critical thinking
Gullibility can be described as a failure of social intelligence in which a person is easily tricked or manipulated into a course of action for which there is no plausible evidence. To express it positively, gullible people are naively trusting and thus fall for nonsensical propositions. This renders them easy prey for exploiters. 
On this blog, we see our fair share of this phenomenon, e.g.:
- people who are easily persuaded by anecdotes,
- who disregard evidence
- who fall for pseudoscience,
- who have irrational belief systems,
- who thrive on fallacies,
- who cherry-pick the evidence that fits their belief,
- who are unable to change their views in the face of evidence,
- who interpret even contradictory facts such that they confirm their belief,
- who have no ability to think critically,
- who would do just about anything to avoid cognitive dissonance.
Let me give you just three well-known examples from the realm of so-called alternative medicine (SCAM).
- Advocates of SCAM believe that natural means safe. Yet the therapies used in SCAM are neither natural nor devoid of risks.
- Advocates of SCAM believe that treatments that have a long tradition of usage must be fine. Yet a long history might just signify that the therapy in question is based on obsolete principles.
- Advocates of integrative medicine believe that, by adding unproven therapies to our medicine bag, we might improve healthcare. Yet it is clear that such a move can only make it less effective.
If I look back on 30 years of research into SCAM, I have to say that it very much looks as though a sucker is indeed born every minute.
Shiatsu is a (mostly) manual therapy that was popularised by Japanese Tokujiro Namikoshi (1905–2000). It developed out of the Chinese massage therapy, ‘tui na’. The word shiatsu means finger pressure in Japanese; however, a range of devices is also being promoted for shiatsu. The evidence that shiatsu is effective for any condition is close to non-existent.
This study aimed to investigate the effect of Shiatsu massage on agitation in mechanically ventilated patients.
A total of 68 mechanically ventilated patients were randomly assigned to two groups. Patients in the intervention group received three 5-minute periods of Shiatsu massage with a 2-minute break between them, while patients in the control group only received a touch on the area considered for the message. Data were collected before and after the intervention using the Richmond Agitation-Sedation Scale (RASS) and then analyzed.
The results showed that the level of agitation significantly decreased in the intervention group compared to the control group (p=.001).
The authors concluded that the application of shiatsu massage seems to be effective in managing agitation in mechanically ventilated patients. Further studies with greater sample size and longer follow-up period are needed to confirm the current findings.
It is good to see that, as far as I know for the first time, an attempt was made to control for placebo and other non-specific effects in a trial of shiatsu. However, in itself, the attempt is not convincing. What we need to know is whether the attempt was successful or not. Were the patients fully blinded and unable to tell the difference between verum and sham? From reading not just the abstract but the full paper, I do not get the impression that patients were successfully blinded. This means that the results might be entirely due to the effect of deblinding.
Tai chi is a meditative exercise therapy based on Traditional Chinese Medicine. On this blog, we have repeatedly discussed this so-called alternative medicine (SCAM). It involves meditative movements rooted in both Traditional Chinese Medicine and the martial arts. Tai chi was originally aimed at enhancing mental and physical health; today it has become a popular alternative therapy.
This systematic review assessed the efficiency of tai chi (TC) in different populations’ cognitive function improvement. Randomized controlled trials (RCTs) published from the beginning of coverage through October 17, 2020 in English and Chinese were retrieved from many indexing databases. Selected studies were graded according to the Cochrane Handbook for Systematic Reviews of Intervention 5.1.0. The outcome measures of cognitive function due to traditional TC intervention were obtained. Meta-analysis was conducted by using RevMan 5.4 software. We follow the PRISMA 2020 guidelines.
Thirty-three RCTs, with a total of 1808 participants, were included. The results showed that TC can progress global cognition when assessed in middle-aged as well as elderly patients suffering from cognitive and executive function impairment. The findings are as follows:
- Montreal Cognitive Assessment Scale: mean difference (MD) = 3.23, 95% CI = 1.88-4.58, p < 0.00001,
- Mini-Mental State Exam: MD = 3.69, 95% CI = 0.31-7.08, p = 0.03,
- Trail Making Test-Part B: MD = -13.69, 95% CI = -21.64 to -5.74, p = 0.0007.
The memory function of older adults assessed by the Wechsler Memory Scale was as follows: MD = 23.32, 95% CI = 17.93-28.71, p < 0.00001. The executive function of college students evaluated by E-prime software through the Flanker test was as follows: MD = -16.32, 95% CI = -22.71 to -9.94, p < 0.00001.
The authors concluded that TC might have a positive effect on the improvement of cognitive function in middle-aged and elderly people with cognitive impairment as well as older adults and college students.
These days, I easily get irritated with such conclusions. That TC might improve cognitive function is obvious. If not, there would be no reason to do a review! But does it?
