EBM
In Austria, even some of the most blatant quackery continues to be supported by the country’s medical association. This has been notorious for a very long time, and many rational doctors have opposed this nonsense. Now my friends and colleagues have courageously sent an open letter to the President of the Austrian Medical Association. In order to support their efforts, I have taken the liberty of translating it:
Dr. Johannes Steinhart
President of the Austrian Medical Association
Weihburggasse 10-12
1010 Vienna
Dear President Steinhart,
In 2014 we founded the “Initiative for Scientific Medicine” with the aim of counteracting the support of pseudo-medicine by medical associations and the Ministry of Health.
We (www.initiative-wissenschaftliche-medizin.at) have been demanding for years that the Austrian Medical Association distance itself from irrational, predominantly esoteric pseudo-medicine and refrain from awarding diplomas in them. We also made these demands on behalf of the supporters of the initiative (currently 1142 supporters, of which 495 are female doctors and 230 natural scientists) during a discussion with the former president Wechselberger in 2015 (unfortunately unsuccessful at the time).
We would like to draw your attention to a resolution of the German Medical Congress 2022 on homeopathy and a court ruling in the first instance in Germany on the subject of bioresonance, which show that our neighbours have obviously begun to treat pseudomedicine for what it is, namely sham medicine.
The 126th German Medical Congress 2022 in Bremen has, among other things, passed a long overdue resolution. The additional title “homeopathy” was deleted from the (model) further training regulations. Prior to this decision, 12 of 17 state medical associations had already taken this decision themselves.
In May 2022 in Reutlingen, two managing directors of a company producing and selling bioresonance devices were sentenced to 2 and 3 years in prison and a fine of 2.5 million euros, and the former sales director to 90 days’ imprisonment for commercial fraud and violation of the Therapeutic Products Advertising Act. The verdict is not yet legally binding. Unfortunately, many Austrian doctors also practice this pseudo-medicine method.
The fact that many colleagues offer esoteric, pseudo-medical “therapies” without proven benefits to their patients and can refer to diplomas and accredited further training courses of the Medical Association/Academy of Physicians is difficult for us to understand, especially in view of the fact that the majority of the accredited further training courses are of high scientific quality. A medical association that argues that such pseudo-medical practices “should better remain in the hands of doctors (as “healers”)” contradicts the principles of evidence-based medicine to which the medical association always refers. The corona pandemic has shown us all the damage potential of science denial.
We believe that the time has also come for the Austrian Medical Association to come clean. We call on the Austrian Medical Association to unreservedly declare its support for scientific medicine, to clearly distance itself from pseudo-medicine, to suspend the awarding of diplomas in pseudo-medicine methods that are far removed from science, and to end the accreditation of pseudo-medicine training courses by the Medical Academy.
We are publishing this open letter on our website and will also publish your reply if you so wish.
With collegial greetings
Dr. Theodor Much, Specialist in Dermatology and Venereology, Baden near Vienna
DDr. Viktor Weisshäupl, retired specialist in anaesthesiology and intensive care medicine, Vienna
It has been reported by several sources that the NHS is advertising for a Reiki healer.
The NHS stated that “the responsibilities of a reiki healer include treating clients using energy principles … and activating the healing process.” The post is paid for by the Sam Buxton Sunflower Healing Trust (SBSHT) which states on its website:
The SBSHT healing therapists, who work within the NHS and other health areas, are proud to be part of a multi-disciplinary team of professionals to provide vital support cancer patients, their relatives and staff. Since 2006, the SBSHT has funded healers to work in NHS, and other health related areas to support cancer patients and their families. A key role of the SBSHT is to increase awareness within the UK of the importance of providing healing support to cancer patients and families. Another vital role is to generate the crucial funds needed to place more healers in NHS, and other health related areas, throughout the country. Complementary therapy (CT) is increasingly demanded and expected by patients undergoing cancer treatments. An increasing amount of research clearly demonstrates that CT is important to support patients through their conventional treatments. SBSHT is committed to providing funds to NHS hospitals and cancer centers to engage the services of a Reiki practitioner or Healer for cancer patients and their families
As a charity we are or have funded healer posts within the centres below.
