critical thinking
Please take a moment to read this short letter by the ‘LIGA MEDICORUM HOMOEOPATHICA INTERNATIONALIS’:
As you know, the World Health Organization (WHO) is predicting that civilization faces a crisis of antibiotic-resistant diseases that may soon result in as many as 10 million deaths per year while pushing as many as 24 million people into extreme poverty.
We, the undersigned, are duly licensed healthcare professionals practicing homeopathy, with the authority to diagnose and treat disease, who have reviewed the extensive research literature demonstrating the clear therapeutic value of homeopathy. Each of us has had extensive clinical experience successfully treating hundreds of thousands of patients suffering from infectious diseases worldwide.
Homeopathy works, does not cause further antibiotic resistance, is generally devoid of side effects, is inexpensive, and is good for health of the planet.
We are calling upon the WHO to encourage the international medical community to immediately begin training in homeopathy as an adjunctive therapeutic measure to avoid this catastrophic loss of life and would like a meeting with you or your representative to discuss the grave challenge of antibiotic resistance at your earliest convenience.
Thank you for considering this urgent appeal.
________________________
I stated above that this is a letter. In fact, it is more – it is a petition directed to the Director-General of the World Health Organization (WHO), Dr. Tedros Adhanom Ghebreyesus, to immediately begin training physicians in homeopathy as an adjunctive therapeutic measure to combat the looming crisis of antibiotic-resistant diseases.
The Liga Medicorum Homoeopathica Internationalis (LMHI) represents homeopathic physicians in more than 70 countries all over the world. The purposes of the association are the development and securing of homeopathy worldwide and the creation of a link among licensed homeopaths with medical diplomas and societies and persons who are interested in homeopathy. The LMHI is exclusively devoted to non-profit activities serving philanthropic benefits.
The LMHI might ring a bell for regular readers of this blog. A few years ago, I reported that its president advocates curing cancers with homeopathy. And in 2014, I reported that a journey to Liberia of leading homeopaths was co-organized by the LMHI; its purpose was to cure Ebola patients of their disease with homeopathy.
I find all of this seriously worrying – not because I fear that the WHO will now start training physicians across the globe in homeopathy. It is worrying, I feel, because it shows how hopelessly deluded homeopaths are. The fact that clinicians so far detached from reality treat ill and vulnerable patients frightens me.
On this blog and elsewhere, I have heard many strange arguments against COVID-19 vaccinations. I get the impression that most proponents of so-called alternative medicine (SCAM) hold or sympathize with such notions. Here is a list of those arguments that have come up most frequently together with my (very short) comments:
COVID is not dangerous
It’s just a flu and nothing to be really afraid of, they say. Therefore, no good reason exists for getting vaccinated. This, I think, is easily countered by pointing out that to date about 5.5 million people have died of COVID-19. In addition, I fear that the issues of ‘long-COVID’ is omitted in such discussions
It’s only the oldies who die
As an oldie myself, I find this argument quite distasteful. More importantly, it is simply not correct.
Vaccines don’t work
True they do not protect us 100% from the infection. But they very dramatically reduce the likelihood of severe illness or death from COVID-19.
Vaccines are unsafe
We have now administered almost 10 billion vaccinations worldwide. Thus we know a lot about the risks. In absolute terms, there is a vast amount of cases, and it would be very odd otherwise; just think of the rate of nocebo effects that must be expected. However, the risks are mostly minor, and serious ones are very rare. Some anti-vaxxers predicted that, by last September, the vaccinated population would be dead. This did not happen, did it? The fact is that the benefits of these vaccinations hugely outweigh the risks.
Vaccines are a vicious tracking system
Some claim that ‘they‘ use vaccines to be able to trace the vaccinated people. Who are ‘they‘, and why would anyone want to trace me when my credit card, mobile phone, etc. already could do that?
Vaccines are used for population control
‘They‘ want to reduce the world population through deadly vaccines to ~5 billion, some anti-vaxxers say. Again, who are ‘they‘ and would ‘they‘ want to do that? Presumably ‘they‘ need us to pay taxes and buy their goods and services.
