bogus claims
Many people believe that homeopathy is essentially plant-based – but they are mistaken! Homeopathic remedies can be made from anything: Berlin wall, X-ray, pus, excrement, dental plaque, mobile phone rays, poisons … anything you can possibly think of. So, why not from vaccines?
This is exactly what a pharmacist specialized in homeopathy thought.
It has been reported that the ‘Schloss-Apotheke’ in Koblenz, Germany offered for sale a homeopathic remedy made from the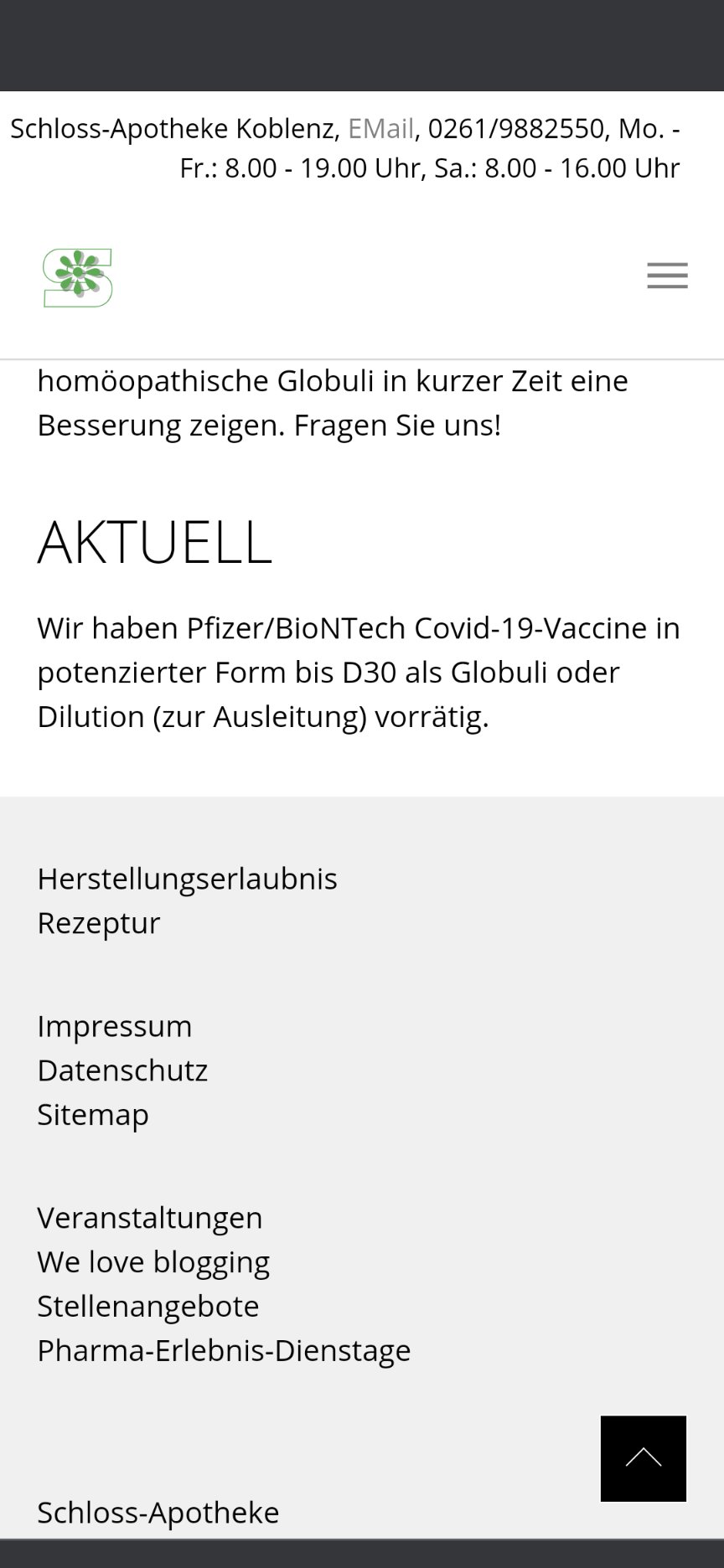 Pfizer vaccine. This has since prompted not only the Chamber of Pharmacists but also the Paul Ehrlich Institute and Pfizer to issue statements. On Friday (30/4/2021) morning, the pharmacy had advertised homeopathic remedies based on the Pfizer/Biontech vaccine. The Westphalia-Lippe Chamber of Pharmacists then issued an explicit warning against it. “We are stunned by this,” said a spokesman. The offer has since disappeared from the pharmacy’s website.
