causation
Cannabis use is a frequently-discussed subject, not just in the realm of so-called alternative medicine (SCAM). In general, SCAM advocates view it as an herbal medicine and recommend it for all sorts of conditions. They also often downplay the risks associated with cannabis use. Yet, these risks might be substantial.
Cannabis potency, defined as the concentration of Δ9-tetrahydrocannabinol (THC), has increased internationally, which could increase the risk of adverse health outcomes for cannabis users. The first systematic review of the association of cannabis potency with mental health and addiction was recently published in ‘The Lancet Psychiatry’.
The authors searched Embase, PsycINFO, and MEDLINE (from database inception to Jan 14, 2021). Included studies were observational studies of human participants comparing the association of high-potency cannabis (products with a higher concentration of THC) and low-potency cannabis (products with a lower concentration of THC), as defined by the studies included, with depression, anxiety, psychosis, or cannabis use disorder (CUD).
Of 4171 articles screened, 20 met the eligibility criteria:
- eight studies focused on psychosis,
- eight on anxiety,
- seven on depression,
- and six on CUD.
Overall, higher potency cannabis, relative to lower potency cannabis, was associated with an increased risk of psychosis and CUD. Evidence varied for depression and anxiety. The association of cannabis potency with CUD and psychosis highlights its relevance in healthcare settings, and for public health guidelines and policies on cannabis sales.
The authors concluded that standardisation of exposure measures and longitudinal designs are needed to strengthen the evidence of this association.
The fact that cannabis use increases the risk of psychosis has long been general knowledge. The notion that the risk increases with increased potency of cannabis seems entirely logical and is further supported by this systematic review. Perhaps it is time to educate the public and make cannabis users more aware of these risks, and perhaps it is time that SCAM proponents negate the harm cannabis can do.
Reports of serious complications of chiropractic manipulation keep on coming. Take this one, for instance:
My daughter went for a routine chiropractor appointment. Now she’s paralysed – 1:20 000 chiropractic neck manipulations result in stroke from vertebral artery dissection.
Or take a recent article by US neurosurgeons:
Cranio-cervical artery dissection (CeAD) is a common cause of cerebrovascular events in young subjects with no clear treatment strategy established. This study evaluated the incidence of major adverse cardiovascular events (MACE) in CeAD patients treated with and without stent placement. COMParative effectiveness of treatment options in cervical Artery diSSection (COMPASS) is a single high-volume center observational, retrospective longitudinal registry that enrolled consecutive CeAD patients over a 2-year period. Patients were ≥ 18 years of age with confirmed extra- or intracranial CeAD on imaging. Enrolled participants were followed for 1 year evaluating MACE as the primary endpoint.
One-hundred ten patients were enrolled (age 53 ± 15.9, 56% Caucasian, and 50% male, BMI 28.9 ± 9.2). Grade I, II, III, and IV blunt vascular injury was noted in 16%, 33%, 19%, and 32%, respectively. Predisposing factors were noted in the majority (78%), including
- sneezing,
- carrying a heavy load,
- chiropractic manipulation.
Stent was placed in 10 (10%) subjects (extracranial carotid n = 9; intracranial carotid n = 1; extracranial vertebral n = 1) at the physician’s discretion along with medical management. Reasons for stent placement were early development of high-grade stenosis or expanding pseudoaneurysm. Stented patients experienced no procedural or in-hospital complications and no MACE between discharge and 1 year follow up. CeAD patients treated with medical management only had 14% MACE at 1 year.
The authors concluded that in this single high-volume center cohort of CeAD patients, stenting was found to be beneficial, particularly with development of high-grade stenosis or expanding pseudoaneurysm. These results warrant confirmation by a randomized clinical trial.
Yes, I know: this study was not meant to investigate the link between chiropractic manipulations and CeAD. The finding that chiropractic manipulation is a predisposing factor for CeAD is entirely incidental. But it is an important finding nevertheless.
Chiropractors will laugh about the notion that manipulation is a risk factor akin to sneezing and thus try to trivialize the danger of their treatments. I would then point out that sneezing is unavoidable and fulfills a purpose. Chiropractic manipulations do neither.
