clinical trial
A recent blog-post pointed out that the usefulness of yoga in primary care is doubtful. Now we have new data to shed some light on this issue.
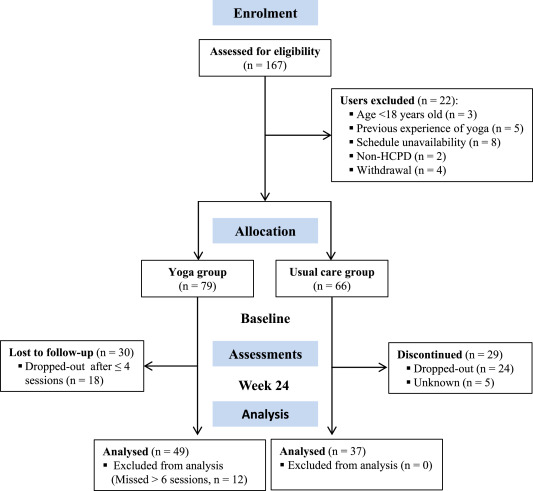
The new paper reports a ‘prospective, longitudinal, quasi-experimental study‘. Yoga group (n= 49) underwent 24-weeks program of one-hour yoga sessions. The control group had no yoga.
Participation was voluntary and the enrolment strategy was based on invitations by health professionals and advertising in the community (e.g., local newspaper, health unit website and posters). Users willing to participate were invited to complete a registration form to verify eligibility criteria.
The endpoints of the study were:
- quality of life,
- psychological distress,
- satisfaction level,
- adherence rate.
The yoga routine consisted of breathing exercises, progressive articular and myofascial warming-up, followed by surya namascar (sun salutation sequence; adapted to the physical condition of each participant), alignment exercises, and postural awareness. Practice also included soft twists of the spine, reversed and balance postures, as well as concentration exercises. During the sessions, the instructor discussed some ethical guidelines of yoga, as for example, non-violence (ahimsa) and truthfulness (satya), to allow the participant to have a safer and integrated practice. In addition, the participants were encouraged to develop their awareness of the present moment and their body sensations, through a continuous process of self-consciousness, keeping a distance between body sensations and the emotional experience. The instructor emphasized the connection between breathing and movement. Each session ended with a guided deep relaxation (yoga nidra; 5–10 min), followed by a meditation practice (5–10 min).
The results of the study showed that the patients in the yoga group experienced a significant improvement in all domains of quality of life and a reduction of psychological distress. Linear regression analysis showed that yoga significantly improved psychological quality of life.
The authors concluded that yoga in primary care is feasible, safe and has a satisfactory adherence, as well as a positive effect on psychological quality of life of participants.
Are the authors’ conclusions correct?
I think not!
Here are some reasons for my judgement:
- The study was far to small to justify far-reaching conclusions about the safety and effectiveness of yoga.
- There were relatively high numbers of drop-outs, as seen in the graph above. Despite this fact, no intention to treat analysis was used.
- There was no randomisation, and therefore the two groups were probably not comparable.
- Participants of the experimental group chose to have yoga; their expectations thus influenced the outcomes.
- There was no attempt to control for placebo effects.
- The conclusion that yoga is safe would require a sample size that is several dimensions larger than 49.
In conclusion, this study fails to show that yoga has any value in primary care.
PS
Oh, I almost forgot: and yoga is also satanic, of course (just like reading Harry Potter!).
Crohn’s disease (CD) is an inflammatory bowel disease characterized by recurring flares altered by periods of inactive disease and remission, affecting physical and psychological aspects and quality of life (QoL). The aim of this study was to determine the therapeutic benefits of soft non-manipulative osteopathic techniques in patients with CD.
