charlatan
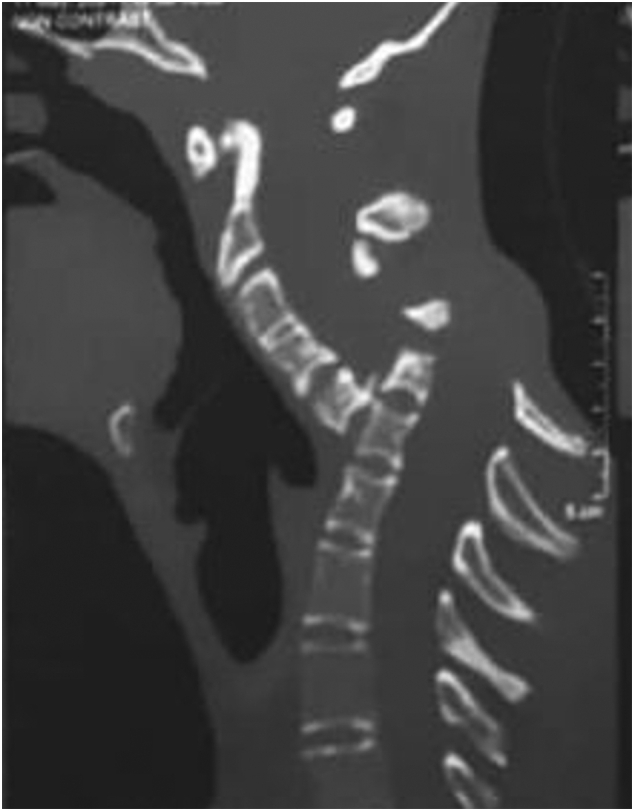
Spondyloptosis is a grade V spondylolisthesis – a vertebra having slipped so far with respect to the vertebra below that the two endplates are no longer congruent. It is usually seen in the lower lumbar spine but rarely can be seen in other spinal regions as well. Spondyloptosis is most commonly caused by trauma. It is defined as the dislocation of the spinal column in which the spondyloptotic vertebral body is either anteriorly or posteriorly displaced (>100%) on the adjacent vertebral body. Only a few cases of cervical spondyloptosis have been reported. The cervical cord injury in most patients is complete and irreversible. In most cases of cervical spondyloptosis, regardless of whether there is a neurologic deficit or not, reduction and stabilization of the fracture-dislocation is the management of choice
The case of a 16-year-old boy was reported who had been diagnosed with spondyloptosis of the cervical spine at the C5-6 level with a neurologic deficit following cervical manipulation by a traditional massage therapist. He could not move his upper and lower extremities, but the sensory and autonomic function was spared. The pre-operative American Spinal Cord Injury Association (ASIA) Score was B with SF-36 at 25%, and Karnofsky’s score was 40%. The patient was disabled and required special care and assistance.
The surgeons performed anterior decompression, cervical corpectomy at the level of C6 and lower part of C5, deformity correction, cage insertion, bone grafting, and stabilization with an anterior cervical plate. The patient’s objective functional score had increased after six months of follow-up and assessed objectively with the ASIA Impairment Scale (AIS) E or (excellent), an SF-36 score of 94%, and a Karnofsky score of 90%. The patient could carry on his regular activity with only minor signs or symptoms of the condition.
The authors concluded that this case report highlights severe complications following cervical manipulation, a summary of the clinical presentation, surgical treatment choices, and a review of the relevant literature. In addition, the sequential improvement of the patient’s functional outcome after surgical correction will be discussed.
This is a dramatic and interesting case. Looking at the above pre-operative CT scan, I am not sure how the patient could have survived. I am also not aware of previous similar cases. This does, however, not mean they don’t exist. Perhaps most affected patients simply died without being diagnosed. So, do we need to add spondyloptosis to the (hopefully) rare but severe complications of spinal manipulation?
A recent article in LE PARISIEN entitled “L’homéopathie vétérinaire, c’est sans effet… mais pas sans risque” – Veterinary homeopathy is without effect … but not without risk, tells it like it is. Here are a few excerpts that I translated for you.
More than 77% of French people have tried homeopathy in their lifetime. But have you ever given it to your pet? Harmless in most cases, its use can be dangerous when it replaces a treatment whose effectiveness is scientifically proven … from a safety point of view, the tiny granules are indeed irreproachable: their use does not induce any drug interaction or undesirable side effects, nor does it run the risk of overdosing or addiction … homeopathic preparations owe their harmlessness to their lack of proper effects. “Neither in human medicine nor in veterinary medicine, at the current stage, clinical studies of all levels do not provide sufficient scientific evidence to support the therapeutic efficacy of homeopathic preparations”, stated the French Veterinary Academy in May 2021. These conclusions are in line with those of the French Academies of Medicine and Pharmacy, the British Royal College of Veterinary Surgeons, and all the international scientific bodies that have given their opinion on the subject.