Pfizer vaccine. This has since prompted not only the Chamber of Pharmacists but also the Paul Ehrlich Institute and Pfizer to issue statements. On Friday (30/4/2021) morning, the pharmacy had advertised homeopathic remedies based on the Pfizer/Biontech vaccine. The Westphalia-Lippe Chamber of Pharmacists then issued an explicit warning against it. “We are stunned by this,” said a spokesman. The offer has since disappeared from the pharmacy’s website.
On Friday afternoon, the manufacturer of the original vaccine also intervened. The Paul Ehrlich Institute released a statement making it clear that a vaccine is only safe “if it is administered in accordance with the marketing authorization.”
The Schloss-Apotheke had advertised the product in question with the following words:
“We have Pfizer/BioNTech Covid-19-Vaccine in potentized form up to D30 as globules or dilution (for discharge) in stock.”
The chamber of pharmacists countered with a warming under the heading “Facts instead of Fake News” on Facebook and Instagram:
“Whatever they might contain: These remedies are no effective protection against Covid-19.”
Pharmacy manager, Annette Eichele, of the Schloss-Apotheke claimed she had not sold homeopathic Corona vaccines and stressed that effective vaccines of this kind do not exist. According to Eichele, only an additional “mini drop” of the original Biontech vaccine had been used and “highly potentized” and prepared homeopathically. According to Eichele, Corona vaccinations that had already been administered were thus to have a “better and more correct effect with this supplementary product, possibly without causing side effects … but this is not scientifically proven”. The homeopathic product had been produced only on customer request and had been sold less than a dozen times in the past weeks. Ten grams of the remedy were sold for about 15 Euros. On Twitter, Eichele stated: „Wir haben nichts Böses getan, wir wollten nur Menschen helfen!“ (We have done nothing evil, we only wanted to help people). I am reminded yet again of Bert Brecht who observed:
“The opposite of good is not evil but good intentions”.
Many chiropractors seem to view the present pandemic as a business opportunity and make no end of false claims to attract customers. This has now been outlawed in the US. Medscape reported that a US district court will decide whether a chiropractor who is charged with 10 counts of making false marketing claims related to COVID-19 will be the first person convicted under a new federal law.
On his website, chiropractor ‘Dr.’ Eric Neptune advertises his services as follows:
Have you ever been told by your medical doctor that you or a member of your family had a specific disease, syndrome, or sickness? Did your doctor then recommend a drug or surgery to fix the issue, or tell you that you would have to live with it for the rest of your life? If so, you are not alone!
Nepute Wellness Center is unlike any medical clinic you may have been to. The clinic team is focused on finding and fixing the CAUSE of your problem vs. seeking out and treating only the SYMPTOMS. Nepute Wellness Center is equipped with state-of-the-art diagnostic equipment and testing, as well as medical doctors, nurses, and chiropractors who have been uniquely trained to treat your whole body, regardless of age, and return your body to a healthy balance so that it can heal itself the way God intended.
If you are tired of trying to treat your symptoms using prescription and over-the-counter pills, or even considering surgery, then Nepute Wellness Center may be right for you! Or like many, you want to be proactive with your health and prevent sickness and disease before you begin to suffer any symptoms, allowing you to live the full life you deserve, then make Nepute Wellness Center your partner in health!
Already over a year ago, Eric Nepute, the owner of Quickwork, based in St. Louis, Missouri, managed to make headlines. He had recorded a video that racked up more than 21 million views and suggested that drinking tonic water would prevent COVID-19 infections. Now, Mr. Neptune is the first person charged by the Federal Trade Commission (FTC) under the new COVID- 19 Consumer Protection Act. His company which has several locations in St. Louis County advertised its vitamin D and zinc products on social media and the internet as drugs that could treat or prevent COVID-19 claiming that their products are “more effective than the available COVID-19 vaccines”.