This paper does not provide an answer. All it shows is that TC trials are of lousy quality and that the observed effects might well be due not to TC itself by to non-specific effects.
Yesterday, my new book arrived on my doorstep.
WHAT JOY!
Its full title is CHARLES, THE ALTERNATIVE PRINCE. AN UNAUTHORISED BIOGRAPHY. I guess that it also clarifies its contents. In case you want to know more, here is the full list of topics:
Foreword by Nick Ross v 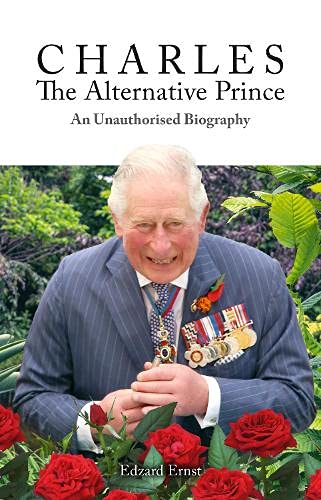
1. Why this Book? 1
2. Why this Author? 5
3. Words and Meanings 10
4. How Did It All Start? 13
5. Laurens van der Post 17
6. The British Medical Association 25
7. Talking Health 31
8. Osteopathy 37
9. Chiropractic 43
10. The Foundation of Integrated Health 50
11. Open Letter to The Times 56
12. The Model Hospital 62
13. Integrated Medicine 66
14. The Gerson Therapy 73
15. Herbal Medicine 77
16. The Smallwood Report 82
17. World Health Organisation 90
18. Traditional Chinese Medicine 96
19. The ‘GetWellUK’ Study 100
20. Bravewell 106
21. Duchy Originals Detox Tincture 110
22. Charles’ Letters to Health Politicians 115
23. The College of Medicine and Integrated Health 120
24. The Enemy of Enlightenment 126
25. Harmony 132
26. Antibiotic Overuse 142
27. Ayurvedic Medicine 147
28. Social Prescribing 154
29. Homeopathy 160
30. Final Thoughts 169
Glossary 180
End Notes 187
Index 202
In case you want to know more, here is chapter 1 of my book:
Over the past two decades, I have supported efforts to focus healthcare on the particular needs of the individual patient, employing the best and most appropriate forms of treatment from both orthodox and complementary medicine in a more integrated way.[1]
The Prince of Wales 1997
This is a charmingly British understatement, indeed! Charles has been the most persistent champion of alternative medicine in the UK and perhaps even in the world. Since the early 1980s, he has done everything in his power
- to boost the image of alternative medicine,
- to improve the status of alternative practitioners,
- to make alternative therapies more available to the general public,
- to lobby that it should be paid for by the National Health Service (NHS),
- to ensure the press reported favourably about the subject,
- to influence politicians to provide more support for alternative medicine.
He has fought for these aims on a personal, emotional, political, and societal level. He has used his time, his intuition, his influence, and occasionally his money to achieve his goals. In 2010, he even wrote a book, ‘Harmony’, in which he explains his ideas in some detail[2] (discussed in chapter 25, arguably the central chapter of this biography). Charles has thus become the undisputed champion of the realm of alternative medicine. For that he is admired by alternative practitioners across the globe.
Yet, his relentless efforts are not appreciated by everyone (another British understatement!). There are those who view his interventions as counter-productive distractions from the important and never-ending task to improve modern healthcare. There are those who warn that integrating treatments of dubious validity into our medical routine will render healthcare less efficient. There are those who claim that the Prince’s preoccupation with matters that he is not qualified to fully comprehend is a disservice to public health. And there are those who insist that the role of the heir to the throne does not include interfering with health politics.
- So, are Charles’ ideas new and exciting?
- Or are they obsolete and irrational?
- Has Charles become the saviour of UK healthcare?
- Or has he hindered progress?
- Is he a role model for medical innovators?
- Or the laughing stock of the experts?
- Is he a successful reformer of healthcare?
- Or are his concepts doomed to failure?
Charles appears to evade critical questions of this nature. Relying on his intuition, he unwaveringly pursues and promotes his personal beliefs, regardless of the evidence (Box 1). He believes strongly in his mission and is, as most observers agree, full of good intentions. If he even notices any criticism, it is merely to reaffirm his resolve and redouble his efforts. He is reported to work tirelessly, and one could easily get the impression that he is obsessed with his idea of integrating alternative medicine into conventional healthcare.
I have observed Charles’ efforts around alternative medicine for the last 30 years. Occasionally, I was involved in some of them. For 19 years, I have headed the world’s most productive team of researchers in alternative medicine. This background puts me in a unique position to write this account of Charles’ ‘love affair’ with alternative medicine. It is not just a simple outline of Charles’ views and actions but also a critical analysis of the evidence that does or does not support them. In writing it, I pursue several aims:
-
- I want to summarise this part of medical history, as it amounts to an important contribution to the recent development of alternative medicine in the UK and beyond.