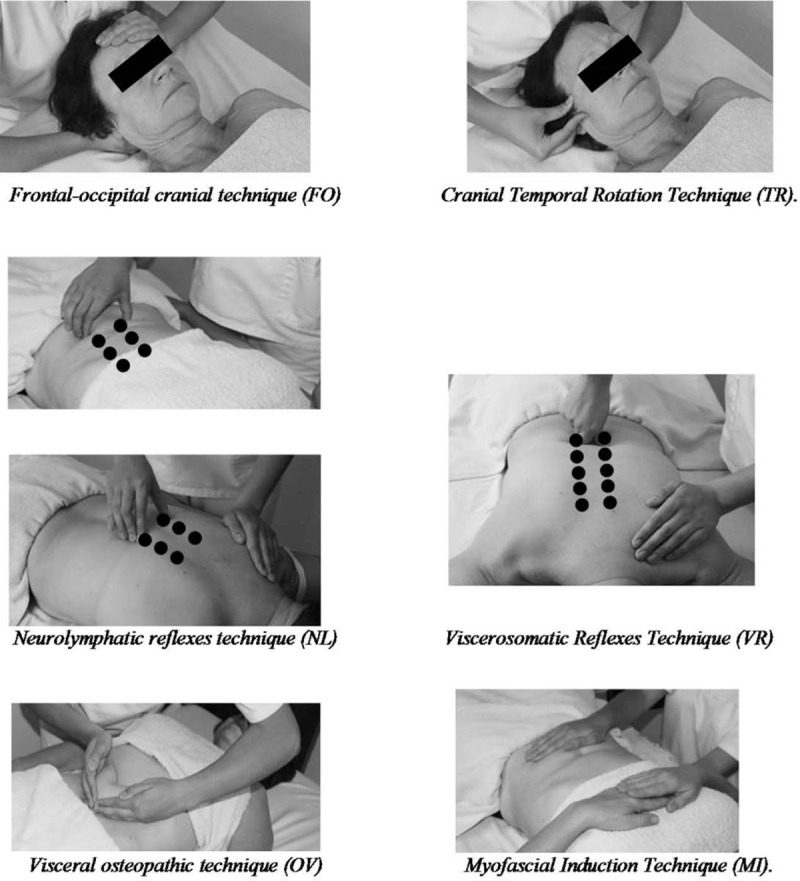
A randomized controlled trial was performed. It included 30 individuals with CD who were divided into 2 groups: 16 in the experimental group (EG) and 14 in the control group (CG). The EG was treated with the 6 manual techniques depicted below. All patients were advised to continue their prescribed medications and diets. The intervention period lasted 30 days (1 session every 10 days). Pain, global quality of life (GQoL) and QoL specific for CD (QoLCD) were assessed before and after the intervention. Anxiety and depression levels were measured at the beginning of the study.
A significant effect was observed of the treatment in both the physical and task subscales of the GQoL and also in the QoLCD but not in pain score. When the intensity of pain was taken into consideration in the analysis of the EG, there was a significantly greater increment in the QoLCD after treatment in people without pain than in those with pain. The improvements in GQoL were independent from the disease status.
The authors concluded that soft, non-manipulative osteopathic treatment is effective in improving overall and physical-related QoL in CD patients, regardless of the phase of the disease. Pain is an important factor that inversely correlates with the improvements in QoL.
Where to begin?
Here are some of the most obvious flaws of this study:
- It was far too small for drawing any far-reaching conclusions.
- Because the sample size was so small, randomisation failed to create two comparable groups.
- Sub-group analyses are based on even smaller samples and thus even less meaningful.
- The authors call their trial a ‘single-blind’ study but, in fact, neither the patients nor the therapists (physiotherapists) were blind.
- The researchers were physiotherapists, their treatments were mostly physiotherapy. It is therefore puzzling why they repeatedly call them ‘osteopathic’.
- It also seems unclear why these and not some other soft tissue techniques were employed.
- The CG did not receive additional treatment at all; no attempt was thus made to control for placebo effects.
- The stated aim to determine the therapeutic benefits… seems to be a clue that this study was never aimed at rigorously testing the effectiveness of the treatments.
My conclusion therefore is (yet again) that poor science has the potential to mislead and thus harm us all.
Excellent journals always publish excellent science!
If this is what you believe, you might want to read a study of chiropractic just published in the highly respected SCIENTIFIC REPORTS.
The objective of this study was to investigate whether a single session of chiropractic care could increase strength in weak plantar flexor muscles in chronic stroke patients. Maximum voluntary contractions (strength) of the plantar flexors, soleus evoked V-waves (cortical drive), and H-reflexes were recorded in 12 chronic stroke patients, with plantar flexor muscle weakness, using a randomized controlled crossover design. Outcomes were assessed pre and post a chiropractic care intervention and a passive movement control. Repeated measures ANOVA was used to asses within and between group differences. Significance was set at p < 0.05. Following the chiropractic care intervention there was a significant increase in strength (F (1,11) = 14.49, p = 0.002; avg 64.2 ± 77.7%) and V-wave/Mmax ratio (F(1,11) = 9.67, p = 0.009; avg 54.0 ± 65.2%) compared to the control intervention. There was a significant strength decrease of 26.4 ± 15.5% (p = 0.001) after the control intervention. There were no other significant differences. Plantar flexor muscle strength increased in chronic stroke patients after a single session of chiropractic care. An increase in V-wave amplitude combined with no significant changes in H-reflex parameters suggests this increased strength is likely modulated at a supraspinal level. Further research is required to investigate the longer term and potential functional effects of chiropractic care in stroke recovery.