The FTC warned Nepute’s company in May 2020 about making unsubstantiated claims for other products regarding efficacy against COVID-19 and advised him to immediately stop making claims that were not supported by scientific evidence. However, Nepute seemed undeterred.
The FTC is seeking to fine Nepute and Quickwork up to US$43,792 for each violation of the COVID-19 Consumer Protection Act. In addition, the FTC seeks to bar the company from making health claims unless they are true and can be substantiated by scientific evidence.
Through his attorney, Neptune told the local NBC TV news affiliate, “I feel that I have not done anything wrong. I encourage everyone to live a healthy lifestyle during this unprecedented time. My attorneys are reviewing the complaint and I have no further comments at this time.”
In 2008, the British Chiropractic Association sued Simon Singh because he disclosed that they were promoting chiropractic for infant colic. The BCA lost the case, plenty of money, and all its reputation. Ever since the issue is a very sore point for chiropractic pride. The data show that Simon was quite correct in stating that they are happily promoting bogus treatments without a jot of evidence. Here for instance is my systematic review:
Some chiropractors claim that spinal manipulation is an effective treatment for infant colic. This systematic review was aimed at evaluating the evidence for this claim. Four databases were searched and three randomised clinical trials met all the inclusion criteria. The totality of this evidence fails to demonstrate the effectiveness of this treatment. It is concluded that the above claim is not based on convincing data from rigorous clinical trials.
But chiropractors steadfastly refuse to accept defeat and keep on trying to find positive results. Now Danish chiropractors have made another attempt.
The purpose of this study is to evaluate the effect of chiropractic care on infantile colic. This multicenter, single-blind randomized controlled trial was conducted in four Danish chiropractic clinics, 2015–2019. Information was distributed in the maternity wards and by maternal and child health nurses. Children aged 2–14 weeks with unexplained excessive crying were recruited through home visits and randomized (1:1) to either chiropractic care or control group. Both groups attended the chiropractic clinic twice a week for 2 weeks. The intervention group received chiropractic care, while the control group was not treated. The parents were not present in the treatment room and unaware of their child’s allocation.
The primary outcome was change in daily hours of crying before and after treatment. Secondary outcomes were changes in hours of sleep, hours being awake and content, gastrointestinal symptoms, colic status and satisfaction. All outcomes were based on parental diaries and a final questionnaire.
Of 200 recruited children, 185 completed the trial (treatment group n = 96; control group n = 89). Duration of crying in the treatment group was reduced by 1.5 h compared with 1 h in the control group (mean difference − 0.6, 95% CI − 1.1 to − 0.1; P = 0.026), but when adjusted for baseline hours of crying, age, and chiropractic clinic, the difference was not significant (P = 0.066). The proportion obtaining a clinically important reduction of 1 h of crying was 63% in the treatment group and 47% in the control group (p = 0.037), and NNT was 6.5. We found no effect on any of the secondary outcomes.

The authors concluded that excessive crying was reduced by half an hour in favor of the group receiving chiropractic care compared with the control group, but not at a statistically significant level after adjustments. From a clinical perspective, the mean difference between the groups was small, but there were large individual differences, which emphasizes the need to investigate if subgroups of children, e.g. those with musculoskeletal problems, benefit more than others from chiropractic care.
This seems to be a rigorous trial. However, I don’t quite understand why the authors even mention that, before adjusting, the results seemed to favor chiropractic. This only makes a squarely negative study look positive! Why would anyone want to do that? Could this perhaps hint at a reason for this odd behavior? “The study was primarily funded by the Foundation for Chiropractic Research and Postgraduate Education.”
On 17/2/2020 I posted this article:
The drop in cases and deaths due to COVID-19 infections in India has been attributed to India’s national policy of using homeopathy. Early in the epidemic, the national “Ministry of AYUSH, recommended the use of Arsenic album 30 as preventive medicine against COVID-19. Its prophylactic use has been advised in states like Karnataka, Tamil Nadu, Kerala, and Maharashtra. The ‘OFFICIAL HOMEOPATHY RESOURCE’ is now claiming that homeopathy is the cause of the observed outcome…
If you click on the link, you will find that the OFFICIAL HOMEOPATHY RESOURCE has now removed the original. No problem! Thanks to Alan Henness, we can still access it; he announced in a tweet that he has archived a copy. So, here is the full article again:
India’s National Policy of Using Homeopathic Medicine To Prevent COVID is Dramatically Working
A dramatic plunge in cases and deaths of COVID in India can be attributed to India’s national policy of using homeopathy.