Placebo effects are a fascinating subject. In so-called alternative medicine (SCAM), they are particularly important because much of SCAM seems to rely on little more than placebo effects. Therefore, I think this new paper is of some relevance to us.
The aim of this systematic review was to quantify the placebo effect of intraarticular injections for knee osteoarthritis in terms of pain, function, and objective outcomes. Factors influencing placebo effect were investigated.
Out of 2,363 records, 50 articles on 4,076 patients were included. The meta-analysis showed significant improvements up to the 6-month follow-up: Visual Analogue Scale (VAS)-pain −13.4 mean difference (MD) (95% confidence interval [CI]: −21.7/−5.1; P < 0.001), Western Ontario and McMaster Osteoarthritis Index (WOMAC)-pain −3.3 MD (95% CI: −3.9/−2.7; P < 0.001). Other significant improvements were WOMAC-stiffness −1.1 MD (95% CI: −1.6/−0.6; P < 0.001), WOMAC-function −10.1 MD (95% CI: −12.2/−8.0; P < 0.001), and Evaluator Global Assessment −21.4 MD (95% CI: −29.2/−13.6; P < 0.001). The responder rate was 52% (95% CI: 40% to 63%). Improvements were greater than the “minimal clinically important difference” for all outcomes (except 6-month VAS-pain). The level of evidence was moderate for almost all outcomes.
The authors concluded that the placebo effect of knee injections is significant, with functional improvements lasting even longer than those reported for pain perception. The high, long-lasting, and heterogeneous effects on the scales commonly used in clinical trials further highlight that the impact of placebo should not be overlooked in the research on and management of knee osteoarthritis.
The authors furthermore confirmed that “the main finding of this meta-analysis is that placebo is an important component of the effect of injective treatments for patients with KOA, with saline injections being able to provide relevant and long-lasting results not only in terms of pain relief but also with respect to stiffness resolution and function improvement. These results are both statistically and clinically significant and can be perceived by patients up to 6 months.”
I would dispute that!
To explain why it might help to read our 1995 BMJ paper on the subject:
We often and wrongly equate the response seen in the placebo arm of a clinical trial with the placebo effect. In order to obtain the true placebo effect, other non-specific effects can be identified by including an untreated control group in clinical trials. A review of the literature shows that most authors confuse the perceived placebo effect with the true placebo effect. The true placebo effect is highly variable, depending on several factors that are not fully understood. A distinction between the perceived and the true placebo effects would be helpful in understanding the complex phenomena involved in a placebo response.
In other words, what the authors picked up in their analysis (i.e. the changes that occurred in the placebo groups between the start of a trial and after placebo application) is not just the placebo response; it is, in fact, a combination of a placebo effect, concomitant interventions/care, regression towards the mean, natural history of the condition and possibly other factors.
Does it matter?
Yes, it does!
Placebo effects are not nearly as powerful and long-lasting as the authors conclude. And this means virtually all their implications for clinical practice are incorrect.
The ‘My Resilience in Adolescence (MYRIAD) Trial’evaluated the effectiveness and cost-effectiveness of SBMT compared with teaching-as-usual (TAU).
MYRIAD was a parallel group, cluster-randomised controlled trial. Eighty-five eligible schools consented and were randomized 1:1 to TAU (43 schools, 4232 students) or SBMT (42 schools, 4144 students), stratified by school size, quality, type, deprivation, and region. Schools and students (mean (SD); age range=12.2 (0.6); 11–14 years) were broadly UK population-representative. Forty-three schools (n=3678 pupils; 86.9%) delivering SBMT, and 41 schools (n=3572; 86.2%) delivering TAU, provided primary end-point data. SBMT comprised 10 lessons of psychoeducation and mindfulness practices. TAU comprised standard social-emotional teaching. Participant-level risk for depression, social-emotional-behavioural functioning and well-being at 1 year follow-up were the co-primary outcomes. Secondary and economic outcomes were included.
