conflict of interest
Well-conducted systematic reviews (SRs) should in principle provide the most reliable evidence on the effectiveness of acupuncture. However, limitations on the methodological rigour of SRs may impact the trustworthiness of their conclusions. This cross-sectional study was aimed at evaluating the methodological quality of recent SRs of acupuncture.
The Cochrane Database of Systematic Reviews, MEDLINE, and EMBASE were searched for SRs focusing on manual acupuncture or electro-acupuncture published during January 2018 and March 2020. Eligible SRs needed to contain at least one meta-analysis and be published in the English language. Two independent reviewers extracted the bibliographical characteristics of the included SRs with a pre-designed questionnaire and appraised the methodological quality of the reviews with the validated AMSTAR 2 (A MeaSurement Tool to Assess systematic Reviews 2). The associations between bibliographical characteristics and methodological quality ratings were explored using Kruskal-Wallis rank tests and Spearman’s rank correlation coefficients.
A total of 106 SRs were appraised. The results were as follows:
- one (0.9%) SR was of high methodological quality,
- no review (0%) was of moderate quality,
- six (5.7%) were of low quality,
- 99 (93.4%) were of critically low quality.
Only ten (9.4%) provided an a priori protocol, only four (3.8%) conducted a comprehensive literature search, only five (4.7%) provided a list of excluded studies, and only six (5.7%) performed a meta-analysis appropriately. Cochrane SRs, updated SRs, and SRs that did not search non-English databases had relatively higher overall quality. The vast majority (87.7%) of the 106 reviews included in this analysis originated from Asia. Conflicts of interest of the review authors were declared in only 2 of the 106 reviews.
The authors concluded that the methodological quality of SRs on acupuncture is unsatisfactory. Future reviewers should improve critical methodological aspects of publishing protocols, performing comprehensive search, providing a list of excluded studies with justifications for exclusion, and conducting appropriate meta-analyses. These recommendations can be implemented via enhancing the technical competency of reviewers in SR methodology through established education approaches as well as quality gatekeeping by journal editors and reviewers. Finally, for evidence users, skills in SR critical appraisal remain to be essential as relevant evidence may not be available in pre-appraised formats.
On this blog, I have often complained about the lack of critical input and the poor quality of systematic reviews of so-called alternative medicine (SCAM), particularly of acupuncture, and especially of Chinese reviews, and even more especially Chinese reviews of (mostly) Chinese studies. This new paper is a valuable confirmation of this fast-growing deficit.
One does not need to be a prophet to predict that this pollution of the literature with complete rubbish will have detrimental effects. Because poor reviews almost always draw an over-optimistic picture of the value of acupuncture, this phenomenon must seriously mislead the public. The end result will be that the public believes acupuncture to be effective.
I cannot help thinking that this is, in fact, the intended aim of the authors of such poor, false-positive reviews. Moreover, a glance at the subject areas of the reviews in the list below gives the impression that China is heavily promoting the idea that acupuncture is a panacea. Yet there is good evidence to show that acupuncture is little more than placebo therapy.
In my last post, I have reported that I am an author of many of the frequently-cited systematic acupuncture reviews. You might thus assume that I am a significant part of this pollution by rubbish reviews. This would, however, be an entirely wrong conclusion. The above analysis covers a period when my unit had already been closed, and I am thus not responsible for a single of the papers included in the above analysis.
List of included systematic reviews
| ID | Included systematic reviews |
| 1 | Acupuncture for primary insomnia: An updated systematic review of randomized controlled trials |
| 2 | Efficacy and safety of acupuncture for essential hypertension: A meta-analysis |
| 3 | Acupuncture for the treatment of sudden sensorineural hearing loss: A systematic review and meta-analysis: Acupuncture for SSNHL |
| 4 | Effectiveness of Acupuncturing at the Sphenopalatine Ganglion Acupoint Alone for Treatment of Allergic Rhinitis: A Systematic Review and Meta-Analysis |
| 5 | Acupuncture and clomiphene citrate for anovulatory infertility: a systematic review and meta-analysis |
| 6 | Acupuncture for primary trigeminal neuralgia: A systematic review and PRISMA-compliant meta-analysis |
| 7 | Acupuncture as an adjunctive treatment for angina due to coronary artery disease: A meta-analysis |
| 8 | Conventional treatments plus acupuncture for asthma in adults and adolescent: A systematic review and meta-analysis |
| 9 | Optimizing acupuncture treatment for dry eye syndrome: A systematic review |
| 10 | Acupuncture using pattern-identification for the treatment of insomnia disorder: a systematic review and meta-analysis of randomized controlled trials |
| 11 | Efficacy and Safety of Auricular Acupuncture for Cognitive Impairment and Dementia: A Systematic Review |
| 12 | Acupuncture for cognitive impairment in vascular dementia, alzheimer’s disease and mild cognitive impairment: A systematic review and meta-analysis |
| 13 | Effectiveness of pharmacopuncture for cervical spondylosis: A systematic review and meta-analysis |