Early in the epidemic, the national “Ministry of AYUSH, (medical alternatives), in its guidelines, issued an advisory to states across India recommending the use of a traditional homeopathic drug, Arsenic album 30 as a form of preventive medicine against COVID-19. Its prophylactic use has been advised in states like Karnataka, Tamil Nadu, Kerala and Maharashtra and in some places, it has been used in high-risk areas. In places like Bhopal, claims were raised when doctors said that mild COVID cases were successfully treated with homeopathy.” [Times of India]
And now the results of that policy and use are clear, even though scientists in the conventional paradigm are mystified as to why the drop is so dramatic. They know nothing about homeopathy and its history of successfully treating epidemics.
India has a population of 1 billion, 300 million people. Relative to this massive population the number of cases per day and especially the number of deaths per day are now exceptionally low. According to the Daily Mail:
“Scientists are trying to work out why coronavirus cases in India are falling when at one point it looked like the country might overtake the US as the worst-hit nation.
In September the country was reporting some 100,00 new cases per day, but that went into decline in October and is now sitting at around 10,000 per day – leaving experts struggling to explain why.”


But why?
Why did the original disappear?
The reason seems obvious:
Saturday’s official toll recorded another 2,600 deaths and 340,000 new infections in India, bringing the total number of cases to 16.5 million, second only to the US. There have been 190,000 deaths attributed to Covid in India since the start of the pandemic. These figures are dramatic but most likely they are gross underestimates of the truth.
The egg on the face of homeopathy gets bigger if we consider things like the COVID-19 advice from ‘HOMEOPATHY INTERNATIONAL’, or the fact that UK’s biggest provider of homeopathy training encouraged the use of homeopathic potions made with phlegm to protect against and treat Covid-19. The egg finally turns into a veritable omelette, once we learn that the leading academic journal in homeopathy, HOMEOPATHY, promoted the idea that homeopathic have a place in the fight against the pandemic – not just once but repeatedly – and that the leading UK homeopath, Elizabeth Thompson, recommended homeopathy for COVID-19 infections after herself falling ill with the virus.
No, I do not feel the slightest tinge of Schadenfreude, about all this. I am writing about it because I still hope that it will prevent some people from risking their health with useless therapies and perhaps even stop some charlatans to make ridiculously irresponsible claims about them. So, please do me a favor and heed my message:
The promotion of homeopathy and other ineffective therapies costs many lives!
Indian homeopaths aimed at evaluating the efficacy of individualized homeopathy (IH) for atopic dermatitis (AD). They conducted a double-blind, randomized, placebo-controlled, short-term, preliminary trial in an Indian homeopathy hospital. Patients were randomized to either IH (n = 30) or identical-looking placebo (n = 30) using computerized randomization and allocation. Outcomes were patient-oriented scoring of AD (PO-SCORAD; primary endpoint), Dermatological Life Quality Index (DLQI) score, and AD burden score for adults (ADBSA; secondary endpoints), measured monthly for 3 months. An intention-to-treat sample was analyzed after adjusting baseline differences.
On PO-SCORAD, improvement was higher in IH against placebo, but nonsignificant statistically (pmonth 1 = 0.433, pmonth 2 = 0.442, pmonth 3 = 0.229). Secondary outcomes were also nonsignificant – both DLQI and ADBSA (p > 0.05). Four adverse events (diarrhea, injury, common cold) were recorded.
The authors concluded that there was a small, but nonsignificant direction of effect towards homeopathy, which renders the trial inconclusive. A properly powered robust trial is indicated.
Thee questions:
- Why use statistics only to ignore its results?
- Why discredit research into so-called alternative medicine (SCAM) in this way?
- Who on earth would publish such misleading conclusions?
This article was published in Complementary Medicine Research which claims to be an international peer-reviewed journal that aims to bridge the gap between conventional and complementary/alternative medicine on a sound scientific basis, promoting their mutual integration. It boasts that “experts of both conventional medicine and complementary/alternative medicine cooperate on the journal’s editorial board, ensuring a high standard of scientific quality”. Its editor is Harald Walach who we have met several times before.