- I hope to explain how Charles and other enthusiasts of alternative medicine think, what motivates them and what logic they follow.
- I will contrast Charles’ beliefs with the published evidence as it pertains to each of the alternative modalities (treatments and diagnostic methods) he supports.
- I want to stimulate my readers’ ability to think critically about health in general and alternative medicine in particular.
My book will thus provide an opportunity to weigh the arguments for and against alternative medicine. In that way, it might even provide Charles with a substitute for a discussion about his thoughts on alternative medicine which, during almost half a century, he so studiously managed to avoid.
In pursuing these aims there are also issues that I hope to avoid. From the start, I should declare an interest. Charles and I once shared a similar enthusiasm for alternative medicine. But, as new evidence emerged, I changed my mind and he did not. This led to much-publicised tensions and conflicts. Yet it would be too easy to dismiss this book as an act of vengeance. It isn’t. I have tried hard to be objective and dispassionate, setting out Charles’ claims as fairly as I can and comparing them with the most reliable evidence. As much as possible:
-
- I do not want my personal discords with Charles to get in the way of objectivity.
- I do not want to be unfairly dismissive of Charles and his ambitions.
- I do not want to be disrespectful about anyone’s deeply felt convictions.
- I do not aim to weaken the standing of our royal family.
My book follows Charles’ activities in roughly chronological order. Each time we encounter a new type of alternative medicine, I will try to contrast Charles’ perceptions with the scientific evidence that was available at the time. Most chapters of this book are thus divided into four parts
-
- A short introduction
- Charles’ views
- An outline of the evidence
- A comment about the consequences
While writing this book, one question occurred to me regularly: Why has nobody so far written a detailed history of Charles’s passion for alternative medicine? Surely, the account of Charles ‘love affair’ with alternative medicine is fascinating, diverse, revealing, and important!
I hope you agree.
BOX 1
The nature of evidence in medicine and science
- Evidence is the body of facts, often created through experiments under controlled conditions, that lead to a given conclusion.
- Evidence must be neutral and give equal weight to data that fail to conform to our expectations.
- Evidence is normally used towards rejecting or supporting a hypothesis.
- In alternative medicine, the most relevant hypotheses often relate to the efficacy of a therapy.
- Such hypotheses are best tested with controlled clinical trials where a group of patients is divided into two subgroups and only one is given the therapy to be tested; subsequently the results of both groups are compared.
- Experience does not amount to evidence and is a poor indicator of efficacy; it can be influenced by several phenomena, e.g. placebo effects, natural history of the condition, regression towards the mean.
- If the results of clinical studies are contradictory, the best available evidence is usually a systematic review of the totality of rigorous trials.
- Systematic reviews are methods to minimise random and selection biases. The most reliable systematic reviews are, according to a broad consensus, those from the Cochrane Collaboration.
[1] https://www.princeofwales.gov.uk/speech/article-hrh-prince-wales-titled-science-and-homeopathy-must-work-harmony-daily-telegraph
[2] https://www.amazon.co.uk/Harmony-New-Way-Looking-World/dp/0007348037
In case you want to know even more – and I hope you do – please get yourself a copy.
Guest post by Richard Rasker
Author’s disclaimer: this article is mostly based on the situation in the US, but also applies to many other countries as well, at least in part. Also, corrections are welcome, as I have not been able to find information on all legal details mentioned here. My apologies in advance for any inaccuracies or untruths. These will be corrected if signalled.
Homeopathy has been around for well over 200 years now. Despite the fact that it has been thoroughly debunked by science as a legitimate form of medicine already as early as 1835 (and many, many times more since then), and is based on principles that fly in the face of basic laws of chemistry, physics, and even logic, it still has quite a lot of practitioners and followers. And despite the fact that there is not a single homeopathic ‘remedy’ with proven efficacy for even one condition, homeopaths keep claiming that it is a very effective form of medicine. In fact, quite a few practitioners even maintain that their treatments are better than regular medical treatments, which are often dismissed as ‘allopathy’, and ‘just suppressing symptoms’, whereas they themselves claim to ‘treat the root cause of diseases’. And yes, this not only sounds arrogant, it is arrogant.
Where does this arrogance come from? How can these people keep on making claims that have been proven false countless times already? And why are they allowed to pretend that they are a kind of doctor, even if many of them have no medical training whatsoever?
It turns out that homeopaths not only think that they are special, but that in many countries, they indeed enjoy quite a few what I would call Peculiar Perks and Privileges:
• Homeopaths are allowed to treat people suffering from medical complaints without having received any medical training whatsoever.
• Homeopaths are exempt from most of the rules that real doctors are subject to. E.g. homeopaths do not have to bother with things like keeping medical records; they are not obliged to register anything about their patients conditions, treatments, or treatment outcomes.
