critical thinking
Chiropractors often refer their patients for full-length (three- to four-region) radiographs of the spine as part of their clinical assessment, which are frequently completed by radiographers in medical imaging practices. Overuse of spinal radiography by chiropractors has previously been reported and remains a contentious issue.
The purpose of this scoping review was to explore the issues surrounding the utilization of full-length spinal radiography by chiropractors and examine the alignment of this practice with current evidence.
A search of four databases (AMED, EMBASE, MedLine and Scopus) and a hand search of Google was conducted. Articles were screened against an inclusion/exclusion criterion for relevance. Themes and findings were extracted from eligible articles, and evidence was synthesized using a narrative approach.
In total, 25 articles were identified, five major themes were extracted, and subsequent conclusions drawn by authors were charted to identify confluent findings:
- (1) The historical integration of FLS radiography in chiropractic,
- (2) Clinical indications for FLS radiography in chiropractic,
- (3) Risks associated with FLS radiography,
- (4) Chiropractic techniques which prescribe the use of FLS radiography,
- (5) Current trends in the utilisation of FLS radiography in chiropractic.
This review identified a paucity of literature addressing this issue and an underrepresentation of relevant perspectives from radiographers. Several issues surrounding the use of full-length spinal radiography by chiropractors were identified and examined, including barriers to the adherence to published guidelines for spinal imaging, an absence of a reporting mechanism for the utilization of spinal radiography in chiropractic and the existence of a spectrum of beliefs amongst chiropractors about the clinical utility and limitations of full-length spinal radiography.
The authors concluded that this review has identified a scarcity of literature addressing the completion of chiropractor‐referred FLS X‐rays. Our review has outlined several pressing issues that warrant further investigation including a lack of quantitative measures to assess the utilisation of FLS X‐rays by chiropractors, a lack of consensus of what constitutes appropriate clinical justification for imaging and the existence of a spectrum of beliefs amongst chiropractic authors about the clinical utility and limitations of FLS radiography. This provides radiographers with a definitive opportunity to demonstrate clinical leadership in this space and seek to begin a constructive dialogue with chiropractic referrers about the risks associated with unnecessary or unjustified spinal radiography. In doing this, diagnostic radiographers as evidence‐based health practitioners can actively contribute to the conversation surrounding the issues identified by this study and can be better positioned to advocate for the interests of the discipline and the safety of their patients.
The authors of this review make a number of further relevant points:
- Between 2014 and 2015, approximately 130,000 three‐ to four‐region spinal X‐rays were performed in Australia. Most were requested by chiropractors.
- In Australia, chiropractors often request FLS X‐ray examinations by radiographers.
- A spectrum of beliefs and knowledge exists amongst chiropractic practitioners surrounding the appropriate use of FLS radiography which may not always align with the principles of evidence‐based practice.
- The risks associated with the overutilization of diagnostic imaging are well documented. Aside from the inherent risks of unnecessary exposure to ionizing radiation, increased reliance on diagnostic imaging by any practitioner in the absence of sufficient clinical justification increases economic burdens encumbered upon the health care system. As such, FLS radiography should be used judiciously to ensure risks associated with its use are minimized, thus ensuring that it remains available to chiropractors and other practitioners where its use is clinically justified.
- Imaging that is not clinically indicated also carries a risk of overdiagnosis that being the radiological diagnosis of disease which does not ultimately impact on a patient’s course of treatment.
- The use of FLS radiography by chiropractors for the detection of red flags in the absence of any significant clinical indications for imaging could be considered a practice that carries a high risk of overdiagnosis.
When I first raised the issue of chiropractic overuse of imaging in 1998, I got fiercely attacked by a gang of chiros. Each time hence that I mention the subject, chiros loudly protest, and I do, of course, understand why. Imaging gives chiros the flair of being ‘cutting edge’; more importantly, in most countries, it is an easy source of additional income.
So, I do not expect that things will be different this time. Yet, I feel that, instead of constantly trying to shoot the messenger, chiropractors might be well advised to consider the message.
This cohort study was designed as undertaken to evaluate the protective effect of Arsenicum album 30C against COVID-19.