I had a look at the long list of members of the editorial board and was unable to see many ‘experts in conventional medicine’. If that is so, the journal’s peer review process is bound to turn into a farcical procedure where any rubbish will pass.
The journal reminds authors that “published research must comply with internationally-accepted standards for research practice and reporting.” I believe that the internationally accepted standards of research reporting include something about not misleading the public by claiming that the absence of an effect is a small effect in favor of homeopathy. By revealing that there was no significant effect, the authors of this study demonstrate that IH was not effective as a treatment of AD. It is in my mind unethical to try to disguise this result by making it look like a small positive effect or claiming the result was inconclusive.
High standard of scientific quality?
No, quite the opposite!
Some time ago, I published ‘The 10 commandments of quackery’. Since then, I discovered that there are several errors that occur with such regularity in the comment section of this blog as well as in most other discussions about so-called alternative medicine (SCAM), that – in the hope to improve the logical reasoning of my readers (and often times my own) – it seems timely to publish the
10 ‘commandments’ of rational thought
- Thou shalt not confuse popularity of a therapy with its efficacy or safety (appeal to popularity).
- Thou shalt not assume that the test of time is a valid substitute for evidence (appeal to tradition).
- Thou shalt not believe that natural therapies are necessarily harmless (appeal to nature).
- Thou shalt not think that those who question your claim need to prove that you are wrong (reversal of the burden of proof).
- Thou shalt not assume that a therapy administered before a symptomatic improvement was necessarily the cause of that outcome (post hoc ergo propter hoc).
- Thou shalt not suppose that, because you do not know or understand an issue, it cannot be true (appeal to ignorance).
- Thou shalt not misrepresent your opponent’s position in order to make it easier for you to defeat it (straw man fallacy).
- Thou shalt not argue that, because others do wrong, you are permitted to do the same (tu quoque fallacy).
- Thou shalt not assume that your argument is correct because some authority agrees with you (appeal to authority).
- Thou shalt not attack your opponents instead of their arguments (ad hominem).
Yes, I know, one could add a lot more. But these 10 ‘commandments’ relate to the errors in rational thought that I feel would, if taken on board, be most useful in our discussions about SCAM.
In Germany, homeopathy had a free ride for a very long time. In recent years, however, several doctors, pharmacists, scientists, etc. have started opposing the fact that the public has to pay for ineffective treatments such as homeopathics. As a consequence, homeopaths have begun to fight back. The weapons they chose are often not the most subtle. Now they seem to have reached a new low; the Board of the German Central Association of Homeopathic Physicians (DZVhÄ) has sent an open letter to the Board of the German Society of Internal Medicine (DGIM) and to the participating colleagues of the 127th Congress of the DGIM from April 17 – 20, 2021 in an attempt to stop an invited lecture of a critic of homeopathy.
Here is my translation of the letter:
Dear colleagues on the board of the DGIM,
We were very surprised to read that an ENT colleague will speak on homeopathy at the 127th Congress of Internal Medicine. Dr. Lübbers is known up and down the country as a media-active campaigner against homeopathy. His “awakening experience” he had, according to his own account, when he had to fish homeopathic pills out of the ear of a child with otitis, since then he is engaged – no: not for better education, in the mentioned case of the parents or other users – against the method homeopathy (which was certainly not “guilty” of the improper application!).
It has surely not escaped you that in all media again and again only a small handful of self-proclaimed “experts” – all from the clique of the skeptic movement! – are heard on the subject of homeopathy. A single (!) fighter against homeopathy is a physician who completed her training in homeopathy and practices for a time as a homeopath. All the others come from non-medical and other occupational groups. In contrast, there are several thousand medical colleagues throughout Germany who stand on the ground of evidence-based medicine, have learned conventional medicine, implement it in their practices, and have completed a recognized continuing education program in homeopathy.
In the German Central Association of Homeopathic Physicians – the oldest medical professional association in Germany – 146 qualified internists are currently registered as members, in addition to numerous other medical specialists, all of whom are actively practicing medicine.