There has not been enough research
If those who make this argument would bother to go on Medline and look for COVID-related research, they might see how ill-informed this argument is. Since 2021, more than 200 000 papers on the subject have emerged.
I trust my immune system
This is just daft. I am triple-vaccinated and also hope that I can trust my immune system – this is why I got vaccinated in the first place. Vaccinations rely on the immune system to work.
It’s all about making money
Yes, the pharma industry aims to make money; this is a sad reality. But does that really mean that their products are useless? I don’t see the logic here.
People should have the choice
I am all for it! But if someone’s poor choice endangers my life, I do object. For instance, I expect other people not to smoke in public places, stop at red traffic lights and drive on the correct side of the street.
Most COVID patients in hospitals have been vaccinated
If a large percentage of the population has been vaccinated and the vaccine conveys not 100% protection, it would be most surprising, if it were otherwise.
I have a friend who…
All sorts of anecdotes are in circulation. The thing to remember here is that the plural of anecdote is anecdotes and not evidence.
SCAM works just as well
Of course, that argument had to be expected from SCAM proponents. The best response here is this: SHOW ME THE EVIDENCE! In response SCAM fans have so far only been able to produce ‘studies’ that are unconvincing or outright laughable.
In conclusion, the arguments put forward by anti-vaxxers or vaccination-hesitant people are rubbish. It is time they inform themselves better and consider information that originates from outside their bubble. It is time they realize that their attitude is endangering others.
Like so many other anti-vaxxers, Djokovic is deep into so-called alternative medicine (SCAM).
An article in THE TELEGRAPH explains it quite clearly. Here are a few passages:
Here is an anti-scientific crank hiding in plain sight … [In his book Djokovic explains] how he suffered from recurring physical ailments – allergies, breathing difficulties, blocked sinuses – until he gave up gluten.
Nothing especially weird so far – until he explains how his gluten intolerance was diagnosed. A Serbian nutritionist called Dr Igor Cetojevic asked Djokovic to hold his right arm out at right angles and resist the pressure as he pushed down on it. Then the exercise was repeated, only this time while Djokovic held a slice of bread against his stomach. “I was noticeably weaker,” writes Djokovic, who adds that “kinesiological arm testing [has] long been used as a diagnostic tool by natural healers.” Yes, and mediums have long claimed to speak to the dead …
Here is a man who broke up his visits to Wimbledon with trips to the nearby Buddhapadipa Temple to meditate by a lake. A man who revealed two years ago that he has a “friend” in Melbourne’s Botanical Gardens – “a Brazilian fig tree that I like to climb”. Yes, Djokovic’s jet-setting spiritualism might sound charming in itself. But its side-effect has been credulousness.
Serve To Win [ND’s book] describes a so-called “researcher” taking two glasses of water and directing loving energy towards one, while swearing angrily at the other. “After a few days … [the angry glass] was tinted slightly green … the other glass was still bright and crystal clear”. Harmless, perhaps, if deeply dippy. But then, last year, Djokovic could be found hosting a former estate agent called Chervin Jafarieh on his Instagram Live channel. Jafarieh was selling bottles of Advanced Brain Nutrients at $50 apiece, which – like Djokovic’s resistance to the Covid vaccination – sounded contrary to the interests of public health…
… Djokovic expressed in a 2018 interview with Shortlist magazine. “I believe that it is our mission to reach a higher frequency through self-care by exploring and respecting our own avatar, our body and, by doing that, raising the vibration of the planet.” …
And so we return to the dark side of this whole peculiar tale. Were Djokovic just a journeyman player, his pseudo-scientific beliefs would be no more than a bizarre footnote. As it is, he is a powerful role model, particularly in the Balkans. Thousands of people have probably emulated his stance on vaccines. Some are likely to suffer consequences as a result…
Another article explains:
New York Times tennis reporter Ben Rothenberg tweeted out after the news of Djokovic’s visa rejection that the Serbian had been “wildly anti-science” over the years. 