- University College Hospital, London
- Addenbrookes Hospital, Cambridge
- Princess Alexandra Hospital, Epping
- Queen Elizabeth Hospital, Welwyn Garden City
- Derriford Hospital, Plymouth
- Wigan NHS Trust, Wigan
- St Josephs Hospice, London
- Eden Valley Hospice and Jigsaw Children’s Hospice, Carlisle
- St Mary’s Hospice, Ulverston and Barrow in Furness NHS Trust
- St Johns Hospice, Lancaster
- Kent and Canterbury Hospital, Canterbury
- Bristol Haematology and Oncology Centre, Bristol
- Rowcroft Hospice, Torquay
- The Lister Hospital, Stevenage
- Barnstaple NHS Trust
- Treliske Hospital, Cornwall
- Poole NHS Trust
- St Michaels Hospice, Herefordshire
The SBSHT was co-founded by Angie Buxton-King in memory of her son Sam, who died of Acute Myeloid Leukaemia in 1998 aged 10. She is a member of the ‘College of Psychic Studies’ which is “committed to serving the evolution of consciousness”. The College website states this:
We were founded in 1884 to support and encourage empirical research into the esoteric. Our programme has since broadened and diversified to meet rising demand and increasingly global interests.
However, our core values remain the same. We continue to shine a light on key themes including consciousness, intuition, self-development and meditation. Our courses, workshops, talks and special events provide a safe and inclusive space in which to explore the full spectrum of human potential under the careful guidance of our expert tutors.
The College offers all sorts of courses; I was particularly fascinated by this one: “Alchemise Your Energy Through Dowsing“.
__________________
Now, one could easily claim that there is nothing wrong with reiki healers invading the NHS; after all, they are funded by a charitable trust at no cost to the taxpayer.
Yet, I disagree!
Reiki healing is implausible and ineffective nonsense. As such it is by no means harmless. Employing such healers in the NHS sends out a strong signal that undermines the principles of rational thinking and evidence-based medicine. If the NHS truly does not value these principles, I suggest they also fill the chronic gaps in ambulance services by flying carpets.
Trevor Zierke is a D.C. who published several videos that have gone viral after saying that “literally 99% of my profession” is a scam. “When I say almost all the usual lines chiropractors tell you are lies, I mean almost all of them,” he stated. Zierke then went on to give examples of issues chiropractors allegedly make up, including someone’s spine being “misaligned,” tension on nerves causing health problems, and someone having back pain because their hips are off-center. “Almost all of these aren’t true,” he concluded.
In a follow-up video, he claimed that the reasons most people are told they need to go to a chiropractor are “overblown or just flat out lies proven wrong by research.” He also noted that, while there are many scams, that “doesn’t mean you can’t get help from a chiropractor.”
In a third TikTok video, Zierke offered some valid reasons to see a chiropractor. He said that one can seek help from a chiropractor if one has musculoskeletal pain that has been ongoing for more than one to two days, and that’s about it. He stated that issues that a chiropractor couldn’t really fix include “GI pain, hormonal issues, nutrition,” among others.
In comments, users were largely supportive of Zierke’s message.
One said: “As a physiotherapist, I’ve been trying to tell this but I don’t want to like offend any chiropractor in doing so,” a commenter shared.
“Working in a chiropractic office, this is fair,” a further user wrote. “I have issues that I know an adjustment will help & other pain that would be better stretched/released.”
In an email, Zierke reiterated the intention of his videos: “I would just like to clarify that chiropractors, in general, are not a scam or are inherently scammers (I myself am a practicing chiropractor), but rather a lot of very popular sales tactics, phrases, and wording used to imply patients need treatment, and methods of treatment, have never been proven to be true,” he explained. “When chiropractors say & use these methods stating things that are not factually true—I believe it’s scammy behavior and practices. There are still a lot of very good, honest, and integral chiropractors out there,” he concluded. “They can provide a lot of help and relief to patients. But that’s unfortunately not the majority, and I’ve heard too many stories of people falling victim to some of these scam-like tactics from bad apple chiropractors.”
None of what DC Zierke said can surprise those who have been following my blog. On the contrary, I could add a few recent posts to his criticism of chiropractic, for example:
- Pediatric chiropractic seems to be on the rise
- Catastrophic injuries after chiropractic treatment
- Chiropractic: “a safe form of treatment”?