 An analysis of the data from 84 schools (n=8376 participants) found no evidence that SBMT was superior to TAU at 1 year. Standardised mean differences (intervention minus control) were: 0.005 (95% CI −0.05 to 0.06) for risk for depression; 0.02 (−0.02 to 0.07) for social-emotional-behavioural functioning; and 0.02 (−0.03 to 0.07) for well-being. SBMT had a high probability of cost-effectiveness (83%) at a willingness-to-pay threshold of £20 000 per quality-adjusted life year. No intervention-related adverse events were observed.
An analysis of the data from 84 schools (n=8376 participants) found no evidence that SBMT was superior to TAU at 1 year. Standardised mean differences (intervention minus control) were: 0.005 (95% CI −0.05 to 0.06) for risk for depression; 0.02 (−0.02 to 0.07) for social-emotional-behavioural functioning; and 0.02 (−0.03 to 0.07) for well-being. SBMT had a high probability of cost-effectiveness (83%) at a willingness-to-pay threshold of £20 000 per quality-adjusted life year. No intervention-related adverse events were observed.
The authors concluded that the findings do not support the superiority of SBMT over TAU in promoting mental health in adolescence.
Even though the results are negative, MYRIAD must be praised for its scale and rigor, and for highlighting the importance of large, well-designed studies before implementing measures of this kind on a population basis. Co-author Tim Dalgliesh, director of the Cambridge Centre for Affective Disorders, said: “For policymakers, it’s not just about coming up with a great intervention to teach young people skills to deal with their stress. You also have to think about where that stress is coming from in the first place.”
“There had been some hope for an easy solution, especially for those who might develop depression,” says Til Wykes, head of the School of Mental Health and Psychological Sciences at the Institute of Psychiatry, Psychology, and Neuroscience, King’s College London. “There may be lots of reasons for developing depression, and these are probably not helped by mindfulness,” she says. “We need more research on other potential factors that might be modified, and perhaps this would provide a more targeted solution to this problem.”
Personally, I feel that mindfulness has been hyped in recent years. Much of the research that seemed to support it was less than rigorous. What is now needed is a realistic approach based on sound evidence and critical thinking.
Third molar extraction is a painful treatment and thus is often used to investigate the effects of analgesics on pain. Hypnotherapy is said to help to reduce pain and to decrease the intake of postoperative systemic analgesics. Therefore, it seems reasonable to study the effects of hypnotherapy on the pain caused by third molar extraction.
In this study, the effectiveness of a brief hypnotic induction for patients undergoing third molar extractions was investigated. Data were collected from 33 patients with third molar extractions on the right and left sides. Patients received two different types of interventions in this monocentric randomized crossover trial. Third molar extraction was conducted on one side with reduced preoperative local anesthetics and an additional brief hypnotic induction (Dave Elman technique). The other side was conducted with regular preoperative local anesthetics without a brief hypnotic induction (standard care). Intake of postoperative systemic analgesics was allowed in both treatments.
Patients’ expectations about hypnosis were assessed at baseline. The primary outcome was the area under the curve with respect to ground of pain intensity after the treatment. Secondary outcomes were the amount of postoperative analgesics consumed and the preferred treatment.
There was no evidence that the area under the curve with respect to ground of pain differed between the two interventions (controlling for gender). There was, however, evidence to show that the patients’ expectations affected the effectiveness of the brief hypnotic induction. This means that patients with high expectations about hypnosis benefit more from treatment with reduced preoperative local anesthetics and additional brief hypnotic induction.
The authors concluded that, in this study, additional a brief hypnotic induction with reduced preoperative local anesthetic use did not generally reduce posttreatment pain after third molar extraction more than regular local anesthetics. The expectation of the patients about the effectiveness of hypnosis affected the effectiveness of the brief hypnotic induction so that patients with high expectations had a larger benefit from a brief hypnotic induction than patients with low expectations.
The most interesting findings here are, in my view, that:
- Hypnotherapy is not as effective as many enthusiasts claim.
- Expectation influences the outcome of hypnotherapy.
