critical thinking
In Germany, the anti-vax movement is frighteningly strong and it constitutes one of the main reasons for the relatively immunization rate. In no small part, this is due to the many anti-vax Heilpraktiker who practice in Germany. In an attempt to put the record straight, the ‘Verband Klassischer Homöopathen Deutschlands’ (VKHD, Association of Classical Homeopaths of Germany) recently published an article entitled ‘Heilpraktiker – Homeopathy – Vaccination’ (Heilpraktiker – Homöopathie – Impfen). Here is a short excerpt (my translation):
… There is a clear conceptual similarity between homeopathy and vaccination [1]. From a historical point of view, this was already reflected in the early days of homeopathy, when its discoverer, Samuel Hahnemann, expressed himself very positively with regard to the smallpox vaccination newly introduced at that time [2]. Thus, it is historically wrong to insinuate that users of homeopathy have a fundamentally negative attitude towards vaccinations [3]. In this context, terms such as “vaccination opponents” or “vaccination refusers” are misleading and defamatory [4].
A critical (not skeptical) approach to the topic of vaccinations is basically a characteristic of people with medical expertise. Such an attitude corresponds to the critical consideration necessary in daily practice and in each individual case to advise on suitable therapy options [5]. Properly working alternative practitioners give differentiated advice accordingly [6]. A fundamentally vaccine-rejecting attitude is precisely not a characteristic of a critical assessment that has taken place. The same applies to an unreflective recommendation of vaccinations or therapy methods, without taking into account individual factors as well as scientific and social backgrounds [7].
For the VKHD, we cannot give exact figures on recovered, vaccinated, or unvaccinated members. It is not the responsibility of a professional association to demand such information from its members [8]. We assume that alternative practitioners who provide information on vaccinations do so in accordance with a responsible ethical attitude, regardless of their own vaccination status [9] …
I have taken the liberty of inserting some references into this text. They relate to my comments, which are as follows:
- A conceptual similarity between vaccination and homeopathy exists only in the minds of homeopaths. They often claim that both use highly diluted remedies. This is wrong because homeopathic remedies do not usually contain active ingredients, whereas vaccines do. This fact also explains why homeopathics do not produce immune reactions, whereas vaccines do.
- Correct! Hahnemann was in favor of vaccination. That is why he would be ashamed today if he knew how many homeopaths oppose vaccination.
- What has this got to do with ‘historical’? I assume that the ‘insinuations’ refer to the situation today. Further, I don’t think anyone is suggesting that all homeopaths are ‘fundamentally’ opposed to vaccination. However, that many of them are anti-vaxers is an indisputable fact.
- I would rather think they are accurate.
- Correct.
- How can they without any medical background?
- Is it to be implied here that real medical people do?
- Maybe not ‘demand’, but inquire or request would be possible and desirable, wouldn’t it?
- It is nice that you believe this. But belief is not evidence.
Osteopathic manipulative treatment (OMT) is advocated not merely for spinal or musculoskeletal problems, as many consumers seem to think, osteopaths also claim it to be effective for (almost) every condition. Some osteopaths who believe in the gospel of Andrew Still, the founder of osteopathy, recommend it even to facilitate breastfeeding.
But is it effective?
A double-blind randomised controlled trial to answer this question was conducted between July 2013 and March 2016. Breastfed term infants were eligible if one of the following criteria was met: suboptimal breastfeeding behaviour, maternal cracked nipples or maternal pain. The infants were randomly assigned to the intervention or the control group. The intervention consisted of two sessions of early OMT, while in the control group, the manipulations were performed on a doll behind a screen. The primary outcome was the exclusive breastfeeding rate at 1 month, which was assessed in an intention-to-treat analysis. Randomisation was computer generated and only accessible to the osteopath practitioner. The parents, research assistants and paediatricians were masked to group assignment.