Therefore, when homeopathy delays diagnosis or is used in place of proven effective treatments, its use represents a “loss of opportunity” for your pet. The greatest danger of homeopathy is not that the remedies are ineffective, but that some homeopaths believe that their therapies can be used as a substitute for genuine medical treatment,” summarizes a petition to the UK veterinary regulatory body signed by more than 1,000 British veterinarians. At best, this claim is misleading and, at worst, it can lead to unnecessary suffering and death.”
But how can we explain the number of testimonies from pet owners who say that “it works”? “I am very satisfied with the Kalium Bichromicum granules for my cat with an eye ulcer, which is healing very well”… These improvements, real or supposed, can be explained by “contextual effects”, among which the famous placebo effect (which is not specific to humans), your subjective interpretation of his symptoms, or the natural history of the disease.
When these contextual effects are ignored or misunderstood, the spontaneous resolution or reduction of the disease can be wrongly attributed to homeopathy, and thus maintain the illusion of its effectiveness. This confusion is all the more likely because homeopathy owes much of its popularity to its use to treat “everyday ailments”: nausea, allergies, fatigue, bruises, nervousness, etc., which tend to get better on their own with time, or which have a fluctuating expression…
In April 2019, the association published an open letter addressed to the National Council of the Order of Veterinarians, calling on it to take a position on the compatibility of homeopathy with the “ethical and scientific requirements” of the profession. The organization, whose official function is to guarantee the quality of the service rendered to the public by the 20,000 veterinarians practicing in France, issued its conclusions last October. It invited veterinary training centers to remove homeopathy from their curricula, under penalty of having their accreditation withdrawn, and thus their ability to deliver training credits.
In my view, this is a remarkably good and informative text. How often do homeopathy fans claim IT WORKS FOR ANIMALS AND THUS CANNOT BE A PLACEBO! The truth is that, as we have so often discussed on this blog, homeopathy does not work beyond placebo for animals. This renders veterinary homeopathy:
- a waste of money,
- potentially dangerous,
- in the worst cases a form of animal abuse.
My advice is that, as soon as a vet recommends homeopathy, you look for the exit.
I was alerted to the following short article from ‘The Blackpool Gazette‘:
Criminals have been using the brand name Pfizer to sell fake homeopathic vaccines to residents, according to police. The white tablets are sold under the pretence that they are an alternative to traditional vaccines, but actually contain no active ingredient. Analysis conducted by Lancashire Police revealed the tablets were nothing more than sugar pills. “Please note Pfizer do not produce any tablets as a cure or prophylactic for COVID-19,” a spokesman for the force added.
Homeopathy is a “treatment” based on the use of highly diluted substances, which practitioners claim can help the body heal itself, according to the NHS. A 2010 House of Commons Science and Technology Committee report on homeopathy said that homeopathic remedies perform no better than placebos. In 2017, NHS England said it would no longer fund homeopathy on the NHS as the lack of any evidence for its effectiveness did not justify the cost. This was backed by a High Court judgement in 2018.
I think there might be a slight misunderstanding here. The homeopathic remedy might not be fake, as it was produced according to the concepts of homeopathy. It is homeopathy itself that is fake. To me, it looks as though we are dealing with the German product I mentioned a while ago. Let me remind you:
Many people believe that homeopathy is essentially plant-based – but they are mistaken! Homeopathic remedies can be made from anything: Berlin wall, X-ray, pus, excrement, dental plaque, mobile phone rays, poisons … anything you can possibly think of. So, why not from vaccines?
This is exactly what a pharmacist specialized in homeopathy thought.
It has been reported that the ‘Schloss-Apotheke’ in Koblenz, Germany offered for sale a homeopathic remedy made from the Pfizer vaccine. This has since prompted not only the Chamber of Pharmacists but also the Paul Ehrlich Institute and Pfizer to issue statements. On Friday (30/4/2021) morning, the pharmacy had advertised homeopathic remedies based on the Pfizer/Biontech vaccine. The Westphalia-Lippe Chamber of Pharmacists then issued an explicit warning against it. “We are stunned by this,” said a spokesman. The offer has since disappeared from the pharmacy’s website.
Pfizer vaccine. This has since prompted not only the Chamber of Pharmacists but also the Paul Ehrlich Institute and Pfizer to issue statements. On Friday (30/4/2021) morning, the pharmacy had advertised homeopathic remedies based on the Pfizer/Biontech vaccine. The Westphalia-Lippe Chamber of Pharmacists then issued an explicit warning against it. “We are stunned by this,” said a spokesman. The offer has since disappeared from the pharmacy’s website.
On Friday afternoon, the manufacturer of the original vaccine also intervened. The Paul Ehrlich Institute released a statement making it clear that a vaccine is only safe “if it is administered in accordance with the marketing authorization.”
The Schloss-Apotheke had advertised the product in question with the following words:
“We have Pfizer/BioNTech Covid-19-Vaccine in potentized form up to D30 as globules or dilution (for discharge) in stock.”