Question: Why does the German Society for Internal Medicine invite an ENT specialist, of all people, who lectures on homeopathy without any expertise of his own? Why not at least a specialist colleague in internal medicine? Or even a colleague who could report on the subject from her own scientific or practical experience? For example, on the topic of “hyperaldosteronism,” would you also invite a urologist or orthodontist? And if so, why?
Dear Board of Directors of the DGIM: As an honorary board member of the German Central Association of Homeopathic Physicians e.V.. (DZVhÄ) – and a specialist in internal medicine – I am quite sure that we could immediately name several colleagues with sufficient expertise as homeopathically trained and experienced internists, if you are really interested in a solid and correct discourse on the subject of homeopathy. Under the above-mentioned circumstances, there is, of course, rather the suspicion that it should not be about, but rather exclusively against homeopathy.
If it is planned for a later congress, e.g. in 2022, to deal again with the topic of homeopathy in a truly professionally well-founded and possibly even more balanced form: please contact us at any time! As medical colleagues, we are very interested in a fair and unprejudiced professional discourse.
Yours sincerely
Dr. med. Ulf Riker, Internist – Homeopathy – Naturopathy
2nd chairman DZVhÄ / 1st chairman LV Bayern
________________
What are Riker and the DZVhÄ trying to say with this ill-advised, convoluted, and poorly written letter?
Let me try to put his points a little clearer:
- They are upset that the congress of internists invited a non-homeopath to give a lecture about homeopathy.
- The person in question, Dr. Lübbers, is an ENT specialist and, like all other German critics of homeopathy (apart from one, Dr. Grams), does not understand homeopathy.
- There are thousands of physicians who do understand it and are fully trained in homeopathy.
- They would therefore do a much better job in providing a lecture.
- So, would the German internists please invite homeopaths for their future meetings?
And what is Riker trying to achieve?
- It seems quite clear that he aims to prevent criticism of homeopathy.
- He wishes to replace it with pro-homeopathy propaganda.
- Essentially he wants to stifle free speech, it seems to me.
To reach these aims, he does not hesitate to embarrass himself by sending and making publicly available a very stupid letter. He also behaves in a most unprofessional fashion and does not mind putting a few untruths on paper.
Having said that, I will admit that they are in good company. Hahnemann was by all accounts a most intolerant and cantankerous chap himself. And during the last 200 years, his followers have given ample evidence that critical thinking has remained an alien concept for them. Consequently, such behavior seems not that unusual for German defenders of homeopathy. In recent times they have:
- Made the results of the largest investigation into homeopathy disappear because its results were devastatingly negative.
- Went to Liberia to cure Ebola with homeopathy.
- Published lots of untruths and exaggerations.
- Hired a journalist to systematically defame me and other critics.
- Likened critics to Roland Freisler, the infamous judge of the Nazi era.
- Threatened critics with legal action.
- Started a media campaign to promote homeopathy.
- Published libelous statements about me.
Quite a track record, wouldn’t you agree?
But, I think, attempting to suppress free speech beats it all and must be a new low in the history of homeopathy.
Energy healing is an umbrella term for a range of paranormal healing practices. Their common denominator is the belief in a mystical ‘energy’ that can be used for therapeutic purposes. Forms of energy healing have existed in many ancient cultures. The ‘New Age’ movement has brought about a revival of these ideas, and today energy healing systems are amongst the most popular alternative therapies in the US as well as in many other countries.
Energy healing relies on the esoteric belief in some form of ‘energy’ which is distinct from the concept of energy understood in physics and refers to some life force such as chi in Traditional Chinese Medicine, or prana in Ayurvedic medicine. Some proponents employ terminology from quantum physics and other ‘cutting-edge’ science to give their treatments a scientific flair which, upon closer scrutiny, turns out to be but a veneer of pseudo-science. The ‘energy’ that energy healers refer to is not measurable and lacks biological plausibility.
The purpose of this study was to evaluate the effects of energy healing (EH) therapy prior to and following posterior surgical correction for adolescent idiopathic scoliosis (AIS) compared to controls.
Patients were prospectively randomized to one of two groups: standard operative care for surgery (controls) vs. standard care with the addition of three EH sessions. The outcomes included visual analog scales (VAS) for pain and anxiety (0-10), days until conversion to oral pain medication, and length of hospital stay. For the experimental group, VAS was assessed pre- and post-EH session.
