prince suggesting a meeting on the possibility of a study on integrating SCAM in England’s NHS. The Prince had written to Burnham’s predecessor, Alan Johnson, demanding greater access to SCAM in the NHS alongside conventional medicine. Charles stated that “despite waves of invective over the years from parts of the medical and scientific establishment” he continued to lobby “because I cannot bear people suffering unnecessarily when a complementary approach could make a real difference”.
In June 2014, BBC NEWS published the following text about a BBC4 broadcast entitled ‘THE ROYAL ACTIVIST’ aired on the same day: Prince Charles has been a well-known supporter of complementary medicine. According to a… former Labour cabinet minister, Peter Hain, it was a topic they shared an interest in. He had been constantly frustrated at his inability to persuade any health ministers anywhere that that was a good idea, and so he, as he once described it to me, found me unique from this point of view, in being somebody that actually agreed with him on this, and might want to deliver it. Mr Hain added: “When I was Secretary of State for Northern Ireland in 2005-7, he was delighted when I told him that since I was running the place I could more or less do what I wanted to do. I was able to introduce a trial for complementary medicine on the NHS, and it had spectacularly good results, that people’s well-being and health was vastly improved. And when he learnt about this he was really enthusiastic and tried to persuade the Welsh government to do the same thing and the government in Whitehall to do the same thing for England, but not successfully,” added Mr Hain.
In October 2015, the Guardian obtained the infamous “black spider memos” which revealed that Charles had repeatedly lobbied politicians in favour of SCAM.
THE COLLEGE OF MEDICINE
In 2009, it was announced that the ‘College of Integrated Medicine’ (the successor of the FIH) was to have a second base in India. In 2011, Charles forged a link between ‘The College of Medicine’ and an Indian holistic health centre. The collaboration was reported to include clinical training to European and Western doctors in Ayurveda and homoeopathy and traditional forms of medicine to integrate them in their practice. The foundation stone for the extended campus of the Royal College known as the International Institution for Holistic and Integrated Medicine was laid by Dr Michael Dixon in collaboration with the Royal College of Medicine.
In 2020, Charles became the patron of the College of Medicine which, by then, had re-christened itself ‘College of Medicine and Integrated Health’. The College chair, Michael Dixon, was quoted stating: ‘This is a great honour and will support us as an organisation committed to taking medicine beyond drugs and procedures. This generous royal endorsement will enable us to be ever more ambitious in our mission to achieve a more compassionate and sustainable health service.”
DUTCHY ORIGINALS DETOX TINCTURE
In 2011, after the launch of Charles’ range of herbal tinctures, I had the audacity to publicly criticise Charles for selling the Duchy Herbals detox tincture which I named ‘Dodgy Originals Detox Tincture’.
ANTIBIOTIC OVERUSE
In 2016, speaking at a global leaders summit on antimicrobial resistance, Prince Charles warned that Britain faced a “potentially disastrous scenario” because of the “overuse and abuse” of antibiotics. The Prince explained that he had switched to organic farming on his estates because of the growing threat from antibiotic resistance and now treats his cattle with homeopathic remedies rather than conventional medication. As some of you may be aware, this issue has been a long-standing and acute concern to me,” he told delegates from 20 countries “I have enormous sympathy for those engaged in the vital task of ensuring that, as the world population continues to increase unsustainably and travel becomes easier, antibiotics retain their availability to overcome disease… It must be incredibly frustrating to witness the fact that antibiotics have too often simply acted as a substitute for basic hygiene, or as it would seem, a way of placating a patient who has a viral infection or who actually needs little more than patience to allow a minor bacterial infection to resolve itself.”
DUMFRIES HOUSE
In 2017, Charles declared that he will open a centre for SCAM in the recently purchased Dumfries House in Scotland. Currently, the College of Medicine and Integrated Health is offering two-day Foundation Courses at this iconic location. Gabriel Chiu, a US celebrity cosmetic and reconstructive surgeon, and his wife Christine, joined the Prince of Wales as he opened the integrated health and wellbeing centre on the Dumfries House Estate in East Ayrshire in 2019. As he unveiled a plaque, Prince Charles said: “I’m so glad that all of you have been able to get here today, particularly because I could not be more proud to see the opening of this new integrated health centre at Dumfries House. It’s something I’ve been wanting to do for the last 35 years. I’m also so proud of all the team at Dumfries House who built it, an all in-house team.”
HOMEOPATHY
Generations of royals have favoured homeopathy, and allegedly it is because of this influence that homeopathy became part of the NHS in 1948. Homeopathy has also been at the core of Charles’ obsession with SCAM from its beginning. In 2017, ‘Country News’ published an article about our heir to the throne stating that Prince of Wales has revealed he uses homeopathic treatments for animals on his organic farm at Highgrove to help reduce reliance on antibiotics, the article stated. He said his methods of farming tried wherever possible to ‘‘go with the grain of nature’’ to avoid dependency on antibiotics, pesticides and other forms of chemical intervention.
In the same year, it was revealed that UK farmers were being taught how to treat their livestock with homeopathy “by kind permission of His Royal Highness, The Prince Of Wales”
In 2019, the Faculty of Homeopathy announced that His Royal Highness The Prince of Wales had accepted to become Patron of the Faculty of Homeopathy. Dr Gary Smyth, President of the Faculty of Homeopathy commented, “As the Faculty celebrates its 175th anniversary this year, it is an enormous honour for us to receive the Patronage of His Royal Highness The Prince of Wales and I am delighted to announce this news today.” Charles’ move amazed observers who saw it as a deliberate protest against the discontinuation of reimbursement of homeopathy by the NHS.
In 2020, Charles fell ill with the corona-virus and happily made a swift recovery. It was widely reported that his recovery was due to homeopathy, a notion denied by Clarence House.
_______________________
Happy Birthday Charles
Research by a reputable independent research company done for Securivita a German insurance company shows that those receiving homeopathic care were much better off. Over 15,700 patients were involved in the study which also used a comparison group.
The study showed that in a wide range of patients with various pathological problems that if they had homeopathic care they faired dramatically better than those just getting conventional medicine.
Children having homeopathy treatment from birth, were particularly healthier and with less problems. Over the three year study period, the number of children needing antibiotics decreased by 16.7 per cent in the homeopathy group, whereby it increased by 73.9 per cent in the conventional medical comparison group!
The number of hospitalizations in the comparison group increased by 32.6 per cent whereby in the homeopathy treatment group it decreased by 9.8 per cent!
Adults and children treated homoeopathically had dramatic improvements in allergies, dermatitis, asthma, just to name a few.
These are just a few examples of the remarkable benefits of homeopathic treatment outlined in the study by by the Leipzig Health Forum , an independent analytical institute specializing in health services conducted for Securvita Krankenkasse Insurer.
“We don’t need fewer, but more homeopathic doctors who will continue on this successful path,” says Götz Hachtmann , director of the health insurance company Securvita.