Expectation is, of course, a determinant of the size of the placebo response. Thus, this finding is interesting but far from unexpected. I would go as far as postulating that similar results would be obtained with most treatments regardless of whether they are alternative or conventional. The difference is that, in the case of alternative therapies, the expectation is a major (if not the only) determinant of the outcome, while it merely somewhat improves the outcome of an effective treatment. To put it differently, so-called alternative medicine (SCAM) relies entirely/mostly on expectation, while conventional medicine does not.
Earlier this year, I started the ‘WORST PAPER OF 2022 COMPETITION’. You will ask what is there to win in this competition? I agree: a competition without a prize is no fun. Therefore, I suggest offering the winner (that is the author of the winning paper) one of my books that best fits his/her subject. I am sure this will over-joy him or her. And how do we identify the winner? I suggest that I continue blogging about nominated papers (I hope to identify about 10 in total), and towards the end of the year, I let my readers decide democratically.
In this spirit of democratic voting, let me suggest to you ENTRY No 6:
This study was to ascertain the efficacy of dry cupping therapy (DCT) and optimal cup application time duration for cervical spondylosis (CS). It was designed as a randomized clinical trial involving 45 participants with clinically diagnosed CS. The eligible subjects were randomly allocated into three groups, each having 15 participants. Each of the three groups, i.e., A, B, and C, received DCT daily for 15 days for 8 min, 10 min, and 12 min, respectively. All the participants were evaluated at the baseline, 7th, and 15th day of the trial using the neck disability index (NDI) as well as the visual analog scale (VAS).
The baseline means ± SD of NDI and VAS scores were significantly reduced in all three groups at the end of the trial. Although all three groups were statistically equal in terms of NDI, group C demonstrated greater efficacy in terms of VAS.
The authors concluded that the per-protocol analysis showed that dry cupping effectively alleviated neck pain across all treatment groups. Although this effect on neck disability index was statistically equal in all three groups, the 12-min protocol was more successful in reducing pain.
Who would design such a study and why?
- The authors claim they wanted to ascertain the efficacy of DCT. A trial is for testing, not ascertaining. And this study does certainly not test for efficacy.
- The groups were too small to generate a meaningful result of what, in fact, was an equivalence study.
- Intra-group changes in symptoms between baseline and time points during treatment are irrelevant in a controlled trial.
- The slightly better results of group C are most likely due to chance or non-specific effects (a longer application of a placebo would generate better outcomes that a shorter one).
- The study participants had cervical spondylosis, yet the conclusion is about neck pain. The two are not identical.
- The title of the paper promises that we learn something about the safety of DCT. Sadly, a trial with just 45 patients has no chance in hell to pick up adverse effects in a reliable way.
- As there is no control group, the study cannot tell us anything about possible specific effects of DCT.
The authors of the study have impressive affiliations:
- Department of Ilaj bil Tadbir, Luqman Unani Medical College Hospital and Research Center, Bijapur, India.
- Department of Ilaj bil Tadbir, National Institute of Unani Medicine, Bengaluru, India.
- Department of Moalajat, Luqman Unani Medical College Hospital and Research Center, Bijapur, India.
I would have hoped that researchers from national institutions and medical colleges should be able to design a trial that has at least a small chance to produce a meaningful finding. As it turns out, my hope was badly disappointed.
On 18/7/2022 the ‘WORLD FEDERATION OF CHIROPRACTIC’ published a statement on cervical artery dissection (CAD). Below are a few excerpts to which I have added a few numbers [in brackets] which refer to my comments below:
… On rare occasions, CAD has been reported to have occurred after a patient visited a chiropractor or other provider of manual therapy [1]. However, the best evidence available to date indicates that spinal manipulation does not stress the arteries enough to cause tearing of the arteries leading to dissection-related strokes [2]. Additional studies have concluded that patients are as likely to have consulted a primary care physician as receive spinal manipulation from a chiropractor prior to experiencing a CAD-related stroke [3]…
The provision of safe, high-quality, evidence-based, patient-centered care for these and other conditions is a priority for the chiropractic profession [4]. Rigorous research is core to the pursuit of that objective [5]. We urge caution in making claims that are in conflict with the current state of the evidence.