• Homeopaths, unlike real doctors, are not legally obliged to keep up with the current state of medical science – quite the contrary, in fact: homeopaths are allowed to treat patients in ways that fly in the face of modern science, and are instead based on ancient belief in (sympathetic) magic.
• Homeopaths are not accountable to anyone or any organization with regard to their activities and professional conduct. Even when patients in their care suffer harm, they are almost never disciplined. (And real doctors are usually expected to clean up the mess.)
• Homeopaths are allowed to lie about their ‘remedies’, e.g. they can claim that it contains an ‘active ingredient’ that is completely absent.
• Homeopathic preparations can be legally registered, sold and marketed as medicines without any testing of efficacy and safety whatsoever[1].
• European law even goes one step further: member states are required to register homeopathic preparations as medicines without requiring any evidence of therapeutic efficacy. This is bizarre, as the same EU laws demand that real medicines must have proven efficacy before they can be registered. In effect, EU law gives homeopathy the explicit privilege to lie to its customers about the efficacy of their ‘medicines’.
So yes, homeopathy must be Very Special indeed to have all these privileges! And it is therefore quite understandable that many homeopaths think of themselves as healthcare professionals. Yet in spite of this, many homeopaths are not quite satisfied, and crave the ultimate prize: official recognition of homeopathy as a part of real medicine.
I argue that this is an excellent idea, under one condition: if homeopaths want to be regarded as real medical professionals, then they should also be held to the same standards as medical professionals. This means that homeopathic preparations should only be approved as medicines after providing proper scientific evidence of both safety and efficacy. Also, homeopaths should no longer be allowed to treat patients without receiving any medical training. Instead, they should be educated to the same standards as other doctors before being allowed to practice their medicine.
So I really hope that homeopaths get what they want: the same rights and obligations as real doctors. Let’s see how long they last if they actually have to demonstrate the viability and benefits of their diagnoses, remedies and treatments!
But joking apart, at the very least the bizarre privileges for homeopathy should be abandoned, and lawmakers should re-evaluate the rationale (or rather the lack thereof) behind these privileges, which are as archaic and outdated as homeopathy itself.
An important point of action therefore would be to properly educate those lawmakers and legal institutions about the medical and scientific consensus on homeopathy, as these organizations still base a lot of their views and decisions on the long-refuted principles of homeopathy[2]. In doing so, it should be emphasized that not only does modern science not support any of the premises of homeopathy, but that in well over 200 years, homeopathy itself has never come up with even one(!) ‘remedy’ for which there is actual evidence of efficacy in a properly conducted scientific trial.
[1]: In the US, the only requirement for approval of a homeopathic preparation as a medicine is that a group of homeopaths (the Homeopathic Pharmacopoeia Convention of the United States(**)) gives a particular preparation their blessing. However, this decision is solely based on a declaration from the manufacturer of the product that a so-called ‘proving’ has taken place, which means that a dozen or so healthy people have taken the product and recorded any unusual ‘symptoms’ they experienced. Homeopaths believe that this preparation can then treat sick people with similar symptoms. This is nothing short of insane, for more than one reason:• This ‘proving’ proves nothing at all, as it involves no patients and no illness whatsoever. If any pharmaceutical company would test their products in this way, they would be forced to close their business immediately.
• There is not a shred of evidence that what makes healthy people feel ill can cure sick people. Give a healthy person poison, and he will get sick. Give a sick person poison, and he will get even sicker – regardless of the actual symptoms caused by the disease or the poison.
• The whole concept that a homeopathic preparation can cause symptoms in healthy people, yet cure those symptoms in sick people is in fact extremely silly. Just think about it: according to homeopaths, if you give a healthy person Remedy X, they then would get all sorts of symptoms associated with that remedy. But now comes the million-dollar question: how do you cure these people after they developed these symptoms? Well, you give them Remedy X again of course!
**: Recently, the Center for Inquiry has filed a lawsuit under the Freedom of Information act to obtain access to the so-called Homeopathic Pharmacopoeia of the United States (HPUS). The HPUS is a register listing all homeopathic preparations that have been granted the legal status of medicine, complete with all details about those preparations. However, even though the HPUS is highly important from a legal and medical point of view, it is not publicly accessible, with access costing up to $15,000 per year.
[2]: Many legal organizations still appear to listen primarily to homeopaths rather than to scientists. E.g. in this editorial, the old and long discredited myths about the viability of homeopathy are repeated verbatim:“By way of background, homeopathy is the practice of treating symptoms with very small doses of substances that have produced similar symptoms in healthy subjects, and it is based on the principle that “like cures like.” In one sense, homeopathic medicine is the grandfather of vaccines and allergy shots, which are based on the same principle. Homeopathy is a system of medicine that has a well-established framework for demonstrating the effectiveness of products; in particular, effectiveness is shown using “provings,” a procedure employed in healthy individuals to determine the dose of a drug sufficient to produce symptoms.”