The study is in German and can be found here.
____________________________
Blessed are those who don’t read German (at least in this instance)!
As I am not amongst the blessed, I ought to tell you a bit about the ‘massive’ study. The OHR, the ‘OFFICIAL HOMEOPATHIC RESOURCE’ (btw what makes the OHR ‘official’?) claims that the study can be found here. The OHR is evidently not well enough resourced for translating the German text into English; if they were, they would know that the link goes not to a ‘study’ but to some kind of a glossy marketing brochure about the ‘study’ (there is no actual published scientific paper on the ‘study’). It provides hardly any relevant information; all we learn is that 15 700 individuals who regularly consulted homeopathic physicians were compared over a three year period to an equally sized control group who did not consult homeopathic doctors… And that’s essentially it! No further relevant details are offered.
By contrast, quite a bit of information is offered about the findings, for instance:
- In the homeopathy group, the hospitalisation rate of depressive patients dropped by 10%, while it increased in controls by 33%.
- The days off work dropped by 17% vs an increase in controls of 17%.
- The use of antibiotics decreased by 17% vs an increase of 74%.
And how do they explain these differences?
Yes, you guessed it:
they are due to homeopathy!
One does not need to have a perfumer’s nose to smell a few badly decomposing rats here, for example:
- We do not learn how many variables were tested in this ‘study’. Therefore, it is likely that the ‘results’ provided are the positive ones, while the not so positive potential effects of homeopathy remained unmentioned. Perhaps the death rate was higher in the homeopathy group? Perhaps they suffered more heart attacks? Perhaps they had a lower quality of life? Perhaps they caused more costs? Perhaps they committed more suicides? etc. etc.
- Even more obvious is the stench of selection bias. The individuals in the homeopathy group were clearly different from the controls to start with. They might have been more health conscious. They clearly were more cautious about antibiotics. They might have been of better general health. They might have been younger. They could have contained more women. They might have been more afraid of going into a hospital. They might have been keener to attend work. In fact, the only variable in which the two groups were comparable is sample size.
Even if we eventually we see this ‘study’ published in a peer-reviewed journal with full methodological details etc., it will not allow even the smartest spin-doctor to establish cause and effect. Its findings would not be more conclusive than those of previously discussed attempts to produce positive evidence for homeopathy. The ‘positive’ findings could have been the result of hundreds of causes, none of which are related to homeopathy.
In a nutshell: this new German ‘study’ is a textbook example for arguing in favour of conducting proper research rather that rampant pseudo-research.
But I must not always be so negative!!!
So, let me try to point out the positive sides of this ‘study’:
The ‘massive independent study’ is a true masterpiece of advertising and marketing for both Securivita and homeopathy.
Well done guys!
I am proud of you!
- That’s exactly the stuff needed for successfully misleading the public.
- That’s precisely the info required to increase your cash flow.
- That’s helpful ‘research’ for convincing politicians.
- That’s definitely the type of baloney to impresses the Ullmanns of this world.
- That’s even the sort of ‘science’ which the ‘OFFICIAL HOMEOPATHIC RESOURCE’ cannot recognise for what it truly is:
invalid junk.
Prof Ernst is far too critical about homeopathy!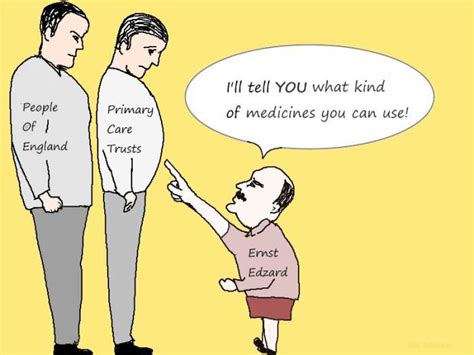
He is biased against it!
He cherry-picks the evidence!
He does not understand homeopathy!
If you are one of the many who believe such notions, please read on.
The website of the NHS England has a fairly detailed account of homeopathy. Here is the section entitled ‘What can we conclude from the evidence?‘ – but I recommend reading the full text:
There have been several reviews of the scientific evidence on the effectiveness of homeopathy.
The House of Commons Science and Technology Committee said there’s no evidence that homeopathy is effective as a treatment for any health condition.
There’s no evidence behind the idea that substances that cause certain symptoms can also help treat them.
Nor is there any evidence behind the idea that diluting and shaking substances in water can turn those substances into medicines.
The ideas that underpin homeopathy aren’t accepted by mainstream science, and aren’t consistent with long-accepted principles on the way the physical world works.
The Committee’s 2010 report on homeopathy said the “like cures like” principle is “theoretically weak”, and that this is the “settled view of medical science”.
For example, many homeopathic remedies are diluted to such an extent that it’s unlikely there’s a single molecule of the original substance remaining in the final remedy. In cases like these, homeopathic remedies consist of nothing but water.
Some homeopaths believe that, as a result of the succussion process, the original substance leaves an “imprint” of itself on the water. But there’s no known mechanism by which this can occur.
The 2010 report said: “We consider the notion that ultra-dilutions can maintain an imprint of substances previously dissolved in them to be scientifically implausible.”
Some people who use homeopathy may see an improvement in their health condition as the result of a phenomenon known as the placebo effect.
If you choose health treatments that provide only a placebo effect, you may miss out on other treatments that have been proven to be more effective.
__________________________________
Since 1948, homeopathy had been part of the NHS, there were 5 homeopathic NHS hospitals, and the costs for homeopathy were covered. Why would the NHS decision makers suddenly turn against it? They must have loved homeopathy for at least 4 reasons:
-
-
- It is inexpensive.
- It has support in high places.
- It did not cause any direct harm.
- It had many supporters who fought tooth and nail for it.
-
It is therefore hardly reasonable to assume that the NHS is biased against homeopathy. But, why do they now say that it is
- implausible,
- not effective beyond placebo,
- and can cause harm by making people miss out on effective therapies?
The answer is simple: BECAUSE THESE STATEMENTS ARE IN ACCORDANCE WITH THE OVERWHELMING MAJORITY OF THE BEST EVIDENCE AVAILABLE TO DATE.
So, here you are: the NHS now confirms what I (and many other experts) have been saying since years. And we all insist on the fact that this not because we are biased, stupid, uninformed, paid by BIG PHARMA, or want to deprive anyone of anything. We do it for one reason only:
BECAUSE IT’S THE TRUTH!
In response to the recommendation, the health ministry announced the formation of a working group of medical experts to suggest proposals for further regulation of homeopathy. A spokesman said that medicines whose efficiency is not clinically proven should not be procured using public funds, nor prescribed to treat the sick.
Russia has proved a profitable market for foreign suppliers of homeopathic medicine such as French company Boiron, which opened its Russian subsidiary in 2005. “Today, the Russian market is our company’s fourth largest in terms of turnover, after France, the US and Italy. Russia has always been interesting for Boiron because of the large population, and a relatively high incidence of illness and lower level of medicine consumption in comparison with Europe,” general director of Boiron in Russia Irina Nikulina said.