Participants were enrolled in a homeopathy intervention (HI) cohort (who received Arsenicum album) or in a non-intervention (NI) cohort (who received no systematic intervention) from COVID-19 containment areas of Delhi. Individuals of age 5 years or above were given four medicated pills of Arsenicum album 30C, while those from 1 to 5 years old were given two medicated pills in each dose.
The analysis included 10,180 individuals residing in 11 COVID-19 containment areas in Delhi, out of which 6,590 individuals were in the HI cohort and 3,590 individuals were in the NI cohort. The overall protective effect of Arsenicum album 30C was 83% (95% confidence interval [CI], 76.77 to 88.17): 45 cases per 6,590 (8.34 per 10,000 person-weeks) in the Arsenicum album 30C group versus 143 cases per 3,590 (45.01 per 10,000 person-weeks) in the NI cohort. The protective effect of Arsenicum album 30C against laboratory-confirmed COVID-19 was 74% (95% CI, 55.08 to 85.41): 18 cases per 6,590 (3.32 per 10,000 person-weeks) in the Arsenicum album 30C group versus 38 cases per 3,590 (11.85 per 10,000 person-weeks) in the NI cohort.
The authors concluded that the use of Arsenicum album 30C was associated with some protection against probable and laboratory-confirmed COVID-19 in a containment-zone setting. Randomized controlled trials are needed to confirm or refute these results.
It is remarkable, I feel, that the authors conclude Arsenicum album 30C was associated with some protection. All too often enthusiasts of homeopathy claim a causal link where there is none – but not this time, and I wonder why.
Unfortunately, I was unable to read the full text of the paper (it’s behind a paywall and I would be grateful for anyone to make it available). Thus, I cannot comment on one of the most crucial questions related to the study: how were the patients divided into the two groups?
It is clear that it was not by randomization. Yet only randomization would have created two fully comparable groups. The most likely explanation for the findings of this trial is therefore that the two groups differed in terms of one or more prognostic factors. This would explain why a group of patients receiving a placebo (Arsenicum album C30 is a dilution of Arsenic at a ratio of 1: 1000000000000000000000000000000000000000000000000000000000000 and therefore is a pure placebo [unless, of course, one believes in homeopathic magic) experience different outcomes from those receiving nothing.
As I said, the answer can only be found by studying the precise selection criteria used in this study. Until this is cleared up, I can only say three things for sure:
- A causal link between the treatment and the result is highly unlikely.
- It is regrettable that researchers do not use randomization for potentially important trials.
- It seems unethical to encourage placebo use for the prevention of a serious illness.
_______________________
UPDATE
I just received the full text from one of the authors. This is what they say about the allocation of the participants:
“Participants were enrolled in two cohorts: the homeopathy intervention (HI) cohort and the non-intervention (NI) cohort. Recruitment to the cohorts was at cluster level (containment area): the clusters were allotted to the HI cohort or the NI cohort as per convenience.”
I am afraid, this tells me very little, and my concerns noted above still apply.
A few other points are of relevance:
- The study was conducted between April and August 2020. This begs the question of why it took 2 years to publish the findings.
- The outcomes were verified via telephone. This means that social desirability might have influenced the results.
- The paper also confirms that there were many important differences between the groups that might have prognostic significance.
- The conclusion at the end of the paper does imply causality in stronger terms than the abstract: “The use of Arsenicum album 30C may help protect against COVID-19 infection. Randomized controlled trials are needed
to confirm or refute our findings.
The purpose of this study was to examine the trends in the expenditure and utilization of chiropractic care in a representative sample of children and adolescents in the United States (US) aged <18 years.
The researchers evaluated serial cross-sectional data (2007-2016) from the Medical Expenditure Panel Survey. Weighted descriptive statistics were conducted to derive national estimates of expenditure and utilization, and linear regression was used to determine trends over time. Sociodemographic and clinical characteristics of chiropractic users were also reported.
A statistically significant increasing trend was observed for the number of children receiving chiropractic care (P <.05) and chiropractic utilization rate (P < .05). Increases in chiropractic expenditure and the number of chiropractic visits were also observed over time but were not statistically significant (P > .05). The mean annual number of visits was 6.4 visits, with a mean expenditure of $71.49 US dollars (USD) per visit and $454.08 USD per child. Children and adolescent chiropractic users in the United States were primarily 14 to 17 years old (39.6%-61.6%), White (71.5%-76.9%), male (50.6%-51.3%), and privately insured (56.7%-60.8%). Chiropractic visits in this population primarily involved low back conditions (52.4%), spinal curvature (14.0%), and head and neck complaints (12.8%).