As long as legal and official organizations ignore science and blindly follow homeopathy’s misleading explanations and information, homeopathy will keep its undeserved privileges (and also note that ‘privilege’ literally means “[its] own law”)
Guest post by Tobias Katz
What do we know?
ICU admission
Taken from the BMJ (Ref 1): ICNARC latest report 31/12/21 showed that the proportion of patients admitted to critical care in December 2021 with confirmed covid-19 who were unvaccinated was 61%.
Prevention of infection
The government’s week 45 Covid surveillance report (Ref 3) is clear that vaccination prevention of infection (positive PCR, for Delta) effectiveness is estimated at 65% for Oxford-AstraZeneca and 80% for Pfizer.
Prevention of transmission
The Lancet’s (Ref 4) paper, suggests once infected, initial viral load is similar for vaccinated and unvaccinated individuals, suggesting likely equal chance of transmitting on the virus.
Protection of the individual
Ref 3, is clear cut that vaccination protects individuals from hospitalisation and severe infection (for Delta).
(Omicron) “Among those who had received 2 doses of AstraZeneca, there was no effect against Omicron from 20 weeks after the second dose. Among those who had received 2 doses of Pfizer or Moderna effectiveness dropped from around 65-70% down to around 10% by 20 weeks after the 2nd dose. 2 to 4 weeks after a booster dose vaccine effectiveness ranged from around 65 to 75%, dropping to 55 to 70% at 5 to 9 weeks and 40-50% from 10+ weeks after the booster.” (Ref 2)
Effectiveness here is measured by admission to hospital and shows the necessity for booster jabs when fighting Omicron.
Who are Dr James and Dr Malhotra?
Steven James, consultant anaesthetist, has recently been in the news for confronting Sajid Javid RE mandatory vaccinations for hospital and nursing staff. “The science isn’t strong enough” to support the policy he stated and “I’ve got antibodies”, suggesting that he’s as protected as he would be if he had a vaccine.
Aseem Malhotra, who goes by the name of ‘lifestylemedicinedoctor’ on Instagram is an extremely controversial cardiology consultant who seems to be Djokovic’s biggest fan and whose tweets are passionately quoted and forwarded by anti-vaxxers.
With tweets such as “Mark my words, with everything we know and don’t know about the current vaccine Novak Djokovic will ultimately be proven to be on the right side of history #BadPharma #truth #transparency #InformedConsent”:
Mark my words, with everything we know and don’t know about the current vaccine Novak Djokovic will ultimately be proven to be on the right side of history #BadPharma #truth #transparency #InformedConsent
— Dr Aseem Malhotra (@DrAseemMalhotra) January 9, 2022
And a retweet: “Dr Jordan Peterson Oh well. It’s just fertility. Women’s Periods May Be Late After Coronavirus Vaccination, Study Suggests”; he stirs the cooking pot of anti-establishment rhetoric and only deepens an already fractured relationship between doctors and their patients caused by the pandemic.
Oh well. It's just fertility. Women’s Periods May Be Late After Coronavirus Vaccination, Study Suggests https://t.co/ndQC9QgwMH
— Dr Jordan B Peterson (@jordanbpeterson) January 8, 2022
You’d think a mature, well-researched doctor would be able to tell the difference between the menstrual cycle and becoming fertile. You’d also hope he would not be short-sighted enough to support one of the most anti-science/anti-conventional medicine public figures in the world (see here)… Alas, no.
I feel as though both of these figures need to be reminded of their ethical duty of candour as doctors and reminded that their public actions have consequences. I may not completely disagree with Dr James (RE mandatory vaccinations) but the way in which he conducted himself during this nationally broadcasted video left many shaking with rage as it undermines many of his health professional colleagues. Me, included.
When a doctor appears on national news, opposing [mandatory] vaccination and offering incorrect explanations of why this is so, it should be obvious to them that their opinion will inevitably act as anti-vaccine propaganda, whether meant for this or not.
Malhotra’s ideas (cutting back on statins, healthy diet etc.) are often worth consideration/evaluation and as a new-age medical ‘influencer’ with 130k+ followers on Twitter, with ample publications behind him, he deserves to be listened to. Not necessarily agreed with, but listened to. But he also has a duty as a doctor to guard against complacency. Similar to James’ public actions, Malhotra’s tweets that are so one-sided give a biased, inaccurate and frankly dangerous view on the efficacy and safety profile of COVID vaccinations that have been safely and effectively used in millions of people to prevent hospitalisations. Is he doing it for the views? The hits? The likes? The retweets? To have people recognise him for his Pioppi diet?
What should we do?
Candour
Doctors, including James and Malhotra have an ethical responsibility not to spread imperfect information to a wide-receiving audience where their actions can be misconstrued and misrepresented so easily. Doing so may bolster anti-vaccine views, cause less ‘on-the-fence’ people to get the jabs and essentially lead to more preventable deaths.
