bogus claims
I have reported about the risks of chiropractic manipulation many times before. This is not because, as some seem to believe, I have an axe to grind but because the subject is important. This week, another case of stroke after chiropractic manipulation was in the news. Some will surely say that it is alarmist to mention such reports which lack lots of crucial details. Yet, as long as chiropractors do not establish a proper monitoring system where serious adverse effects of spinal manipulation are noted, I think it is important to record even incomplete cases in this fashion.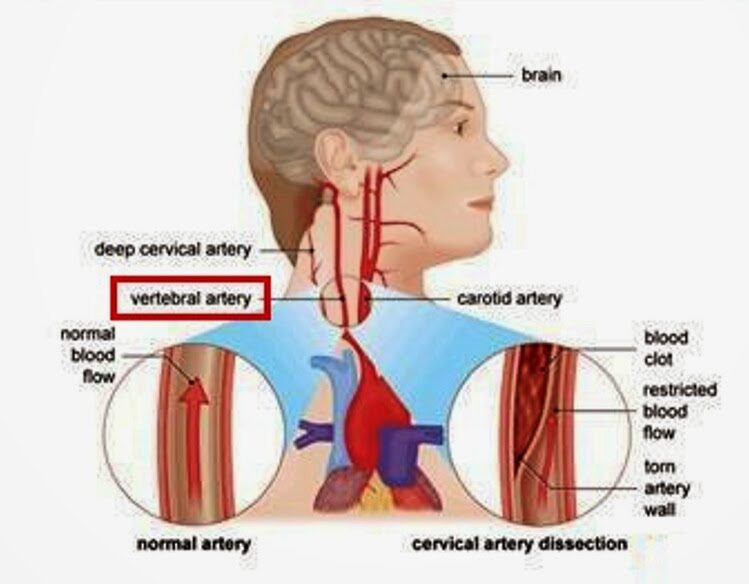
Barbara Shand is a working mom who lives in Alberta, Canada. She went to see a chiropractor because she had neck pain. “Near the very end of the appointment, the chiropractor asked: ‘Do you want your neck adjusted?’ I said: ‘Sure.’” “As soon as she did it, everything went black,” Shand recalls.
The patient was then rushed to a hospital by ambulance. “When I did open my eyes, I couldn’t focus. It was all blurry, I had massive vertigo, I didn’t know what was up or down,” Shand told the journalist. The diagnosis, Shand explains, was a right vertebral artery dissection, followed by a stroke. Mrs. Sands continues to struggle with coordination and balance.
The Alberta College and Association of Chiropractors acknowledges “there have been reported cases of stroke associated with visits to various healthcare practitioners, including those that provide cervical spine manipulation.” But they claim it is rare. They did not comment on the informed consent which, according to Shand’s description, was more than incomplete.
The fact that the ACAC admits that such events have happened before is laudable and a step in the right direction (some chiropractic organizations don’t even go that far). Yet, their caveat that such cases are rare is problematic. Without a monitoring system, nobody can tell how frequent they are! What we do see is merely the tip of a much bigger iceberg. There have been hundreds of cases like Mrs. Shand. The truth of the matter is this: Chiropractic neck manipulations are not supported by sound evidence of effectiveness for any condition. This means that even rare risks (if they are truly rare) would tilt the risk/benefit balance into the negative.
The conclusion is, I think, to avoid neck manipulations at all costs. Or, as one neurologist once put it:
don’t let the buggars touch your neck!
‘CLAMP DOWN ON THE BOGUS SCIENCE OF HOMEOPATHY’ is the title of a comment by Oliver Klamm in The Times today. Here is the background to his article.
In September 2020, the website of Homeopathy UK, www.homeopathy-uk.org, featured a page titled “Conditions Directory” with text that stated “Please find below a list of conditions where homeopathy can help …” followed by a list of medical conditions that included depression, diabetes, infertility, psoriasis and asthma. When consumers clicked-through the links to the conditions listed on that page, they were taken to separate pages for each that contained anecdotal descriptions from doctors detailing how they had applied homeopathic methods to the relevant conditions.
The UK Advertising Standards Authority received a complainant that challenged whether the ad discouraged essential treatment for conditions for which medical supervision should be sought, namely depression, diabetes, infertility, psoriasis and asthma.