| 14 | Acupuncture combined with swallowing training for poststroke dysphagia: a meta-analysis of randomised controlled trials |
| 15 | Scalp acupuncture treatment for children’s autism spectrum disorders: A systematic review and meta-analysis |
| 16 | Acupuncture for Post-stroke Shoulder-Hand Syndrome: A systematic review and meta-analysis |
| 17 | Systematic review of acupuncture for the treatment of alcohol withdrawal syndrome |
| 18 | Acupuncture for hip osteoarthritis |
| 19 | Clinical Benefits of Acupuncture for the Reduction of Hormone Therapy-Related Side Effects in Breast Cancer Patients: A Systematic Review |
| 20 | Combination therapy of scalp electro-acupuncture and medication for the treatment of Parkinson’s disease: A systematic review and meta-analysis |
| 21 | Acupuncture for migraine: A systematic review and meta-analysis |
| 22 | Acupuncture to Promote Recovery of Disorder of Consciousness after Traumatic Brain Injury: A Systematic Review and Meta-Analysis |
| 23 | Acupuncture Compared with Intramuscular Injection of Neostigmine for Postpartum Urinary Retention: A Systematic Review and Meta-Analysis of Randomized Controlled Trials |
| 24 | Acupuncture for the relief of hot flashes in breast cancer patients: A systematic review and meta-analysis of randomized controlled trials and observational studies |
| 25 | Effectiveness and Safety of Acupuncture for Perimenopausal Depression: A Systematic Review and Meta-Analysis of Randomized Controlled Trials |
| 26 | Acupuncture plus Chinese Herbal Medicine for Irritable Bowel Syndrome with Diarrhea: A Systematic Review and Meta-Analysis |
| 27 | Electroacupuncture as an adjunctive therapy for motor dysfunction in acute stroke survivors: A systematic review and meta-analyses |
| 28 | Acupuncture for Acute Pancreatitis: A Systematic Review and Meta-analysis |
| 29 | Acupuncture for chronic fatigue syndrome: a systematic review and meta-analysis |
| 30 | Compare the efficacy of acupuncture with drugs in the treatment of Bell’s palsy: A systematic review and meta-analysis of RCTs |
| 31 | The effectiveness and safety of acupuncture for the treatment of myasthenia gravis: a systematic review and meta-analysis of randomized controlled trials |
| 32 | Acupuncture therapy for fibromyalgia: A systematic review and meta-analysis of randomized controlled trials |
| 33 | The effectiveness of acupuncture therapy in patients with post-stroke depression: An updated meta-analysis of randomized controlled trials |
| 34 | Fire needling for herpes zoster: A systematic review and meta-analysis of randomized clinical trials |
| 35 | Comparison between the Effects of Acupuncture Relative to Other Controls on Irritable Bowel Syndrome: A Meta-Analysis |
| 36 | Manual Acupuncture for Optic Atrophy: A Systematic Review and Meta-Analysis |
| 37 | Effect of warm needling therapy and acupuncture in the treatment of peripheral facial paralysis: A systematic review and meta-analysis |
| 38 | The Effect of Acupuncture in Breast Cancer-Related Lymphoedema (BCRL): A Systematic Review and Meta-Analysis |
| 39 | The Efficacy of Acupuncture in Chemotherapy-Induced Peripheral Neuropathy: Systematic Review and Meta-Analysis |
| 40 | The maintenance effect of acupuncture on breast cancer-related menopause symptoms: a systematic review |
| 41 | The effectiveness of acupuncture in the management of persistent regional myofascial head and neck pain: A systematic review and meta-analysis |
| 42 | Acupuncture for the Treatment of Adults with Posttraumatic Stress Disorder: A Systematic Review and Meta-Analysis |
| 43 | The effectiveness of superficial versus deep dry needling or acupuncture for reducing pain and disability in individuals with spine-related painful conditions: a systematic review with meta-analysis |
| 44 | Effects of dry needling trigger point therapy in the shoulder region on patients with upper extremity pain and dysfunction: a systematic review with meta-analysis |
| 45 | Is dry needling effective for low back pain?: A systematic review and PRISMA-compliant meta-analysis |
| 46 | The effectiveness and safety of acupuncture for patients with atopic eczema: a systematic review and meta-analysis |
| 47 | Comparing verum and sham acupuncture in fibromyalgia syndrome: a systematic review and meta-analysis |
| 48 | Acupuncture for symptomatic gastroparesis |
| 49 | The Efficacy and Safety of Acupuncture for the Treatment of Children with Autism Spectrum Disorder: A Systematic Review and Meta-Analysis |
| 50 | Acupuncture Versus Sham-acupuncture: A Meta-analysis on Evidence for Non-immediate Effects of Acupuncture in Musculoskeletal Disorders |
| 51 | Acupuncture Treatment for Post-Stroke Dysphagia: An Update Meta-Analysis of Randomized Controlled Trials |
| 52 | Effectiveness of Acupuncture Used for the Management of Postpartum Depression: A Systematic Review and Meta-Analysis |
| 53 | Clinical effects and safety of electroacupuncture for the treatment of post-stroke depression: a systematic review and meta-analysis of randomised controlled trials |
| 54 | Placebo effect of acupuncture on insomnia: a systematic review and meta-analysis |
| 55 | Acupuncture for Chronic Pain-Related Insomnia: A Systematic Review and Meta-Analysis |
| 56 | Evidence for Dry Needling in the Management of Myofascial Trigger Points Associated With Low Back Pain: A Systematic Review and Meta-Analysis |
| 57 | Warm needle acupuncture in primary osteoporosis management: a systematic review and meta-analysis |
| 58 | Acupuncture for overactive bladder in adults: a systematic review and meta-analysis |
| 59 | Traditional acupuncture for menopausal hot flashes: A systematic review and meta-analysis of randomized controlled trials |
| 60 | The effectiveness of acupuncture for osteoporosis: A systematic review and meta-analysis |