About the WFC
The World Federation of Chiropractic is an international, non-governmental organization whose members are the national associations of over 90 countries in seven world regions. It is a non-state actor in official relations with the World Health Organization and is the global authority for matters related to the chiropractic profession [6]…
References
Cassidy JD, Boyle E, Côté P, He Y, Hogg-Johnson S, Silver FL, Bondy SJ. Risk of Vertebrobasilar Stroke and Chiropractic Care: Results of a Population-Based Case-Control and Case-Crossover Study. Eur Spine J. 2008 Apr;17(Suppl 1):176–83. Open access here.#
Chaibi A, Russell MB. A risk-benefit assessment strategy to exclude cervical artery dissection in spinal manual-therapy: a comprehensive review. Ann Med. 2019 Mar;51(2):118-127. Open access here.
Church EW, Sieg EP, Zalatimo O, Hussain NS, Glantz M, Harbaugh RE. Systematic Review and Meta-analysis of Chiropractic Care and Cervical Artery Dissection: No Evidence for Causation. Cureus. 2016 Feb 16;8(2):e498. Open access here.
Kosloff TM, Elton D, Tao J, Bannister WM. Chiropractic care and the risk of vertebrobasilar stroke: results of a case-control study in U.S. commercial and Medicare Advantage populations. Chiropr Man Therap. 2015 Jun 16;23:19. Open access here.
Rubinstein SM, Peerdeman SM, van Tulder MW, Riphagen I, Haldeman S. A systematic review of the risk factors for cervical artery dissection. Stroke. 2005 Jul;36(7):1575-80. Open access here.
Whedon JM, Mackenzie TA, Phillips RB, Lurie JD. Risk of traumatic injury associated with chiropractic spinal manipulation in Medicare Part B beneficiaries aged 66 to 99 years. Spine (Phila Pa 1976). 2015 Feb 15;40(4):264-70. Open access here
Here are my brief comments based on the evidence discussed in dozens of posts previously published on this blog:
- As there is no post-marketing surveillance, nobody can say with any degree of confidence that CADs after chiropractic are rare.
- This is not the ‘best’ evidence. In fact, it has been refuted repeatedly.
- This study has also been refuted.
- Chiropractic is very far from being evidence-based.
- Rigorous research fails to show that chiropractic neck manipulations generate more good than harm.
- The WFC is a lobby group for chiropractic; its mission is ” to advance awareness, utilization, and integration of chiropractic internationally”. Its current director is Richard Brown who spear-headed the disaster when the BCA sued Simon Singh, lost, and caused immense reputational damage to chiropractic worldwide.
Ischemic heart disease (IHD) related to cardiovascular or cerebrovascular disease is the leading cause of mortality and an important issue of public health worldwide. The cost of long-term healthcare for IHD patients may result in a huge financial burden. This study analyzed the medical expenditure incurred for and survival of IHD patients treated with Chinese herbal medicine (CHM) and Western medicine.
Subjects were randomly selected from the National Health Insurance Research Database in Taiwan. The Cox proportional hazards regression model, Kaplan–Meier estimator, logrank test, chi-square test, and analysis of variance were applied. Landmark analysis was used to assess the cumulative incidence of death in IHD patients.
A total of 11,527 users were identified as CHM combined with Western medicine and 11,527 non-CHM users. CHM users incurred a higher medical expenditure for outpatient care within 1 (24,529 NTD versus 18,464 NTD, value <0.0001) and 5 years (95,345 NTD versus 60,367 NTD, value <0.0001). However, CHM users had shorter hospitalizations and lower inpatient medical expenditure (7 days/43,394 NTD in 1 year; 11 days/83,141 NTD in 5 years) than non-CHM users (11 days/72,939 NTD in 1 year; 14 days/107,436 NTD in 5 years).
The CHM group’s adjusted hazard ratio for mortality was 0.41 lower than that of the non-CHM group by Cox proportional hazard models with time-dependent exposure covariates. Danshen, Huang qi, Niu xi, Da huang, and Fu zi were the most commonly prescribed Chinese single herbs; Zhi-Gan-Cao-Tang, Xue-Fu-Zhu-Yu-Tang, Tian-Wang-Bu-Xin-Dan, Sheng-Mai-San, and Yang-Xin-Tang were the five most frequently prescribed herbal formulas in Taiwan.