One hundred twenty-eight mother-infant dyads were randomised, with 64 assigned to each group. In each group, five infants were lost to follow-up. In the intervention group, 31 of 59 (53%) of infants were still exclusively breastfed at 1 month vs 39 of 59 (66%) in the control group, (OR 0.55, 95% CI 0.26 to 1.17; p=0.12). After adjustment for suboptimal breastfeeding behaviour, caesarean section, use of supplements and breast shields, the adjusted OR was 0.44 (95% CI 0.17 to 1.11; p=0.08). No adverse effects were reported in either group.
The authors concluded succinctly that OMT did not improve exclusive breastfeeding at 1 month.
Surprised?
Suppose not!
The only question that I can think of is this: why did osteopaths ever think that OMT might facilitate breastfeeding?
Aromatherapy, the use of essential oils for medicinal purposes, exists in several guises. One of them is inhalation aromatherapy which is a complementary therapy used in different clinical settings. But is there any sound evidence about its effectiveness?
The aim of this review was to assess the effectiveness of inhalational aromatherapy in the care of hospitalized pediatric patients.
A systematic review of clinical trials and quasi-experimental studies was conducted, based on PRISMA recommendations, searching Medline, Web of Science, Scopus, SciELO, LILACS, CINAHL, Science Direct, EBSCO, and updated databases. The Down and Black 2020, RoB 2020 CLARITY, and ROBINS-I 2020 scales were used through the Distiller SR software to verify the studies’ internal validity and risk of bias.
From 446 articles identified, 9 fulfilled the inclusion criteria. Seven were randomized controlled trials (RCTs), one pilot RCT, and one non-randomized quasi-experimental trial.
Different outcomes were analyzed, with pain being the most frequently measured variable. None of the 6 studies that evaluated pain showed significant effects with inhalation aromatherapy. Additionally, non-significant effects were found regarding nausea, vomiting, and behavioral/emotional variables.
The authors concluded that the findings are still inconclusive, and more evidence is required from future studies with high methodological quality, blinding, and adequate sample sizes.
Inconclusive?
Really?
Call me a skeptic, but I think the findings show quite clearly that there is no sound evidence to suggest that inhalation aromatherapy might be effective for kids.
This study assessed the effectiveness of Oscillococcinum in the protection from upper respiratory tract infections (URTIs) in patients with COPD who had been vaccinated against influenza infection over the 2018-2019 winter season.
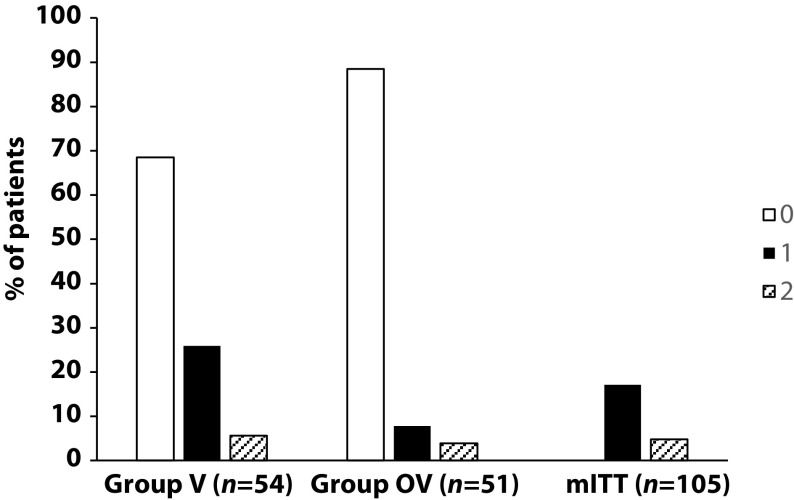
A total of 106 patients were randomized into two groups:
- group V received influenza vaccination only
- group OV received influenza vaccination plus Oscillococcinum® (one oral dose per week from inclusion in the study until the end of follow-up, with a maximum of 6 months follow-up over the winter season).
The primary endpoint was the incidence rate of URTIs (number of URTIs/1000 patient-treatment exposure days) during follow-up compared between the two groups.