More and more we are seeing social media take over and often act as the public’s primary source of news. More doctors than ever are now in the [social] media limelight. Some, such as Dr Alex George (mental health advocate) are promoting health responsibly. Others, seek to undermine it. In an era when Joe Rogan has more daily views than Fox News’ Tucker Carlson, to ignore and not rebut [health] social media giants like Malhotra would just worsen the situation. Malhotra and James need to be challenged by the scientific community, as the BBC so brilliantly did here.
Complacency
If doctors want to become socialite Instagram influencers, they must do this without complacency. I think this means being responsible when offering controversial and potentially public health implicating opinions where evidence isn’t clear cut.
Final thoughts
Using all the possible information above, as the vaccines are not 100% without risk, transmission is not completely cut post-vaccine and as we have a decent-ish way of monitoring infection (lateral flows and PCRs), I feel as though mandating vaccines for all NHS staff is currently unjust. I see Steve’s point. But I’d be extremely careful in how I’d make this point. And certainly not on live Sky News when the nation is watching, where it will inevitably be seized upon by the anti-vax community.
Saying this, the data is pretty clear that there is evidence that the vaccines offer protection against infection, reducing viral load quicker once infected and against hospitalisation and so if you’re a rational doctor who thinks that at least one time your lateral flow test may give a false negative, it makes complete sense to get your vaccine to protect your patients…
References
- https://www.bmj.com/content/376/bmj.o5?fbclid=IwAR2MgoD_vYo0FsaVsQdLxfeYCukuRu2RegcJa-HclA13byhH71g-AnNhnP8
- https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/1045329/Vaccine_surveillance_report_week_1_2022.pdf
- https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/1032859/Vaccine_surveillance_report_-_week_45.pdf
- https://www.thelancet.com/journals/laninf/article/PIIS1473-3099(21)00690-3/fulltext
I have decided to herewith start
The ‘WORST PAPER OF 2022’ competition
And I have already come across an article that I can nominate for it. It is entitled ‘What is the goal of science? ‘Scientific’ has been co-opted, but science is on the side of chiropractic‘. It is worth reading it in full, but in case you are in a hurry, I have extracted some bon mots for you:
- Most of what chiropractors do in natural health care is scientific; it just has not been proven in a laboratory at the level we would like.
- It might be useful to review scientific method here. First, you make an observation, then pose a testable question based on that observation. You state your hypothesis, then design and perform an experiment, collect data and draw a conclusion.
- A lot of our information is based on observations or hypotheses, and that is not a bad thing.
- [conventional] medicine fails to be scientific because it ignores clinical observations out of hand.
- the majority of the observations that we in the natural health community work with are not even taken seriously. We would like to think that this is not because the medical “scientific” journals sell ads to drug companies.
- we have multibillion-dollar corporations controlling our observations and our conversations about health — not very scientific.
- When something is labeled anecdotal, to the medical community it means it is unimportant. That is not necessarily true; it means a lot of people have made the same observation.
- [the pharma industries] have positioned themselves to be the ones who decide what is or is not true in our health care system.
- Combining the “anecdotal” information from colleagues and one’s individual clinical observations, elegant and effective models for disease and strategies for treatment begin to emerge.
- everyone in natural health care knows to combine therapies and the effects are often cumulative. For example, many asthmatics respond to magnesium supplementation. Some respond to taking vitamin C or another antioxidant. Most of us know that combining the two supplements increases favorable results.
- drugs have side effects and often harm the patient. They often work against each other. We don’t have that problem with vitamins and minerals; you will not harm the patient.
- we are not treating a disease, we are correcting a deficiency. If the asthmatic is deficient in magnesium, symptoms will improve. Giving magnesium is not a treatment of the asthma; it is fixing infrastructure.
- We don’t really treat disease; we improve infrastructure.
- When our patients improve, we know we are on the right track. That is what the scientific method is all about.
- Finding errors in physiology and correcting them may produce results where medicine has failed so miserably. We are following scientific method, but studies are expensive and some things, even though they seem to hold up anecdotally, have not been proven.
As the year is still young, this paper might not actually win the competition but I hope you agree that it is a worthy competitor.
Some of you will ask what is there to win in the ‘WORST PAPER OF 2022’ competition? I agree: a competition without a prize is no fun. Therefore, I suggest donating to the winner one of my books that best fits his/her subject. I am sure this will over-joy him or her.
Now we only need to determine how we identify the winner. I suggest that I continue blogging about nominated papers (I hope to identify about 10 in total), and towards the end of the year, I let my readers decide democratically.
Please take a moment to read this short letter by the ‘LIGA MEDICORUM HOMOEOPATHICA INTERNATIONALIS’:
As you know, the World Health Organization (WHO) is predicting that civilization faces a crisis of antibiotic-resistant diseases that may soon result in as many as 10 million deaths per year while pushing as many as 24 million people into extreme poverty.