Fifty patients were enrolled-28 controls and 22 EH patients. The controls had a median of 12 levels fused vs. 11 in the EH group (p = 0.04). Pre-operative thoracic and lumbar curve magnitudes were similar (p > 0.05). Overall VAS pain scores increased from pre- to post-operative (p < 0.001), whereas the VAS anxiety scores decreased immediately post-operative (p < 0.001). The control and pre-EH assessments were statistically similar. Significant decreases in VAS pain and anxiety scores from pre to post-EH assessments were noted for the EH group. Both groups transitioned to oral pain medication a median of 2 days post-operative (p = 0.11). The median days to discharge were four in the controls and three in the EH group (p = 0.07).
The authors concluded that EH therapy resulted in a decrease in patient’s pre-operative anxiety. Offering this CAM modality may enhance the wellbeing of the patient and their overall recovery when undergoing posterior surgical correction for AIS.
I am getting tired of explaining that this trial design tells us as good as nothing about the effects of the tested therapy per se. As we have discussed ad nauseam on this blog, A+B is always more than B alone. Such trials appear to be rigorous and fool many people, but they are unable to control for context effects, like placebo or attention. Therefore, I need to re-write the conclusions:
The placebo effect and the extra attention associated with EH therapy resulted in a decrease in patients’ pre-operative anxiety. EH itself is most likely bar any effect. Further studies in this area are not required.
Battlefield Acupuncture (BFA) – I presume the name comes from the fact that it is so simple, it could even be used under combat situations – is a form of ear acupuncture developed 20 years ago by Dr Richard Niemtzow. BFA employs gold semipermanent needles that are placed at up to 5 specific sites in one or both ears. The BFA needles are small conical darts that pierce the outer ear in designated locations and remain in place until they fall out typically within 3–4 days.
The US Defense and Veterans Center for Integrative Pain Management and the Veterans Health Administration National Pain Management Program Office recently completed a 3-year acupuncture education and training program, which deployed certified BFA trainers for the Department of Defense and Veterans Administration medical centers. Over 2800 practitioners were thus trained to provide BFA. The total costs amounted to $ 5.4 million.
This clearly begs the question:
DOES IT WORK?
This review aims to investigate the effects and safety of BFA in adults with pain. Electronic databases were searched for randomized controlled trials (RCTs) published in English evaluating efficacy and safety of BFA in adults with pain, from database inception to September 6, 2019. The primary outcome was pain intensity change, and the secondary outcome was safety. Nine RCTs were included in this review, and five trials involving 344 participants were analyzed quantitatively. Compared with no intervention, usual care, sham BFA, and delayed BFA interventions, BFA had no significant improvement in the pain intensity felt by adults suffering from pain. Few adverse effects (AEs) were reported with BFA therapy, but they were mild and transitory.
The authors of this review concluded that BFA is a safe, rapid, and easily learned acupuncture technique, mainly used in acute pain management, but no significant efficacy was found in adult individuals with pain, compared with the control groups. Given the poor methodological quality of the included studies, high-quality RCTs with rigorous evaluation methods are needed in the future.
And here are my comments:
- SAFE? Impossible to tell on the basis of 344 patients.
- RAPID? True, but meaningless, as it does not work.
- EASILY LEARNT? True, it’s simple and seems ever so stupid.
- NO SIGNIFICANT EFFICACY? That I can easily believe.
I am amazed that anyone would fall for an idea as naive as BFA. That it should be the US military is simply hilarious, in my view. I am furthermore baffled that anyone recommends more study of such monumental nonsense.
Why, oh why?
Acupuncture is far-fetched (to put it mildly). Ear acupuncture is positively ridiculous. BFA seems beyond ridiculous and must be the biggest military hoax since general Grigory Aleksandrovich Potemkin painted façades to fool Catherine the Great into thinking that an area was far richer than it truly was.
Low back pain must be one of the most frequent reasons for patients to seek out some so-called alternative medicine (SCAM). It would therefore be important that the information they get is sound. But is it?