The chamber of pharmacists countered with a warming under the heading “Facts instead of Fake News” on Facebook and Instagram:
“Whatever they might contain: These remedies are no effective protection against Covid-19.”
Pharmacy manager, Annette Eichele, of the Schloss-Apotheke claimed she had not sold homeopathic Corona vaccines and stressed that effective vaccines of this kind do not exist. According to Eichele, only an additional “mini drop” of the original Biontech vaccine had been used and “highly potentized” and prepared homeopathically. According to Eichele, Corona vaccinations that had already been administered were thus to have a “better and more correct effect with this supplementary product, possibly without causing side effects … but this is not scientifically proven”. The homeopathic product had been produced only on customer request and had been sold less than a dozen times in the past weeks. Ten grams of the remedy were sold for about 15 Euros. On Twitter, Eichele stated: „Wir haben nichts Böses getan, wir wollten nur Menschen helfen!“ (We have done nothing evil, we only wanted to help people). I am reminded yet again of Bert Brecht who observed:
“The opposite of good is not evil but good intentions”.
_______________________
If I am right, the remedy is not truly fake but a genuine product of a fake concept, namely homeopathy. In that case, the term ‘criminal’ might need to be applied to homeopathy itself – an interesting thought!
The cardiothoracic surgeon and famous US woo merchant, Dr. Mehmet Oz, is probably known to most readers. I have previously mentioned him several times, for instance, here and here. His institution, Columbia University in New York City, has had many (I’d say too many) years of patience with his relentless promotion of outright and often dangerous quackery. Now it has been reported that the university has finally cut ties with Dr. Oz:
“It took Columbia far too long to remove Oz from its otherwise distinguished medical faculty,” Henry Miller, MD, of the Pacific Research Institute in California, told MedPage Today via email. Miller stressed that “the ‘Oz controversy’ was never about free speech. It was about an unethical grifter whose claims and pronouncements were not supported by science and were injurious to consumers — in the interest of financial benefit to Oz himself. That constitutes professional misconduct.”
The university’s Irving Medical Center quietly ended its relationship with Oz at the end of April, according to The Daily Beast. He had been removed from several pages of the medical center’s website in mid-January. In 2018, Oz’s title had been changed to professor emeritus and special lecturer, according to reports. A spokesperson for Columbia University confirmed the 2018 change in an email to MedPage Today.
In 2015, Miller and colleagues sent a letter to Lee Goldman, MD, MPH, dean of the Faculties of Health Sciences and Medicine at the university, calling for Oz’s expulsion. Oz had “repeatedly shown disdain for science and for evidence-based medicine” and “manifested an egregious lack of integrity by promoting quack treatments and cures in the interest of personal financial gain,” according to Miller’s group…
In 2014, Oz was called to testify before the Senate Subcommittee on Consumer Protection, Product Safety, and Insurance during a hearing on false advertising in the diet and weight-loss industry. Senators grilled Oz regarding statements he made on “The Dr. Oz Show” that promoted green coffee bean extract as a “miracle pill” for weight loss.
But long before that hearing, tensions had built between Oz and the medical community because of his penchant for spouting dubious medical claims on his TV show and in the media. For example, in a 2011 segment, ABC News‘ chief health and medical editor Richard Besser, MD, called out a purported “study” of arsenic in apple juice that Oz conducted for an episode of his show.
Besser charged that Oz’s science was shoddy because he reported total arsenic rather than the breakdown between organic and inorganic arsenic — only the latter of which is known to be toxic. Even the FDA sent the show a letter before the segment aired saying it would be “irresponsible and misleading” to report the results.
Oz again broke with medical science during the pandemic when he touted hydroxychloroquine as a cure for COVID-19, even as evidence mounted that it had no effect on disease course.
Oz is currently running for a U.S. Senate seat in Pennsylvania as a Republican candidate. Former President Trump endorsed Oz, touting Oz’s medical and academic credentials in a statement, according to NPR: “He even said that I was in extraordinary health, which made me like him even more (although he also said I should lose a couple of pounds!).”
__________________________
I have to admit that I find these reports somewhat puzzling. Don’t get me wrong: it’s not that I don’t think Oz deserves to be dismissed. In fact, he had already richly deserved it many years ago. What I find, however, odd is that giving someone the title ’emeritus professor’ can hardly be called ‘cutting ties’ with him. In some ways, it is even the opposite (I should know because I currently have this status).
When I looked up Oz, Columbia listed him as:
Oz, Mehmet C. (MD)
Special Lecturer in the Department of Surgery
Phone: 212.305.4434 · Fax: 212.342.3520
Location: MHB, Rm. 435-62
Similarly, the website of the Irving Medical Center is full of entries about Oz. Confusion is therefore more than justified, I think.
What is needed, I feel, is a clear statement from Columbia University about its relationship with Dr. Oz. Are they still proud of his considerable fame/notoriety, or did they in fact have the integrity to cut ties with one of the most self-aggrandizing woo merchants of all times?