- Malpractice Litigation Involving Chiropractic Spinal Manipulation
- Best Practices for the Chiropractic Care of Children
- No effect from adding chiropractic manipulations to exercises for neck pain
- Hurray! The new professional standard by the General Chiropractic Council protects UK chiropractors
- Manual therapy (mainly chiropractic and osteopathy) does not have clinically relevant effects on back pain compared with sham treatment
- Chiropractic Paediatric Courses … it is high time to stop this dangerous nonsense
- Chiropractic ‘subluxation’ is by no means a notion of the past
- Another indirect risk of chiropractic
- And again: chiropractic for infant colic
- Chiropractic misinformation during the COVID-19 pandemic
- The lack of chiropractic ethics: “valid consent was not obtained in a single case”
I rest my case.
About a year ago, I reported last on the situation of homeopathy in France. Now it might be time for another update. The end of the reimbursement of homeopathy was, of course, a heavy blow for the laboratories concerned, especially Boiron and Weleda.
Are these firms now going bust?
Is the French public missing homeopathy?
The cessation of reimbursement took place in two steps: in 2020, the reimbursement rate was reduced to 15 % and expired completely in 2021. The new director of Weleda France, Ludovic Rassat, explains that, in 2020, when the reimbursement was reduced to 15 %, the impact on sales was just 20 %. The decrease was limited because of the supplementary health insurance which 80 % of French people have still supplemented the reimbursement up to 100 %. In 2021, this generosity stopped and the reimbursement fell from 100 to 0 %. This led to a 60 % drop in sales and to losses of 13 million Euros for Weleda France.
According to an Ipsos survey commissioned by Boiron Laboratories in October 2018, 70 % of all French used homeopathy to relieve their first symptoms, 74 % thought homeopathic remedies were effective and 71 % thought homeopathy was a good complement to conventional treatments. One might, therefore, have assumed that French consumers would continue using their beloved remedies despite the cessation of reimbursement. However, this was not the case. The most obvious explanation for this phenomenon, I think, is that the above-mentioned survey had generated false-positive results and that people correctly judged homeopathic remedies to be superfluous.
Faced with unsustainable losses, the French manufacturers of homeopathic products are now forced to react. A press release by Weleda France from 4 July 2022 stated that “This project would result in the discontinuation of pharmaceutical production and medical information in France and the closure of the Weleda division. This would result in the cessation of production activities at the Huningue site and an adjustment of the organisation of activities at headquarters. In total, 127 jobs could be cut at Weleda France.” If this step is taken as planned, Weleda France will have to earn its money purely on its cosmetic and anthroposophical products, according to the director.
In 2019, Laboratoires Boiron owned 4 production laboratories and 28 distribution facilities in France. In March 2020, the company announced that it had decided to cut 646 jobs in France and close 13 of its 31 sites, due to the poor economic results that followed the cessation of reimbursement of its products by the social security system. Following the decision by the Minister of Health, Agnès Buzyn, to stop the reimbursement of homeopathic preparations by the social security system, Boiron announced that the Montrichard site in the Loir-et-Cher region had not managed to find a buyer. As a result, the site, which employed around 80 people, closed on 31 December 2021.
And the French consumers?
Are they missing homeopathy?
Are they suffering from homeopathy withdrawal?
Are they more frequently ill without homeopathy?
Are they switching to more expensive conventional drugs?
I currently spend much of my time in France and cannot say that I have noticed any of this. On the contrary, most people I talk to are delighted that homeopathy is no longer reimbursed. But this is no evidence, of course. I am unable to find any reliable data to answer the above questions.
When the French health minister decided against homeopathy two years ago, she said: “It’s possible to leave the doctor’s office without a prescription! Let’s take advantage of this debate on homeopathy to reflect more broadly on our use of medicine. The ultimate goal is to consume less.” She was correct, it seems.