“Let’s not lose sight of how wildly anti-science Djokovic has publicly been for years,” Rothenberg began. “Here he was last year preaching about how you can change water with emotion.
“Naive, but maybe these real consequences today can be a reality check for his nonsense?”
Former New York Times reporter Steven Greenhouse said it was “sad to see such a brilliant tennis player join the anti-science, pro-poppycock anti-vaxxers”.
Tennis Channel producer David Kane added: “I sort of don’t care whether Australia bungled L’Affaire Novak because of political/media pressure. This is about someone who has been stridently anti-science and never indicated a good faith effort to receive this essentially mandatory vaccine.F around & find out, as they say.”
And a Guardian article provides further information:
His belief in alternative medicine is complemented by his commitment to alternative history. He frequently retreats to Visoko, in the hills of Bosnia and Herzegovina, where he meets up with the businessman Semir Osmanagic – whose claims that there are ancient man-made structures with magical healing powers, refuted by scientists, have turned the hills into a lucrative tourist destination. Djokovic has also expressed his support for the ultranationalist alternative historian Jovan Deretic, whose writings claim, among other things, that numerous European cultures, including ancient Greeks, Celts and Etruscans, are descended from Serbs.
I am quite confident that I play tennis as splendidly as Djokovic understands medicine. Yet, I do not pretend to be able to teach you how to do a perfect ‘top slice’. In contrast, Djokovic loves to take the role of ambassador for SCAM and other weird stuff.
His father stated that “Novak is the Spartacus of the new world who does not tolerate injustice, colonialism and hypocrisy but fights for the equality of all on this planet, regardless of skin color, religious belief and money they have.” Personally, I see this differently: Djokovic is badly affected by proctophasia; he tolerates no end of BS and fights for pseudoscience. And sadly, his views are all too persuasive to gullible consumers – not exactly what we need in a global health crisis!
In so-called alternative medicine (SCAM) we have an amazing number of ‘discoveries’ which – IF TRUE – should have changed the world. Here I list of 10 of my favorites:
- Diluting and shaking a substance makes it not weaker but stronger.
Homeopaths call this process ‘potentisation’. They use it to produce highly ‘potent’ remedies that contain not a single molecule of the original substance. The assumption is that potentisation transfers energy or information. Therefore, they claim, molecules are no longer required for achieving a clinical effect.
2. A substance that causes a certain symptom in a healthy person can be used to cure that symptom when it occurs in a patient.
The ‘like cures like’ principle of homeopathy is based on the notion that the similimum provokes an artificial disease which in turn defeats the condition the patient is suffering from.
3. Subluxations of the spine are the cause of most diseases that affect us humans.
DD Palmer, the inventor of chiropractic, insisted that almost all diseases are due to subluxations. These misplaced vertebrae, he claimed, are the root cause of any disease by inhibiting the flow of the ‘innate’ which in turn caused ill health.
4. Adjusting such subluxations is the best way to restore health.
Palmer, therefore, was sure that only adjustments of these subluxations were able to restore health. All other medical interventions were useless or even dangerous, in his view. Thus Palmer opposed medicines or vaccinations.
5. An imbalance of two life forces is the cause of all illnesses.
Practitioners of TCM believe that all illnesses originate from an energetic imbalance. Harmony between the two life forces ‘yin and yang’ means health.
6. Balance can be restored by puncturing the skin at specific points.
Acupuncturists are convinced that their needling is nothing less than attacking the root cause of his or her problem. Therefore, they are convinced that acupuncture is a cure-all.
7. Our organs are represented in specific areas on the sole of our feet.
Reflexologists have maps of the sole of a foot where specific organs of the body are located. They palpate the foot and when they feel a gritty area, they conclude that the corresponding organ is in trouble.
8. Massaging these areas will positively influence the function of specific organs.
Once the diseased or endangered organ is identified, the area in question needs to be massaged until the grittiness disappears. This intervention, in turn, will have a positive influence on the organ in question.