| 61 | Long-term effects of acupuncture for chronic prostatitis/chronic pelvic pain syndrome: Systematic review and single-Arm meta-Analyses |
| 62 | Does acupuncture the day of embryo transfer affect the clinical pregnancy rate? Systematic review and meta-analysis |
| 63 | Acupuncture treatments for infantile colic: a systematic review and individual patient data meta-analysis of blinding test validated randomised controlled trials |
| 64 | Acupuncture performed around the time of embryo transfer: a systematic review and meta-analysis |
| 65 | Is Acupuncture Effective for Improving Insulin Resistance? A Systematic Review and Meta-analysis |
| 66 | Efficacy of acupuncture in the management of post-apoplectic aphasia: A systematic review and meta-analysis of randomized controlled trials |
| 67 | Acupuncture for lumbar disc herniation: a systematic review and meta-analysis |
| 68 | Traditional Chinese acupuncture and postpartum depression: A systematic review and meta-analysis |
| 69 | Acupuncture for Chronic Pain: Update of an Individual Patient Data Meta-Analysis |
| 70 | Acupuncture Therapy for Functional Effects and Quality of Life in COPD Patients: A Systematic Review and Meta-Analysis |
| 71 | Electroacupuncture for Reflex Sympathetic Dystrophy after Stroke: A Meta-Analysis |
| 72 | The Effect of Patient Characteristics on Acupuncture Treatment Outcomes |
| 73 | The efficacy and safety of acupuncture in women with primary dysmenorrhea: A systematic review and meta-analysis |
| 74 | Role of acupuncture in the treatment of insulin resistance: A systematic review and meta-analysis |
| 75 | Appropriateness of sham or placebo acupuncture for randomized controlled trials of acupuncture for nonspecific low back pain: A systematic review and meta-analysis |
| 76 | Evidence of efficacy of acupuncture in the management of low back pain: a systematic review and meta-analysis of randomised placebo- or sham-controlled trials |
| 77 | The effects of acupuncture on pregnancy outcomes of in vitro fertilization: A systematic review and meta-analysis |
| 78 | Acupuncture for migraine without aura: a systematic review and meta-analysis |
| 79 | Acupuncture for acute stroke |
| 80 | Acupuncture at Tiaokou (ST38) for Shoulder Adhesive Capsulitis: What Strengths Does It Have? A Systematic Review and Meta-Analysis of Randomized Controlled Trials |
| 81 | Acupuncture for hypertension |
| 82 | The effect of acupuncture on Bell’s palsy: An overall and cumulative meta-analysis of randomized controlled trials |
| 83 | Effects of acupuncture on cancer-related fatigue: a meta-analysis |
| 84 | Acupuncture for adults with overactive bladder |
| 85 | Electroacupuncture for Postoperative Urinary Retention: A Systematic Review and Meta-Analysis |
| 86 | Meta-Analysis of Electroacupuncture in Cardiac Anesthesia and Intensive Care |
| 87 | Acupuncture therapy improves health-related quality of life in patients with chronic obstructive pulmonary disease: A systematic review and meta-analysis |
| 88 | The effect of acupuncture on the quality of life in patients with migraine: A systematic review and meta-analysis |
| 89 | Cognitive improvement effects of electro-acupuncture for the treatment of MCI compared with Western medications: A systematic review and Meta-analysis 11 Medical and Health Sciences 1103 Clinical Sciences |
| 90 | Oriental herbal medicine and moxibustion for polycystic ovary syndrome: A meta-analysis |
| 91 | The Effect of Acupuncture and Moxibustion on Heart Function in Heart Failure Patients: A Systematic Review and Meta-Analysis |
| 92 | Acupuncture therapy for the treatment of stable angina pectoris: An updated meta-analysis of randomized controlled trials |
| 93 | Traditional manual acupuncture combined with rehabilitation therapy for shoulder hand syndrome after stroke within the Chinese healthcare system: a systematic review and meta-analysis |
| 94 | Effects of moxibustion on pain behaviors in patients with rheumatoid arthritis: A meta-analysis |
| 95 | Acupuncture Treatment for Chronic Pelvic Pain in Women: A Systematic Review and Meta-Analysis of Randomized Controlled Trials |
| 96 | The effectiveness of dry needling for patients with orofacial pain associated with temporomandibular dysfunction: a systematic review and meta-analysis |
| 97 | Acupuncture for postherpetic neuralgia systematic review and meta-analysis |
| 98 | Acupoint selection for the treatment of dry eye: A systematic review and meta-analysis of randomized controlled trials |
| 99 | Warm-needle moxibustion for spasticity after stroke: A systematic review of randomized controlled trials |
| 100 | Acupuncture for menstrual migraine: a systematic review |
| 101 | The efficacy of acupuncture for stable angina pectoris: A systematic review and meta-analysis |
| 102 | Acupuncture and weight loss in Asians: A PRISMA-compliant systematic review and meta-analysis |
| 103 | Effects of Acupuncture on Breast Cancer-Related lymphoedema: A Systematic Review and Meta-Analysis |
| 104 | Acupuncture for infertile women without undergoing assisted reproductive techniques (ART): A systematic review and meta-analysis |
| 105 | Moxibustion for alleviating side effects of chemotherapy or radiotherapy in people with cancer |
| 106 | Acupuncture for stable angina pectoris: A systematic review and meta-analysis |
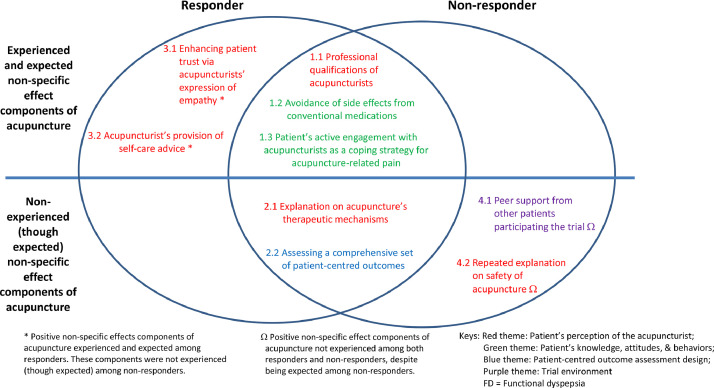
The non-specific effects constitute part of the overall effect of acupuncture. It is unclear whether responders and non-responders of acupuncture experience non-specific effects differently. This analysis aimed to compare their experiences in a nested qualitative study embedded in an acupuncture trial on functional dyspepsia.