There was no significant difference in any of the demographic characteristics, baseline COPD, or clinical data between the two treatment groups (OV and V). The URTI incidence rate was significantly higher in group V than in group OV (2.9 versus 1.2 episodes/1000 treatment days, difference OV-V = -1.7; p=0.0312). There was a significant delay in occurrence of an URTI episode in the OV group versus the V group (mean ± standard error: 48.7 ± 3.0 versus 67.0 ± 2.8 days, respectively; p=0.0158). Limitations to this study include its small population size and the self-recording by patients of the number and duration of URTIs and exacerbations.
The authors concluded that the use of Oscillococcinum in patients with COPD led to a significant decrease in incidence and a delay in the appearance of URTI symptoms during the influenza-exposure period. The results of this study confirm the impact of this homeopathic medication on URTIs in patients with COPD.
Primary endpoint, comparison of the number of upper respiratory tract infections in the two treatment groups during follow-up
This prospective, randomized, single-center study was funded by Laboratoires Boiron, was conducted in the Pneumology Department of Charles Nicolle Hospital, Tunis, and was written up by a commercial firm specializing in writing for the pharmaceutical industry. The latter point may explain why it reads well and elegantly glosses over the many flaws of the trial.
If I did not know better, I might suspect that the study was designed to deceive us (Boiron would, of course, never do this!): The primary endpoint was the incidence rate of URTIs (number of URTIs/1000 patient-treatment exposure days) in the two groups during the follow-up period. This rate is calculated as the number of episodes of URTIs per 1000 days of follow-up/treatment exposure. The rates were then compared between the OV and V groups. The following symptoms were considered indicative of an URTI: fever, shivering, runny or blocked nose, sneezing, muscular aches/pain, sore throat, watery eyes, headaches, nausea/vomiting, diarrhoea, fatigue and loss of appetite.
This means that there was no verification whatsoever of the primary endpoint. In itself, this flaw would perhaps not be so bad. But put it together with the fact that patients were not blinded (there were no placebos!), it certainly is fatal.
In essence, the study shows that patients who perceive to receive treatment will also perceive to have fewer URTIs.
SURPRISE, SURPRISE!
The Corona Committee (Corona Ausschuss) was founded in Berlin in July 2020 by the lawyers Viviane Fischer, Antonia Fischer, Dr. Reiner Füllmich, and Dr. Justus Hoffmann. Its aim is to provide a “factual analysis” of the coronavirus events and the consequences of the measures taken against them. In live sessions lasting several hours, the committee hears experts from all COVID-affected fields.
In an interview, Dr. Fuellmich said: “The decision to set up a Corona Inquiry Committee came about in the first telephone conversation Viviane Fischer and I ever had. After I had spoken out in the USA via various videos since April 2020 about the fact that the principle ‘audiatur et altera pars’ (hear the other side as well) had been blatantly violated here on the part of the government, I had come back to Germany from the USA because I felt that this was now my place and that I had to stand up here to ensure that our democracy and our constitutional state did not go completely to the dogs. I wanted to organize a symposium on the legal issues surrounding Corona, but I didn’t know any critical lawyers in Germany. I called my old friend Dr. Wolfgang Wodarg, whom I knew from the Justice Working Group at Transparency International, and he then referred me to Viviane Fischer.”
The ‘Speerspitze‘, an “anonymous collective of contrarians, Corona deniers, Nazi witches and conspiracy heretics” considers the work of the Corona Committee to be “one of the most important pillars of the fight against the madness to which we have been subjected for the last year and a half and [has] great respect for all the activists, actors, and interviewees of the Committee who publicly denounce with their name and face what is happening.” Numerous further websites have joined in the promotion of the Corona Committee.
However, if you look at the information that the Corona Committee is disseminating, and if you are able to think critically, you are likely to come to very different conclusions:
– There is the expert who warns that the unvaccinated could soon be picked up and put into concentration camps. There is the threat of a “manhunt”, and loving parents might then have to hide their children under the boards of the floor at home to prevent them from being sprayed to death.