The authors concluded that the number of children visiting a chiropractor and percent utilization showed a statistically significant, increasing trend from 2007 to 2016; however, total expenditure and the number of chiropractic visits did not significantly differ during this period. These findings provide novel insight into the patterns of chiropractic utilization in this understudied age group.
Why are these numbers increasing?
Is it because of increasing and sound evidence showing that chiropractors do more good than harm to kids?
No!
A recent systematic review of the evidence for effectiveness and harms of specific spinal manipulation therapy (SMT) techniques for infants, and children suggests the opposite.
Its authors searched electronic databases up to December 2017. Controlled studies, describing primary SMT treatment in infants (<1 year) and children/adolescents (1–18 years), were included to determine effectiveness. Controlled and observational studies and case reports were included to examine harms. One author screened titles and abstracts and two authors independently screened the full text of potentially eligible studies for inclusion. Two authors assessed the risk of bias in included studies and the quality of the body of evidence using the GRADE methodology. Data were described according to PRISMA guidelines and CONSORT and TIDieR checklists. If appropriate, a random-effects meta-analysis was performed.
Of the 1,236 identified papers, 26 studies were eligible. In all but 3 studies, the therapists were chiropractors. Infants and children/adolescents were treated for various (non-)musculoskeletal indications, hypothesized to be related to spinal joint dysfunction. Studies examining the same population, indication, and treatment comparison were scarce. Due to very low-quality evidence, it is uncertain whether gentle, low-velocity mobilizations reduce complaints in infants with colic or torticollis, and whether high-velocity, low-amplitude manipulations reduce complaints in children/adolescents with autism, asthma, nocturnal enuresis, headache or idiopathic scoliosis. Five case reports described severe harms after HVLA manipulations in 4 infants and one child. Mild, transient harms were reported after gentle spinal mobilizations in infants and children and could be interpreted as a side effect of treatment.
The authors concluded that, based on GRADE methodology, we found the evidence was of very low quality; this prevented us from drawing conclusions about the effectiveness of specific SMT techniques in infants, children and adolescents. Outcomes in the included studies were mostly parent or patient-reported; studies did not report on intermediate outcomes to assess the effectiveness of SMT techniques in relation to the hypothesized spinal dysfunction. Severe harms were relatively scarce, poorly described and likely to be associated with underlying missed pathology. Gentle, low-velocity spinal mobilizations seem to be a safe treatment technique in infants, children and adolescents. We encourage future research to describe effectiveness and safety of specific SMT techniques instead of SMT as a general treatment approach.
But chiros do more than just SMT, I hear some say.
Yes, they do!
But they nevertheless manipulate virtually every patient, and the additional treatments they use are merely borrowed from other disciplines.
So, why are the numbers increasing then?
I suggest this as a main reason:
chiropractors are systematically misleading the public about the value of their trade.
Due to polypharmacy combined with the rising popularity of so-called alternative medicines (SCAM), oncology patients are at particular risk of drug-drug interactions (DDI) or herb-drug interactions (HDI). Caution is therefore indicated.
The aims of this study were to assess DDI and HDI in outpatients taking oral anticancer drugs.
All prescribed and non-prescribed medications, including SCAM, were prospectively collected by hospital pharmacists during a structured interview with the patient. DDI and HDI were analyzed using four interaction software programs: Thériaque®, Drugs.com®, Hédrine, and Memorial Sloan Kettering Cancer Center (MSKCC) database. All detected interactions were characterized by severity, risk, and action mechanism. The need for pharmaceutical intervention to modify drug use was determined on a case-by-case basis.