Purposive sampling was used to capture the experience of responders (n=15) and non-responders (n=15) to acupuncture via individual in-depth interviews. Design and analysis followed a framework analysis approach, with reference to an existing model on acupuncture non-specific effects. Themes emerging outside of this model were purposefully explored.
The findings suggest that responders had a more trusting relationship with the acupuncturist in response to their expression of empathy. In turn, they were more actively engaged in lifestyle modifications and dietary advice offered by acupuncturists. Non-responders were not satisfied with the level of reassurance regarding acupuncture safety. They were also expecting more peer support from fellow participants, regarded that as an empowerment process for initiating and sustaining lifestyle changes.
The authors concluded that our results highlighted key differences in acupuncture non-specific effect components experienced by responders and non-responders. Positive non-specific effects contributing to overall benefits could be enhanced by emphasizing on empathy expression from acupuncturists, trust-building, offering appropriate explanations on safety, and organizing patient support groups. Further research on the relative importance of each component is warranted.
I doubt that this tiny study lends itself to drawing any firm conclusions. However, what they seem to imply and what the authors (proponents of acupuncture) ignore totally is the following: acupuncture responders are those people who respond to the context of the treatment situation. Thus their positive result is not due to the specific effects of acupuncture itself but to non-specific effects. In other words, acupuncture operates predominantly or entirely via non-specific effects. Or, to put it bluntly: this analysis confirms what we have discussed many times before (see for instance here, here, and here), namely that
acupuncture is a placebo therapy.
The 13th European Congress for Integrative Medicine is about to take place online between 4 and 7 November 2021. It will host 125+ speakers presenting from around the world. The programme will cover the following topics.
- Anthroposophic Medicine
- Arts in Healthcare
- Acupuncture
- Antimicrobial Resistance
- Ayurveda
- Covid Research
- Diabetes
- Homeopathy
- Immunology
- Integrative Oncology
- Lifestyle Medicine
- Medical Education
- Mental Health & Stress Management
- Mind and Body Connection
- Mistletoe Therapy
- Nutrition, Gut Health & Microbiome
- Pain Management
- Patient Activation & Self-Management
- Planetary & Environmental Health
- Research and Evaluation
- Social Prescribing
- Traditional Health
- Yoga
Even looking at the more detailed list of lectures, I did not find a single contribution on conventional medicine (“Integrative medicine combines conventional medicine with…” [see below]) or a lecture that is remotely critical of integrative medicine. The definition of INTEGRATED MEDICINE (IM) adopted here seems similar to the US definition we recently discussed. Here is the European definition:
Integrative medicine combines conventional medicine with evidence-informed complementary medicine and therapies to achieve the optimum health and wellbeing of the patient. Focusing on a holistic, patient-centred approach to healthcare, it takes into consideration the patient’s physical and psychological wellbeing and treats the whole person rather than just the disease.
Allow me to do a quick analysis of this definition by looking at its key elements:
- Evidence-informed: While proper medicine is BASED on evidence, IM is merely INFORMED by it. The difference is fundamental. It allows IM clinicians to use any un- or disproven so-called alternative medicine (SCAM) they can think of or invent. The evidence for homeopathy fails to show that it is effective? Never mind, IM does not need to be evidence-based, it is evidence-informed. IM physicians know homeopathy is a placebo therapy (if not they would be ill-informed which would make them unethical), but they nevertheless use homeopathy (try to find an IM clinic that does not offer homeopathy!), because IM is not EBM. IM is evidence-informed!
- Therapies that achieve optimum health and wellbeing. This is odd because the website also states that “therapies can include anything from acupuncture, yoga, massage, aromatherapy, herbal medicine, nutrition, exercise along with many more approaches, tailored to the needs of the individual” indicating that virtually anything can be included. Anyway, “optimum health and wellbeing” seems a strange and unachievable criterion. In fact, it is nothing but a ‘bait and switch‘ salesmen’s trick.
- Holistic: This is a little trick that IM proponents love. With it, they imply that normal medicine is not holistic. However, this implication is demonstrably wrong. Any good medicine is holistic, and if a sector of healthcare fails to account for the whole person, we need to reform it. (Here are the conclusions of an editorial I published in 2007 entitled ‘Holistic heath care?‘: good health care is likely to be holistic but holistic health care, as it is marketed at present, is not necessarily good. The term ‘holistic’ may even be a ‘red herring’ which misleads patients. What matters most is whether or not any given approach optimally benefits the patient. This goal is best achieved with effective and safe interventions administered humanely — regardless of what label we put on them.) Creating a branch of medicine that, like IM, pretends to have a monopoly on holism is grossly misleading and can only hinder this process.
- Patient-centred: This is the same mean little trick in a different guise. They imply that conventional medicine is not patient-centred. Yet, all good medicine is, of course, patient-centred. To imply otherwise is just daft.
- Consideration of the patient’s physical and psychological wellbeing and treating the whole person rather than just the disease: Same trick yet again! The implication is that physical and psychological wellbeing and the whole person are not all that relevant in conventional medicine where only disease labels are being treated.
Altogether, this definition of IM is unworthy of anyone with the slightest ability to think critically. I find it much worse than the latest US definition (which already is fairly awful). In fact, it turns out to be a poorly disguised bonanza of strawman fallacies combined with ‘bait and switch’ deception.
How can this be?
How can a professional organisation engage in such mean trickery?