9. Healing energy can be sent into our body where it stimulates the self-healing process and restores health.
Various types of energy healers are convinced that they can transmit energy that comes from a divine or other source into a patient’s body. The energy enables the body to heal itself. Thus, energy healing is a panacea and does not even require a proper diagnosis to be effective.
10. Toxins accumulate in our bodies and must be eliminated through a wide range of SCAMs.
The toxins in question can originate from within the body and/or from the outside. They accumulate and make us sick. Therefore, we need to eliminate them, and the best way to achieve this is to use this or that SCAM
I could, of course, list many more such ‘discoveries’ – SCAM is full of them. They are all quite diverse but have one important thing in common: they are false (i.e. there is no good evidence for them and they fly in the face of science).
If they were true, they would have changed the world by revolutionizing science, physics, physiology, anatomy, pathology, therapeutics, etc.
ALL THESE UGLY FACTS DESTROYING SUCH BEAUTIFUL THEORIES!
WHAT A SHAME!!!
Astrology is nonsense!
Hold on, did we not recently discuss an RCT showing that being born under the sign of Pisces was associated with a decreased risk of death? Yes, indeed, we did!
And isn’t there a branch of homeopathy that heavily relies on astrology? Yes, indeed, astro-homeopathy does exist.
This suggests to me that a sizable proportion of my readers do believe in astrology. As I have made a New Year’s resolution to try to be nice and patient to even the weirdest of them, I herewith offer astrology fans an insight into what 2022 will bring. For that purpose, I have taken one key prediction for each star sign from a website fittingly entitled YEARLY HOROSCOPE:
- Aries will have big surprises from his life partner.
- Taurus: dept can increase by leaps and bounds.
- Gemini: expect big developments.
- Cancer: You will have a hard time keeping up with messages and appointments.
- Leo: your abilities will be appreciated.
- Virgo: you should seriously consider advancing your education.
- Libra: you’ll need to work closely with others.
- Scorpio: you, and everyone around you will focus on a variety of challenges.
- Sagittarius: you’ll refuel what might be called your inspiration tank.
- Capricorn: you may meet a fortunate contact.
- Aquarius: don’t burn any bridges that you don’t have.
Being an Aquarius myself, I am struck by the wisdom of not burning bridges that I don’t have. It is brilliant! And so fitting!!!
But then I look at the predictions for all the other signs, and I must say: they also apply to me. In fact, ALL of them apply to me, and not just me – they all apply to everyone.
Does that mean that astrology is nonsense after all?
Does that mean that my attempt to be nice to and patient with even the weirdest of the proponents of so-called alternative medicine (SCAM) has already ended in defeat?
I hope not!
For my last post of the year 2021, I take the liberty to borrow parts of a BMJ editorial entitled A NEW YEAR’S RESOLUTION OF HEALTH WORKERS:
The prospect of a return to normality seems within reach. But what will that normality look like? We believe that health workers, who have been at the frontline of the pandemic, must offer a vision of a healthier future. We must not let the terrible events of this year recast the pre-pandemic world in a glowing light. The normality we departed from at the onset of the pandemic was unjust, unsustainable, and shaped the evolution of, and responses to, the pandemic with devastating consequences, particularly for the most deprived and vulnerable.
The start of a new year offers an opportunity to question old ways of working and to ask how we can create a better future for everyone. It is a cliché to say that you should never waste a crisis. Just as in wartime and in the global financial crisis, many have profited greatly from the pandemic, whether as providers of online services or by taking advantage of the rush to procure essential goods such as personal protective equipment.
But many were far less fortunate, living in circumstances that rendered them vulnerable to an infection that spread especially rapidly through communities where successive generations had been living ever more precarious lives. As the recovery begins, the powerful groups who benefited from the social and economic systems that created those conditions will, once again, seek to shape the world to their advantage. Health workers cannot remain silent. They must offer a compelling vision of how we should reconfigure the world so that it produces and sustains health for all, resilient in the face of future threats…
A country navigating the pandemic is like a ship navigating treacherous and unpredictable waters in a storm. If the ship, its crew, and its passengers are to come through the experience unscathed it needs three things. First, it needs an experienced captain who understands the ship and commands the trust of the crew. Unfortunately, in some of the countries worst affected, captains were either away from the bridge, denied there was a storm, or had lost the trust of those on whom they depended.