We, the undersigned, are duly licensed healthcare professionals practicing homeopathy, with the authority to diagnose and treat disease, who have reviewed the extensive research literature demonstrating the clear therapeutic value of homeopathy. Each of us has had extensive clinical experience successfully treating hundreds of thousands of patients suffering from infectious diseases worldwide.
Homeopathy works, does not cause further antibiotic resistance, is generally devoid of side effects, is inexpensive, and is good for health of the planet.
We are calling upon the WHO to encourage the international medical community to immediately begin training in homeopathy as an adjunctive therapeutic measure to avoid this catastrophic loss of life and would like a meeting with you or your representative to discuss the grave challenge of antibiotic resistance at your earliest convenience.
Thank you for considering this urgent appeal.
________________________
I stated above that this is a letter. In fact, it is more – it is a petition directed to the Director-General of the World Health Organization (WHO), Dr. Tedros Adhanom Ghebreyesus, to immediately begin training physicians in homeopathy as an adjunctive therapeutic measure to combat the looming crisis of antibiotic-resistant diseases.
The Liga Medicorum Homoeopathica Internationalis (LMHI) represents homeopathic physicians in more than 70 countries all over the world. The purposes of the association are the development and securing of homeopathy worldwide and the creation of a link among licensed homeopaths with medical diplomas and societies and persons who are interested in homeopathy. The LMHI is exclusively devoted to non-profit activities serving philanthropic benefits.
The LMHI might ring a bell for regular readers of this blog. A few years ago, I reported that its president advocates curing cancers with homeopathy. And in 2014, I reported that a journey to Liberia of leading homeopaths was co-organized by the LMHI; its purpose was to cure Ebola patients of their disease with homeopathy.
I find all of this seriously worrying – not because I fear that the WHO will now start training physicians across the globe in homeopathy. It is worrying, I feel, because it shows how hopelessly deluded homeopaths are. The fact that clinicians so far detached from reality treat ill and vulnerable patients frightens me.
On this blog and elsewhere, I have heard many strange arguments against COVID-19 vaccinations. I get the impression that most proponents of so-called alternative medicine (SCAM) hold or sympathize with such notions. Here is a list of those arguments that have come up most frequently together with my (very short) comments:
COVID is not dangerous
It’s just a flu and nothing to be really afraid of, they say. Therefore, no good reason exists for getting vaccinated. This, I think, is easily countered by pointing out that to date about 5.5 million people have died of COVID-19. In addition, I fear that the issues of ‘long-COVID’ is omitted in such discussions
It’s only the oldies who die
As an oldie myself, I find this argument quite distasteful. More importantly, it is simply not correct.
Vaccines don’t work
True they do not protect us 100% from the infection. But they very dramatically reduce the likelihood of severe illness or death from COVID-19.
Vaccines are unsafe
We have now administered almost 10 billion vaccinations worldwide. Thus we know a lot about the risks. In absolute terms, there is a vast amount of cases, and it would be very odd otherwise; just think of the rate of nocebo effects that must be expected. However, the risks are mostly minor, and serious ones are very rare. Some anti-vaxxers predicted that, by last September, the vaccinated population would be dead. This did not happen, did it? The fact is that the benefits of these vaccinations hugely outweigh the risks.
Vaccines are a vicious tracking system
Some claim that ‘they‘ use vaccines to be able to trace the vaccinated people. Who are ‘they‘, and why would anyone want to trace me when my credit card, mobile phone, etc. already could do that?
Vaccines are used for population control
‘They‘ want to reduce the world population through deadly vaccines to ~5 billion, some anti-vaxxers say. Again, who are ‘they‘ and would ‘they‘ want to do that? Presumably ‘they‘ need us to pay taxes and buy their goods and services.
There has not been enough research
If those who make this argument would bother to go on Medline and look for COVID-related research, they might see how ill-informed this argument is. Since 2021, more than 200 000 papers on the subject have emerged.
I trust my immune system
This is just daft. I am triple-vaccinated and also hope that I can trust my immune system – this is why I got vaccinated in the first place. Vaccinations rely on the immune system to work.
It’s all about making money
Yes, the pharma industry aims to make money; this is a sad reality. But does that really mean that their products are useless? I don’t see the logic here.
People should have the choice
I am all for it! But if someone’s poor choice endangers my life, I do object. For instance, I expect other people not to smoke in public places, stop at red traffic lights and drive on the correct side of the street.
Most COVID patients in hospitals have been vaccinated
If a large percentage of the population has been vaccinated and the vaccine conveys not 100% protection, it would be most surprising, if it were otherwise.
I have a friend who…
All sorts of anecdotes are in circulation. The thing to remember here is that the plural of anecdote is anecdotes and not evidence.