The present study sought to assess the quality of web-based consumer health information available at the intersection of LBP and CAM. The investigators searched Google using six unique search terms across four English-speaking countries. Eligible websites contained consumer health information in the context of CAM for LBP. They used the DISCERN instrument, which consists of a standardized scoring system with a Likert scale from one to five across 16 questions, to conduct a quality assessment of websites.
Across 480 websites identified, 32 were deemed eligible and assessed using the DISCERN instrument. The mean overall rating across all websites 3.47 (SD = 0.70); Summed DISCERN scores across all websites ranged from 25.5-68.0, with a mean of 53.25 (SD = 10.41); the mean overall rating across all websites 3.47 (SD = 0.70). Most websites reported the benefits of numerous CAM treatment options and provided relevant information for the target audience clearly, but did not adequately report the risks or adverse side-effects adequately.
The authors concluded that despite some high-quality resources identified, our findings highlight the varying quality of consumer health information available online at the intersection of LBP and CAM. Healthcare providers should be involved in the guidance of patients’ online information-seeking.
In the past, I have conducted several similar surveys, for instance, this one:
Background: Low back pain (LBP) is expected to globally affect up to 80% of individuals at some point during their lifetime. While conventional LBP therapies are effective, they may result in adverse side-effects. It is thus common for patients to seek information about complementary and alternative medicine (CAM) online to either supplement or even replace their conventional LBP care. The present study sought to assess the quality of web-based consumer health information available at the intersection of LBP and CAM.
Methods: We searched Google using six unique search terms across four English-speaking countries. Eligible websites contained consumer health information in the context of CAM for LBP. We used the DISCERN instrument, which consists of a standardized scoring system with a Likert scale from one to five across 16 questions, to conduct a quality assessment of websites.
Results: Across 480 websites identified, 32 were deemed eligible and assessed using the DISCERN instrument. The mean overall rating across all websites 3.47 (SD = 0.70); Summed DISCERN scores across all websites ranged from 25.5-68.0, with a mean of 53.25 (SD = 10.41); the mean overall rating across all websites 3.47 (SD = 0.70). Most websites reported the benefits of numerous CAM treatment options and provided relevant information for the target audience clearly, but did not adequately report the risks or adverse side-effects adequately.
Conclusion: Despite some high-quality resources identified, our findings highlight the varying quality of consumer health information available online at the intersection of LBP and CAM. Healthcare providers should be involved in the guidance of patients’ online information-seeking.
Or this one:
Background: Some chiropractors and their associations claim that chiropractic is effective for conditions that lack sound supporting evidence or scientific rationale. This study therefore sought to determine the frequency of World Wide Web claims of chiropractors and their associations to treat, asthma, headache/migraine, infant colic, colic, ear infection/earache/otitis media, neck pain, whiplash (not supported by sound evidence), and lower back pain (supported by some evidence).
Methods: A review of 200 chiropractor websites and 9 chiropractic associations’ World Wide Web claims in Australia, Canada, New Zealand, the United Kingdom, and the United States was conducted between 1 October 2008 and 26 November 2008. The outcome measure was claims (either direct or indirect) regarding the eight reviewed conditions, made in the context of chiropractic treatment.
Results: We found evidence that 190 (95%) chiropractor websites made unsubstantiated claims regarding at least one of the conditions. When colic and infant colic data were collapsed into one heading, there was evidence that 76 (38%) chiropractor websites made unsubstantiated claims about all the conditions not supported by sound evidence. Fifty-six (28%) websites and 4 of the 9 (44%) associations made claims about lower back pain, whereas 179 (90%) websites and all 9 associations made unsubstantiated claims about headache/migraine. Unsubstantiated claims were made about asthma, ear infection/earache/otitis media, neck pain,
Conclusions: The majority of chiropractors and their associations in the English-speaking world seem to make therapeutic claims that are not supported by sound evidence, whilst only 28% of chiropractor websites promote lower back pain, which is supported by some evidence. We suggest the ubiquity of the unsubstantiated claims constitutes an ethical and public health issue.
The findings were invariably disappointing and confirmed those of the above paper. As it is nearly impossible to do much about this lamentable situation, I can only think of two strategies for creating progress:
- Advise patients not to rely on Internet information about SCAM.
- Provide reliable information for the public.
Both describe the raison d’etre of my blog pretty well.