Second, it needs a crew that is adequate for the size of the ship, that is well trained, and that is working as a team to achieve the same goal. Yet in too many countries, skeleton crews were working in health systems that were highly fragmented. Dissenting voices who raise the alarm about the integrity of the ship, the working of the team, or its leadership must not be silenced or lives can be lost. It also needs passengers who are as seaworthy as possible so that they can withstand the storm. One of the sentinel challenges of covid-19 was finding large segments of the population weighted by a disproportionate burden of preventable disease that predisposed them to severe covid-19 once infected.
Third, we need a ship that is securely constructed. Yet in many of the countries that have fared worst, we have been working in vessels that are full of holes. Social safety nets have been ripped asunder, allowing too many people to fall through the holes. We have made many demands on our people—to stay at home, to face loss of income—and we have added greater uncertainty to what were already difficult situations, particularly for certain racially and economically marginalised groups. The disproportionate exposure to covid-19 of many in these groups—a consequence of precarious jobs and social circumstances that denied them the luxury of social distancing—drove, in large part, the high burden of covid-19 among minority and marginalised groups worldwide.
As we look to the prospect of a covid-19 secure future, with effective vaccines, new treatments, and continued countermeasures as necessary, we must ask how we can strengthen the foundations of our societies, coming together to repair the torn safety nets. We must never be afraid to challenge our political leaders when they are going in the wrong direction, and we must insist that they really are guided by the science, and not just those bits that support their beliefs. And we must ensure that our fellow citizens are as healthy as possible so they can withstand the inevitable storms that lie ahead. We must insist that our health systems and other public systems are adequately staffed, with the tools needed to do the job, with teams that are working together, pulling in the same direction. If we do all this, then we, and the populations we serve, can be confident that we can weather any future storms.
___________________________
The editorial was written by 4 authors:
- Martin McKee, professor of European public health
- May C I van Schalkwyk, NIHR doctoral research fellow
- Nason Maani, assistant professor in public health evaluation
- Sandro Galea, dean
I think it is most sensible and thought-provoking and I suspect many of us agree with its sentiments. If it did not make you think, perhaps this information will do so:
The editorial was published one year ago in the Christmas issue of the BMJ
2020!
Yes, 2021 has disappointed many of our hopes and turned out to be a difficult year.
I wish us all that 2022 will be better, much better.
Always on the lookout for so-called alternative medicine (SCAM) that we have not yet covered on this blog, I came across a really weird one. ‘Access Consciousness’ (AC) is claimed to be a form of self-improvement therapy based on the idea that you are not wrong, that you know, and that consciousness can shift anything. It gives you access to the possibilities that exist when you no longer stick yourself and no longer believe that you are stuck. [1] Gary Douglas ([pictured below] “bestselling author, international speaker and business innovator”) pioneered this set of transformational tools in the 1990s. His work is claimed to have now spread to more than 170 countries and is claimed to have transformed the lives of tens of thousands of people. 
Access Consciousness allegedly empowers people to help themselves. The techniques of AC focus on your knowledge about yourself and the world around you. Part of what makes AC so different, according to its promoters, is that it is continuously being created. [2] AC promises to assist people with their health, weight, money, sex, relationships, anxiety, etc. It promises members, known as ‘Accessories,’ to become more conscious. To fully get it, Accessories should take part in classes. There they have 32 points on their heads lightly touched which is supposed to help them let go of all the thoughts, ideas, and emotions stored in any lifetime. Accessories are claimed to be able to “uncreate” memories of the past, or preconceived ideas picked up throughout a lifetime. As far as I can see, there is no evidence to suggest that AC is effective.