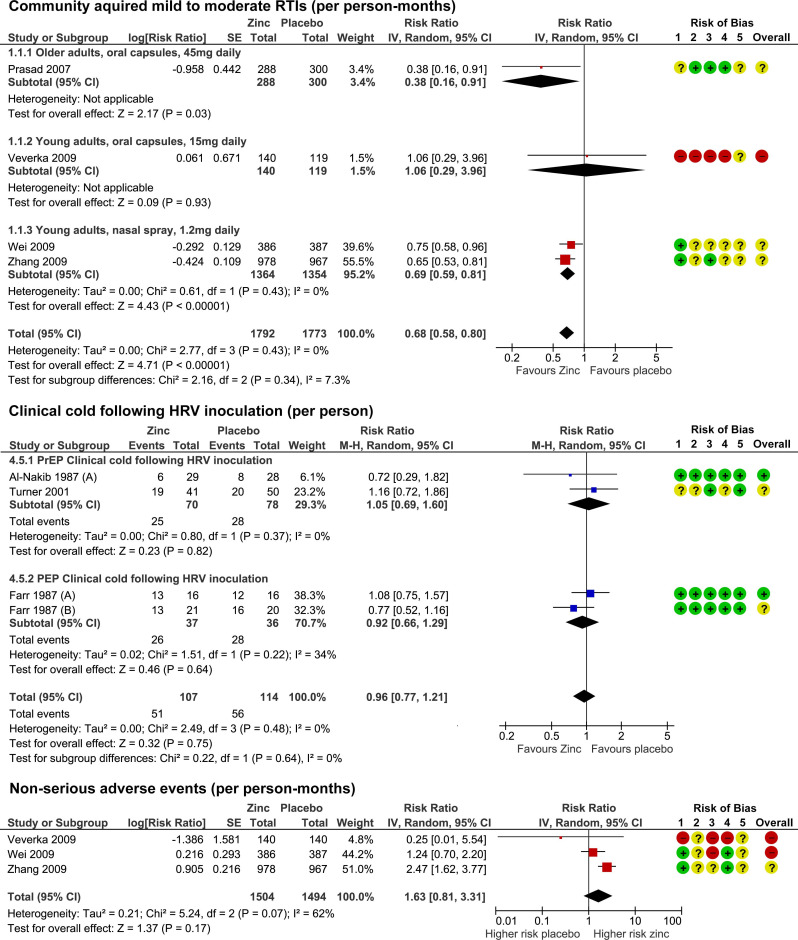
Zinc has been in the limelight recently. The reason is that it has been recommended as a preventative and/or treatment of COVID infections. The basis for such recommendations has been some trial evidence suggesting it is effective for viral respiratory tract infections (RTIs). But the evidence has been full of contradictions which means, we need a systematic review that critically evaluated the totality of the available data.
This systematic review was aimed at evaluating the benefits and risks of zinc formulations compared with controls for the prevention or treatment of acute RTIs in adults.
Seventeen English and Chinese databases were searched in April/May 2020 for randomized clinical trials (RCTs), and from April/May 2020 to August 2020 for SARS-CoV-2 RCTs. Cochrane rapid review methods were applied. Quality appraisals used the Risk of Bias 2.0 and Grading of Recommendations, Assessment, Development and Evaluation (GRADE) approach.
Twenty-eight RCTs with 5446 participants were identified. None were specific to SARS-CoV-2. Compared with placebo, oral or intranasal zinc prevented 5 RTIs per 100 person-months (95% CI 1 to 8, numbers needed to treat (NNT)=20, moderate-certainty/quality). Sublingual zinc did not prevent clinical colds following human rhinovirus inoculations (relative risk, RR 0.96, 95% CI 0.77 to 1.21, moderate-certainty/quality). On average, symptoms resolved 2 days earlier with sublingual or intranasal zinc compared with placebo (95% CI 0.61 to 3.50, very low-certainty/quality) and 19 more adults per 100 were likely to remain symptomatic on day 7 without zinc (95% CI 2 to 38, NNT=5, low-certainty/quality). There were clinically significant reductions in day 3 symptom severity scores (mean difference, MD -1.20 points, 95% CI -0.66 to -1.74, low-certainty/quality), but not average daily symptom severity scores (standardised MD -0.15, 95% CI -0.43 to 0.13, low-certainty/quality). Non-serious adverse events (AEs) (eg, nausea, mouth/nasal irritation) were higher (RR 1.41, 95% CI 1.17 to 1.69, NNHarm=7, moderate-certainty/quality). Compared with active controls, there were no differences in illness duration or AEs (low-certainty/quality). No serious AEs were reported in the 25 RCTs that monitored them (low-certainty/quality).