The authors concluded that combining Chinese and Western medicine can reduce hospital expenditure and improve survival for IHD patients.
Why, you will ask, do I think that this study deserves to be in the ‘worst paper cometition’?
It is not so bad!
It is an epidemiological case-control study with a large sample size that generates interesting findings.
Agreed!
But, as a case-control study, it cannot establish a causal link between CHM and the outcomes. You might argue that the conclusions avoid doing this – “can … improve survival” is not the same as “does improve survival”. This may be true, yet the title of the article leaves little doubt about the interpretation of the authors:
Chinese Herbal Medicine as an Adjunctive Therapy Improves the Survival Rate of Patients with Ischemic Heart Disease: A Nationwide Population-Based Cohort Study
I find it difficult not to view this as a deliberate attempt of the authors, editors, and reviewers to mislead the public.
Looking at the details of the study, it is easy to see that the two groups were different in a whole range of parameters that were measured. More importantly, they most likely differ in a range of variables that were not measured and had significant influence on IHD survival. It stands to reason, for instance, that patients who elected to use CHM in addition to their standard care were more health conscious. They would thus have followed a healthier diet and lifestyle. It would be foolish to claim that such factors do not influence IHD survival.
The fact that the authors fail even to mention this possibility, interpret an association as a causal link, and thus try to mislead us all makes this paper, in my view, a strong contender for my
WORST PAPER OF 2022 COMPETITION
A study by an international team of researchers estimated the proportion of healthcare interventions tested within Cochrane Reviews that are effective according to high-quality evidence.
They selected a random sample of 2428 (35%) of all Cochrane Reviews published between 1 January 2008 and 5 March 2021 and extracted data about interventions within these reviews that were compared with placebo, or no treatment, and whose outcome quality was rated using Grading of Recommendations Assessment, Development and Evaluation (GRADE). They then calculated the proportion of interventions whose effectiveness was based on high-quality evidence according to GRADE, had statistically significant positive effects and were judged as beneficial by the review authors. They also calculated the proportion of interventions that suggested harm.
Of 1567 eligible interventions, 87 (5.6%) had high-quality evidence on first-listed primary outcomes, positive, statistically significant results, and were rated by review authors as beneficial. Harms were measured for 577 (36.8%) interventions, 127 of which (8.1%) had statistically significant evidence of harm. Our dependence on the reliability of Cochrane author assessments (including their GRADE assessments) was a potential limitation of our study. 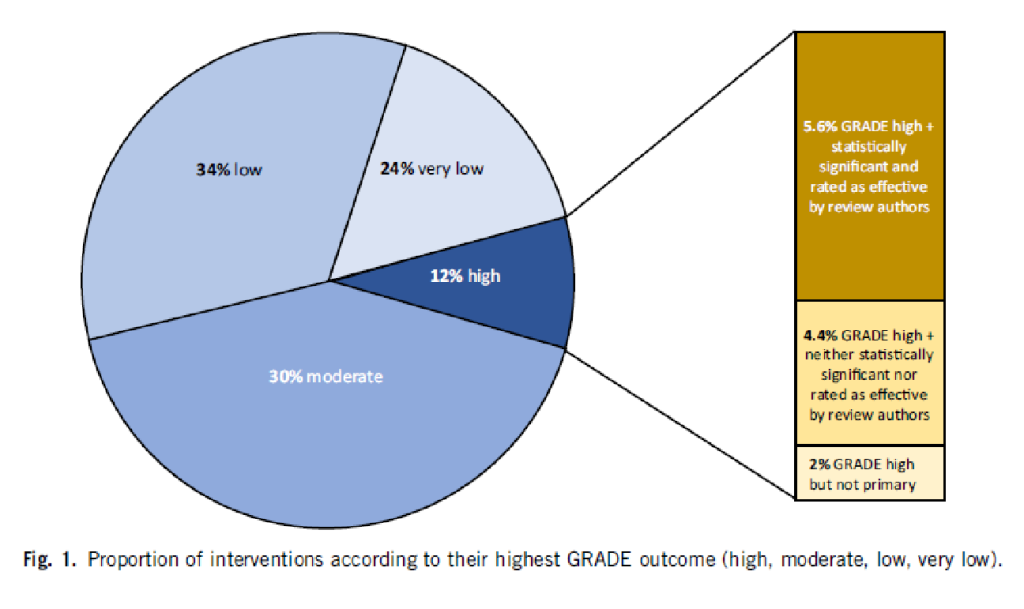
The authors drew the following conclusions: While many healthcare interventions may be beneficial, very few have high-quality evidence to support their effectiveness and safety. This problem can be remedied by high-quality studies in priority areas. These studies should measure harms more frequently and more rigorously. Practitioners and the public should be aware that many frequently used interventions are not supported by high-quality evidence.