Some ex-members have alleged that AC is a “scam cooked up by a conman to rinse the vulnerable of their savings, a Scientology knock-off, and even a cult”. One ex-Accessory, for instance, claimed the group “programs its members to think like robots. It is very clever how it is done. Because it’s not like any other cult but it is mind control.” [3] In each 90-minute session, which costs up to US$ 300, 5,000 to 10,000 years of “limitations” are released, it is claimed.
My conclusion: there is no evidence that AC is plausible or effective and it is a SCAM and possibly also a cult.
[1] About Access Consciousness | Dr. Dain Heer (drdainheer.com)
[2] About Access Consciousness | Access Consciousness
[3] ‘Scientology knock-off’: Whistleblower exposes ‘cult’ that thinks ‘children are sexy’ (EXCLUSIVE) — RT UK News
THE GUARDIAN published an interesting article about vaccination hesitancy yesterday. Here is a short passage from it:
One major missing piece of the puzzle, currently under consideration, is a strategy that gets to the bottom of why 5 million people remained unvaccinated, especially those in communities with an ingrained distrust of authority.
No 10 even turned to an artificial intelligence (AI) company earlier in the year to determine the causes of vaccine hesitancy, but Whitehall sources acknowledge there is still a lack of understanding about how many of the unvaccinated remain so because of entrenched anti-vax ideology, misconceptions that could be turned around, a lack of time or transport to get to vaccine centres, or just apathy.
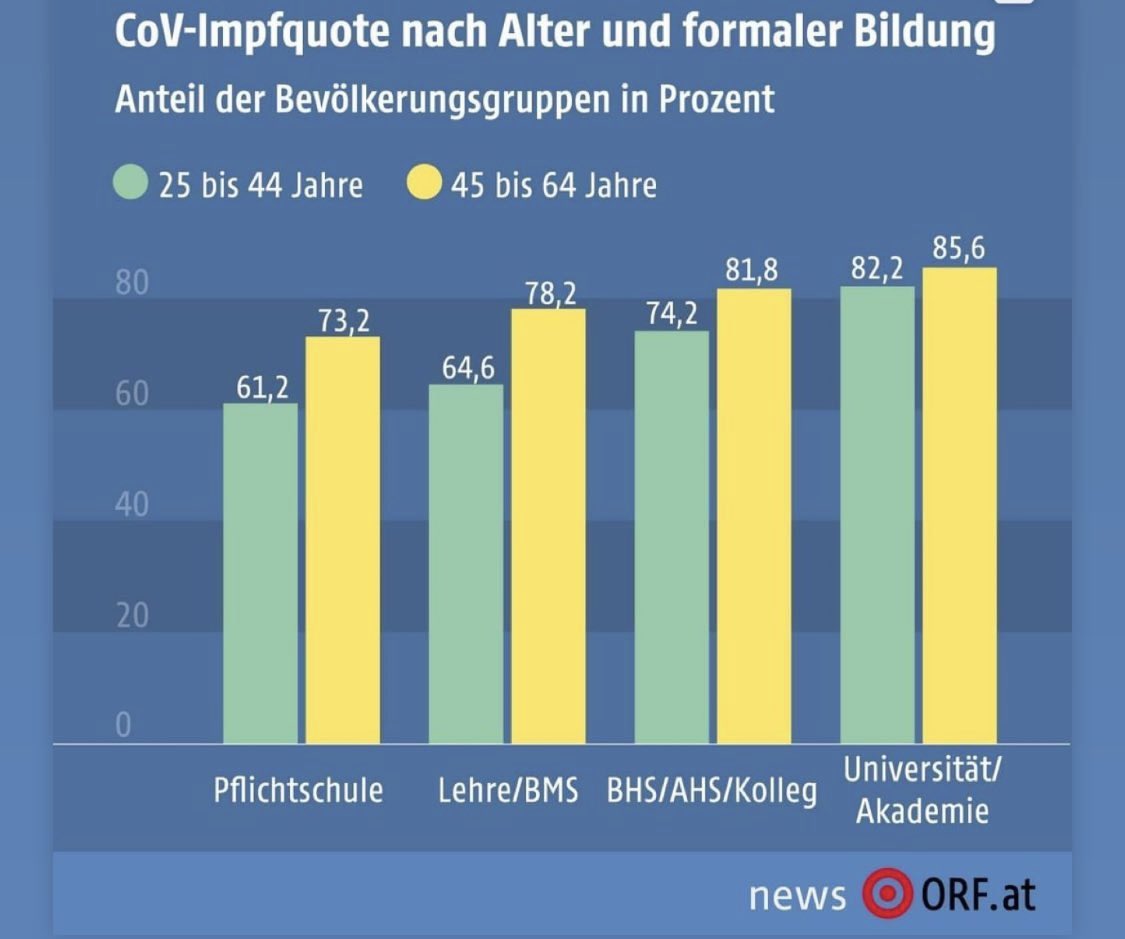
Yesterday, it was also reported in DER STANDARD that the Austrian Science Minister Martin Polaschek has commissioned a study from Statistics Austria, which for the first time was to look at the vaccination status of the population according to socio-economic characteristics.