Harad Matthes, the boss of the anthroposophical Krankenhaus Havelhoehe and professor for Integrative and Anthroposophical Medicine at the Charite in Berlin, has featured on my blog before (see here and here). Now he is making headlines again.
‘Die Zeit‘ reported that Matthes went on German TV to claim that the rate of severe adverse effects of COVID-19 vaccinations is about 40 times higher than the official figures indicate. In the MDR broadcast ‘Umschau’ Matthes said that his unpublished data show a rate of 0,8% of severe adverse effects. In an interview, he later confirmed this notion. Yet, the official figures in Germany indicate that the rate is 0,02%.
How can this be?
Die ZEIT ONLINE did some research and found that Matthes’ data are based on extremely shoddy science and mistakes. The Carite also distanced themselves from Matthes’ evaluation: “The investigation is an open survey and not really a scientific study. The data are not suitable for drawing definitive conclusions regarding incidence figures in the population that can be generalized” The problems with Matthes’ ‘study’ seem to be sevenfold:
- The data are not published and can thus not be scrutinized.
- Matthes’ definition of a severe adverse effect is not in keeping with the generally accepted definition.
- Matthes did not verify the adverse effects but relied on the information volunteered by people over the Internet.
- Matthes’ survey is based on an online questionnaire accessible to anyone. Thus it is wide open to selection bias.
- The sample size of the survey is around 10 000 which is far too small for generalizable conclusions.
- There is no control group which makes it impossible to differentiate a meaningful signal from mere background noise.
- The data contradict those from numerous other studies that were considerably more rigorous.
Despite these obvious flaws Matthes insisted in a conversation with ZEIT ONLINE that the German official incidence figures are incorrect. As Germany already has its fair share of anti-vaxxers, Matthes’ unfounded and irresponsible claims contribute significantly to the public sentiments against COVID vaccinations. They thus endangering public health.
In my view, such behavior amounts to serious professional misconduct. I, therefore, feel that his professional body, the Aerztekammer, should look into it and prevent further harm.
I just stumbled over a paper we published way back in 1997. It reports a questionnaire survey of all primary care physicians working in the health service in Devon and Cornwall. Here is an excerpt:
Replies were received from 461 GPs, a response rate of 47%. A total of 314 GPs (68%, range 32-85%) had been involved in complementary medicine in some way during the previous week. One or other form of complementary medicine was practised by 74 of the respondents (16%), the two most common being homoeopathy (5.9%) and acupuncture (4.3%). In addition, 115 of the respondents (25%) had referred at least one patient to a complementary therapist in the previous week, and 253 (55%) had endorsed or recommended treatment with complementary medicine. Chiropractic, acupuncture and osteopathy were rated as the three most effective therapies, and the majority of respondents believed that these three therapies should be funded by the health service. A total of 176 (38%) respondents reported adverse effects, most commonly after manipulation.
What I found particularly interesting (and had totally forgotten about) were the details of these adverse effects: Serious adverse effects of spinal manipulation included the following:
- paraplegia,
- spinal cord transection,
- fractured vertebra,
- unspecified bone fractures,
- fractured neck of femur,
- severe pain for years after manipulation.
Adverse effects not related to manipulation included:
- death after a coffee enema,
- liver toxicity,
- anaphylaxis,
- 17 cases of delay of adequate medical attention,
- 11 cases of adverse psychological effects,
- 14 cases of feeling to have wasted money.
If I remember correctly, none of the adverse effects had been reported anywhere which would make the incidence of underreporting 100% (exactly the same as in a survey we published in 2001 of adverse effects after spinal manipulations).
Today is WORLD ASTHMA DAY, a good opportunity perhaps to revisit a few of our own evaluations of so-called alternative medicine (SCAM) for asthma. Here are the abstracts of some of our systematic reviews on the subject:
Objective: The objective of this systematic review was to assess the effectiveness of yoga as a treatment option for asthma.
Method: Seven databases were searched from their inception to October 2010. Randomized clinical trials (RCTs) and non-randomized clinical trials (NRCTs) were considered, if they investigated any type of yoga in patients with asthma. The selection of studies, data extraction, and validation were performed independently by two reviewers.
Results: Six RCTs and one NRCT met the inclusion criteria. Their methodological quality was mostly poor. Three RCTs and one NRCT suggested that yoga leads to a significantly greater reduction in spirometric measures, airway hyperresponsivity, dose of histamine needed to provoke a 20% reduction in forced expiratory volume in the first second, weekly number of asthma attacks, and need for drug treatment. Three RCTs showed no positive effects compared to various control interventions.
Conclusions: The belief that yoga alleviates asthma is not supported by sound evidence. Further, more rigorous trials are warranted.