The authors concluded that in adult populations unlikely to be zinc deficient, there was some evidence suggesting zinc might prevent RTIs symptoms and shorten duration. Non-serious AEs may limit tolerability for some. The comparative efficacy/effectiveness of different zinc formulations and doses were unclear. The GRADE-certainty/quality of the evidence was limited by a high risk of bias, small sample sizes and/or heterogeneity. Further research, including SARS-CoV-2 clinical trials is warranted.
The authors provide a short comment on the assumed mode of action of zinc. The rationale for topical intranasal and sublingual zinc is based on the in vitro effects of zinc ions that can inhibit viral replication, stabilize cell membranes and reduce mucosal inflammation. Other conceivable mechanisms include the activation of T lymphocytes, monocytes, and granulocytes.
The authors also remind us to be cautious: clinicians and consumers need to be aware that considerable uncertainty remains regarding the clinical efficacy of different zinc formulations, doses, and administration routes, and the extent to which efficacy might be influenced by the ever changing epidemiology of the viruses that cause RTIs. The largest body of evidence comes from sublingual lozenges and zinc gluconate and acetate salts, suggesting these are suitable choices. Yet, this does not mean that other administration routes and zinc salts are less effective. The new evidence on the prophylactic effects of low-dose nasal sprays adds weight to the otherwise inconclusive findings from the handful of RCTs evaluating zinc nasal sprays or gels for acute treatment. A minimum therapeutic dose for zinc is also yet to be determined. An earlier review suggested the minimum dose for sublingual lozenges is 75 mg. However, the present analysis does not support this conclusion. Furthermore, a daily oral dose of 15 mg has been shown to upregulate lymphocytes within days, so it is plausible that much lower doses might also be effective.
The ‘My Resilience in Adolescence (MYRIAD) Trial’evaluated the effectiveness and cost-effectiveness of SBMT compared with teaching-as-usual (TAU).
MYRIAD was a parallel group, cluster-randomised controlled trial. Eighty-five eligible schools consented and were randomized 1:1 to TAU (43 schools, 4232 students) or SBMT (42 schools, 4144 students), stratified by school size, quality, type, deprivation, and region. Schools and students (mean (SD); age range=12.2 (0.6); 11–14 years) were broadly UK population-representative. Forty-three schools (n=3678 pupils; 86.9%) delivering SBMT, and 41 schools (n=3572; 86.2%) delivering TAU, provided primary end-point data. SBMT comprised 10 lessons of psychoeducation and mindfulness practices. TAU comprised standard social-emotional teaching. Participant-level risk for depression, social-emotional-behavioural functioning and well-being at 1 year follow-up were the co-primary outcomes. Secondary and economic outcomes were included.
 An analysis of the data from 84 schools (n=8376 participants) found no evidence that SBMT was superior to TAU at 1 year. Standardised mean differences (intervention minus control) were: 0.005 (95% CI −0.05 to 0.06) for risk for depression; 0.02 (−0.02 to 0.07) for social-emotional-behavioural functioning; and 0.02 (−0.03 to 0.07) for well-being. SBMT had a high probability of cost-effectiveness (83%) at a willingness-to-pay threshold of £20 000 per quality-adjusted life year. No intervention-related adverse events were observed.
An analysis of the data from 84 schools (n=8376 participants) found no evidence that SBMT was superior to TAU at 1 year. Standardised mean differences (intervention minus control) were: 0.005 (95% CI −0.05 to 0.06) for risk for depression; 0.02 (−0.02 to 0.07) for social-emotional-behavioural functioning; and 0.02 (−0.03 to 0.07) for well-being. SBMT had a high probability of cost-effectiveness (83%) at a willingness-to-pay threshold of £20 000 per quality-adjusted life year. No intervention-related adverse events were observed.
The authors concluded that the findings do not support the superiority of SBMT over TAU in promoting mental health in adolescence.
Even though the results are negative, MYRIAD must be praised for its scale and rigor, and for highlighting the importance of large, well-designed studies before implementing measures of this kind on a population basis. Co-author Tim Dalgliesh, director of the Cambridge Centre for Affective Disorders, said: “For policymakers, it’s not just about coming up with a great intervention to teach young people skills to deal with their stress. You also have to think about where that stress is coming from in the first place.”
“There had been some hope for an easy solution, especially for those who might develop depression,” says Til Wykes, head of the School of Mental Health and Psychological Sciences at the Institute of Psychiatry, Psychology, and Neuroscience, King’s College London. “There may be lots of reasons for developing depression, and these are probably not helped by mindfulness,” she says. “We need more research on other potential factors that might be modified, and perhaps this would provide a more targeted solution to this problem.”