– There is the man who claims that Israel’s government is currently carrying out a holocaust on its own population (“You can see that by how many people are dying from the vaccinations”). A guest declares that there are “something like living octopuses” in the vaccine against Corona.
Anyone who takes a look at the many tediously long videos will quickly realize that every Corona denier, vaccination opponent, conspiracy theorist, mask opponent, and lateral thinker, no matter how paranoid, have their say here and spreads their pipe dreams under the guise of evidence-based information with the nodding approval of the lawyers present. Opposition is never raised and there is no trace of ‘audiatur et altera pars’; everyone agrees: worldwide, all governments are hell-bound at smashing everything there is to govern.
For those who are still not fed up, the website of the Corona Committee offers written answers to 31 very specific questions. Here is just one.
QUESTION: IS THE COVID-19 DISEASE SEVERE AND WIDESPREAD?
ANSWER: No, most people have no or only mild flu symptoms. Children and adolescents are extremely rarely affected. Post-mortem examinations by a Hamburg forensic pathologist on over 100 elderly people who died with a positive corona test revealed at least one other serious cause of death in all cases. Other published figures are mostly based on non-transparent attributions and assumptions without excluding other causes. Often, no attention was even paid to other pathogens or previous medication.
Factual analyses?
Afraid not!
For a long time, I have been wondering where the penetratingly vociferous opposition to COVID vaccinations in Germany might come from. After studying the dangerous nonsense that the Corona Committee has been spreading for many months, I wonder a little less.
(texts in German were translated by me)
Conversion therapy has been banned last week in Canada. These therapies – also known as sexual orientation change effort (SOCE), reparative therapy, reintegrative therapy, reorientation therapy, ex-gay therapy, and gay cure – rely on the assumption that sexual orientation can be changed, an idea long discredited by major medical associations in the US, the UK, France, and elsewhere. The new law makes “providing, promoting, or advertising conversion therapy” a criminal offense. It will also be an offense to profit from the provision of conversion therapy. In addition, the bill states a person cannot remove a “child from Canada with the intention that the child undergo conversion therapy outside Canada.” Prime Minister Justin Trudeau hailed the law’s Royal Assent: “It’s official: Our government’s legislation banning the despicable and degrading practice of conversion therapy has received Royal Assent — meaning it is now law.”
Conversion therapy is the attempt to change an individual’s sexual or gender identity by psychological, medical, or surgical interventions. Often, informed consent is insufficient or lacking. In conventional medicine, numerous treatments have been tried for this purpose, some of them dangerous and all of them ineffective. In alternative medicine, approaches that have been advocated include:
- Homeopathy (see below),
- Hypnotherapy,
- Spiritual healing,
- Prayer,
- Eye Movement Desensitization,
- Rebirthing,
- and others.
- Faith-based organizations or leaders
- Licensed healthcare professionals
- Unlicensed healthcare professionals
As previously reported, the German ‘Association of Catholic Doctors’ claimed that homeopathic remedies can cure homosexuality. Specifically, they advised that ‘…the working group ‘HOMEOPATHY’ of the Association notes homeopathic therapy options for homosexual tendencies…repertories contain special rubrics pointing to characteristic signs of homosexual behavior, including sexual peculiarities such as anal intercourse. And a homeopathic remedy called ‘Dr. Reckeweg R20 Glandular Drops for Women’ was claimed to treat “lesbian tendencies.” The product is “derived and potentised from fetal tissues.”
Several countries are now in the process of banning conversion therapy. France has already banned it and so has Germany. The UK government intends to introduce a legislative ban on the practice of conversion therapy. The consultation on how to best do this is open until 4 February 2022.
On Dec. 1, the College of Chiropractors of B.C. (BCCA) held its AGM and registrants voted in favour of a non-binding resolution calling for the regulator to “take a stand” against an expected vaccine mandate for health professionals. Subsequently, Health Minister Adrian Dix then “expressed his extreme displeasure” about the remarks of some chiropractors.
“Minister Dix indicated it was an embarrassment that a health profession would in such resounding numbers … support such unfounded and false claims while people are dying from COVID-19,” said the BCCA’s executive director Angie Knott. In bold and underlined text, she added, “He also stated that it made him question the validity of self-regulation.”