Some clinicians believe that spinal manipulation is an effective treatment for asthma. The aim of this systematic review was to critically evaluate the evidence for or against this claim. Four electronic databases were searched without language restrictions from their inceptions to September 2008. Bibliographies and departmental files were hand-searched. The methodological quality of all included studies was assessed with the Jadad score. Only randomised clinical trials of spinal manipulation as a treatment of asthma were included. Three studies met these criteria. All of them were of excellent methodological quality (Jadad score 5) and all used sham-manipulation as the control intervention. None of the studies showed that real manipulation was more effective than sham-manipulation in improving lung function or subjective symptoms. It is concluded that, according to the evidence of the most rigorous studies available to date, spinal manipulation is not an effective treatment for asthma.
Contradictory results from randomised controlled trials of acupuncture in asthma suggest both a beneficial and detrimental effect. The authors conducted a formal systematic review and meta-analysis of all randomised clinical trials in the published literature that have compared acupuncture at real and placebo points in asthma patients. The authors searched for trials published in the period 1970-2000. Trials had to measure at least one of the following objective outcomes: peak expiratory flow rate, forced expiratory volume in one second (FEV1) and forced vital capacity. Estimates of the standarised mean difference, between acupuncture and placebo were computed for each trial and combined to estimate the overall effect. Hetereogeneity was investigated in terms of the characteristics of the individual studies. Twelve trials met the inclusion criteria but data from one could not be obtained. Individual patient data were available in only three. Standardised differences between means ranging from 0.071 to 0.133, in favour of acupuncture, were obtained. The overall effect was not conventionally significant and it corresponds to an approximate difference in FEV1 means of 1.7. After exploring hetereogenenity, it was found that studies where bronchoconstriction was induced during the experiment showed a conventionally significant effect. This meta-analysis did not find evidence of an effect of acupuncture in reducing asthma. However, the meta-analysis was limited by shortcomings of the individual trials, in terms of sample size, missing information, adjustment of baseline characteristics and a possible bias against acupuncture introduced by the use of placebo points that may not be completely inactive. There was a suggestion of preferential publication of trials in favour of acupuncture. There is an obvious need to conduct a full-scale randomised clinical trial addressing these limitations and the prognostic value of the aetiology of the disease.
Background: Emotional stress can either precipitate or exacerbate both acute and chronic asthma. There is a large body of literature available on the use of relaxation techniques for the treatment of asthma symptoms. The aim of this systematic review was to determine if there is any evidence for or against the clinical efficacy of such interventions.
Methods: Four independent literature searches were performed on Medline, Cochrane Library, CISCOM, and Embase. Only randomised clinical trials (RCTs) were included. There were no restrictions on the language of publication. The data from trials that statistically compared the treatment group with that of the control were extracted in a standardised predefined manner and assessed critically by two independent reviewers.
Results: Fifteen trials were identified, of which nine compared the treatment group with the control group appropriately. Five RCTs tested progressive muscle relaxation or mental and muscular relaxation, two of which showed significant effects of therapy. One RCT investigating hypnotherapy, one of autogenic training, and two of biofeedback techniques revealed no therapeutic effects. Overall, the methodological quality of the studies was poor.
Conclusions: There is a lack of evidence for the efficacy of relaxation therapies in the management of asthma. This deficiency is due to the poor methodology of the studies as well as the inherent problems of conducting such trials. There is some evidence that muscular relaxation improves lung function of patients with asthma but no evidence for any other relaxation technique.
Background: Asthma is one of the most common chronic diseases in modern society and there is increasing evidence to suggest that its incidence and severity are increasing. There is a high prevalence of usage of complementary medicine for asthma. Herbal preparations have been cited as the third most popular complementary treatment modality by British asthma sufferers. This study was undertaken to determine if there is any evidence for the clinical efficacy of herbal preparations for the treatment of asthma symptoms.
Methods: Four independent literature searches were performed on Medline, Pubmed, Cochrane Library, and Embase. Only randomised clinical trials were included. There were no restrictions on the language of publication. The data were extracted in a standardised, predefined manner and assessed critically.
Results: Seventeen randomised clinical trials were found, six of which concerned the use of traditional Chinese herbal medicine and eight described traditional Indian medicine, of which five investigated Tylophora indica. Three other randomised trials tested a Japanese Kampo medicine, marihuana, and dried ivy leaf extract. Nine of the 17 trials reported a clinically relevant improvement in lung function and/or symptom scores.
Conclusions: No definitive evidence for any of the herbal preparations emerged. Considering the popularity of herbal medicine with asthma patients, there is urgent need for stringently designed clinically relevant randomised clinical trials for herbal preparations in the treatment of asthma.
Breathing techniques are used by a large proportion of asthma sufferers. This systematic review was aimed at determining whether or not these interventions are effective. Four independent literature searches identified six randomized controlled trials. The results of these studies are not uniform. Collectively the data imply that physiotherapeutic breathing techniques may have some potential in benefiting patients with asthma. The safety issue has so far not been addressed satisfactorily. It is concluded that too few studies have been carried out to warrant firm judgements. Further rigorous trials should be carried out in order to redress this situation.