Perhaps a look at the list of speakers will go some way towards answering the question. Have a good look, you might recognize many individuals as members of our ALTERNATIVE MEDICINE HALL OF FAME.
PS
Registration costs £ 249 (standard rate)
PPS
Perhaps I should also mention at least 4 of the many commercial sponsors of the conference:
- Boiron
- Helixor
- Iscador
- Weleda
I have reported about Lyma twice before (see here and here). So, why again? I know, it’s just a supplement, but it is still a special case because
- it is being marketed very aggressively,
- it is the “world’s 1st super supplement”,
- we have on this blog a long debate with one of the experts responsible for Lyma.
On 18 March 2019, Paul Clayton, a clinical pharmacologist employed by the firm, stated the following about Lyma: you will realise that all the actives bar one (the ashwagandha) are food derivates / extracts. I take this to mean that, except for ashwagandha, all the ingredients of Lyma ought to be inherently safe. If we accept this for a moment (even though I am not sure that it is entirely correct), it means that ashwagandha determines the safety of Lyma more than any of the other ingredients. Paul Clayton also assured us that Lyma is totally safe, meaning that no serious concerns about ashwagandha’s safety have been reported.
Sadly, this does not seem to be quite true. There have been several reports of liver injury after the consumption of the herbal remedy. Here is another article that is not Medline-listed: Inagaki K, Mori N, Honda Y, Takaki S, Tsuji K, Chayama K. A case of drug-induced liver injury with prolonged severe intrahepatic cholestasis induced by Ashwagandha. Kanzo 2017; 58: 448-54. (20 year old man developed jaundice a month after increasing the dose of ashwagandha [bilirubin 20.7 mg/dL, ALT 94 U/L, Alk P 343 U/L, INR 1.02], jaundice persisting for more than 2 months, but ultimately resolving).
Perhaps the most concerning paper is this latest article:
Background & aims: Ashwagandha (Withania somnifera) is widely used in Indian Ayurvedic medicine. Several dietary supplements containing ashwagandha are marketed in the US and Europe, but only one case of drug-induced liver injury (DILI) due to ashwagandha has been published. The aim of this case series was to describe the clinical phenotype of suspected ashwagandha-induced liver injury.
Methods: Five cases of liver injury attributed to ashwagandha-containing supplements were identified; three were collected in Iceland during 2017-2018 and two from the Drug-Induced Liver Injury Network (DILIN) in 2016. Other causes for liver injury were excluded. Causality was assessed using the DILIN structured expert opinion causality approach.
Results: Among the five patients, three were males; mean age was 43 years (range 21-62). All patients developed jaundice and symptoms such as nausea, lethargy, pruritus and abdominal discomfort after a latency of 2-12 weeks. Liver injury was cholestatic or mixed (R ratios 1.4-3.3). Pruritus and hyperbilirubinaemia were prolonged (5-20 weeks). No patient developed hepatic failure. Liver tests normalized within 1-5 months in four patients. One patient was lost to follow-up. One biopsy was performed, showing acute cholestatic hepatitis. Chemical analysis confirmed ashwagandha in available supplements; no other toxic compounds were identified. No patient was taking potentially hepatotoxic prescription medications, although four were consuming additional supplements, and in one case, rhodiola was a possible causative agent along with ashwagandha.
Conclusions: These cases illustrate the hepatotoxic potential of ashwagandha. Liver injury is typically cholestatic or mixed with severe jaundice and pruritus, but self-limited with liver tests normalizing in 1-5 months.
In the lengthy exchanges between Paul Clayton and others on my blog – truly worth reading! – Paul assured us all that he is a serious scientist who would not mislead the consumer. At the time, he might not have been aware of the above-mentioned reports (the most recent of the above-mentioned papers was published in April 2020). Today, however, he must know of these concerns. Therefore, we can soon expect some serious measures from him and his employers, the firm that manufactures/sells Lyma.
I wonder what they will do. As far as I can see, it will have to be the voluntary withdrawal of Lyma from the market or, at the very least, the inclusion of a warning in all their materials:
“This product may cause severe liver damage”.
As discussed regularly on this blog, there is plenty of evidence to show that many chiropractors, homeopaths, and naturopaths discourage their patients from getting vaccinated. Now, a further investigation from the US seems to confirm these findings.
This analysis aims to evaluate differences between categories of so-called alternative medicine (SCAM) regarding vaccination behavior among US adults.
The data from the 2017 National Health Interview Survey (NHIS; n = 26,742; response rate 80.7%) was used for this purpose. Prevalences of flu vaccination, consultations with SCAM practitioners in the past 12 months, and their potential interactions were examined.
A total of 42.7% of participants had received the flu vaccination in the past 12 months, 32.4% had seen one or more SCAM practitioners. Users of any type of SCAM were as likely as non-users to have received a flu vaccination (44.8% users versus 41.7% non-users; p = 0,862; adjusted odds ratio [AOR] = 1.01, 95% confidence interval [CI] = 0.95-1.07).
Regarding specific SCAMs, individuals consulting with
- naturopaths (p < 0.001; AOR = 0.67, 95 %CI = 0.54-0.82),
- homeopaths (p < 0.001; AOR = 0.55; 95 %CI = 0.44-0.69),
- chiropractors (p = 0.016; AOR = 0.9, 95 %CI = 0.83-0.98)
were less likely, while other SCAM approaches showed no significant association with flu vaccination behavior. Independent predictors for a flu shot were prior diabetes, cancer, current asthma, kidney disease, overweight and current pregnancy. As well, higher educational level, age, ethnicity, health insurance coverage, and having seen a general physician or medical specialist in the past 12 months were also associated with a higher vaccination rate.