294 patients were included, with a mean age of 67 years. The median number of chronic drugs per patient was 8 [1-29] and 55% of patients used at least one SCAM. At least 0ne interaction was found for 267 patients (90.8%): 263 (89.4%) with DDI, 68 (23.1%) with HDI, and 64 (21.7%) with both DDI and HDI. Only 13% of the DDI were found in Thériaque® and Drugs.com® databases, and 125 (2.5%) were reported with a similar level of risk on both databases. 104 HDI were identified with only 9.5% of the interactions found in both databases. 103 pharmaceutical interventions were performed, involving 61 patients (20.7%).
The authors concluded that potentially clinically relevant drug interactions were frequently identified in this study, showing that several databases and structured screening are required to detect more interactions and optimize medication safety.
This figure of potential HDIs is high – much higher than in most previous studies. A possible explanation could be that the study was carried out in France where the use of herbal remedies is considerable. As some HDIs can cause serious problems for patients, my advice is to think twice about using herbal remedies while taking prescription drugs. I think this advice is sound regardless of whether someone is suffering from cancer or any other condition.
It has been reported by several outlets that a young woman is fighting for her life after a chiropractic adjustment went horribly wrong. Caitlin Jensen had only recently graduated from University. When she went for what was meant to be a simple chiropractic adjustment on June 16, she suffered four dissected arteries in her neck, this damage led to cardiac arrest, stroke and her being without a pulse for over 10 minutes, requiring resuscitation.
She was rushed to the Memorial Hospital in Savannah, Georgia, where she was operated on. She was then taken to the neuro ICU in a critical condition with a traumatic brain injury. Every day since she’s been fighting. Currently, she is conscious and able to respond to verbal commands by blinking her eyes, as well as wiggling the toes of her left foot. However, most of her body remains paralyzed.
Her mother Darlene has been posting updates about her daughter’s condition on Facebook. On Saturday Darlene shared the latest news on the condition of her daughter. “She gave her best effort to smile today, and it was the most beautiful thing I’ve ever seen,” Darlene said. “She is progressing with her movements on the left side – wiggling and flexing. She can’t lift her arm yet, or turn her head. Her right side is unchanged – still no movement. Her face doesn’t move very much yet, but she can open her eyes widely to show surprise, and the left corner of her mouth tries to smile. Adorable. Still working on the pneumonia. The antiplatelet therapy seems to be going OK. We don’t see any signs of internal bleeding and are praying that it stays that way.”
And the day before, Darlene posted: “Two weeks ago tonight we didn’t know if Caitlin would make it through the night,” Darlene said. “Dire and catastrophic are two of the words that we heard from our ICU team. We knew they didn’t casually throw around words like that. But – she is alive, and every day is a little better. The accomplishments are both small and monumental at the same time. Today, she gave us a thumbs up. We have been working on this, and she got it! She also nodded again today. It helps to see these things because it reassures us that she is working hard to stay with us and recover. Caitlin is strong, disciplined, and well practised in exercising her brain, and I truly believe that her science background and all of her time studying is going to help her in this long journey. “
Studies have found that traumatic cervical artery dissection is one of the leading causes of stroke in patients under the age of 45, and recent chiropractic neck manipulation is among factors that can be associated with risk of vertebral artery dissection.
Following the tragedy, Caitlin’s mother, Darlene, launched a GoFundMe and has raised more than US$20,000 (AU $29,334 or £16,512) for her ongoing medical expenses.
It is clear that these news reports lack important medical details. What is equally clear is the fact that most such cases are never reported in the medical literature and are thus available only in this fragmented form. The reason for this lamentable situation is obvious: there is no post-marketing surveillance system for chiropractic (such a safeguard would be bad for business, of course).
Consequently, chiropractors across the globe continue to be able to say that such reports are unreliable. The medical literature, they are keen to point out, holds only very few case studies of serious risks of chiropractic spinal manipulation. Hence they falsely claim on every possible occasion that their adjustments are safe. The end effect is that many consumers continue to wrongly assume that chiropractic manipulations might be worth a try.
Guest post by Björn Geir
I have tried to find a form or type of quackery that can be confirmed to have died out and is no longer practised. Once I thought I had found one, but it turns out that phrenology is still “a thing” and is being practised by a few eccentrics.
I am almost convinced by now that any quackery or SCAM, as Professor Ernst has proposed to call it, never dies. Once someone has invented a SCAM, it will live on forever, like the proverbial zombie, neither dead nor properly alive and useful. Even bloodletting, the archetypical reject from the practice of medicine, is still being practised in some corners of this world. Google “Wet cupping” or “Hijama” if you don’t believe me.