According to figures from Russian pharmaceutical market analysts DSM Group, Boiron sold 35 percent of all the homeopathic medicine sold in Russia last year, or 2.88 billion rubles (USD 49.5 million) worth of medicine. Boiron produces Russia’s most popular homeopathic medicine, called Oscillococcinum, which is marketed to relieve flu symptoms and accounted for 18.98 percent of all homeopathic medicines sold in 2016.
__________________________
The many international initiatives aimed at minimising the harm done by homeopathy are slowly beginning to yield results. It took many years for politicians to realise that the supposedly harmless homeopathy is, in fact, not harmless at all. Homeopathy causes harm by:
- wasting people’s money,
- distracting patients from effective treatments,
- the ill-conceived advice homeopaths give to patients,
- making a mockery of evidence-based medicine,
- violating the principles of medical ethics,
- undermining rational thinking in society.
One therefore has to applaud Russia’s ‘Commission against Pseudoscience’, hope that the working group does produce robust advice, and support similar initiatives in other countries.
In 2011, the following leading researchers of so-called alternative medicine (SCAM) – no I was not invited – had a meeting in Italy, did a brainstorm and decided what we would need to know about SCAM by 2020 (today, in other words):
They proposed 6 core areas of research that should be investigated to achieve a robust knowledge base and to allow stakeholders to make informed decisions:
- Research into the prevalence of SCAM in Europe: Reviews show that we do not know enough about the circumstances in which SCAM is used by Europeans. To enable a common European strategic approach, a clear picture of current use is of the utmost importance.
- Research into differences regarding citizens’ attitudes and needs towards SCAM: Citizens are the driver for CAM utilization. Their needs and views on SCAM are a key priority, and their interests must be investigated and addressed in future SCAM research.
- Research into safety of SCAM: Safety is a key issue for European citizens. SCAM is considered safe, but reliable data is scarce although urgently needed in order to assess the risk and cost-benefit ratio of SCAM.
- Research into the comparative effectiveness of SCAM: Everybody needs to know in what situation SCAM is a reasonable choice. Therefore, we recommend a clear emphasis on concurrent evaluation of the overall effectiveness of SCAM as an additional or alternative treatment strategy in real-world settings.
- Research into effects of context and meaning: The impact of effects of context and meaning on the outcome of SCAM treatments must be investigated; it is likely that they are significant.
- Research into different models of SCAM health care integration: There are different models of SCAM being integrated into conventional medicine throughout Europe, each with their respective strengths and limitations. These models should be described and concurrently evaluated; innovative models of SCAM provision in health care systems should be one focus for SCAM research.

‘Look, half the work is done! All you need to do is fill in the top part so we can legally say the bottom part.’
The researchers then added:
We also propose a methodological framework for SCAM research. We consider that a framework of mixed methodological approaches is likely to yield the most useful information. In this model, all available research strategies including comparative effectiveness research utilising quantitative and qualitative methods should be considered to enable us to secure the greatest density of knowledge possible. Stakeholders, such as citizens, patients and providers, should be involved in every stage of developing the specific and relevant research questions, study design and the assurance of real-world relevance for the research.
Furthermore, structural and sufficient financial support for research into SCAM is needed to strengthen SCAM research capacity if we wish to understand why it remains so popular within the EU. In order to consider employing SCAM as part of the solution to the health care, health creation and self-care challenges we face by 2020, it is vital to obtain a robust picture of SCAM use and reliable information about its cost, safety and effectiveness in real-world settings. We need to consider the availability, accessibility and affordability of SCAM. We need to engage in research excellence and utilise comparative effectiveness approaches and mixed methods to obtain this data.
Our recommendations are both strategic and methodological. They are presented for the consideration of researchers and funders while being designed to answer the important and implicit questions posed by EU citizens currently using SCAM in apparently increasing numbers. We propose that the EU actively supports an EU-wide strategic approach that facilitates the development of SCAM research. This could be achieved in the first instance through funding a European SCAM coordinating research office dedicated to foster systematic communication between EU governments, public, charitable and industry funders as well as researchers, citizens and other stakeholders. The aim of this office would be to coordinate research strategy developments and research funding opportunities, as well as to document and disseminate international research activities in this field.
With the aim to develop sustainability as second step, a European Centre for SCAM should be established that takes over the monitoring and further development of a coordinated research strategy for SCAM, as well as it should have funds that can be awarded to foster high quality and robust independent research with a focus on citizens health needs and pan-European collaboration.
We wish to establish a solid funding for SCAM research to adequately inform health care and health creation decision-making throughout the EU. This centre would ensure that our vision of a common, strategic and scientifically rigorous approach to SCAM research becomes our legacy and Europe’s reality. We are confident that our recommendations will serve these essential goals for EU citizens.
As I know all of the members of the panel personally, I am not surprised by the content of this document. That does not mean, however, that I do not find it remarkable. In my view, it is remarkable because of the nature of the 6 items that we allegedly need to know by 2020, and because of the fact that, even though none of them seem particularly demanding, today we have clarity or sound information on none of them. I also thought that both the research topics and the research methods were on the woolly side and, to a large degree, avoided what would be standard in conventional medicine. The ‘vision’ of the 13 researchers thus turns out to be the view of 13 partially sighted people on an array of platitudes.
Being just a bit sarcastic, the document could be seen as a plea for letting SCAM researchers:
- continue to play on their far from level playing field,
- use their preferred and largely inadequate methodologies,
- pretend they do cutting edge science,
- continue to avoid the real issues,
- enjoy a life free of demanding challenges,
- have pots of EU money for doing largely useless work.
In a word, I am confident that their recommendations would not have served any essential goals for EU citizens.
Maintenance Care is an approach whereby patients have chiropractic manipulations even when symptom-free. Thus, it is an ideal method to keep chiropractors in clover. Previous reviews concluded that evidence behind this strategy is lacking. Since then, more data have emerged. It was therefore timely to review the evidence.
Fourteen original research articles were included in the review. Maintenance Care was defined as a secondary or tertiary preventive approach, recommended to patients with previous pain episodes, who respond well to chiropractic care. Maintenance Care is applied to approximately 30% of Scandinavian chiropractic patients. Both chiropractors and patients believe in the efficacy of Maintenance Care. Four studies investigating the effect of chiropractic Maintenance Care were identified, with disparate results on pain and disability of neck and back pain. However, only one of these studies utilized all the existing evidence when selecting study subjects and found that Maintenance Care patients experienced fewer days with low back pain compared to patients invited to contact their chiropractor ‘when needed’. No studies were found on the cost-effectiveness of Maintenance Care.