In the article we find the following further statements (quotes in bold, followed by my comments in normal print):
- Data were collected by a team of researchers from the Centre for Chiropractic Research at the New Zealand College of Chiropractic. These researchers can be assumed to be highly motivated in generating a positive finding.
- The entire spine and both sacroiliac joints were assessed for vertebral subluxations, and chiropractic adjustments were given where deemed necessary, by a New Zealand registered chiropractor. As there is now near-general agreement that such subluxations are a myth, the researchers treated a non-existing entity.
- The chiropractor did not contact on a segment deemed to be subluxated during the control set-up and no adjustive thrusts were applied during any control intervention. The patients therefore were clearly able to tell the difference between real and control treatments. Participants were not checked for blinding success.
- Maximum isometric plantarflexion force was measured using an isometric strain gauge. Such measurements crucially depend on the motivation of the patient.
- The grant proposal for this study was reviewed by the Australian Spinal Research Foundation to support facilitation of funding from the United Chiropractic Association. Does this not mean the researchers had a conflict of interest?
- The authors declare no competing interests. Really? They were ardent subluxationists supported by the United Chiropractic Association, an organisation stating that chiropractic is concerned with the preservation and restoration of health, and focuses particular attention on the subluxation, and subscribes to to the obsolete concept of vitalism: we ascribe to the idea that all living organisms are sustained by an innate intelligence, which is both different from and greater than physical and chemical forces. Further, we believe innate intelligence is an expression of universal intelligence.
So, in essence, what we have here is an under-powered study sponsored by vitalists and conducted by subluxationists treating a mythical entity with dubious interventions without controlling for patients’ expectation pretending their false-positive findings are meaningful.
I cannot help wondering what possessed the SCIENTIFIC REPORTS to publish such poor science.
Acupuncture is all over the news today. The reason is a study just out in BMJ-Open.
The aim of this new RCT was to investigate the efficacy of a standardised brief acupuncture approach for women with moderate-tosevere menopausal symptoms. Nine Danish primary care practices recruited 70 women with moderate-to-severe menopausal symptoms. Nine general practitioners with accredited education in acupuncture administered the treatments.
The acupuncture style was western medical with a standardised approach in the pre-defined acupuncture points CV-3, CV-4, LR-8, SP-6 and SP-9. The intervention group received one treatment for five consecutive weeks. The control group received no acupuncture but was offered treatment after 6 weeks. Outcomes were the differences between the two groups in changes to mean scores using the scales in the MenoScores Questionnaire, measured from baseline to week 6. The primary outcome was the hot flushes scale; the secondary outcomes were the other scales in the questionnaire. All analyses were based on intention-to-treat analysis.
Thirty-six patients received the intervention, and 34 were in the control group. Four participants dropped out before week 6. The acupuncture intervention significantly decreased hot flushes, day-and-night sweats, general sweating, menopausal-specific sleeping problems, emotional symptoms, physical symptoms and skin and hair symptoms compared with the control group at the 6-week follow-up. The pattern of decrease in hot flushes, emotional symptoms, skin and hair symptoms was already apparent three weeks into the study. Mild potential adverse effects were reported by four participants, but no severe adverse effects were reported.
The authors concluded that the standardised and brief acupuncture treatment produced a fast and clinically relevant reduction in moderate-to-severe menopausal symptoms during the six-week intervention.
The only thing that I find amazing here is the fact the a reputable journal published such a flawed trial arriving at such misleading conclusions.
- The authors call it a ‘pragmatic’ trial. Yet it excluded far too many patients to realistically qualify for this characterisation.
- The trial had no adequate control group, i.e. one that can account for placebo effects. Thus the observed outcomes are entirely in keeping with the powerful placebo effect that acupuncture undeniably has.
- The authors nevertheless conclude that ‘acupuncture treatment produced a fast and clinically relevant reduction’ of symptoms.
- They also state that they used this design because no validated sham acupuncture method exists. This is demonstrably wrong.
- In my view, such misleading statements might even amount to scientific misconduct.
So, what would be the result of a trial that is rigorous and does adequately control for placebo-effects? Luckily, we do not need to rely on speculation here; we have a study to demonstrate the result:
Background: Hot flashes (HFs) affect up to 75% of menopausal women and pose a considerable health and financial burden. Evidence of acupuncture efficacy as an HF treatment is conflicting.