The world will have to live with health-related scam and swindle but its popularity can and should be suppressed and held to an acceptable low. If truth and science are promoted and SCAM is vigilantly and constantly opposed, then public trust in it can be held back and even reversed as now has been shown in Norway.
My somewhat abridged translation of an article published on June 30th on the Norwegian state broadcasting services website.
————
Norwegians have become much more sceptical towards natural medicine
Fifteen years ago, most Norwegians had faith in natural medicine. Not anymore.
– This is dramatic. A total reversal of opinion, says John Spilling of Ipsos, a company that performs an annual survey of public opinion in Norway. About 3500 people have been interviewed every year since 1985.
The survey, called Norwegian Monitor, has shown that the alternative industry had its heyday in the 80´s and 90´s, at least according to the Norwegian population’s confidence in natural medicine.
On average, eight out of ten thought this kind of therapy and naturopaths could help when ordinary doctors had given up.
But after the turn of the millennium, something started to happen.
The confidence plummeted.
A screenshot from the article showing the representation of the annual Norwegian Monitor survey results for the statement: Naturopaths and natural medicine can often help when ordinary doctors and medicine fall short.
The results are represented as follows:
Black – Impossible to answer
Grey – No answer
Dark red – Totally disagree
Light red – Partially disagree
Dark blue – Partially agree
Light blue – Totally agree
The graph in the article is interactive so you can find the individual rates by hovering over the bars in the article online.
This year only three out of ten fully or partially agree that natural medicine and naturopaths can help. Mr. Spilling is surprised by the magnitude of change, which also has been steadily declining instead of the usual ups and downs seen in so many other areas.
– I see almost no parallels, he says.
The patients stopped coming
The article interviews Ms. Hilde Moldestad. A homeopath since many decades, now retired and leads the Norwegian Homeopathic Patient Association.
Ms. Moldestad marked the decline already while practising.
– The patients stopped coming, because the trends were such that no one was to believe that there was anything good about homeopathy.
She also noted a strongly declining interest within the patient association.
– There are less and less members. People are not so interested in being team members anymore, they want it free online.
Ms. Moldestad is determined that homeopathy works.
– The irony is that the more research that shows that homeopathy works, the stronger the opposition to using the method.
The [Norwegian] National Research Center for Alternative Medicine writes that there is no solid evidence that homeopathic medicines have an effect. And both the Norwegian Medicines Agency and the Norwegian Pharmacists’ Association believe that in practice the pills only contain water and sugar.
– But we are up in a paradigm shift. The damage that has been inflicted on humanity during the period in which school medicine has been allowed to dominate, can no longer be undermined, says Ms. Moldestad in the patient association.The article then interviews Mr. Gunnar Tjomlid, an active Norwegian sceptic who talks about some local background stories of local interest and speculates that perhaps this change correlates with the introduction and distribution of internet access in Norway.
Less use
It is not only the Norwegian Monitor survey that shows a decline for the alternative industry. Every two years, the National Research Center for Alternative Medicine (Nafkam) conducts a survey on, among other things, how often Norwegians visit alternative therapists.
– In 2012, you had just under 40 percent who had been to an alternative therapist. And in December 2020, it was 22 percent. So, there has been a declining trend, says Mr. Ola Lillenes, information director at Nafkam.
At the same time, self-treatment, especially with self-help techniques, has increased.
– Healing and homeopathy are probably among those who have fallen the most through these years.
Education and emotions
Jarle Botnen runs the Bø Institute of Natural Medicine in Telemark. In addition, he is part of the steering group in the association of alternative treatment organizations. Over 1000 therapists are affiliated with this organisation which is named Saborg.
– There is a noticeable decline, that is exactly correct, says Botnen.
He has several theories as to why Norwegians have become more sceptical of natural medicine.
Norwegians have received more education and have less trust in their own feelings.
People are used to simple solutions, such as over-the-counter painkillers. They do not treat the cause of the ailments, which takes more time.
It is difficult to distinguish charlatans from the serious [alternative practitioners]. The industry has also not managed to cooperate well enough, according to Botnen.