The response of ‘Homeopathy UK’ said that, as a registered charity, they sought to share information about homeopathy for the benefit of others, rather than for commercial gain, and that they would always recommend that patients seeking homeopathic care did so under the supervision of a qualified medical practitioner…
The ASA upheld the complaint and argued as follows:
The CAP Code required that marketers must not discourage essential treatment for conditions for which medical supervision should be sought. For example, they must not offer specific advice on, diagnosis or treatment for such conditions unless that advice, diagnosis or treatment was conducted under the supervision of a suitably qualified medical professional. The ad referred to “depression”, “diabetes”, “infertility”, “psoriasis” and “asthma”, which we considered were conditions for which medical supervision should be sought. Any advice, diagnosis or treatment, therefore, must be conducted under the supervision of a suitably qualified medical professional. We acknowledged that the articles had been written by GMC-registered doctors, who we considered would be suitably qualified to offer advice, diagnosis or treatment. However, we noted that the ad and the articles to which it linked referred to homeopathy in general, rather than treatment by a specific individual. We understood that there were no minimum professional qualifications required to practice homeopathy, which could result in consumers being advised, diagnosed, or treated for the conditions listed in the ad by a practitioner with no medical qualification. We therefore considered Homeopathy UK would not be able to demonstrate that all such treatment would be conducted under the supervision of a suitably qualified health professional.
Furthermore, we understood that, although elsewhere on the website there were links to specific clinics, not all treatment would be conducted under the supervision of a suitably qualified health professional across those clinics. Because Homeopathy UK had not supplied evidence that treatment would always be carried out by a suitably qualified health professional. Also, because reference to the conditions listed in the ad, and discussed in the related articles, could discourage consumers from seeking essential treatment under the supervision of a suitably qualified health professional, we concluded that the ad had breached the Code.
On that point the ad breached CAP Code (Edition 12) rule 12.2 (Medicines, medical devices, health-related products and beauty products).
The ad must not appear again in the form complained about. We told Homeopathy UK to ensure their future marketing communications did not to refer to conditions for which advice should be sought from suitably qualified health professionals.
___________________________
Depression, diabetes, and asthma have few things in common. Just two characteristics stand out, in my view:
- they are potentially fatal;
- homeopathy is ineffective in changing their natural history.
- It was therefore high time that the ASA stopped this criminally dangerous nonsense of deluded homeopaths.
The article by Oliver Klamm concludes with the following wise words about homeopathy:
“For public officials and opinion formers, the time for appeasing this dangerous quackery should be long past.”
I have not often seen a paper reporting a small case series with such an impressively long list of authors from so many different institutions:
- Hospital of Lienz, Lienz, Austria.
- WissHom: Scientific Society for Homeopathy, Koethen, Germany; Umbrella Organization for Medical Holistic Medicine, Vienna, Austria; Vienna International Academy for Holistic Medicine (GAMED), Otto Wagner Hospital Vienna, Austria; Professor Emeritus, Medical University of Vienna, Department of Medicine I, Vienna, Austria. Electronic address: [email protected].
- Resident Specialist in Hygiene, Medical Microbiology and Infectious Diseases, Außervillgraten, Austria.
- St Mary’s University, London, UK.
- Umbrella Organization for Medical Holistic Medicine, Vienna, Austria.
- Shaare Zedek Medical Center, The Center for Integrative Complementary Medicine, Jerusalem, Israel.
- Apotheke Zum Weißen Engel – Homeocur, Retz, Austria.
- Reeshabh Homeo Consultancy, Nagpur, India.
- Umbrella Organization for Medical Holistic Medicine, Vienna, Austria; Vienna International Academy for Holistic Medicine (GAMED), Otto Wagner Hospital Vienna, Austria; Chair of Complementary Medicine, Medical Faculty, Sigmund Freud University Vienna, Austria; KLITM: Karl Landsteiner Institute for Traditional Medicine and Medical Anthropology, Vienna, Austria.
- WissHom: Scientific Society for Homeopathy, Koethen, Germany.
In fact, there are 12 authors reporting about 13 patients! But that might be trivial – so, let’s look at the paper itself. The aim of this study was to describe the effect of adjunctive individualized homeopathic treatment delivered to hospitalized patients with confirmed symptomatic SARS-CoV-2 infection.
Thirteen patients with COVID-19 were admitted. The mean age was 73.4 ± 15.0 (SD) years. The treating homeopathic doctor was instructed by the hospital on March 27, 2020, to adjunctively treat all inpatient COVID-19 patients homeopathically. The high potency homeopathic medicinal products were administered orally. Five globules were administered sublingually where they dissolved, three times a day. In ventilated patients in the ICU, medication was administered as a sip from a water beaker or 1 ml three times a day using a syringe. All ventilated patients exhibited dry cough resulting in respiratory failure. They were given Influenzinum, as were the patients at the general inpatient ward.