Personally, I feel that mindfulness has been hyped in recent years. Much of the research that seemed to support it was less than rigorous. What is now needed is a realistic approach based on sound evidence and critical thinking.
Novak Djokovic not only is against getting COVID vaccinations, he is also deeply into so-called alternative medicine (SCAM). Many of us have seen him winning this year’s Wimbledon final and drinking from a mysterious white bottle during Wimbledon 2022. Consequently, people are wondering: what does the white bottle contain?
‘Magic potion, that is all I can say,’ Djokovic said about the contents of the bottle ahead of the Wimbledon final after a clip went viral on Twitter. Now The Telegraph is suggesting that the ‘magic potion’ is, in fact, merely isotonic powder.
This, of course, begs the question: what is isotonic powder?
It is the powder used for making an isotonic drink that typically contains 40-80g of carbohydrate per liter. The drink then has the same osmolarity as body fluids and is therefore the most effective way to rehydrate during and following exercise. There are plenty of such products for sale. They are designed to provide the carbs and electrolytes needed to fuel exercise and replace the salts lost during sweating and maintain hydration.
It is suggested that Djokovic and some other tennis players take the powder pure without dissolving it in water. This must be jolly unpleasant, and I would not recommend it. If you want to save money, you can make an isotonic drink yourself:
- take 200ml of pineapple or other fruit juice,
- add it to 400ml of water,
- add a pinch of salt.
The pinch of salt might also come in handy if, one day, we hear that the powder Djokovic takes also contains this or that SCAM such as “peptides with specific functionality” developed by the pharmaceutical firm that Djokovic partly owns.
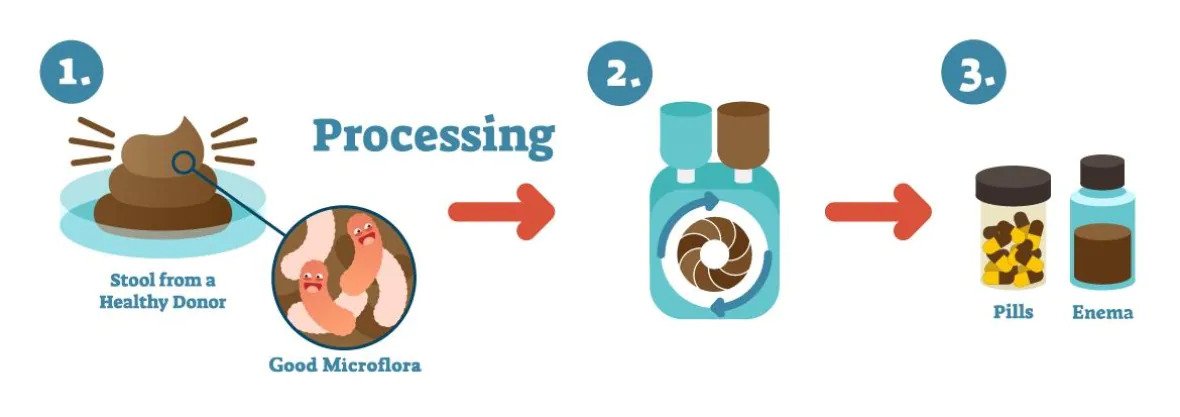
I have previously reported that a Canadian naturopath, Jason Klop, is under investigation for selling fecal Microbiota transplants to treat autistic children. Now, there is a new twist in this story.
On Twitter, J.N. Stea summarized it nicely:
This naturopath is fighting a judge so that he can charge parents about $15,000 to give his nephew’s poop to children as a treatment for autism. His lawyer argues that he should be allowed to since naturopathy isn’t scientific anyway.
Klop’s lawyer defends the naturopath against an investigation into his business of selling fecal microbiota transplants to families of autistic children. The College of Naturopathic Physicians (CoN) had banned Klop for selling, advertising, and manufacturing pills made from human feces claiming that Klop has been engaging in conduct not acceptable for a naturopathic physician. Klop’s lawyer, Jason Gratl, argued this was difficult to prove in a field that has a few restrictions and some ambiguous boundaries.