The authors concluded that SCAM users were equally likely to receive an influenza vaccination compared with non-users. Different complementary therapies showed varied associations with vaccination behavior. Further analyses may be needed to distinguish influencing factors among patients’ vaccination behavior.
This investigation confirms the prevalent anti-vax stance within chiropractic, homeopathy, and naturopathy. The effect is strongest by far with homeopaths. Nothing new! We knew this for a very long time. The question is WHAT ARE WE DOING ABOUT IT? Or more specifically, are the professional organizations of these SCAM professions finally going to take any actions against even the most rabid anti-vaxxers in their midst?
And the answer?
You guessed it: NO!
And the irony of all this must not get lost here: chiropractors, homeopaths, naturopaths, and their respective organizations all pride themselves regularly that they attribute particular importance to disease prevention.
One argument that we hear regularly in the comment sections of this blog and elsewhere goes something like this:
“Why worry about a bit of so-called alternative medicine (SCAM like homeopathy or chiropractic, or Reiki, or Bach flower remedies, or detox, etc.)? Why should it bother us? Why not let everyone use what they want? Why not be a bit more tolerant?”
Tolerance is defined as sympathy or indulgence for beliefs or practices differing from or conflicting with one’s own. It is, of course, a quality that normally should be welcomed, taught, and celebrated. So, why not be more tolerant with enthusiasts of pseudoscientific SCAM?
In my view, there are several reasons.
- Ineffective therapies harm patients. The public tends to believe that SCAM is inherently safe. This is, of course, not true – think of chiropractic, for instance. But some treatments seem entirely harmless. Homeopathy might be a good example; its remedies contain nothing and therefore homeopathy can do no harm. Sadly, this is not true either. If a patient uses homeopathy to treat a serious condition, she is likely to harm herself by not treating that condition effectively. In extreme cases, this course of action can be fatal.
- Ineffective therapies are a waste of resources. It seems obvious that the money spent on something that does not work is money wasted. This is true whether we buy a car that is beyond repair or a SCAM that does not work beyond placebo.
- Pseudoscience makes a mockery of evidence-based medicine. If we are tolerant towards useless SCAM and accept that some people make money on, and mislead the public about SCAM, we basically send out a message that evidence is of secondary importance. This would weaken the trust in evidence-based medicine which, in turn, is bound to render healthcare less effective and stand in the way of progress.
- Pseudoscience undermines rationality and one form of irrationality begets another. Perhaps the biggest danger of tolerating promoters of quackery is that this undermines rational thinking far beyond the realm of healthcare. “Those who can make you believe absurdities can make you commit atrocities,” wrote Voltaire. I fear that he might have been correct.
In my view, tolerance about pseudoscientific, implausible, ineffective, or harmful SCAMs is misplaced. On the contrary, I feel that it is our duty to limit the harm they do to the public, patients, and progress by exposing them for what they are.
The ‘International Chiropractors Association’ (ICA) has just issued a statement entitled “International Chiropractors Association Affirms Policy on Health Freedom“. On the background of the fact that US President Biden, issued a series of Executive Orders related to mandating federal employees and federal contractors to receive the COVID-19 vaccine, the ICA try to explain their position regarding vaccinations. Here are a few passages from this statement:
…In a world of public health that promotes evidence-based decision making, we see the importance of natural immunity being ignored and replaced with a totalitarian approach of compulsory vaccination. At a time when the Surgeon General says misinformation has become an urgent threat to public health, misinformation is now being used in an attempt to discredit the chiropractic profession, the International Chiropractors Association, and all chiropractic patients who desire to focus on improving health naturally. After enduring 18 months of shutdowns, lockdowns, flattening the curve, masking, limitations of speech on social media; and a cancel culture environment that threatens the basic freedoms our country was founded upon in 1776, ICA will not compromise on the importance of protecting health freedom…
The ICA Policy on Immunization and Vaccination has remained unchanged for almost 50 years and clearly states:
“The International Chiropractors Association recognizes that the use of vaccines is not without risk and questions the wisdom of mass vaccination programs. Chiropractic principles favor the enhancement of natural immunity over artificial immunization.
The ICA supports each individual’s right to select his or her own health care and to be made aware of the possible adverse effects of vaccines upon a human body. In accordance with such principles and based upon the individual’s right to freedom of choice, the ICA is opposed to compulsory programs which infringe upon such rights.
The International Chiropractors Association is supportive of a conscience clause or waiver in compulsory vaccination laws, providing an elective course of action for all regarding immunization, thereby allowing patients freedom of choice in matters affecting their bodies and health.”
The International Chiropractors Association maintains that all healthcare interventions, including the chiropractic adjustment, are associated with some level of risk and that every individual is entitled to be informed of those risks, no matter how insignificant. All individuals must retain the freedom to accept or reject any healthcare product, procedure, or medication including vaccinations. The International Chiropractors Association therefore strongly opposes the use of medical mandates that violate personal sovereignty, violate the principles of informed consent, and constrain the rights of patients to make their own health care choices…
The ICA encourages the recognition that natural efforts to enhance the innate immune system ability to adapt to novel viruses are grounded in science and rejects the notion that the patients’ freedom to rely on naturally acquired immunity is not based upon unscientific beliefs.
The ICA rejects the premise that the chiropractic profession’s long history of promoting health freedom and supporting conscientious exemptions is based upon unscientific or non-mainstream beliefs…
I find this statement clear as mud and have the following questions:
- Do the ICA recommend vaccinations?
- In particular, do they encourage their members to get vaccinated with the COVID-19 vaccines?
- Do they advise to recommend COVID-19 vaccinations to their patients?
- Or do they think that natural immunity is preferable and advise their members and patients accordingly?
- Do they believe that spinal manipulation enhances natural immunity?