The authors concluded that knowledge of chiropractic Maintenance Care has advanced. There is reasonable consensus among chiropractors on what Maintenance Care is, how it should be used, and its indications. Presently, Maintenance Care can be considered an evidence-based method to perform secondary or tertiary prevention in patients with previous episodes of low back pain, who report a good outcome from the initial treatments. However, these results should not be interpreted as an indication for Maintenance Care on all patients, who receive chiropractic treatment.
I have to admit, I have problems with these conclusions.
- Maintenance Care is not normally defined as secondary or tertitary prevention. It also includes primary prevention, which means that chiropractors recommend it for just about anyone. By definition it is long term care, that is not therapeutically necessary, but performed at regular intervals to help prevent injury and enhance quality of life. This form of care is provided after maximal therapeutic benefit is achieved, without a trial of treatment withdrawal, to prevent symptoms from returning or for those without symptoms to promote health or prevent future problems.
- I am not convinced that the evidence would be positive, even if we confined it to secondary and tertiary prevention.
To explain my last point, let’s have a look at the 4 RCT and check whether they really warrant such a relatively positive conclusion.
FIRST STUDY For individuals with recurrent or persistent non-specific low back pain (LBP), exercise and exercise combined with education have been shown to be effective in preventing new episodes or in reducing the impact of the condition. Chiropractors have traditionally used Maintenance Care (MC), as secondary and tertiary prevention strategies. The aim of this trial was to investigate the effectiveness of MC on pain trajectories for patients with recurrent or persistent LBP.
This pragmatic, investigator-blinded, two arm randomized controlled trial included consecutive patients (18–65 years old) with non-specific LBP, who had an early favorable response to chiropractic care. After an initial course of treatment, eligible subjects were randomized to either MC or control (symptom-guided treatment). The primary outcome was total number of days with bothersome LBP during 52 weeks collected weekly with text-messages (SMS) and estimated by a GEE model.
Three hundred and twenty-eight subjects were randomly allocated to one of the two treatment groups. MC resulted in a reduction in the total number of days per week with bothersome LBP compared with symptom-guided treatment. During the 12 month study period, the MC group (n = 163, 3 dropouts) reported 12.8 (95% CI = 10.1, 15.5; p = <0.001) fewer days in total with bothersome LBP compared to the control group (n = 158, 4 dropouts) and received 1.7 (95% CI = 1.8, 2.1; p = <0.001) more treatments. Numbers presented are means. No serious adverse events were recorded.
MC was more effective than symptom-guided treatment in reducing the total number of days over 52 weeks with bothersome non-specific LBP but it resulted in a higher number of treatments. For selected patients with recurrent or persistent non-specific LBP who respond well to an initial course of chiropractic care, MC should be considered an option for tertiary prevention.
SECOND STUDY Back and neck pain are associated with disability and loss of independence in older adults. Whether long‐term management using commonly recommended treatments is superior to shorter‐term treatment is unknown. This randomized clinical trial compared short‐term treatment (12 weeks) versus long‐term management (36 weeks) of back‐ and neck‐related disability in older adults using spinal manipulative therapy (SMT) combined with supervised rehabilitative exercises (SRE).
Eligible participants were ages ≥65 years with back and neck disability for ≥12 weeks. Coprimary outcomes were changes in Oswestry Disability Index (ODI) and Neck Disability Index (NDI) scores after 36 weeks. An intent‐to‐treat approach used linear mixed‐model analysis to detect between‐group differences. Secondary analyses included other self‐reported outcomes, adverse events, and objective functional measures.
THIRD STUDY A prospective single blinded placebo controlled study was conducted. To assess the effectiveness of spinal manipulation therapy (SMT) for the management of chronic nonspecific low back pain (LBP) and to determine the effectiveness of maintenance SMT in long-term reduction of pain and disability levels associated with chronic low back conditions after an initial phase of treatments. SMT is a common treatment option for LBP. Numerous clinical trials have attempted to evaluate its effectiveness for different subgroups of acute and chronic LBP but the efficacy of maintenance SMT in chronic nonspecific LBP has not been studied. Sixty patients, with chronic, nonspecific LBP lasting at least 6 months, were randomized to receive either (1) 12 treatments of sham SMT over a 1-month period, (2) 12 treatments, consisting of SMT over a 1-month period, but no treatments for the subsequent 9 months, or (3) 12 treatments over a 1-month period, along with “maintenance spinal manipulation” every 2 weeks for the following 9 months. To determine any difference among therapies, we measured pain and disability scores, generic health status, and back-specific patient satisfaction at baseline and at 1-, 4-, 7-, and 10-month intervals. Patients in second and third groups experienced significantly lower pain and disability scores than first group at the end of 1-month period (P = 0.0027 and 0.0029, respectively). However, only the third group that was given spinal manipulations (SM) during the follow-up period showed more improvement in pain and disability scores at the 10-month evaluation. In the nonmaintained SMT group, however, the mean pain and disability scores returned back near to their pretreatment level.SMT is effective for the treatment of chronic nonspecific LBP. To obtain long-term benefit, this study suggests maintenance SM after the initial intensive manipulative therapy.
FORTH STUDY Evidence indicates that supervised home exercises, combined or not with manual therapy, can be beneficial for patients with non-specific chronic neck pain (NCNP). The objective of the study is to investigate the efficacy of preventive spinal manipulative therapy (SMT) compared to a no treatment group in NCNP patients. Another objective is to assess the efficacy of SMT with and without a home exercise program.Ninety-eight patients underwent a short symptomatic phase of treatment before being randomly allocated to either an attention-group (n = 29), a SMT group (n = 36) or a SMT + exercise group (n = 33). The preventive phase of treatment, which lasted for 10 months, consisted of meeting with a chiropractor every two months to evaluate and discuss symptoms (attention-control group), 1 monthly SMT session (SMT group) or 1 monthly SMT session combined with a home exercise program (SMT + exercise group). The primary and secondary outcome measures were represented by scores on a 10-cm visual analog scale (VAS), active cervical ranges of motion (cROM), the neck disability index (NDI) and the Bournemouth questionnaire (BQ). Exploratory outcome measures were scored on the Fear-avoidance Behaviour Questionnaire (FABQ) and the SF-12 Questionnaire. Our results show that, in the preventive phase of the trial, all 3 groups showed primary and secondary outcomes scores similar to those obtain following the non-randomised, symptomatic phase. No group difference was observed for the primary, secondary and exploratory variables. Significant improvements in FABQ scores were noted in all groups during the preventive phase of the trial. However, no significant change in health related quality of life (HRQL) was associated with the preventive phase. This study hypothesised that participants in the combined intervention group would have less pain and disability and better function than participants from the 2 other groups during the preventive phase of the trial. This hypothesis was not supported by the study results. Lack of a treatment specific effect is discussed in relation to the placebo and patient provider interactions in manual therapies. Further research is needed to delineate the specific and non-specific effects of treatment modalities to prevent unnecessary disability and to minimise morbidity related to NCNP. Additional investigation is also required to identify the best strategies for secondary and tertiary prevention of NCNP.