__________________________________
So, if you suffer from asthma, my advice is to stay away from SCAM. This might be easier said than done because SCAM practitioners are only too willing to lure asthma patients into their cult. In 2003, we have demonstrated this phenomenon by conducting a survey with chiropractors. Here is our short paper in full:
Classic chiropractic theory claims that vertebral subluxation blocks the flow of ‘‘innate intelligence’’ which, in turn, affects the health of asthma patients (1). Chiropractictors often use spinal manipulation (SM) to correct such malalignments and treat asthma (2). Several clinical trials of chiropractic SM exist, but the most rigorous ones are clearly negative (3,4). Chronic medication with corticosteroids can lead to osteoporosis, a condition, which is a contra-indication to chiropractic SM (5). Given this background, we aimed to determine whether chiropractors would advise an asthma patient on long-term corticosteroids (5 years) to try chiropractic as a treatment for this condition.
All 350 e-mail addresses listed at www.interadcom.com/chiro/html were randomised into two groups. A (deceptive) letter from a (fictitious) patient was sent to group A while group B was asked for advice on chiropractic treatment for asthma as part of a research project. Thus, groups A and B were asked the same question in di¡erent contexts: is chiropractic safe and e¡ective for an asthma patient on long-term steroids. After data collection, respondents from group A were informed that the e-mail had been part of a research project.
Of 97 e-mails in group A, we received 31 responses (response rate = 32% (95% CI, 0.23^ 0.41)). Seventy-four per cent (23 respondents) recommended visiting a chiropractor (95% CI, 0.59^ 0.89). Thirty-five per cent (11 respondents) mentioned minimal or no adverse effects of SM (95% CI, 0.18 ^ 0.52). Three chiropractors responded that some adverse e¡ects exist, e.g. risk of bone fracture, or stroke. Two respondents noted that other investigations (X-rays, spinal and neurological examination) were required before chiropractic treatment. Three respondents suggested additional treatments and one warned about a possible connection between asthma and the measles vaccine. Of 77 e-mails sent to group B, we received 16 responses (response rate = 21% (95% CI, 0.17^ 0.25)). Eleven respondents (69%) recommended visiting a chiropractor (95% CI, 0.46 ^ 0.91). Ten respondents mentioned minimal or no adverse effects of SM (95% CI, 0.39^ 0.87). Five chiropractors responded that adverse effects of SM exist (e.g. bone fracture). Five respondents suggested pre-testing the patient to check bone density, allergy, diet, exercise level, hydration and blood. Additional treatments were recommended by three respondents. The pooled results of groups A and B suggested that the majority of chiropractors recommend chiropractic treatment for asthma and the minority mention any adverse effects.
Our results demonstrate that chiropractic advice on asthma therapy is as readily available over the Internet as it is likely to be misleading. The majority of respondents from both groups (72%) recommended chiropractic treatment. This usually entails SM, a treatment modality which has been demonstrated to be ineffective in rigorous clinical trials (3,4,6). The advice may also be dangerous: the minority of the respondents of both groups (17%) caution of the risk of bone fracture. Our findings also suggest that, for the research question asked, a degree of deception is necessary. The response rate in group B was 12% lower than that of group A, and the answers received differed considerably between groups. In group A, 10% acknowledged the possibility of adverse e¡ects, this figure was 33% in group B. In conclusion, chiropractors readily provide advice regarding asthma treatment, which is often not evidence-based and has the potential to put patients at risk.
__________________________
As I stated above: if you suffer from asthma, my advice is to
stay away from SCAM.
Acupuncture for animals has a long history in China. In the West, it was introduced in the 1970s when acupuncture became popular for humans. A recent article sums up our current knowledge on the subject. Here is an excerpt:
Acupuncture is used mainly for functional problems such as those involving noninfectious inflammation, paralysis, or pain. For small animals, acupuncture has been used for treating arthritis, hip dysplasia, lick granuloma, feline asthma, diarrhea, and certain reproductive problems. For larger animals, acupuncture has been used for treating downer cow syndrome, facial nerve paralysis, allergic dermatitis, respiratory problems, nonsurgical colic, and certain reproductive disorders.Acupuncture has also been used on competitive animals. There are veterinarians who use acupuncture along with herbs to treat muscle injuries in dogs and cats. Veterinarians charge around $85 for each acupuncture session.[8]Veterinary acupuncture has also recently been used on more exotic animals, such as chimpanzees (Pan troglodytes)[9] and an alligator with scoliosis,[10] though this is still quite rare.
To put it in a nutshell: acupuncture for animals is not evidence-based.
How can I be so sure?