- Do they think that spinal manipulations are an effective alternative to COVID-19 vaccinations?
- Do they believe that scientific evidence trumps dogma or vice versa?
- Which of the two should, according to their conviction, must influence the decision-making processes in healthcare?
- If the ICA object to misinformation about COVID, why do they not stop their members from promoting it?
- What makes them think that information about the possible adverse effects of vaccines upon a human body is unavailable?
- If the ICA recognizes the risks of spinal manipulation, why do they not inform the public about them regularly and objectively?
- If the ICA knows about the importance of informed consent, why do not all of their members adhere to it?
- And finally, why do the ICA insist on the term ‘international’ in the name of their organization, if they purely deal with the US situation?
I do not expect the ICA to give me the answers to these questions. But perhaps their Wiki page goes some way towards answering some of them: “… The ICA supports the efforts of the National Vaccine Information Center (NVIC).[13] The NVIC is known for promoting false and misleading information about vaccines, in particular the discredited claim that vaccines cause autism.
The ICA’s annual conferences have featured anti-vaccination propaganda. In 2018 Guest Speaker Beau Pierce (Pierce co-produced a series entitled Vaccines Revealed) hosted a session entitled Vaccines Revealed.,[14] and Jeff Hays, known for producing the anti-Vaccine propaganda Vaccines Revealed, was invited to host a session the 2017 ICA Council on Chiropractic Pediatrics Annual Conference. In 2016 the widely discredited anti-vaccination propaganda film VAXXED was shown at a conference sponsored by the ICA’s Council on Chiropractic Pediatrics …”
SAY NO MORE!
Therapeutic touch (TT) is a form of paranormal or energy healing developed by Dora Kunz (1904-1999), a psychic and alternative practitioner, in collaboration with Dolores Krieger, a professor of nursing. TT is popular and practised predominantly by US nurses; it is currently being taught in more than 80 colleges and universities in the U.S., and in more than seventy countries. According to one TT-organisation, TT is a holistic, evidence-based therapy that incorporates the intentional and compassionate use of universal energy to promote balance and well-being. It is a consciously directed process of energy exchange during which the practitioner uses the hands as a focus to facilitate the process.
The question is: does TT work beyond a placebo effect?
This review synthesized recent (January 2009–June 2020) investigations on the effectiveness and safety of therapeutic touch (TT) as a therapy in clinical health applications. A rapid evidence assessment (REA) approach was used to review recent TT research adopting PRISMA 2009 guidelines. CINAHL, PubMed, MEDLINE, Cochrane databases, Web of Science, PsychINFO, and Google Scholar were screened between January 2009-March 2020 for studies exploring TT therapies as an intervention. The main outcome measures were for pain, anxiety, sleep, nausea, and functional improvement.
Twenty-one studies covering a range of clinical issues were identified, including 15 randomized controlled trials, four quasi-experimental studies, one chart review study, and one mixed-methods study including 1,302 patients. Eighteen of the studies reported positive outcomes. Only four exhibited a low risk of bias. All others had serious methodological flaws, bias issues, were statistically underpowered, and scored as low-quality studies. Over 70% of the included studies scored the lowest score possible on the GSRS weight of evidence scale. No high-quality evidence was found for any of the benefits claimed.
The authors drew the following conclusions:
After 45 years of study, scientific evidence of the value of TT as a complementary intervention in the management of any condition still remains immature and inconclusive:
- Given the mixed result, lack of replication, overall research quality and significant issues of bias identified, there currently exists no good quality evidence that supports the implementation of TT as an evidence‐based clinical intervention in any context.
- Research over the past decade exhibits the same issues as earlier work, with highly diverse poor quality unreplicated studies mainly published in alternative health media.
- As the nature of human biofield energy remains undemonstrated, and that no quality scientific work has established any clinically significant effect, more plausible explanations of the reported benefits are from wishful thinking and use of an elaborate theatrical placebo.
TT turns out to be a prime example of a so-called alternative medicine (SCAM) that enthusiastic amateurs, who wanted to prove TT’s effectiveness, have submitted to multiple trials. Thus the literature is littered with positive but unreliable studies. This phenomenon can create the impression – particularly to TT fans – that the treatment works.
This course of events shows in an exemplary fashion that research is not always something that creates progress. In fact, poor research often has the opposite effect. Eventually, a proper scientific analysis is required to put the record straight (the findings of which enthusiasts are unlikely to accept).
In view of all this, and considering the utter implausibility of TT, it seems an unethical waste of resources to continue researching the subject. Similarly, continuing to use TT in clinical settings is unethical and potentially dangerous.
I was surprised to discover that there is an entire website by a homeopath. He used to comment regularly on my blog but eventually got banned (I think). Now that chap writes pages and pages explaining that my criticisms of homeopathy are all wrong and that I actually haven’t got a clue. This seems to suggest that his homeopathy is not very effective for anger control. The texts are so intensely funny that I took the liberty of copying a short passage for you (without altering a single word).
Here we go:
When I started this blog in 2013, it was aimed to rebut Professor Edzard Ernst’s scientific examination and critique of homeopathy.
After 7 years of engaging with his posts, I realised that he does not have a clue about homeopathy due to rejecting the central tenet of homeopathy that disorder of the vital force leads to disease and, over time, to incurable medical conditions.
This blog aims to dispel false notions about the philosophy and practice of homeopathy and I recommend that the widely used clinical approach to homeopathy is discarded and replaced with spiritual/dynamic approach to homeopathy that is aligned with the principles set out in Hahnemann’s Organon of Medicine.
Dr. Edzard Ernst has, for more than two decades, engaged in a comical and polemical critique of what he considers to be ‘homeopathy’:
- He does not hold a recognized qualification in homeopathy.