Objective: To assess the efficacy of Chinese medicine acupuncture against sham acupuncture for menopausal HFs.
Design: Stratified, blind (participants, outcome assessors, and investigators, but not treating acupuncturists), parallel, randomized, sham-controlled trial with equal allocation. (Australia New Zealand Clinical Trials Registry: ACTRN12611000393954)
Setting: Community in Australia.
Participants: Women older than 40 years in the late menopausal transition or postmenopause with at least 7 moderate HFs daily, meeting criteria for Chinese medicine diagnosis of kidney yin deficiency.
Interventions:10 treatments over 8 weeks of either standardized Chinese medicine needle acupuncture designed to treat kidney yin deficiency or noninsertive sham acupuncture.
Measurements: The primary outcome was HF score at the end of treatment. Secondary outcomes included quality of life, anxiety, depression, and adverse events. Participants were assessed at 4 weeks, the end of treatment, and then 3 and 6 months after the end of treatment. Intention-to-treat analysis was conducted with linear mixed-effects models.
Results: 327 women were randomly assigned to acupuncture (n = 163) or sham acupuncture (n = 164). At the end of treatment, 16% of participants in the acupuncture group and 13% in the sham group were lost to follow-up. Mean HF scores at the end of treatment were 15.36 in the acupuncture group and 15.04 in the sham group (mean difference, 0.33 [95% CI, −1.87 to 2.52]; P = 0.77). No serious adverse events were reported.
Limitation: Participants were predominantly Caucasian and did not have breast cancer or surgical menopause.
Conclusion: Chinese medicine acupuncture was not superior to noninsertive sham acupuncture for women with moderately severe menopausal HFs.
My conclusion from all this is simple: acupuncture trials generate positive findings, provided the researchers fail to test it rigorously.
Did we not have a flurry of systematic reviews of homeopathy in recent months?
And were they not a great disappointment to homeopaths and their patients?
Just as we thought that this is more than enough evidence to show that homeopathy is not effective, here comes another one.
This new review evaluated RCTs of non-individualised homeopathic treatment (NIHT) in which the control group received treatments other than placebo (OTP). Specifically, its aim was to determine the comparative effectiveness of NIHT on health-related outcomes for any given condition.
For each eligible trial, published in the peer-reviewed literature up to the end of 2016, the authors assessed its risk of bias (internal validity) using the seven-domain Cochrane tool, and its relative pragmatic or explanatory attitude (external validity) using the 10-domain PRECIS tool. The researchers grouped RCTs by whether these examined homeopathy as an alternative treatment (study design 1a), adjunctively with another intervention (design 1b), or compared with no intervention (design 2). RCTs were sub-categorised as superiority trials or equivalence/non-inferiority trials. For each RCT, a single ‘main outcome measure’ was selected to use in meta-analysis.
Seventeen RCTs, representing 15 different medical conditions, were eligible for inclusion. Three of the trials were more pragmatic than explanatory, two were more explanatory than pragmatic, and 12 were equally pragmatic and explanatory. Fourteen trials were rated ‘high risk of bias’ overall; the other three trials were rated ‘uncertain risk of bias’ overall. Ten trials had data that were extractable for meta-analysis. Significant heterogeneity undermined the planned meta-analyses or their meaningful interpretation. For the three equivalence or non-inferiority trials with extractable data, the small, non-significant, pooled effect size was consistent with a conclusion that NIHT did not differ from treatment by a comparator (Ginkgo biloba or betahistine) for vertigo or (cromolyn sodium) for seasonal allergic rhinitis.
The authors concluded that the current data preclude a decisive conclusion about the comparative effectiveness of NIHT. Generalisability of findings is restricted by the limited external validity identified overall. The highest intrinsic quality was observed in the equivalence and non-inferiority trials of NIHT.
I do admire the authors’ tenacity in meta-analysing homeopathy trials and empathise with their sadness of the multitude of negative results they thus have to publish. However, I do disagree with their conclusions. In my view, at least two firm conclusions ARE possible:
- This dataset confirms yet again that the methodological quality of homeopathy trials is lousy.
- The totality of the trial evidence analysed here fails to show that non-individualised homeopathy is effective.