__________________________________________________________________________
I honestly do not think that the findings from these 4 small trials justify the far-reaching conclusion that Maintenance Care can be considered an evidence-based method… For that statement to be evidence-based, one would need to see more and better studies. Therefore, the honest conclusion, I think, is that maintenance care is not supported by sound evidence for effectiveness; as chiropractic manipulations are costly and not risk-free, its risk/benefit balance fails to be positive. Therefore, this approach cannot be recommended.
I almost forgot!
This would have been no good, after all, Charles has for decades been the most influential supporter of so-called alternative medicine (SCAM) in the UK. He is one of SCAM’s greatest proponent.
So, here is my up-dated, extended and illustrated summary of his achievements in this area.
HAPPY BIRTHDAY CHARLES!
Charles went on a journey of ‘spiritual discovery’ into the wilderness of northern Kenya. His guru and guide at the time was Laurens van der Post (later discovered to be a fraud and compulsive fantasist and to have fathered a child with a 14-year old girl entrusted to him during a sea voyage).
 Van der Post wanted to awake Charles’ mind and attune it to the vitalistic ideas of Carl Jung’s ‘collective unconscious’, and it is this belief in vitalism that provides the crucial link to alternative medicine: virtually every form of alternative therapies is based on the assumption that some sort of vital force exists. Charles was so taken by van der Post that he made him the godfather of Prince William. After Post’s death, he established an annual lecture in his honour (the lecture series was discontinued after Van der Post was discovered to be a fraud).
Van der Post wanted to awake Charles’ mind and attune it to the vitalistic ideas of Carl Jung’s ‘collective unconscious’, and it is this belief in vitalism that provides the crucial link to alternative medicine: virtually every form of alternative therapies is based on the assumption that some sort of vital force exists. Charles was so taken by van der Post that he made him the godfather of Prince William. After Post’s death, he established an annual lecture in his honour (the lecture series was discontinued after Van der Post was discovered to be a fraud).

Some time in the 1970s, Charles met Jimmy Saville and befriended him. Apparently, Saville later advised Charles on several occasions in various health-related matters.

Throughout the 1980s, Charles lobbied for the statutory regulation of chiropractors and osteopaths in the UK. In 1993, this finally became reality. These two SCAM professions are to this day the only ones regulated by statute in the UK.
Osteopathy has strong Royal links: Prince Charles is the President of the GOsC; Princess Diana was the President of the GCRO; and Princess Anne is the patron of the British School of Osteopathy (statement dated 2011).
In 1982, Prince Charles was elected as President of the British Medical Association (BMA) and promptly challenged the medical orthodoxy by advocating alternative medicine. In a speech at his inaugural dinner as President, the Prince lectured the medics: ‘Through the centuries healing has been practised by folk healers who are guided by traditional wisdom which sees illness as a disorder of the whole person, involving not only the patient’s body, but his mind, his self-image, his dependence on the physical and social environment, as well as his relation to the cosmos.’ The BMA-officials ordered a full report on alternative medicine which promptly condemned this area as implausible nonsense.
Six years later, a second report, entitled Complementary Medicine – New Approaches to Good Practice, heralded an astonishing about-turn stating that: “the demand for non-conventional therapies had become so pressing that organised medicine in Britain could no longer ignore its contribution”. At the same time, however, the BMA set in motion a further chapter in the history of SCAM by insisting that it was “unacceptable” to allow the unrestricted practice of non-conventional therapies, irrespective of training or experience.
In 1993, Charles founded his lobby group which, after being re-named several times, ended up being called the ‘Foundation for Integrated Health’ (FIH). It was closed down in 2010 amidst allegations of money laundering and fraud. Its chief executive, George Gray, was later convicted and went to jail. The FIH had repeatedly been a little economical with the truth.
In 2000, Charles wrote an open letter to The Times stating that…It makes good sense to evaluate complementary and alternative therapies. For one thing, since an estimated £1.6 billion is spent each year on them, then we want value for our money. The very popularity of the non-conventional approaches suggests that people are either dissatisfied with their orthodox treatment, or they find genuine relief in such therapies. Whatever the case, if they are proved to work, they should be made more widely available on the NHS…But there remains the cry from the medical establishment of “where’s the proof?” — and clinical trials of the calibre that science demands cost money…The truth is that funding in the UK for research into complementary medicine is pitiful…So where can funding come from?…Figures from the department of complementary medicine at the University of Exeter show that less than 8p out of every £100 of NHS funds for medical research was spent on complementary medicine. In 1998-99 the Medical Research Council spent no money on it at all, and in 1999 only 0.05 per cent of the total research budget of UK medical charities went to this area…
In 2001, Charles worked on plans to help build a model hospital of integrated medicine. It was to train doctors to combine conventional medicine and alternative treatments, such as homeopathy, Ayurvedic medicine and acupuncture, and was to have up to 100 beds. The prince’s intervention marked the culmination of years of campaigning by him for the NHS to assign a greater role to alternative medicine. Teresa Hale, founder of the Hale Clinic in London, said: “Twenty-five years ago people said we were quacks. Now several branches, including homeopathy, acupuncture and osteopathy, have gained official recognition.” The proposed hospital, which was due to open in London in 2003/4, was to be overseen by Mosaraf Ali, who runs the Integrated Medical Centre (IMC) in London. But the hospital never materialised.
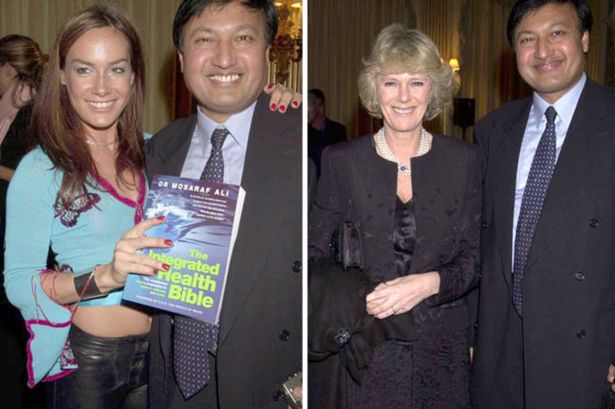
This might be due to Mosaraf Ali falling in disrepute: Raj Bathija, 69 and from India, went for a massage at the clinic of Dr Mosaraf Ali and his brother Imran in 2005 after suffering from two strokes. However, he claims that shortly after the treatment, his legs became pale and discoloured. Four days afterwards, Mr Bathija was admitted to hospital, where he had to have both legs amputated below the knee due to a shortage of blood. According to Mr Bathija, Dr Ali and his brother were negligent in that they failed to diagnose his condition and neglected to advise him to go to hospital. His daughter Shibani said: “My father was in a wheelchair but was making progress with his walking. He hoped he might become a bit more independent. With the amputations, that’s all gone.” Dr Ali was sued (if anyone knows the outcome of this case, please let me know).