The study yielded fascinating findings that might shed some light on the phenomenon of ‘entrenched anti-vax ideology’:
- Across all age groups, the proportion of vaccinated persons, including recovered persons, is 67%.
- Slightly less than four percent of the population are only recovered, and about 30% are neither one nor the other.
- There are no marked differences between men and women.
- The willingness to vaccinate is strongly related to the level of education.
- The vaccination rate in the group of 25-64 year-olds with a university degree is about 84% and thus significantly higher than among those who have only basic education (68%).
- In this age group, it also seems important whether someone has a job (76%) or not (69%).
- People employed in the information and communication sector (85%) and public administration (83%) are the most likely to be vaccinated.
- Workers in agriculture and forestry (67%) and construction (65%) are the least likely to accept vaccinations.
- Health and social services personnel have a vaccination rate of 79%.
- More than half of the 600,000 schoolchildren had already been vaccinated, and in the upper secondary school it was even 72%.
- The rate among teachers is also high, at 85%.
- 86% of the approximately 395,000 students at universities had been vaccinated.
- As 92% of all medical students were vaccinated.
- The vaccination rate among Austrian nationals, at about 70%, is clearly higher than that of people without an Austrian passport (52%).
- The difference between those born in Austria and those not born in Austria is only five percentage points.
- The willingness to be vaccinated is higher among people from Turkey (73%) than among those born in Austria (68%).
- Among Germans and Afghans, it is around 72%.
- People from Romania (43%) and the Russian Federation (45%) have the lowest vaccination rates.
- The percentage of vaccinated people is highest among those between 75 and 84 years.
Similar findings have, of course, been reported from other countries. However, what seems new to me here is the finding that vaccination rates are strongly correlated to the level of education: the anti-vax brigade tends to be uneducated and ignorant. If confirmed, this suggests that education might be a way to make them accept vaccinations.
PS
Of course, correlation is not causality. But there seems to be a dose-response relationship between education and willingness to vaccinate. This makes a causal effect more likely.
THOSE WHO KNOW NOTHING MUST BELIEVE EVERYTHING
Bloodletting therapy (BLT) has been widely used for centuries until it was discovered that it is not merely useless for almost all diseases but also potentially harmful. Yet in so-called alternative medicine (SCAM) BLT is still sometimes employed, for instance, to relieve acute gouty arthritis (AGA). This systematic review aimed to evaluate the feasibility and safety of BLT in treating AGA.
Seven databases were searched from the date of establishment to July 31, 2020, irrespective of the publication source and language. BLT included fire needle, syringe, three-edged needle, and bloodletting followed by cupping. The included articles were evaluated for bias risk by using the Cochrane risk of bias assessment tool.