“What does it take to be a naturopath and do something that is not appropriate in a field so wide-ranging and open to interpretation?” the lawyer, Gratl, asked the court suggesting that the lack of scientific evidence supporting the use of fecal Microbiota Transplants (FMT) to treat autism is not necessarily relevant in this instance.
“Naturopaths can rely on science in certain aspects, but they are not bound to science,” Gratl said. He explained that naturopathic practices could be based on anecdotes and historical knowledge. Later, he pointed out that the field also includes homeopathy, which, some believe, involves magical thinking. It is definitely not scientific in its core.” After describing the case as a “tragedy”, Gratl called the allegations against his client “entirely unverfounded and scurrilous.”
I suspect it is nothing new to most readers, yet I find it gratifying to hear from a lawyer that naturopathy
- is not science,
- relies on anecdote instead of evidence,
- and involves magical thinking.
I do think, however, that despite all this, naturopaths should not be allowed to do any odd nonsense that comes to their minds and fills their bank accounts quickly.
A study by an international team of researchers estimated the proportion of healthcare interventions tested within Cochrane Reviews that are effective according to high-quality evidence.
They selected a random sample of 2428 (35%) of all Cochrane Reviews published between 1 January 2008 and 5 March 2021 and extracted data about interventions within these reviews that were compared with placebo, or no treatment, and whose outcome quality was rated using Grading of Recommendations Assessment, Development and Evaluation (GRADE). They then calculated the proportion of interventions whose effectiveness was based on high-quality evidence according to GRADE, had statistically significant positive effects and were judged as beneficial by the review authors. They also calculated the proportion of interventions that suggested harm.
Of 1567 eligible interventions, 87 (5.6%) had high-quality evidence on first-listed primary outcomes, positive, statistically significant results, and were rated by review authors as beneficial. Harms were measured for 577 (36.8%) interventions, 127 of which (8.1%) had statistically significant evidence of harm. Our dependence on the reliability of Cochrane author assessments (including their GRADE assessments) was a potential limitation of our study. 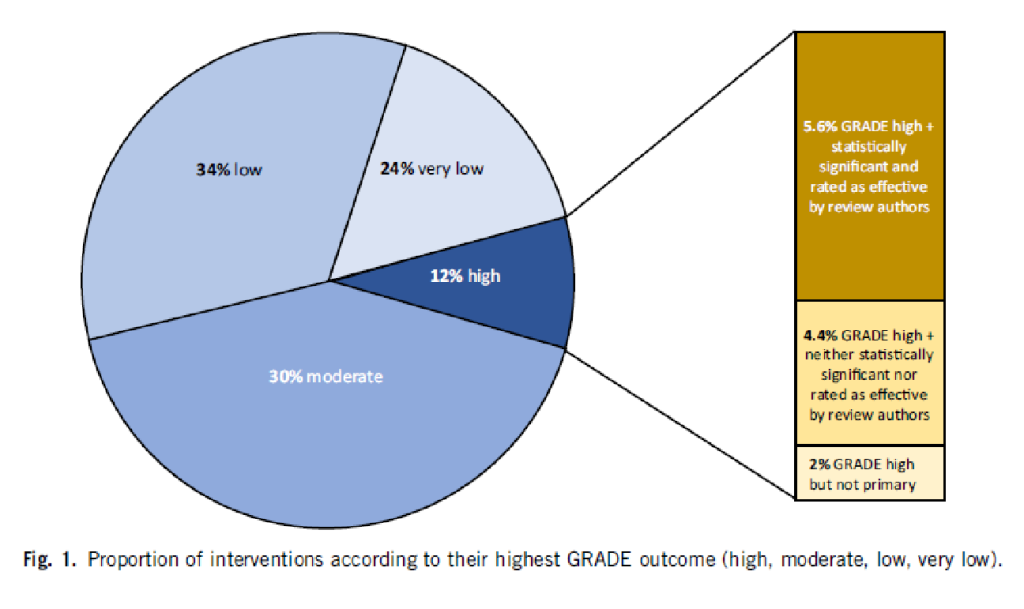
The authors drew the following conclusions: While many healthcare interventions may be beneficial, very few have high-quality evidence to support their effectiveness and safety. This problem can be remedied by high-quality studies in priority areas. These studies should measure harms more frequently and more rigorously. Practitioners and the public should be aware that many frequently used interventions are not supported by high-quality evidence.