At the age of 53, Mrs Parker Bowles went on a trek to the Himalayas to ‘re-energise’ her spirits and encourage her to give up smoking. She was in a party of 12 accompanied by the Prince of Wales’s favourite health guru, Dr Mosaraf Ali. Mrs Parker Bowles subsequently became a regular visitor to Dr Ali’s London practice where she has been encouraged to take up yoga both to combat her back pain and to help her give up smoking.
In the same year, Charles published an editorial in the BMJ promoting his ideas around integrative medicine. Its title: THE BEST OF BOTH WORLDS.
In 2003, Prince Charles’ FIH launched a five-year plan which outlined how to improve access to alternative therapies.
In 2004, Charles publicly supported the Gerson diet as a treatment for cancer and Prof Baum, an eminent oncologist, was invited to respond in an open letter to the British Medical Journal: …Over the past 20 years I have treated thousands of patients with cancer and lost some dear friends and relatives to this dreaded disease…The power of my authority comes with knowledge built on 40 years of study and 25 years of active involvement in cancer research. Your power and authority rest on an accident of birth. I don’t begrudge you that authority but I do beg you to exercise your power with extreme caution when advising patients with life-threatening diseases to embrace unproven therapies.
In 2005, the ‘Smallwood-Report’ was published; it had been commissioned by Charles and paid for by Dame Shirley Porter to inform health ministers. It stated that up to 480 million pounds could be saved, if one in 10 family doctors offered homeopathy as an “alternative” to standard drugs for asthma. Savings of up to 3.5 billion pounds could be achieved by offering spinal manipulation rather than drugs to people with back pain. Because I had commented on this report, Prince Charles’ first private secretary asked my vice chancellor to investigate my alleged indiscretion; even though I was found to be not guilty of any wrong-doing, all local support at Exeter stopped which eventually led to my early retirement. ITV later used this incident in a film entitled THE MEDDLING PRINCE, I later published a full account of this sad story in my memoir.
In a 2006 speech, Prince Charles told the World Health Organisation in Geneva that alternative medicine should have a more prominent place in health care and urged every country to come up with a plan to integrate conventional and alternative medicine into the mainstream. But British science struck back. Anticipating Prince Charles’s sermon in Geneva, 13 of Britain’s most eminent physicians and scientists wrote an “Open Letter” which expressed concern over “ways in which unproven or disproved treatments are being encouraged for general use in Britain’s National Health Service.” The signatories argued that “it would be highly irresponsible to embrace any medicine as though it were a matter of principle.”
In 2008, The Times published my letter asking the FIH to withdraw two guides promoting alternative medicine, stating: “the majority of alternative therapies appear to be clinically ineffective, and many are downright dangerous.” A speaker for the FIH countered the criticism by stating: “We entirely reject the accusation that our online publication Complementary Healthcare: A Guide contains any misleading or inaccurate claims about the benefits of complementary therapies. On the contrary, it treats people as adults and takes a responsible approach by encouraging people to look at reliable sources of information… so that they can make informed decisions. The foundation does not promote complementary therapies.”
In 2009, the Prince held talks with the health Secretary to persuade him to introduce safeguards amid a crackdown by the EU that could prevent anyone who is not a registered health practitioner from selling remedies. This, it seems, was yet another example of Charles’ disregard of his constitutional role.
In the same year, Charles urged the government to protect alternative medicine because “we fear that we will see a black market in herbal products”, as Dr Michael Dixon (LVO,2015; OBE 2001), then medical director of Charles’ FIH, put it.
In 2009, the health secretary wrote to the prince suggesting a meeting on the possibility of a study on integrating complementary and conventional healthcare approaches in England. The prince had written to Burnham’s predecessor, Alan Johnson, to demand greater access to complementary therapies in the NHS alongside conventional medicine. The prince told him that “despite waves of invective over the years from parts of the medical and scientific establishment” he continued to lobby “because I cannot bear people suffering unnecessarily when a complementary approach could make a real difference”. He opposed “large and threatened cuts” in the funding of homeopathic hospitals and their possible closure. He complained that referrals to the Royal London homeopathic hospital were increasing “until what seems to amount to a recent ‘anti-homeopathic campaign’”. He warned against cuts despite “the fact that these homeopathic hospitals deal with many patients with real health problems who otherwise would require treatment elsewhere, often at greater expense”.
In 2009, it was announced that the ‘College of Integrated Medicine’ (the name was only later changed to ‘College of Medicine’, see below) was to have a second base in India. An Indian spokesman commented: “The second campus of the Royal College will be in Bangalore. We have already proposed the setting up of an All India Institute of Integrated Medicine to the Union health ministry. At a meeting in London last week with Prince Charles, we finalized the project which will kick off in July 2010”.
In 2010, Charles publicly stated that he was proud to be perceived as ‘an enemy of the enlightenment’.
In 2010, ‘Republic’ filed an official complaint about FIH alleging that its trustees allowed the foundation’s staff to pursue a public “vendetta” against a prominent critic of the prince’s support for complementary medicines. It also suggested that the imminent closure of Ernst’s department may be partly down to the charity’s official complaint about him after he publicly attacked its draft guide to complementary medicines as “outrageous and deeply flawed”.
In 2010, former fellows of Charles’ disgraced FIH launched a new organisation, The College of Medicine’ supporting the use of integrated treatments in the NHS. One director of the college is Michael Dixon, a GP in Cullompton, formerly medical director of the Foundation for Integrated Health. My own analysis of the activities of the new college leaves little doubt that it is promoting quackery.
In 2010, Charles published his book HARMONY which is full of praise for even the most absurd forms of alternative therapies and even bogus diagnostic tests used by alternative practitioners.

In 2011, after the launch of Charles’ range of herbal tinctures, I had the audacity to publicly criticise Charles for selling the Duchy Herbals detox tincture which I named ‘Dodgy Originals Detox Tincture’.

In 2011, Charles forged a link between ‘The College of Medicine’ and an Indian holistic health centre (see also above). The collaboration was reported to include clinical training to European and Western doctors in ayurveda and homoeopathy and traditional forms of medicine to integrate them in their practice. The foundation stone for the extended campus of the Royal College known as the International Institution for Holistic and Integrated Medicine was laid by Dr Michael Dixon in collaboration with the Royal College of Medicine.
In 2012, Charles was nominated for ‘THE GOLDEN DUCK AWARD’ for his achievements in promoting quackery. However, Andrew Wakefield beat him to it; Charles certainly was a deserving runner-up.
In 2013, Charles called for society to embrace a broader and more complex concept of health. In his article he described a vision of health that includes the physical and social environment, education, agriculture and architecture.
In 2013, Charles’ Highgrove enterprise offered ‘baby-hampers’ for sale at £195 a piece and made a range of medicinal claims for the products it contained. As these claims were not supported by evidence, there is no way to classify them other than quackery.