Twelve patients (92.3%) were speedily discharged without relevant sequelae after 14.4 ± 8.9 days. A single patient admitted in an advanced stage of septic disease died in the hospital. A time-dependent improvement of relevant clinical symptoms was observed in the 12 surviving patients. Six (46.2%) were critically ill and treated in the intensive care unit (ICU). The mean stay at the ICU of the 5 surviving patients was 18.8 ± 6.8 days. In six patients (46.2%) gastrointestinal disorders accompanied COVID-19.
The authors conclude that adjunctive homeopathic treatment may be helpful to treat patients with confirmed COVID-19 even in high-risk patients especially since there is no conventional treatment of COVID-19 available at present.
In the discussion section of the paper, the authors state this: “Given the extreme variability of pathology and clinical manifestations, a single universal preventive homeopathic medicinal product does not seem feasible. Yet homeopathy may have a relevant role to play precisely because of the number and diversity of its homeopathic medicinal products which can be matched with the diversity of the presentations. Patients with mild forms of disease can use homeopathic medicinal products at home using our simple algorithm. As this Case series suggests, adjunctive homeopathic treatment can play a valuable role in more serious presentations. For future pandemics, homeopathy agencies should be prepared by establishing rapid-response teams and efficacious lines of communication.”
There is nothing in this paper that would lead me to conclude that the homeopathic remedies had a positive effect on the natural history of the disease. All this article actually does do is this: it provides a near-perfect insight into the delusional megalomania of some homeopaths. These people are even more dangerous than I had feared.
The aim of this “multicenter cross-sectional study” was to analyze a cohort of breast (BC) and gynecological cancers (GC) patients regarding their interest in, perception of, and demand for integrative therapeutic health approaches.
The BC and GC patients were surveyed at their first integrative clinic visit using validated standardized questionnaires. Treatment goals and potential differences between the two groups were evaluated.
A total of 340 patients (272 BC, 68 GC) participated in the study. The overall interest in IM was 95.3% and correlated with older age, recent chemotherapy, and higher education. A total of 89.4% were using integrative methods at the time of enrolment, primarily exercise therapy (57.5%), and vitamin supplementation (51.4%). The major short-term goal of the BC patients was a side-effects reduction of conventional therapy (70.4%); the major long-term goal was the delay of a potential tumor progression (69.3%). In the GC group, major short-term and long-term goals were slowing tumor progression (73.1% and 79.1%) and prolonging survival (70.1% and 80.6%). GC patients were significantly more impaired by the side-effects of conventional treatment than BC patients [pain (p = 0.006), obstipation (< 0.005)].
The authors concluded that these data demonstrate a high overall interest in and use of IM in BC and GC patients. This supports the need for specialized IM counseling and the implementation of integrative treatments into conventional oncological treatment regimes in both patient groups. Primary tumor site, cancer diagnosis, treatment phase, and side effects had a relevant impact on the demand for IM in our study population.
This paper is, in my mind, an excellent example of pseudo-research:
- The ‘study’ turns out to be little more than a survey.
- The sample is small and not representative; therefore the findings cannot be generalized and are meaningless.
- The patients surveyed are those who decided to attend clinics of integrative medicine.
- These patients had used alternative therapies before and are evidently in favor of alternative medicine.
- The most frequently used alternative therapies (exercise, vitamins, trace elements, massage, lymph drainage) are arguably conventional treatments in Germany where the survey was conducted.
I have repeatedly commented on the plethora of useless surveys in so-called alternative medicine (SCAM). But this one might beat them all in its uselessness. The fact that close to 100% of patients attending clinics of integrative medicine are interested in SCAM and use some form of SCAM says it all, I think.
Why do people waste their time on such pseudo-research?
The best answer to this question is that it can be used for promotion. I found the paper by reading what seems to be a press release entitled: “Eine Studie bestätigt Patientenwunsch nach naturheilkundlicher Unterstützung”. This translates into “a study confirms the wish of patients for naturopathic support”. Needless to explain that the survey did not even remotely show this to be true.
What will they think of next?
I suggest a survey run in a BC clinic which amazingly discovers that nearly 100% of all patients are female.
Neuropathic pain is difficult to treat. Luckily, we have acupuncture! Acupuncturists leave us in no doubt that their needles are the solution. But are they correct or perhaps victims of wishful thinking?
This review was aimed at determining the proportion of patients with neuropathic pain who achieve a clinically meaningful improvement in their pain with the use of different pharmacologic and nonpharmacologic treatments.