Twelve studies involving 894 participants were included in the final analysis. A meta-analysis suggested that BLT was highly effective in relieving pain (MD = -1.13, 95% CI [-1.60, -0.66], P < 0.00001), with marked alterations in the total effective (RR = 1.09, 95% [1.05, 1.14], P < 0.0001) and curative rates (RR = 1.37, 95%CI [1.17, 1.59], P < 0.0001). In addition, BLT could dramatically reduce serum C-reactive protein (CRP) level (MD = -3.64, 95%CI [-6.72, -0.55], P = 0.02). Both BLT and Western medicine (WM) produced comparable decreases in uric acid (MD = -18.72, 95%CI [-38.24, 0.81], P = 0.06) and erythrocyte sedimentation rate (ESR) levels (MD = -3.01, 95%CI [-6.89, 0.86], P = 0.13). Lastly, we demonstrated that BLT was safer than WM in treating AGA (RR = 0.36, 95%CI [0.13, 0.97], P = 0.04).
The authors concluded that BLT is effective in alleviating pain and decreasing CRP level in AGA patients with a lower risk of evoking adverse reactions.
This conclusion is optimistic, to say the least. There are several reasons for this statement:
- All the primary studies came from China (and we have often discussed that such trials need to be taken with a pinch of salt).
- All the studies had major methodological flaws.
- There was considerable heterogeneity between the studies.
- The treatments employed were very different from study to study.
- Half of all studies failed to mention adverse effects and thus violate medical ethics.
I came across this article via a German secondary report about it entitled “Scientists discover what else protects from severe symptoms” (Forscher finden heraus, was noch vor schweren Symptomen schützt). The article rightly stressed that vaccination is paramount and then explains that, once you have caught COVID, nutrition can prevent serious symptoms.
Even though I rarely discuss standard nutritional issues on my blog (nutrition belongs to mainstream not so-called alternative medicine [SCAM], in my view), this subject did attract my attention. Here are the essentials of the original scientific paper:
Australian scientists studied the association between habitual frequency of food intake of certain food groups during the COVID-19 pandemic and manifestations of COVID-19 symptoms in adult outpatients with suspected SARS-CoV-2 infection. They included 236 patients who attended an outpatient clinic for suspected COVID-19 evaluation. Severity of symptoms, habitual food intake frequency, demographics and Bristol chart scores were obtained before diagnostic confirmation with real-time reverse transcriptase PCR using nasopharyngeal swab.
The results of the COVID-19 diagnostic tests were positive for 103 patients (44%) and negative for 133 patients (56%). In the SARS-CoV-2-positive group, symptom severity scores had significant negative correlations with the habitual intake frequency of specific food groups. Multivariate binary logistic regression analysis adjusted for age, sex, and occupation confirmed that SARS-CoV-2-positive patients showed a significant negative association between having higher symptom severity and the habitual intake frequency of legumes and grains, bread, and cereals.
The authors concluded that an increase in habitual frequency of intake of ‘legumes’, and ‘grains, bread and cereals’ food groups decreased overall symptom severity in patients with COVID-19. This study provides a framework for designing a protective diet during the COVID-19 pandemic and also establishes a hypothesis of using a diet-based intervention in the management of SARS-CoV-2 infection, which may be explored in future studies.
So, the authors seem to think that they found a causal relationship: A CHANGE IN DIET DECREASES SYMPTOMS. In different sections of the article, they seem to confirm this notion, and they state that they tested the hypothesis of the effect of diet on SARS-CoV-2 infection symptom severity.
Yey, the investigation was merely a correlative study that cannot establish cause and effect. There are many other variables that might be linked to dietary habits which could be the true cause of the observed phenomenon (or contributors to it).
What’s the harm? If the article makes people adopt a healthier diet, all is pukka!
Perhaps, in this case, that might be true (even though one could argue that this paper might support anti-vax notions arguing that vaccination is not important if it is possible to prevent severe symptoms through dietary changes). But the confusion of correlation with causality is both frequent and potentially harmful. And it is unquestionably poor science!
I feel that we need to be concerned about the fact that even reputable journals let such things pass – not least because the above example shows what the popular press subsequently can make of such misleading messages.