By 2013, the ‘Association of Osteomyologists’ were seeking to become regulated by statute, with the help of Prince Charles as their patron. The chairman and founder of this organisation was knighted for services to alternative medicine. Osteomyologists encourage the use of techniques including cranio-sacral therapy and claim that “we all know that Colleges, Institutions, and Medical Practitioners, are brain washed from the very outset into believing that their discipline is the only way to go.”
In November 2013, Charles invited alternative medicine proponents from across the world, including Dean Ornish, Michael Dixon, chair of College of Medicine, UK and Issac Mathai of Soukya Foundation, Bangalore, to India for a ‘brain storm’ and a subsequent conference on alternative medicine. The prince wanted the experts to collaborate and explore the possibilities of integrating different systems of medicines and to better the healthcare delivery globally, one of the organisers said.

In June 2014, BBC NEWS published the following text about a BBC4 broadcast entitled ‘THE ROYAL ACTIVIST’ aired on the same day: Prince Charles has been a well-known supporter of complementary medicine. According to a… former Labour cabinet minister, Peter Hain, it was a topic they shared an interest in. He had been constantly frustrated at his inability to persuade any health ministers anywhere that that was a good idea, and so he, as he once described it to me, found me unique from this point of view, in being somebody that actually agreed with him on this, and might want to deliver it. Mr Hain added: “When I was Secretary of State for Northern Ireland in 2005-7, he was delighted when I told him that since I was running the place I could more or less do what I wanted to do.*** I was able to introduce a trial for complementary medicine on the NHS, and it had spectacularly good results, that people’s well-being and health was vastly improved. And when he learnt about this he was really enthusiastic and tried to persuade the Welsh government to do the same thing and the government in Whitehall to do the same thing for England, but not successfully,” added Mr Hain. On this blog, I have pointed out that the research in question was fatally flawed and that Charles, once again, overstepped the boundaries of his constitutional role.
In 2015, two books were published which are relevant in this context. My memoir A SCIENTIST IN WONDERLAND recounts most of my dealings with Charles and his sycophants, including how an intervention from his first private secretary eventually led to the closure of my department. The book by Catherine Meyer CHARLES, THE HEART OF A KING is far less critical about our heir to the throne; it nevertheless severely criticises his stance on alternative medicine.
In October 2015, the Guardian obtained the infamous “black spider memos” which revealed that Charles had repeatedly lobbied politicians in favour of alternative medicine (see also above).
 In 2016, speaking at a global leaders summit on antimicrobial resistance, Prince Charles warned that Britain faced a “potentially disastrous scenario” because of the “overuse and abuse” of antibiotics. The Prince explained that he had switched to organic farming on his estates because of the growing threat from antibiotic resistance and now treats his cattle with homeopathic remedies rather than conventional medication. “As some of you may be aware, this issue has been a long-standing and acute concern to me,” he told delegates from 20 countries “I have enormous sympathy for those engaged in the vital task of ensuring that, as the world population continues to increase unsustainably and travel becomes easier, antibiotics retain their availability to overcome disease… It must be incredibly frustrating to witness the fact that antibiotics have too often simply acted as a substitute for basic hygiene, or as it would seem, a way of placating a patient who has a viral infection or who actually needs little more than patience to allow a minor bacterial infection to resolve itself.”
In 2016, speaking at a global leaders summit on antimicrobial resistance, Prince Charles warned that Britain faced a “potentially disastrous scenario” because of the “overuse and abuse” of antibiotics. The Prince explained that he had switched to organic farming on his estates because of the growing threat from antibiotic resistance and now treats his cattle with homeopathic remedies rather than conventional medication. “As some of you may be aware, this issue has been a long-standing and acute concern to me,” he told delegates from 20 countries “I have enormous sympathy for those engaged in the vital task of ensuring that, as the world population continues to increase unsustainably and travel becomes easier, antibiotics retain their availability to overcome disease… It must be incredibly frustrating to witness the fact that antibiotics have too often simply acted as a substitute for basic hygiene, or as it would seem, a way of placating a patient who has a viral infection or who actually needs little more than patience to allow a minor bacterial infection to resolve itself.”
In 2017, the ‘College of Medicine’ mentioned above was discretely re-named ‘College of Medicine and Integrated Health’
In the same year, Charles declared that he will open a centre for alternative medicine in the recently purchased Dumfries House in Scotland. Currently, the College of Medicine and Integrated Health is offering two-day Foundation Courses at this iconic location. Gabriel Chiu, a US celebrity cosmetic and reconstructive surgeon, and his wife Christine, joined the Prince of Wales as he opened the integrated health and wellbeing centre on the Dumfries House Estate in East Ayrshire in 2019. As he unveiled a plaque at the event, Prince Charles said: “I’m so glad that all of you have been able to get here today, particularly because I could not be more proud to see the opening of this new integrated health centre at Dumfries House. It’s something I’ve been wanting to do for the last 35 years. I’m also so proud of all the team at Dumfries House who built it, an all in-house team.
“To reach this point where we can now offer a range of social prescribing opportunities is enormously encouraging and I hope it will be able to make some difference to a lot of the health issues that exist in this area.”
Also in 2017, ‘Country News’ published an article about our heir to the throne stating that Prince of Wales has revealed he uses homeopathic treatments for animals on his organic farm at Highgrove to help reduce reliance on antibiotics, the article stated. He said his methods of farming tried wherever possible to ‘‘go with the grain of nature’’ to avoid dependency on antibiotics, pesticides and other forms of chemical intervention.
In 2018, The Prince of Wales accompanied the Prime Minister of India, Narendra Modi, to the Science Museum in London, and praised Asian medicine practices. The heir to the throne and the Indian Prime Minister then jointly unveiled a plaque for the UK’s first centre of excellence for Indian traditional medicine.
In the same year, it was revealed that UK farmers are being taught how to treat their livestock with homeopathy “by kind permission of His Royal Highness, The Prince Of Wales”
In 2019, the Faculty of Homeopathy announced that His Royal Highness The Prince of Wales had accepted to become Patron of the Faculty of Homeopathy. Dr Gary Smyth, President of the Faculty of Homeopathy comments, “As the Faculty celebrates its 175th anniversary this year, it is an enormous honour for us to receive the Patronage of His Royal Highness The Prince of Wales and I am delighted to announce this news today.” Charles’ move amazed observers who saw it as a deliberate protest against the discontinuation of reimbursement of homeopathy by the NHS.
In 2019, Prince Charles said that yoga had “proven beneficial effects on both body and mind,” and has “tremendous social benefits” that help build “discipline, self-reliance and self-care.”
___________________________________________________________________
So again, Happy Birthday Your Royal Highness – and please don’t forget: it’s not too late to start doing good in the realm of healthcare by supporting good science, critical thinking and evidence-based medicine.