During the meeting in question, 78% of those chiropractors in attendance had voted in favour of the motion. Chiropractors are not trained in treating or preventing infectious disease and are prohibited from offering advice on vaccinations in B.C.
This is not the first time health ministry officials have expressed concerns about the ability of chiropractors to adequately regulate themselves.
- In 2018, CBC reported on an anti-vaccination video that had been created and shared by the college’s then-vice chair Avtar Jassal, in violation of college policy and despite complaints from a member of the public.
- A Freedom of Information request to the ministry later showed that the day after the story was published, the ministry’s director of regulatory initiatives wrote an email saying he was asked to outline “what options we have when a college is not meeting its legal obligation as set out under the HPA [Health Professions Act].”
- Vancouver chiropractor resigns from college board over anti-vaccine video
Even the proper regulation of quackery will merely result in quackery!
Lian gong (LG), also called Lian Gong Shi Ba Fa, is a form of so-called alternative medicine (SCAM) from China. More specifically, it is a set of stretching, breathing exercises, and self-massaging techniques aimed at preventing and relieving stress as well as acute pains around the neck, shoulders, back, hips, legs, joints, and connective tissues. Even though it is relatively new, it is based on old Chinese stretching, breathing, and warm-up exercises dating back more than 1,000 years, including the Eight Silk Brocade (八段錦). Lian gong has spread rapidly from China to other countries, especially to Japan and Brazil.
Lian Gong was developed by Dr. Zhuang Yuan Ming (1919- ), a traditional Chinese medical doctor, who started conducting a series of clinical trials around 1974 in a Shanghai hospital on patients suffering from a variety of stress-related conditions. Lian Gong is now being promoted as “massage in motion”.
One of the few controlled clinical studies of Liam gong aimed to evaluate the effects of LG on the impact of dizziness on the quality of life and fear of falling in primary health care patients. It was designed as a randomized clinical trial with 36 patients with dizziness not caused by central changes. The participants were randomly assigned to 3 groups:
- the Liam gong (LG) group ( n = 11),
- the vestibular rehabilitation (VR) group ( n = 11),
- the control group ( n = 14).
The treatments were carried out over a period of 12 weeks.
Lian gong reduced the influence of dizziness on the quality of life in physical (1.8 points, 95% confidence interval [CI]: 0.2-3.4), functional (4.0 points, 95% CI: 2.1-5.9), and emotional domains of quality of life (4.4 points, 95% CI: 1.7-7.2), with no differences, compared with VR.
The authors concluded that Lian gong was shown to be an effective balance rehabilitation strategy to reduce the impact of dizziness on quality of life, with similar results to those of VR.
Unfortunately, this study has many flaws – not least its minute sample size. Therefore, the conclusions seem more than a little over-optimistic. I would not be all that surprised to learn that these exercises can have beneficial effects for a range of conditions. What seems doubtful in my view, however, is whether it is superior to more conventional exercise therapies.
Yesterday, it was announced that the new German health secretary will be Dr. Karl Lauterbach. This seems a most reasonable choice (when did the UK last have a physician in that post?), and I certainly wish him the best of luck in his new position.
Lauterbach studied medicine at the RWTH Aachen University, University of Texas at San Antonio and University of Düsseldorf, where he graduated. From 1989 to 1992, he studied health policy and management as well as epidemiology at the Harvard School of Public Health in Boston, graduating with a Doctor of Science in 1992. From 1992 to 1993, he held a fellowship at the Harvard Medical School.
From 1998 until 2005, Lauterbach served as the director of the Institute of Health Economics and Clinical Epidemiology (IGKE) at the University of Cologne. He was appointed adjunct professor at the Harvard School of Public Health in 2008. He was a member of the Sachverständigenrat zur Begutachtung der Entwicklung im Gesundheitswesen (the council of experts advising the federal government on developments in the German healthcare system) from 1999 until he was elected to the Bundestag in September 2005.