SCAM works just as well
Of course, that argument had to be expected from SCAM proponents. The best response here is this: SHOW ME THE EVIDENCE! In response SCAM fans have so far only been able to produce ‘studies’ that are unconvincing or outright laughable.
In conclusion, the arguments put forward by anti-vaxxers or vaccination-hesitant people are rubbish. It is time they inform themselves better and consider information that originates from outside their bubble. It is time they realize that their attitude is endangering others.
Like so many other anti-vaxxers, Djokovic is deep into so-called alternative medicine (SCAM).
An article in THE TELEGRAPH explains it quite clearly. Here are a few passages:
Here is an anti-scientific crank hiding in plain sight … [In his book Djokovic explains] how he suffered from recurring physical ailments – allergies, breathing difficulties, blocked sinuses – until he gave up gluten.
Nothing especially weird so far – until he explains how his gluten intolerance was diagnosed. A Serbian nutritionist called Dr Igor Cetojevic asked Djokovic to hold his right arm out at right angles and resist the pressure as he pushed down on it. Then the exercise was repeated, only this time while Djokovic held a slice of bread against his stomach. “I was noticeably weaker,” writes Djokovic, who adds that “kinesiological arm testing [has] long been used as a diagnostic tool by natural healers.” Yes, and mediums have long claimed to speak to the dead …
Here is a man who broke up his visits to Wimbledon with trips to the nearby Buddhapadipa Temple to meditate by a lake. A man who revealed two years ago that he has a “friend” in Melbourne’s Botanical Gardens – “a Brazilian fig tree that I like to climb”. Yes, Djokovic’s jet-setting spiritualism might sound charming in itself. But its side-effect has been credulousness.
Serve To Win [ND’s book] describes a so-called “researcher” taking two glasses of water and directing loving energy towards one, while swearing angrily at the other. “After a few days … [the angry glass] was tinted slightly green … the other glass was still bright and crystal clear”. Harmless, perhaps, if deeply dippy. But then, last year, Djokovic could be found hosting a former estate agent called Chervin Jafarieh on his Instagram Live channel. Jafarieh was selling bottles of Advanced Brain Nutrients at $50 apiece, which – like Djokovic’s resistance to the Covid vaccination – sounded contrary to the interests of public health…
… Djokovic expressed in a 2018 interview with Shortlist magazine. “I believe that it is our mission to reach a higher frequency through self-care by exploring and respecting our own avatar, our body and, by doing that, raising the vibration of the planet.” …
And so we return to the dark side of this whole peculiar tale. Were Djokovic just a journeyman player, his pseudo-scientific beliefs would be no more than a bizarre footnote. As it is, he is a powerful role model, particularly in the Balkans. Thousands of people have probably emulated his stance on vaccines. Some are likely to suffer consequences as a result…
Another article explains:
New York Times tennis reporter Ben Rothenberg tweeted out after the news of Djokovic’s visa rejection that the Serbian had been “wildly anti-science” over the years. 
“Let’s not lose sight of how wildly anti-science Djokovic has publicly been for years,” Rothenberg began. “Here he was last year preaching about how you can change water with emotion.
“Naive, but maybe these real consequences today can be a reality check for his nonsense?”
Former New York Times reporter Steven Greenhouse said it was “sad to see such a brilliant tennis player join the anti-science, pro-poppycock anti-vaxxers”.
Tennis Channel producer David Kane added: “I sort of don’t care whether Australia bungled L’Affaire Novak because of political/media pressure. This is about someone who has been stridently anti-science and never indicated a good faith effort to receive this essentially mandatory vaccine.F around & find out, as they say.”
And a Guardian article provides further information:
His belief in alternative medicine is complemented by his commitment to alternative history. He frequently retreats to Visoko, in the hills of Bosnia and Herzegovina, where he meets up with the businessman Semir Osmanagic – whose claims that there are ancient man-made structures with magical healing powers, refuted by scientists, have turned the hills into a lucrative tourist destination. Djokovic has also expressed his support for the ultranationalist alternative historian Jovan Deretic, whose writings claim, among other things, that numerous European cultures, including ancient Greeks, Celts and Etruscans, are descended from Serbs.
I am quite confident that I play tennis as splendidly as Djokovic understands medicine. Yet, I do not pretend to be able to teach you how to do a perfect ‘top slice’. In contrast, Djokovic loves to take the role of ambassador for SCAM and other weird stuff.
His father stated that “Novak is the Spartacus of the new world who does not tolerate injustice, colonialism and hypocrisy but fights for the equality of all on this planet, regardless of skin color, religious belief and money they have.” Personally, I see this differently: Djokovic is badly affected by proctophasia; he tolerates no end of BS and fights for pseudoscience. And sadly, his views are all too persuasive to gullible consumers – not exactly what we need in a global health crisis!