Sincerely yours
Edzard Ernst
The World Federation of Chiropractic (WFC) claim to have been at the forefront of the global development of chiropractic. Representing the interests of the profession in over 90 countries worldwide, the WFC has advocated, defended and promoted the profession across its 7 world regions. Now, the WFC have formulated 20 principles setting out who they are, what they stand for, and how chiropractic as a global health profession can, in their view, impact on nations so that populations can thrive and reach their full potential. Here are the 20 principles (in italics followed by some brief comments by me in normal print):
1. We envision a world where people of all ages, in all countries, can access the benefits of chiropractic.
That means babies and infants! What about the evidence?
2. We are driven by our mission to advance awareness, utilization and integration of chiropractic internationally.
One could almost suspect that the drive is motivated by misleading the public about the risks and benefits of spinal manipulation for financial gain.
3. We believe that science and research should inform care and policy decisions and support calls for wider access to chiropractic.
If science and research truly did inform care, it would soon be chiropractic-free.
4. We maintain that chiropractic extends beyond the care of patients to the promotion of better health and the wellbeing of our communities.
The best example to show that this statement is a politically correct platitude is the fact that so many chiropractors are (educated to become) convinced that vaccinations are undesirable or harmful.
5. We champion the rights of chiropractors to practice according to their training and expertise.
I am not sure what this means. Could it mean that they must practice according to their training and expertise, even if both fly in the face of the evidence?
6. We promote evidence-based practice: integrating individual clinical expertise, the best available evidence from clinical research, and the values and preferences of patients.
So far, I have seen little to convince me that chiropractors care a hoot about the best available evidence and plenty to fear that they supress it, if it does not enhance their business.
7. We are committed to supporting our member national associations through advocacy and sharing best practices for the benefit of patients and society.
Much more likely for the benefit of chiropractors, I suspect.
8. We acknowledge the role of chiropractic care, including the chiropractic adjustment, to enhance function, improve mobility, relieve pain and optimize wellbeing.
Of course, you have to pretend that chiropractic adjustments (of subluxations) are useful. However, evidence would be better than pretence.
9. We support research that investigates the methods, mechanisms, and outcomes of chiropractic care for the benefit of patients, and the translation of research outcomes into clinical practice.
And if it turns out to be to the detriment of the patient? It seems to me that you seem to know the result of the research before you started it. That does not bode well for its reliability.
10. We believe that chiropractors are important members of a patient’s healthcare team and that interprofessional approaches best facilitate optimum outcomes.
Of course you do believe that. Why don’t you show us some evidence that your belief is true?
11. We believe that chiropractors should be responsible public health advocates to improve the wellbeing of the communities they serve.
Of course you do believe that. But, in fact, many chiropractors are actively undermining the most important public health measure, vaccination.
12. We celebrate individual and professional diversity and equality of opportunity and represent these values throughout our Board and committees.
What you should be celebrating is critical assessment of all chiropractic concepts. This is the only way to make progress and safeguard the interests of the patient.
13. We believe that patients have a fundamental right to ethical, professional care and the protection of enforceable regulation in upholding good conduct and practice.
The truth is that many chiropractors violate medical ethics on a daily basis, for instance, by not obtaining fully informed consent.
14. We serve the global profession by promoting collaboration between and amongst organizations and individuals who support the vision, mission, values and objectives of the WFC.
Yes, those who support your vision, mission, values and objectives are your friends; those who dare criticising them are your enemies. It seems far from you to realise that criticism generates progress, perhaps not for the WFC, but for the patient.
15. We support high standards of chiropractic education that empower graduates to serve their patients and communities as high value, trusted health professionals.
For instance, by educating students to become anti-vaxxers or by teaching them obsolete concepts such as adjustment of subluxation?
16. We believe in nurturing, supporting, mentoring and empowering students and early career chiropractors.
You are surpassing yourself in the formulation of platitudes.
17. We are committed to the delivery of congresses and events that inspire, challenge, educate, inform and grow the profession through respectful discourse and positive professional development.
You are surpassing yourself in the formulation of platitudes.
18. We believe in continuously improving our understanding of the biomechanical, neurophysiological, psychosocial and general health effects of chiropractic care.
Even if there are no health effects?!?
19. We advocate for public statements and claims of effectiveness for chiropractic care that are honest, legal, decent and truthful.
Advocating claims of effectiveness in the absence of proof of effectiveness is neither honest, legal, decent or truthful, in my view.
20. We commit to an EPIC future for chiropractic: evidence-based, people-centered, interprofessional and collaborative.
And what do you propose to do with the increasing mountain of evidence suggesting that your spinal adjustments are not evidence-based as well as harmful to the health and wallets of your patients?
________________________________________________________________
What do I take out of all this? Not a lot!
Perhaps mainly this: the WFC is correct when stating that, in the interests of the profession in over 90 countries worldwide, the WFC has advocated, defended and promoted the profession across its 7 world regions. What is missing here is a small but important addition to the sentence: in the interests of the profession and against the interest of patients, consumers or public health in over 90 countries worldwide, the WFC has advocated, defended and promoted the profession across its 7 world regions.
There is a long-standing debate on the question whether the use of homeopathy saves money. Homeopathy fans usually insist that it does. Even the Smallwood report commissioned by Prince Charles claimed that the NHS could save pots of money, if GPs only used more homeopathy.
And it is true, of course: on average homeopathics are cheaper than drugs. Therefore, replacing drugs with homeopathics would be a cost-saving. But, in healthcare, we cannot think like this; if we did, this logic would tell us that not doing anything at all would be even cheaper.
Somehow, we need to factor into the equation the effectiveness of the interventions that we are evaluating. The way to do this is to conduct proper cost-effectiveness analyses. And the reliable evidence from such assessments fails to confirm the notion that homeopathy might save us money.
So, why did I entitle this post HOW TO SAVE MONEY WITH HOMEOPATHY?
Because, it is true: you can save money, if you adhere to my instructions!
If you or a friend of yours are ill and therefore tempted by the numerous claims of homeopaths, please follow this simple step by step procedure:
- Go to your library, find a reliable book (I recommend this one), inform yourself what homeopathy truly is and absorb in the fact that a typical homeopathic remedy contains exactly zero active molecules.
- Read a bit further and check out what the best evidence from rigorous clinical trials tells us about the effectiveness of homeopathy.
- Go to a pharmacy that specialises in homeopathic products.
- Ask the pharmacist which homeopathic remedies she recommends for the ailment you suffer from.
- Ask the pharmacist to tell you what these would cost.
- Tell the pharmacist what you have just learnt about the evidence.
- Ask her kindly not to mislead customers in future.
- Go home.
- Repeat 3 – 8 as often as you can.
I think you have to agree that by following my instructions, you have saved exactly the amount of money that the pharmacist quoted.
PS
And for those for whom this advice comes too late, because they already have at home a selection of homeopathic remedies, I have the following cost-saving trick: use them for sweetening your tea or coffee. This saves you the cost of buying sugar – every little bit helps!