The pharmaceutical industry has been lobbying to get more of the market for alternative medicine.
The attitude in the media has changed from being positive to natural medicine to often the opposite.
Small brown glass bottles with homeopathic pills lie in a drawer in a pharmacy.
Sales of homeopathic medicines have declined at the same time as Norwegians have become more sceptical of natural medicine.
– We often hear remarks such as “we trust the authorities”, “the authorities have approved the preparation or treatment”. This is reflected in the consumption of chemical and synthetic medicine, which has increased somewhat formidably during this period, Botnen believes.
John Spilling in Ipsos says it is true that people have great confidence in the public sector. Confidence in hospitals and elderly care has also increased, while the alternative industry has had the opposite development.
– Most of Norway’s population does not trust this type of product. I can only understand that the situation of this industry is very different than in 2001.
End of article————-
These are indeed positive and convincing results. I suspect a similar trend has been happening in most other populations? It would be very interesting to know if a similar trend has been observed elsewhere.
A study by an international team of researchers estimated the proportion of healthcare interventions tested within Cochrane Reviews that are effective according to high-quality evidence.
They selected a random sample of 2428 (35%) of all Cochrane Reviews published between 1 January 2008 and 5 March 2021 and extracted data about interventions within these reviews that were compared with placebo, or no treatment, and whose outcome quality was rated using Grading of Recommendations Assessment, Development and Evaluation (GRADE). They then calculated the proportion of interventions whose effectiveness was based on high-quality evidence according to GRADE, had statistically significant positive effects and were judged as beneficial by the review authors. They also calculated the proportion of interventions that suggested harm.
Of 1567 eligible interventions, 87 (5.6%) had high-quality evidence on first-listed primary outcomes, positive, statistically significant results, and were rated by review authors as beneficial. Harms were measured for 577 (36.8%) interventions, 127 of which (8.1%) had statistically significant evidence of harm. Our dependence on the reliability of Cochrane author assessments (including their GRADE assessments) was a potential limitation of our study. 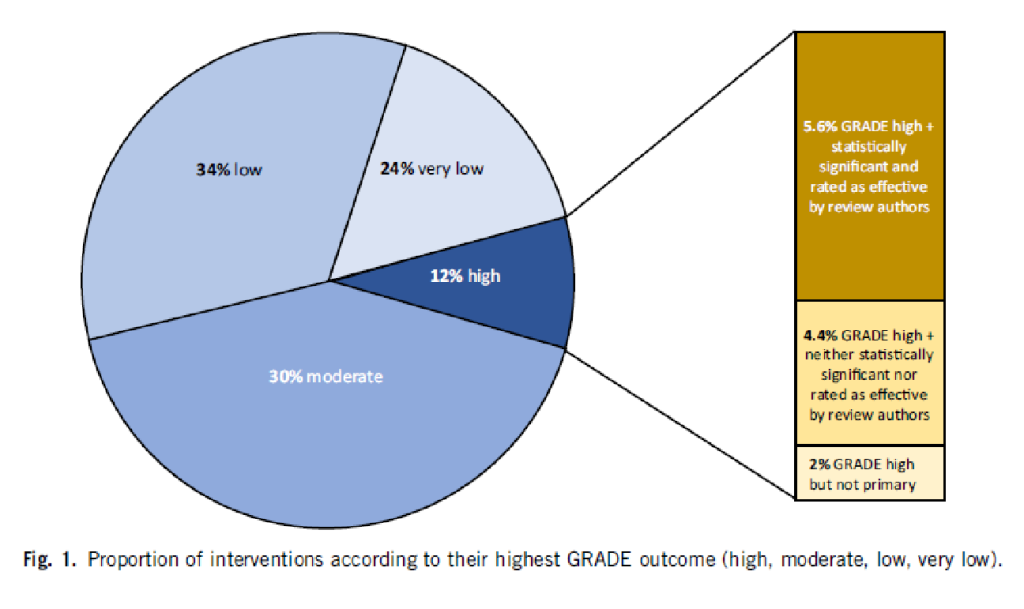
The authors drew the following conclusions: While many healthcare interventions may be beneficial, very few have high-quality evidence to support their effectiveness and safety. This problem can be remedied by high-quality studies in priority areas. These studies should measure harms more frequently and more rigorously. Practitioners and the public should be aware that many frequently used interventions are not supported by high-quality evidence.