- His understanding of homeopathy has, from the very outset, been below par: See my post ‘Arnica’.
- He associated Bach Flower Remedies with ‘homeopathy’ because both use potentised substances.
- He included Berlin Wall remedy in his new book, a remedy that he referred to as homeopathy’s finest in one of his blogs. Berlin Wall originated in the imagination of Colin Griffith (‘New Materia Medica’: isn’t that hilarious?) and it is not listed in the official Homeopathic Pharmacopeia.
- He continues to write blogs about homeopathic treatment of certain clinical conditions and his study of the ‘adjunctive treatment’ of asthma with homeopathy is in opposition to Hahnemann’s instruction that no other medicines should be used during homeopathic treatment.
- He seems to be unable to understand that homeopathy does not treat medical conditions, and that for classical homeopathy, as set out by Kent, most ‘medical conditions’ are beyond the curable stage of homeopathic treatment.
- He seems not even to know in detail Hahnemann’s works: The Organon, Chronic Diseases, and Materia Medica Pura. Evidence of this is that, in 7 years, I never read a post that was written by him that engaged in a critique of these works.
- He writes silly blogs about Boris Johnson almost being a homeopath.
- He has, on last count, six pages of blogs written in derision and criticism of HRH Prince of Wales.
- In discussion, he even asks the question: ‘are you speaking out of your arse?’
- He did a bit of reading on the Russia collusion investigation that he seemed to think was negative against President Trump and worried that the Donald might start world war 3.
- He rated himself as the world’s number one researcher in SCAM (so called alternative medicine of which homeopathy is one of the major forms of treatment).
I rate him as the world’s number one clown-critic of homeopathy.
Before Dr. Ernst started his journey to become the world eminent critic of homeopathy (and every other alternative health modality), he could have done two things:
- Undertaken a meticulous study of the works by Samuel Hahnemann and James Tyler Kent in order to gain an understanding of what Homeopathy is. I have yet to read a post by Edzard Ernst that provides a critique of the original works on homeopathy by the founders of homeopathy. Instead, he seems to have preferred to bypass the tedious work of reading texts and substituted his own interpretation of homeopathy in his critical reviews of ‘homeopathy’.
In Dr. Ernst’s view, the central tenet of homeopathy that there is a ‘vital force’ (living intelligence) in the human body must be rejected because it is an ‘outdated’ concept of ‘vitalism’. It seems to me, from my reading of his posts, that he considers atheism and materialist epistemology to be self-evident and idealist epistemology to be obviously deluded. Edzard Ernst is obviously not the philosophical type because if he was then he would have realised that his rejection of the ‘principle of vitalism’ automatically invalidates homeopathy as a credible subject of scientific investigation. Why did he waste so much time studying something that is evidently nonsense?
- Before embarking on expensive and time consuming trials and meta analyses of homeopathy, Dr. Ernst ought to have first sought to find independently verified scientific evidence of homeopathic cures of non self-resolving clinical conditions and illnesses documented in clinical practice and publications. As far as I am aware, there is no hard medical scientific evidence that homeopathy cures any non self-resolving clinical conditions and illnesses and so how sensible was it that numerous researchers conducted RCTs over several decades to test whether or not homeopathy is an effective treatment for medical conditions?
END OF QUOTE
There is more, much more – and it’s all as hilarious as the above. So, whenever you are having a bad day and feeling a bit low, please read it. It is certain to cheer you up.
Exploring preventive therapeutic measures has been among the biggest challenges during the coronavirus disease 2019 (COVID-19) pandemic caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). A team of Indian and US researchers explored the feasibility and methods of recruitment, retention, and potential signal of efficacy, of selected homeopathic medicines as a preventive measure for developing COVID-19 in a multi-group study.
A six-group, randomized, double-blind, placebo-controlled prophylaxis study was conducted in a COVID-19 exposed population in a quarantine facility in Mumbai, India. Each group received one of the following:
- Arsenicum album 30c,
- Bryonia alba 30c,
- Arsenicum album 30c, Bryonia alba 30c, Gelsemium sempervirens 30c, and Influenzinum 30c
- coronavirus nosode CVN01 30c,
- Camphora 1M,
- placebo.
Six pills twice a day were administered for 3 days. The primary outcome measure used was testing recruitment and retention in this quarantined setting. Secondary outcomes were numbers testing positive for COVID-19 after developing symptoms of illness, the number of subjects hospitalized, and days to recovery.
Good rates of recruitment and retention were achieved. Of 4,497 quarantined individuals, 2,343 sought enrollment, with 2,294 enrolled and 2,233 completing the trial (49.7% recruitment, 97.3% retention). Subjects who were randomized to either Bryonia alba (group 2) or to the CVN01 nosode (group 4) signaled a numerically lower incidence of laboratory-confirmed COVID-19 and a shorter period of illness, with evidence of fewer hospitalizations than those taking placebo. The three other groups did not show signals of efficacy.
The authors concluded that this pilot study supports the feasibility of a larger randomized, double-blind, placebo-controlled trial. Bryonia alba 30c and CVN01 30c should both be explored in disease prevention or shortening the course of disease symptomatology in a COVID-19-exposed population.
Signals of efficacy?
Are they kidding us?
The results failed to be statistically significant!
Hence the conclusions should be rewritten as follows:
This pilot study supports the feasibility of a larger trial in India where people have been told by an irresponsible government to believe in homeopathy. None of the 5 homeopathic treatments generated encouraging findings and none should be explored further. Studies of this nature must be discouraged firstly because homeopaths would not accept the findings of a trial of non-individualized homeopathy, and secondly because such trials will further confuse the public who might think that homeopathy is worth trying.