Because ref 1 in the text above refers to our paper. Here is its abstract:
Acupuncture is a popular complementary treatment option in human medicine. Increasingly, owners also seek acupuncture for their animals. The aim of the systematic review reported here was to summarize and assess the clinical evidence for or against the effectiveness of acupuncture in veterinary medicine. Systematic searches were conducted on Medline, Embase, Amed, Cinahl, Japana Centra Revuo Medicina and Chikusan Bunken Kensaku. Hand-searches included conference proceedings, bibliographies, and contact with experts and veterinary acupuncture associations. There were no restrictions regarding the language of publication. All controlled clinical trials testing acupuncture in any condition of domestic animals were included. Studies using laboratory animals were excluded. Titles and abstracts of identified articles were read, and hard copies were obtained. Inclusion and exclusion of studies, data extraction, and validation were performed independently by two reviewers. Methodologic quality was evaluated by means of the Jadad score. Fourteen randomized controlled trials and 17 nonrandomized controlled trials met our criteria and were, therefore, included. The methodologic quality of these trials was variable but, on average, was low. For cutaneous pain and diarrhea, encouraging evidence exists that warrants further investigation in rigorous trials. Single studies reported some positive intergroup differences for spinal cord injury, Cushing’s syndrome, lung function, hepatitis, and rumen acidosis. These trials require independent replication. On the basis of the findings of this systematic review, there is no compelling evidence to recommend or reject acupuncture for any condition in domestic animals. Some encouraging data do exist that warrant further investigation in independent rigorous trials.
This evidence is in sharp contrast to the misinformation published by the ‘IVAS’ (International Veterinary Acupuncture Society). Under the heading “For Which Conditions is Acupuncture Indicated?“, they propagate the following myth:
Acupuncture is indicated for functional problems such as those that involve paralysis, noninfectious inflammation (such as allergies), and pain. For small animals, the following are some of the general conditions which may be treated with acupuncture:
- Musculoskeletal problems, such as arthritis, intervertebral disk disease, or traumatic nerve injury
- Respiratory problems, such as feline asthma
- Skin problems such as lick granulomas and allergic dermatitis
- Gastrointestinal problems such as diarrhea
- Selected reproductive problems
For large animals, acupuncture is again commonly used for functional problems. Some of the general conditions where it might be applied are the following:
- Musculoskeletal problems such as sore backs or downer cow syndrome
- Neurological problems such as facial paralysis
- Skin problems such as allergic dermatitis
- Respiratory problems such as heaves and “bleeders”
- Gastrointestinal problems such as nonsurgical colic
- Selected reproductive problems
In addition, regular acupuncture treatment can treat minor sports injuries as they occur and help to keep muscles and tendons resistant to injury. World-class professional and amateur athletes often use acupuncture as a routine part of their training. If your animals are involved in any athletic endeavor, such as racing, jumping, or showing, acupuncture can help them keep in top physical condition.
And what is the conclusion?
Perhaps this?
Never trust the promotional rubbish produced by SCAM organizations.
This story made the social media recently:
 Yes, I can well believe that many chiros are daft enough to interpret the incident in this way. Yet I think it’s a lovely story, not least because it reminds me of one of my own experiences:
Yes, I can well believe that many chiros are daft enough to interpret the incident in this way. Yet I think it’s a lovely story, not least because it reminds me of one of my own experiences:
I was on a plane to Toronto and had fallen asleep after a good meal and a few glasses of wine when a stewardess woke me saying: “We think you are a doctor!?”
“That’s right, I am a professor of alternative medicine”, I said trying to wake up.
“We have someone on board who seems to be dying. Would you come and have a look? We moved him into 1st class.”
Arrived in 1st class, she showed me the patient and a stethoscope. The patient was unconscious and slightly blue in the face. I opened his shirt and used the stethoscope only to find that this device is utterly useless on a plane; the sound of the engine by far overwhelms anything else. With my free hand, I tried to find a pulse – without success! Meanwhile, I had seen a fresh scar on the patient’s chest with something round implanted underneath. I concluded that the patient had recently had a pacemaker implant. Evidently, the electronic device had malfunctioned.
At this stage, two stewardesses were pressing me: “The captain needs to know now whether to prepare for an emergency stop in Newfoundland or to fly on. It is your decision.”
I had problems thinking clearly. What was best? The patient was clearly dying and there was nothing I could do about it. I replied by asking them to give me 5 minutes while I tried my best. But what could I do? I decided that I could do nothing but hold the patient’s hand and let him die in peace.
The Stewardesses watched me doing this and must have thought that I was trying some sort of energy healing, perhaps Reiki. This awkward situation continued for several minutes until – out of the blue – I felt a regular, strong pulse. Evidently, the pacemaker had started functioning again. It did not last long until the patient’s color turned pink and he began to talk. I instructed the pilot to continue our path to Toronto.
After I had remained with the patient for another 10 minutes or so, the Stewardesses came and announced: “We have moved your things into 1st class; like this, you can keep an eye on him.” The rest of the journey was uneventful – except the Stewardesses came repeatedly giving me bottles of champagne and fine wine to take with me into Toronto. And each time they politely asked whether my healing method would not also work for the various ailments they happened to suffer from – varicose veins, headache, PMS, fatigue …
So, here is my message to all the fellow energy healers out there:
We honor the creator’s design.
We know of the potential of the body is limitless.
Remember, you did not choose energy healing.
Energy healing chose you.