In case you wonder why the authors are not more outspoken about their own findings, perhaps you need to read their statement of conflicts of interest:
Authors RTM, YYYF, PV and AKLT are (or were) associated with a homeopathy organisation whose significant aim is to clarify and extend an evidence base in homeopathy. RTM holds an independent research consultancy contract with the Deutsche Homöopathie-Union, Karlsruhe, Germany. YYYF and AKLT belong to Living Homeopathy Ltd., which has contributed funding to some (but not this current) HRI project work. RTM and PV have no other relationships or activities that could appear to have influenced the submitted work. JRTD had no support from any organisation for the submitted work; in the last 3 years, and for activities outside the submitted study, he received personal fees, royalties or out-of-pocket expenses for advisory work, invitational lectures, use of rating scales, published book chapters or committee membership; he receives royalties from Springer Publishing Company for his book, A Century of Homeopaths: Their Influence on Medicine and Health. JTRD has no other relationships or activities that could appear to have influenced the submitted study.
If one had wanted to add insult to injury, one could have added that, if, despite such conflicts of interest, the overall result of this new review turned out to be not positive, the evidence must be truly negative.
Highly diluted homeopathic remedies are pure placebos! This is what the best evidence clearly shows. Ergo they cannot be shown in a rigorous study to have effects that differ from placebo. But now there is a study that seems to contradict this widely accepted conclusion.
Can someone please help me to understand what is going on?
In this double-blind, placebo-controlled RCT, 60 patients suffering from insomnia were treated either individualised homeopathy (IH) or placebo for 3 months. Patient-administered sleep diary and Insomnia Severity Index (ISI) were used the primary and secondary outcomes respectively, measured at baseline, and after 3 months.
Five patients dropped out (verum:2,control:3).Intention to treat sample (n=60) was analysed. Trial arms were comparable at baseline. In the verum group, except sleep diary item 3 (P= 0.371), rest of the outcomes improved significantly (all P < 0.01). In the control group, there were significant improvements in diary item 6 and ISI score (P < 0.01) and just significant improvement in item 5 (P= 0.018). Group differences were significant for items 4, 5 and 6(P < 0.01) and just significant (P= 0.014) for ISI score with moderate to large effect sizes; but non-significant (P > 0.01) for rest of the outcomes.
The authors concluded that in this double-blind, randomized, prospective, placebo-controlled, two parallel arms clinical trial conducted on 60 patients suffering from insomnia, there was statistically significant difference measured in sleep efficiency, total sleep time, time in bed, and ISI score in favour of homeopathy over placebo with moderate to large effect sizes. Group differences were non-significant for rest of the outcomes(i.e. latency to fall asleep, minutes awake in middle of night and minutes awake too early). Individualized homeopathy seemed to produce significantly better effect than placebo. Independent replications and adequately powered trials with enhanced methodological rigor are warranted.
I have studied this article in some detail; its methodology is nicely and fully described in the original paper. To my amazement, I cannot find a flaw that is worth mentioning. Sure, the sample was small, the treatment time short, the outcome measure subjective, the paper comes from a dubious journal, the authors have a clear conflict of interest, even though they deny it – but none of these limitations has the potential to conclusively explain the positive result.
In view of what I stated above and considering what the clinical evidence so far tells us, this is most puzzling.
A 2010 systematic review authored by proponents of homeopathy included 4 RCTs comparing homeopathic medicines to placebo. All involved small patient numbers and were of low methodological quality. None demonstrated a statistically significant difference in outcomes between groups.
My own 2011 not Medline-listed review (Focus on Alternative and Complementary Therapies Volume 16(3) September 2011 195–199) included several additional studies. Here is its abstract:
The aim of this review was the critical evaluation of evidence for the effectiveness of homeopathy for insomnia and sleep-related disorders. A search of MEDLINE, AMED, CINAHL, EMBASE and Cochrane Central Register was conducted to find RCTs using any form of homeopathy for the treatment of insomnia or sleep-related disorders. Data were extracted according to pre-defined criteria; risk of bias was assessed using Cochrane criteria. Six randomised, placebo-controlled trials met the inclusion criteria. Two studies used individualised homeopathy, and four used standardised homeopathic treatment. All studies had significant flaws; small sample size was the most prevalent limitation. The results of one study suggested that homeopathic remedies were superior to placebo; however, five trials found no significant differences between homeopathy and placebo for any of the main outcomes. Evidence from RCTs does not show homeopathy to be an effective treatment for insomnia and sleep-related disorders.
It follows that the new trial contradicts previously published evidence. In addition, it clearly lacks plausibility, as the remedies used were highly diluted and therefore should be pure placebos. So, what could be the explanation of the new, positive result?
As far as I can see, there are the following possibilities:
- fraud,
- coincidence,
- some undetected/undisclosed bias,
- homeopathy works after all.