But why does his appointment put the German defenders of homeopathy in a panic? The reason is simple: Lauterbach has in the past repeatedly argued against the reimbursement of homeopathy in Germany. This is, for instance, what DER SPIEGEL wrote in 2019 (my translation):
SPD parliamentary group vice-chairman Karl Lauterbach wants to prohibit public health insurance companies from reimbursing the costs of homeopathy. “We have to talk about this in the coalition,” he told the “Tagesspiegel”. Health insurance companies in Germany are not obliged to cover the costs of homeopathic treatments. However, they can pay for it voluntarily.
Voluntary benefits by health insurers must also be economically and medically reasonable, Lauterbach argues, referring to a similar push in France. According to the French Supreme Health Authority (HAS), the funds do not have sufficient scientific effect. The Ministry of Health had previously commissioned the HAS with the examination. It is considered likely that the French government will soon abolish the coverage of costs.
“In the spirit of reason and education as well as patient protection, it is also wrong in Germany for insurance companies to pay for homeopathy for marketing reasons,” Lauterbach wrote on Twitter in reaction to the decision in France. His demand is not new. Lauterbach had already spoken out in 2010 for a ban on the assumption of costs.
Many observers expect that Lauterbach – after getting the pandemic under control (not an easy task by any measure) – will indeed stop the reimbursement of homeopathy. Germany’s largest homeopathy producer reacted swiftly and is currently running an expensive campaign with full-page advertisements in German newspapers trying to improve the much-damaged public image of homeopathy:
In the advertisement above, for instance, it is implied that homeopaths are all in favor of vaccination. Regular readers of my blog will know that this is not true…
… and so does Dr. Lauterbach!
In 2013, Zuckerman et al. conducted a meta-analysis of 63 studies that showed a negative intelligence-religiosity relation (IRR). Now a new meta-analysis with an updated data set of 83 studies has re-addressed the issue.
The new analysis showed that the correlation between intelligence and religious beliefs in college and non-college samples ranged from -.20 to -.23. There was no support for mediation of the IRR by education but there was support for partial mediation by analytic cognitive style.
In 2012, Canadian scientists tested the hypothesis that an analytic cognitive style is associated with a history of questioning, altering, and rejecting (i.e., unbelieving) supernatural claims, both religious and paranormal. In two studies, they examined associations of God beliefs, religious engagement (attendance at religious services, praying, etc.), conventional religious beliefs (heaven, miracles, etc.), and paranormal beliefs (extrasensory perception, levitation, etc.) with performance measures of cognitive ability and analytic cognitive style. An analytic cognitive style negatively predicted both religious and paranormal beliefs when controlling for cognitive ability as well as religious engagement, sex, age, political ideology, and education. Participants more willing to engage in analytic reasoning were less likely to endorse supernatural beliefs. Further, an association between analytic cognitive style and religious engagement was mediated by religious beliefs, suggesting that an analytic cognitive style negatively affects religious engagement via lower acceptance of conventional religious beliefs.
Some time ago, I reported about a study concluding that a higher religiousness/spirituality is associated with a more frequent use of supplements or additional therapies in individuals with endocrinopathies or metabolic diseases. As so-called alternative medicine (SCAM) has been shown to be associated with worse outcome, addressing religiousness/spirituality which stresses the responsibility of the person for his life might offer an additional resource and should be further studied.
On this blog, we have discussed many times, that advocacy of SCAM is associated with vaccination hesitancy; see, for instance here, here, and here)
Finally, the findings of a recent study suggest that beliefs in an engaged God were associated with greater mistrust in the COVID-19 vaccine. This association was amplified for Hispanic and lower-educated Americans. The authors argued that beliefs in an engaged God may promote distrust of science, reduce motivation to get vaccinated, and derive comfort and strength by placing control over one’s life in the hands of a loving, involved deity.
There are, of course, other factors involved in the complex relationships between intelligence, religiosity, SCAM, and vaccination hesitancy. Yet, it seems clear that such links do exist. I agree that it is well worth investigating them in more detail.