You were called for a time like this.
In case you are beginning to wonder whether I have gone round the bend, the answer is NO! I am not an energy healer. In fact, I am as much NOT an energy healer, as the chiropractor in the above story has NOT saved the life of his patient. Chiropractors and stewardesses, it seems to me, have one thing in common: they do not understand much about medicine.
PS
On arrival in Toronto, the patient was met by a team of fully equipped medics. I explained what had happened and they took him off to the hospital. As far as I know, he made a full recovery after the faulty pacemaker had been replaced. After my return to the UK, British Airways sent me a huge hamper to thank me.
There is a lack of data describing the state of naturopathic or complementary veterinary medicine in Germany. This survey maps the currently used treatment modalities, indications, existing qualifications, and information pathways. It records the advantages and disadvantages of these medicines as experienced by veterinarians. Demographic influences are investigated to describe the distributional impacts of using veterinary naturopathy and complementary medicine.
A standardized questionnaire was used for the cross-sectional survey. It was distributed throughout Germany in a written and digital format from September 2016 to January 2018. Because of the open nature of data collection, the return rate of questionnaires could not be calculated. To establish a feasible timeframe, active data collection stopped when the previously calculated limit of 1061 questionnaires was reached.
With the included incoming questionnaires of that day, a total of 1087 questionnaires were collected. Completely blank questionnaires and those where participants did not meet the inclusion criteria were not included, leaving 870 out of 1087 questionnaires to be evaluated. A literature review and the first test run of the questionnaire identified the following treatment modalities:
- homeopathy,
- phytotherapy,
- traditional Chinese medicine (TCM),
- biophysical treatments,
- manual treatments,
- Bach Flower Remedies,
- neural therapy,
- homotoxicology,
- organotherapy,
- hirudotherapy.
These were included in the questionnaire. Categorical items were processed using descriptive statistics in absolute and relative numbers based on the population of completed answers provided for each item. Multiple choices were possible.
Overall 85.4% of all the questionnaire participants used naturopathy and complementary medicine. The treatments most commonly used were:
- complex homoeopathy (70.4%, n = 478),
- phytotherapy (60.2%, n = 409),
- classic homoeopathy (44.3%, n = 301),
- biophysical treatments (40.1%, n = 272).
The most common indications were:
- orthopedic (n = 1798),
- geriatric (n = 1428),
- metabolic diseases (n = 1124).
Over the last five years, owner demand for naturopathy and complementary treatments was rated as growing by 57.9% of respondents (n = 457 of total 789). Veterinarians most commonly used scientific journals and publications as sources for information about naturopathic and complementary contents (60.8%, n = 479 of total 788). These were followed by advanced training acknowledged by the ATF (Academy for Veterinary Continuing Education, an organisation that certifies independent veterinary continuing education in Germany) (48.6%, n = 383). The current information about naturopathy and complementary medicine was rated as adequate or nearly adequate by many (39.5%, n = 308) of the respondents.
The most commonly named advantages in using veterinary naturopathy and complementary medicine were:
- expansion of treatment modalities (73.5%, n = 566 of total 770),
- customer satisfaction (70.8%, n = 545),
- lower side effects (63.2%, n = 487).
The ambiguity and unclear evidence of the mode of action and effectiveness (62.1%, n = 483) and high expectations of owners (50.5%, n = 393) were the disadvantages mentioned most frequently. Classic homoeopathy, in particular, has been named in this context (78.4%, n = 333 of total 425). Age, gender, and type of employment showed a statistically significant impact on the use of naturopathy and complementary medicine by veterinarians (p < 0.001). The university of final graduation showed a weaker but still statistically significant impact (p = 0.027). Users of veterinary naturopathy and complementary medicine tended to be older, female, self-employed and a higher percentage of them completed their studies at the University of Berlin. The working environment (rural or urban space) showed no statistical impact on the veterinary naturopathy or complementary medicine profession.
The authors concluded that this is the first study to provide German data on the actual use of naturopathy and complementary medicine in small animal science. Despite a potential bias due to voluntary participation, it shows a large number of applications for various indications. Homoeopathy was mentioned most frequently as the treatment option with the most potential disadvantages. However, it is also the most frequently used treatment option in this study. The presented study, despite its restrictions, supports the need for a discussion about evidence, official regulations, and the need for acknowledged qualifications because of the widespread application of veterinary naturopathy and complementary medicine. More data regarding the effectiveness and the mode of action is needed to enable veterinarians to provide evidence-based advice to pet owners.
I can only hope that the findings are seriously biased and not a true reflection of the real situation. The methodology used for recruiting participants (it is fair to assume that those vets who had no interest in SCAM did not bother to respond) strongly indicates that this might be the case. If, however, the findings were true, one would have to conclude that, for German vets, evidence-based healthcare is still an alien concept. The evidence that the preferred SCAMs are effective for the listed conditions is very weak or even negative. If the findings were true, one would need to wonder how much of veterinary SCAM use amounts to animal abuse.