Proponents of so-called alternative medicine (SCAM) are fond of the ‘strawman’ fallacy; meaning they like to present a picture of conventional medicine that is overtly negative in order for SCAM to appear more convincing (Prince Charles, for instance, uses this trick every single time he speaks about SCAM). Therefore I am amazed that this paper has not been exploited in that way by them. I was expecting headlines such as
Evidence-based medicine is not supported by evidence
or
Less than 6% of all conventional treatments are supported by sound evidence.
etc.
Why did they not have a field day with this new paper then?
As the article is behind a paywall, it took me a while to get the full paper (thanks Paul). Now that I have read it, I think I understand the reason.
In the article, the authors provide figures for specific types of treatments. Let me show you some of the percentages of interventions that met the primary outcome (high quality, statistically significant effect, and authors interpret as effective):
- pharmacological 73.8%
- surgical 4.6%
- exercise 5.8%
- diet 1.2%
- alternative 0.0%
- manual therapies 0.0%
So, maybe the headlines should not be any of the above but:
No good evidence to support SCAM?
or
SCAM is destroying the evidence base of medicine.
An epidemiological study from the US just published in the BMJ concluded that “the mortality gap in Republican voting counties compared with Democratic voting counties has grown over time, especially for white populations, and that gap began to widen after 2008.”
In a BMJ editorial, Steven Woolf comments on the study and provides further evidence on how politics influence health in the US. Here are his concluding two paragraphs:
Political influence on US mortality rates became overt during the covid-19 pandemic, when public health policies, controlled by states, were heavily influenced by party affiliation. Republican politicians, often seeking to appeal to President Trump and his supporters, challenged scientific evidence and opposed enforcement of vaccinations and safety measures such as masking. A macabre natural experiment occurred in 2021, a year marked by the convergence of vaccine availability and contagious variants that threatened unvaccinated populations: states led by governors who promoted vaccination and mandated pandemic control measures experienced much lower death rates than the “control” group, consisting of conservative states with lax policies and large unvaccinated populations. This behavior could explain why US mortality rates associated with covid-19 were so catastrophic, vastly exceeding losses in other high income countries.
Observers of health trends in the US should keep their eye on state governments, where tectonic shifts in policy are occurring. While gridlock in Washington, DC incapacitates the federal government, Republican leaders in dozens of state capitols are passing laws to undermine health and safety regulations, ban abortion, limit LGBT+ rights, and implement more conservative policies on voting, school curriculums, and climate policy. To understand the implications for population health, researchers must break with custom; although scientific literature has traditionally avoided discussing politics, the growing influence of partisan affiliation on policies affecting health makes this covariate an increasingly important subject of study.
_____________________
What has this to do with so-called alternative medicine (SCAM)?
Not a lot.
Except, of course, that Trump has been quite sympathetic to both quackery and quacks (see, for instance, here and here). Moreover, the embarrassing Dr. Oz, America’s charlatan-in-chief, is now a Republican candidate for the US senate. And the creation of the NHI office for alternative medicine, currently called NCCIH, was the idea of the Republican senator, Tom Harkin.
I think we get the drift: on the US political level, SCAM seems to be a right-wing thing.
Am I claiming that SCAM is the cause of the higher mortality in Republican counties?
No.
Do I feel that both are related to irresponsible attitudes towards healthcare issues?
Yes.