I would be most grateful, if someone could help solving this puzzle for me (if needed, I can send you the full text of the new article for assessment).
Mistletoe treatment of cancer patients was the idea of Rudolf Steiner. Mistletoe grows on a host tree like a parasite and eventually might kill it. This seems similar to a cancer killing a patient, and Steiner – influenced by the homeopathic ‘like cures like’ notion – thought that mistletoe should thus be an ideal treatment of all cancers. Despite the naivety of this concept, it somehow did catch on, and mistletoe has now become the number one cancer SCAM in Europe which is spreading fast also to the US and other countries.
But, as we all know, the fact that a therapy lacks plausibility does not necessarily mean that it is clinically useless. To decide, we need clinical trials; and to be sure, we need rigorous reviews of all reliable trials. Two such papers have just been published.
The aim of the systematic review was to give an extensive overview about current state of research concerning mistletoe therapy of oncologic patients regarding survival, quality of life and safety.
The authors extensive literature searches identified 3647 hits and 28 publications with 2639 patients were finally included in this review. Mistletoe was used in bladder cancer, breast cancer, other gynecological cancers (cervical cancer, corpus uteri cancer, and ovarian cancer), colorectal cancer, other gastrointestinal cancer (gastric cancer and pancreatic cancer), glioma, head and neck cancer, lung cancer, melanoma and osteosarcoma. In nearly all studies, mistletoe was added to a conventional therapy. Patient relevant endpoints were overall survival (14 studies, n = 1054), progression- or disease-free survival or tumor response (10 studies, n = 1091). Most studies did not show any effect of mistletoe on survival. Especially high quality studies did not show any benefit.
The authors concluded that, with respect to survival, a thorough review of the literature does not provide any indication to prescribe mistletoe to patients.
The aim of the second systematic review by the same team was to give an extensive overview about the current state of evidence concerning mistletoe therapy of oncologic patients regarding quality of life and side effects of cancer treatments. The same studies were used for this analysis as in the first review. Regarding quality of life, 17 publications reported results. Studies with better methodological quality showed less or no effects on quality of life.
The authors concluded that with respect to quality of life or reduction of treatment-associated side effects, a thorough review of the literature does not provide any indication to prescribe mistletoe to patients with cancer.
In 2003, we published a systematic review of the same subject. Here is its abstract:
Mistletoe extracts are widely used in the treatment of cancer. The results of clinical trials are however highly inconsistent. We therefore conducted a systematic review of all randomised clinical trials of this unconventional therapy. Eight databases were searched to identify all studies that met our inclusion/exclusion criteria. Data were independently validated and extracted by 2 authors and checked by the 3rd according to predefined criteria. Statistical pooling was not possible because of the heterogeneity of the primary studies. Therefore a narrative systematic review was conducted. Ten trials could be included. Most of the studies had considerable weaknesses in terms of study design, reporting or both. Some of the weaker studies implied benefits of mistletoe extracts, particularly in terms of quality of life. None of the methodologically stronger trials exhibited efficacy in terms of quality of life, survival or other outcome measures. Rigorous trials of mistletoe extracts fail to demonstrate efficacy of this therapy.
As we see, 16 years and 18 additional trials have changed nothing!
I therefore think that it is time to call it a day. We should stop the funding for further research into this dead-end alley. More importantly, we must stop giving false hope to cancer patients. All that mistletoe therapy truly does is to support a multi-million Euro industry.
The objective of this ‘real world’ study was to evaluate the effectiveness of integrative medicine (IM) on patients with coronary artery disease (CAD) and investigate the prognostic factors of CAD in a real-world setting.
A total of 1,087 hospitalized patients with CAD from 4 hospitals in Beijing, China were consecutively selected between August 2011 and February 2012. The patients were assigned to two groups:
- Chinese medicine (CM) plus conventional treatment, i.e., IM therapy (IM group). IM therapy meant that the patients accepted the conventional treatment of Western medicine and the treatment of Chinese herbal medicine including herbal-based injection and Chinese patent medicine as well as decoction for at least 7 days in the hospital or 3 months out of the hospital.
- Conventional treatment alone (CT group).
The endpoint was a major cardiac event [MCE; including cardiac death, myocardial infarction (MI), and the need for revascularization].