Proponents of so-called alternative medicine (SCAM) are fond of the ‘strawman’ fallacy; meaning they like to present a picture of conventional medicine that is overtly negative in order for SCAM to appear more convincing (Prince Charles, for instance, uses this trick every single time he speaks about SCAM). Therefore I am amazed that this paper has not been exploited in that way by them. I was expecting headlines such as
Evidence-based medicine is not supported by evidence
or
Less than 6% of all conventional treatments are supported by sound evidence.
etc.
Why did they not have a field day with this new paper then?
As the article is behind a paywall, it took me a while to get the full paper (thanks Paul). Now that I have read it, I think I understand the reason.
In the article, the authors provide figures for specific types of treatments. Let me show you some of the percentages of interventions that met the primary outcome (high quality, statistically significant effect, and authors interpret as effective):
- pharmacological 73.8%
- surgical 4.6%
- exercise 5.8%
- diet 1.2%
- alternative 0.0%
- manual therapies 0.0%
So, maybe the headlines should not be any of the above but:
No good evidence to support SCAM?
or
SCAM is destroying the evidence base of medicine.
An epidemiological study from the US just published in the BMJ concluded that “the mortality gap in Republican voting counties compared with Democratic voting counties has grown over time, especially for white populations, and that gap began to widen after 2008.”
In a BMJ editorial, Steven Woolf comments on the study and provides further evidence on how politics influence health in the US. Here are his concluding two paragraphs:
Political influence on US mortality rates became overt during the covid-19 pandemic, when public health policies, controlled by states, were heavily influenced by party affiliation. Republican politicians, often seeking to appeal to President Trump and his supporters, challenged scientific evidence and opposed enforcement of vaccinations and safety measures such as masking. A macabre natural experiment occurred in 2021, a year marked by the convergence of vaccine availability and contagious variants that threatened unvaccinated populations: states led by governors who promoted vaccination and mandated pandemic control measures experienced much lower death rates than the “control” group, consisting of conservative states with lax policies and large unvaccinated populations. This behavior could explain why US mortality rates associated with covid-19 were so catastrophic, vastly exceeding losses in other high income countries.
Observers of health trends in the US should keep their eye on state governments, where tectonic shifts in policy are occurring. While gridlock in Washington, DC incapacitates the federal government, Republican leaders in dozens of state capitols are passing laws to undermine health and safety regulations, ban abortion, limit LGBT+ rights, and implement more conservative policies on voting, school curriculums, and climate policy. To understand the implications for population health, researchers must break with custom; although scientific literature has traditionally avoided discussing politics, the growing influence of partisan affiliation on policies affecting health makes this covariate an increasingly important subject of study.
_____________________
What has this to do with so-called alternative medicine (SCAM)?
Not a lot.
Except, of course, that Trump has been quite sympathetic to both quackery and quacks (see, for instance, here and here). Moreover, the embarrassing Dr. Oz, America’s charlatan-in-chief, is now a Republican candidate for the US senate. And the creation of the NHI office for alternative medicine, currently called NCCIH, was the idea of the Republican senator, Tom Harkin.
I think we get the drift: on the US political level, SCAM seems to be a right-wing thing.
Am I claiming that SCAM is the cause of the higher mortality in Republican counties?
No.
Do I feel that both are related to irresponsible attitudes towards healthcare issues?
Yes.
It seems that no ancient treatment is daft enough for some researchers of so-called alternative medicine (SCAM) to not pick it up. Even bloodletting is back, it seems!
The aim of this study was to investigate the effects of therapeutic phlebotomy on ambulatory blood pressure in patients with grade 1 hypertension. In this randomized-controlled intervention study, patients with unmedicated hypertension grade 1 were randomized into an intervention group (phlebotomy group; 500 mL bloodletting at baseline and after 6 weeks) and a control group (waiting list) and followed up for 8 weeks. The primary endpoint was the 24-h ambulatory mean arterial pressure between the intervention and control groups after 8 weeks. Secondary outcome parameters included ambulatory/resting systolic/diastolic blood pressure, heart rate, and selected laboratory parameters (e.g., hemoglobin, hematocrit, erythrocytes, and ferritin). Resting systolic/diastolic blood pressure/heart rate and blood count were also assessed at 6 weeks before the second phlebotomy to ensure safety. A per-protocol analysis was performed.