Proponents of so-called alternative medicine (SCAM) are fond of the ‘strawman’ fallacy; meaning they like to present a picture of conventional medicine that is overtly negative in order for SCAM to appear more convincing (Prince Charles, for instance, uses this trick every single time he speaks about SCAM). Therefore I am amazed that this paper has not been exploited in that way by them. I was expecting headlines such as
Evidence-based medicine is not supported by evidence
or
Less than 6% of all conventional treatments are supported by sound evidence.
etc.
Why did they not have a field day with this new paper then?
As the article is behind a paywall, it took me a while to get the full paper (thanks Paul). Now that I have read it, I think I understand the reason.
In the article, the authors provide figures for specific types of treatments. Let me show you some of the percentages of interventions that met the primary outcome (high quality, statistically significant effect, and authors interpret as effective):
- pharmacological 73.8%
- surgical 4.6%
- exercise 5.8%
- diet 1.2%
- alternative 0.0%
- manual therapies 0.0%
So, maybe the headlines should not be any of the above but:
No good evidence to support SCAM?
or
SCAM is destroying the evidence base of medicine.
If you have been following my blog for a while, you probably know the answer to this question. A recent article published in JAMA re-emphasizes it in an exemplary fashion:
According to National Health and Nutrition Examination Survey data, 52% of surveyed US adults reported using at least 1 dietary supplement in the prior 30 days and 31% reported using a multivitamin-mineral supplement. The most commonly cited reason for using supplements is for overall health and wellness and to fill nutrient gaps in the diet. Cardiovascular disease and cancer are the 2 leading causes of death and combined account for approximately half of all deaths in the US annually. Inflammation and oxidative stress have been shown to have a role in both cardiovascular disease and cancer, and dietary supplements may have anti-inflammatory and antioxidative effects.
Objective To update its 2014 recommendation, the US Preventive Services Task Force (USPSTF) commissioned a review of the evidence on the efficacy of supplementation with single nutrients, functionally related nutrient pairs, or multivitamins for reducing the risk of cardiovascular disease, cancer, and mortality in the general adult population, as well as the harms of supplementation.
Population Community-dwelling, nonpregnant adults.
Evidence Assessment The USPSTF concludes with moderate certainty that the harms of beta carotene supplementation outweigh the benefits for the prevention of cardiovascular disease or cancer. The USPSTF also concludes with moderate certainty that there is no net benefit of supplementation with vitamin E for the prevention of cardiovascular disease or cancer. The USPSTF concludes that the evidence is insufficient to determine the balance of benefits and harms of supplementation with multivitamins for the prevention of cardiovascular disease or cancer. Evidence is lacking and the balance of benefits and harms cannot be determined. The USPSTF concludes that the evidence is insufficient to determine the balance of benefits and harms of supplementation with single or paired nutrients (other than beta carotene and vitamin E) for the prevention of cardiovascular disease or cancer. Evidence is lacking and the balance of benefits and harms cannot be determined.
Recommendation The USPSTF recommends against the use of beta carotene or vitamin E supplements for the prevention of cardiovascular disease or cancer. (D recommendation) The USPSTF concludes that the current evidence is insufficient to assess the balance of benefits and harms of the use of multivitamin supplements for the prevention of cardiovascular disease or cancer. (I statement) The USPSTF concludes that the current evidence is insufficient to assess the balance of benefits and harms of the use of single- or paired-nutrient supplements (other than beta carotene and vitamin E) for the prevention of cardiovascular disease or cancer. (I statement)
The report also elaborates on potential harms:
For many of the vitamins and nutrients reviewed, there was little evidence of serious harms. However, an important harm of increased lung cancer incidence was reported with the use of beta carotene by persons who smoke tobacco or have occupational exposure to asbestos.
Excessive doses of vitamin supplements can cause several known adverse effects; for example, moderate doses of vitamin A supplements may reduce bone mineral density, and high doses may be hepatotoxic or teratogenic. Vitamin D has potential harms, such as a risk of hypercalcemia and kidney stones, when given at high doses. The potential for harm from other supplements at high doses should be carefully considered.
There is nothing new here, of course. I (and others) have been trying to get these points across for many years. But it is nevertheless most gratifying to see the message repeated by a top journal such as JAMA. I hope JAMA is more successful than I was in changing the behavior of the often all too gullible public!