A total of 1,040 patients finished the 2-year follow-up. Of them, 49.4% received IM therapy. During the 2-year follow-up, the total incidence of MCE was 11.3%. Most of the events involved revascularization (9.3%). Cardiac death/MI occurred in 3.0% of cases. For revascularization, logistic stepwise regression analysis revealed that age ⩾ 65 years [odds ratio (OR), 2.224], MI (OR, 2.561), diabetes mellitus (OR, 1.650), multi-vessel lesions (OR, 2.554), baseline high sensitivity C-reactive protein level ⩾ 3 mg/L (OR, 1.678), and moderate or severe anxiety/depression (OR, 1.849) were negative predictors (P<0.05); while anti-platelet agents (OR, 0.422), β-blockers (OR, 0.626), statins (OR, 0.318), and IM therapy (OR, 0.583) were protective predictors (P<0.05). For cardiac death/MI, age ⩾ 65 years (OR, 6.389) and heart failure (OR, 7.969) were negative predictors (P<0.05), while statin use (OR, 0.323) was a protective predictor (P<0.05) and IM therapy showed a beneficial tendency (OR, 0.587), although the difference was not statistically significant (P=0.218).
The authors concluded that in a real-world setting, for patients with CAD, IM therapy was associated with a decreased incidence of revascularization and showed a potential benefit in reducing the incidence of cardiac death or MI.
What the authors call ‘real world setting’ seems to be a synonym of ‘lousy science’, I fear. I am not aware of good evidence to show that herbal injections and concoctions are effective treatments for CAD, and this study can unfortunately not change this. In the methods section of the paper, we read that the treatment decisions were made by the responsible physicians without restriction. That means the two groups were far from comparable. In their discussion section, the authors state; we found that IM therapy was efficacious in clinical practice. I think that this statement is incorrect. All they have shown is that two groups of patients with similar diagnoses can differ in numerous ways, including clinical outcomes.
The lessons here are simple:
- In clinical trials, lack of randomisation (the only method to create reliably comparable groups) often leads to false results.
- Flawed research is currently being used by many proponents of SCAM (so-called alternative medicine) to mislead us about the value of SCAM.
- The integration of dubious treatments into routine care does not lead to better outcomes.
- Integrative medicine, as currently advocated by SCAM-proponents, is a nonsense.
Once again, I am indebted to the German homeopathy lobbyist, Jens Behnke (research officer at the Karl and Veronica Carstens-Foundation); this time for alerting me via a tweet to the existence of the ‘Institute for Scientific Homeopathy’ run by Dr K Lenger. Anyone who combines the terms ‘scientific’ and ‘homeopathy’ has my full attention.
The institution seems to be small (too small to have its own website); in fact, it seems to have just one member: Dr Karin Lenger. But size is not everything! Lenger has achieved something extraordinary: she has answered the questions that have puzzled many of us for a long time; she has found the ‘modus operandi’ of homeopathy by discovering that:
- Homeopathy is a regulation therapy that acts (and reacts) as per the principle of resonance to deal hypo- and hyper-functions of pathological pathways.
- As per resonance principle, the fundamental principles of homeopathy have the same frequencies so that the resonance principle can work.
- Pathological pathways are cured by using their highly potentized substrates, inhibitors, and enzymes.
- The efficacy of homeopathy now has a scientific base and is completely explained by applying biochemical and biophysical laws.
Progress at last!
If that is not noteworthy, what is?
But there is more!
This website, for instance, explains that Lenger Karin Dr.rer.nat., pursued Diploma in Biochem, studied Biochemistry at the Universities of Tubingen and Cologne. Her research topics revolved around enzymatic gene regulation, cancer research, enzymatic mechanisms of steroid hormones at the Medical University of Lubeck. In 1987 she became a Lecturer for Homeopathy at DHU ((Deutsche Homöopathie Union = German Homeopathy Union). Since 1995 she worked as a Homeopathic Practitioner and developed the “biochemical homeopathy” by using highly potentized substrates of pathological enzymes for her patients. She detected magnetic photons in high homeopathic potencies by two magnetic resonance methods and developed a model of physical and biochemical function of homeopathy.