Fifty-three hypertension participants (56.7 ± 10.5 years) were included in the analysis (n = 25 intervention group, n = 28 control group). The ambulatory measured mean arterial pressure decreased by -1.12 ± 5.16 mmHg in the intervention group and increased by 0.43 ± 3.82 mmHg in the control group (between-group difference: -1.55 ± 4.46, p = 0.22). Hemoglobin, hematocrit, erythrocytes, and ferritin showed more pronounced reductions in the intervention group in comparison with the control group, with significant between-group differences. Subgroup analysis showed trends regarding the effects on different groups classified by serum ferritin concentration, body mass index, age, and sex. Two adverse events (AEs) (anemia and dizziness) occurred in association with the phlebotomy, but no serious AEs.
The authors concluded that therapeutic phlebotomy resulted in only minimal reductions of 24-h ambulatory blood pressure measurement values in patients with unmedicated grade 1 hypertension. Further high-quality clinical studies are warranted, as this finding contradicts the results of other studies.
This paper requires a few short comments:
- The effect on blood pressure was not ‘minimal’, as the authors pretend, it was non-existent (i.e. not significant and due to chance only).
- This lack of effect had to be expected considering human physiology.
- The fact that hemoglobin, hematocrit, erythrocytes, and ferritin all change after bloodletting is equally expected.
- Mild adverse effects are also no surprise.
- What is a surprise, however, that such a trial was ever conducted and passed by an ethics committee. Any medic who has not slept through his/her cardiovascular physiology lectures could have predicted the results quite accurately. And running a trial where the result is well-known before the study has started can hardly be called ethical.
Nausea and vomiting are common symptoms of patients with advanced cancer. While there is some evidence for acupuncture point stimulation in the treatment of these symptoms for patients having anticancer treatment, there is little for when they are not related to such treatment.
This study aimed to determine whether acupressure at the pericardium 6 sites can help treat nausea and vomiting suffered by palliative care patients with advanced cancer. The researchers conducted a double-blind randomized controlled trial-active versus placebo acupressure wristbands. In-patients with advanced cancer in two specialist palliative care units who fitted either or both of the following criteria were approached: nausea that was at least of moderate severity; vomiting daily on average for the prior 3 days.
A total of 57 patients were randomized to have either active or placebo acupressure wristbands. There was no difference in any of the outcome measures between the two groups:
- change from the baseline number of vomits;
- Visual Analogue Scale for ‘did acupressure wristbands help you to feel better?’;
- the total number of doses of antiemetic medication;
- the need for escalation of antiemetics.
The authors concluded that, in contrast to a previously published feasibility study, active acupressure wristbands were no better than placebo for specialist palliative care in patients with advanced cancer and nausea and vomiting.
When the research into acupuncture for nausea and vomiting began some 20 years ago, the evidence turned out to be encouraging. Later, as the studies became more and more rigorous, many trials failed to confirm the initial findings. Today, the totality of the evidence is far less convincing than it seemed years ago.
This is a phenomenon that can be observed not just in acupuncture research but in many types of treatment:
- Initially, over-enthusiastic researchers become victims of their own optimism.
- These investigators are less into testing hypotheses than into confirming their own wishful thinking.
- Thus, several positive trials emerge.
- These, however, turn out to be methodologically flawed.
- Eventually, the subject might be picked up by real scientists who truly test hypotheses.
- More and more negative studies thus emerge.
- Depending on how many flawed studies were initially published and how critical the authors of systematic reviews are, it can take years until the totality of the evidence depicts the true picture which discloses the initial findings as false-positive.
The message is, I think, clear: poor quality studies have the potential to mislead us for many years. Eventually, however, the self-cleansing ability of science should generate the truth about the value of any treatment. In other words:
poor-quality science is not just useless, it causes long-term harm
and
critical thinking prevents harm