Karin Lenger detected magnetic photons in highly diluted and potentized homeopathic remedies. Since the living body is an electromagnetic wavepackage (Einstein), the homeopathic law of Similars (Hahnemann 1755-1843) can be expressed as: the frequencies of the patient must match the frequencies of the remedies. Homeopathy is a regulation therapy curing hypo and hyperfunction of a pathological pathway by resonance: highly potentized substrates, inhibitors, enzymes, receptors of the distinct pathological pathways cure according to biochemical rules: A homeopathic symptom picture is obtained by poisoning a volunteer with a toxin. Simultaneously he develops psychological symptoms, the toxicological pathway and e.g. frequencies I-V. The highly potentized toxin has the frequencies I-V. The patient has symptoms as if he was poisoned by the toxin: during his illness he developed the toxicological pathway, frequencies I-V and psychological symptoms. The potentized toxin cures simultaneously the patient’s frequencies by resonance, his pathological pathway and the psychological symptoms. A stitch of honey bee, apis mellifica, causes a red oedema; a patient developing a red oedema at the finger-joint by rheumatism is cured by highly potentized Apis mellifica. Paralyses caused by a lack of the neurotransmitter acetylcholine bound to the acetylcholine-receptor at the post-synapsis can be healed by using these potentized remedies: the venom of cobra, Naja tripudians containing the receptor’s irreversible inhibitor cobrotoxin, the reversible inhibitor Atropine and Acetylcholine, daily applied. The availability of acetylcholine is maintained by glycolysis and fatty acid oxidation. This can be supported by giving these remedies: Lecithin, Lipasum, Glycerinum, Glucosum and Coenzyme A.
And in case, you are not yet fully convinced, a recent publication is bound to ball you over. Here is its abstract, if you need more, the link allows you to read the full paper as well:
Homeopathy, a holistic therapy, is believed to cure only acute symptoms of a beginning illness according to the Laws of Similars; but not deep, bleeding, septic wounds. The homeopaths refuse to heal according to special medical indications. Based on Lenger’s detection of magnetic photons in homeopathic remedies a biochemical and biophysical model of homeopathic healing was developed Biochemical, pathological pathways can be treated by their highly potentized substrates and inhibitors. Three groups of patients with moderate, severe and septic wounds had been successfully treated with the suitable remedies depending on the biochemical pathological state.
___________________________________________________________
Do I sense a Nobel Prize in the offing?
Surely!
Lenger’s clinical trial is baffling. But much more impressive are the ‘magnetic photons’ and the reference to Einstein. This is even more significant, if we consider what the genius (Einstein, not Lenger!) is reported to have said about homeopathy: Einstein reflected for a little while and then said: “If one were to lock up 10 very clever people in a room and told them they were only allowed out once they had come up with the most stupid idea conceivable, they would soon come up with homeopathy.”
I would warn every parent who thinks that taking their child to a chiropractor is a good idea. For this, I have three main reasons:
- Chiropractic has not been shown to be effective for any paediatric condition.
- Chiropractors often advise parents against vaccinating their children.
- Chiropractic spinal manipulations can cause harm to kids.
The latter point seems to be confirmed by a recent PhD thesis of which so far only one short report is available. Here are the relevant bits of information from it:
Katie Pohlman has successfully defended her PhD thesis, which focused on the assessment of safety in pediatric manual therapy. As a clinical research scientist at Parker University, Dallas, Texas, she identified a lack of prospective patient safety research within the chiropractic population in general and investigated this deficit in the paediatric population in particular.
Pohlman used a cross-sectional survey to assess the barriers and facilitators for participation in a patient safety reporting system. At the same time, she also conducted a randomized controlled trial comparing the quantity and quality of adverse event reports in children under 14 years receiving chiropractic care.
The RCT recruited 69 chiropractors and found adverse events reported in 8.8% and 0.1% of active and passive surveillance groups respectively. Of the adverse events reported, 56% were considered mild, 26% were moderate and 18% were severe. The frequency of adverse events was more common than previously thought.
This last sentence from the report is somewhat puzzling. Our systematic review of the risks of spinal manipulation showed that data from prospective studies suggest that minor, transient adverse events occur in approximately half of all patients receiving spinal manipulation. The most common serious adverse events are vertebrobasilar accidents, disk herniation, and cauda equina syndrome. Estimates of the incidence of serious complications range from 1 per 2 million manipulations to 1 per 400,000. Given the popularity of spinal manipulation, its safety requires rigorous investigation.
The 8.8% reported by Pohlman are therefore not even one fifth of the average incidence figure reported previously in all age groups.
What could be the explanation for this discrepancy?
There are, of course, several possibilities, including the fact that infants cannot tell the clinician when their pain has increased. However, the most likely one, in my view, lies in the fact that RCTs are wholly inadequate for investigating risks because they typically include far too few patients to generate reliable incidence figures about adverse events. More importantly, clinicians included in such studies are self-selected (and thus particularly responsible/cautious) and are bound to behave most carefully while being part of a clinical trial. Therefore it seems possible – I would speculate even likely – that the 8.8% reported by Pohlman is unrealistically low.
Having said that, I do feel that the research by Kathie Pohlman is a step in the right direction and I do applaud her initiative.