Randomized controlled trials were included that reported a responder analysis of adults with neuropathic pain-specifically diabetic neuropathy, postherpetic neuralgia, or trigeminal neuralgia-treated with any of the following 8 treatments: exercise, acupuncture, serotonin-norepinephrine reuptake inhibitors (SNRIs), tricyclic antidepressants (TCAs), topical rubefacients, opioids, anticonvulsant medications, and topical lidocaine.
A total of 67 randomized controlled trials were included. There was moderate certainty of evidence that anticonvulsant medications (risk ratio of 1.54; 95% CI 1.45 to 1.63; number needed to treat [NNT] of 7) and SNRIs (risk ratio of 1.45; 95% CI 1.33 to 1.59; NNT = 7) might provide a clinically meaningful benefit to patients with neuropathic pain. There was low certainty of evidence for a clinically meaningful benefit for rubefacients (ie, capsaicin; NNT = 7) and opioids (NNT = 8), and very low certainty of evidence for TCAs. Very low-quality evidence demonstrated that acupuncture was ineffective. All drug classes, except TCAs, had a greater likelihood of deriving a clinically meaningful benefit than having withdrawals due to adverse events (number needed to harm between 12 and 15). No trials met the inclusion criteria for exercise or lidocaine, nor were any trials identified for trigeminal neuralgia.
The authors concluded that there is moderate certainty of evidence that anticonvulsant medications and SNRIs provide a clinically meaningful reduction in pain in those with neuropathic pain, with lower certainty of evidence for rubefacients and opioids, and very low certainty of evidence for TCAs. Owing to low-quality evidence for many interventions, future high-quality trials that report responder analyses will be important to strengthen understanding of the relative benefits and harms of treatments in patients with neuropathic pain.
This review was published in a respected mainstream journal and conducted by a multidisciplinary team with the following titles and affiliations:
- Associate Professor in the College of Pharmacy at the University of Manitoba in Winnipeg.
- Pharmacist in Edmonton, Alta, and Clinical Evidence Expert for the College of Family Physicians of Canada.
- Family physician and Assistant Professor at the University of Alberta.
- Family physician and Associate Professor in the Department of Family Medicine at the University of Alberta.
- Pharmacist, Clinical Evidence Expert Lead for the College of Family Physicians of Canada, and Associate Clinical Professor in the Department of Family Medicine at the University of Alberta.
- Pharmacist in Edmonton and Clinical Evidence Expert for the College of Family Physicians of Canada.
- Pharmacist and Clinical Evidence Expert at the College of Family Physicians of Canada.
- Family physician, Director of Programs and Practice Support at the College of Family Physicians of Canada, and Adjunct Professor in the Department of Family Medicine at the University of Alberta.
- Professor in the Faculty of Pharmaceutical Sciences at the University of British Columbia in Vancouver.
- Pharmacist at the CIUSSS du Nord-de-l’lle-de-Montréal and Clinical Associate Professor in the Faculty of Pharmacy at the University of Montreal in Quebec.
- Care of the elderly physician and Assistant Professor in the Department of Family Medicine at the University of Alberta.
- Family physician and Professor in the Department of Family Medicine at the University of Alberta.
- Assistant Professor in the Department of Family Medicine at Queen’s University in Kingston, Ont.
- Research assistant at the University of Alberta.
- Medical student at the University of Alberta.
- Nurse in Edmonton and Clinical Evidence Expert for the College of Family Physicians of Canada.
As far as I can see, the review is of sound methodology, it minimizes bias, and its conclusions are therefore trustworthy. They suggest that acupuncture is not effective for neuropathic pain.
But how can this be? Do the authors not know about all the positive evidence on acupuncture? A quick search found positive recent reviews of acupuncture for all of the three indications in question:
- Diabetic neuropathy: Acupuncture alone and vitamin B combined with acupuncture are more effective in treating DPN compared to vitamin B.
- Herpes zoster: Acupuncture may be effective for patients with HZ.
- Trigeminal neuralgia: Acupuncture appears more effective than pharmacotherapy or surgery.
How can we explain this obvious contradiction?
Which result should we trust?
Do we believe pro-acupuncture researchers who published their papers in pro-acupuncture journals, or do we believe the findings of researchers who could not care less whether their work proves or disproves the effectiveness of acupuncture?
I think that these papers offer an exemplary opportunity for us to study how powerful the biases of researchers can be. They also remind us that, in the realm of so-called alternative medicine (SCAM), we should always be very cautious and not accept every conclusion that has been published in supposedly peer-reviewed medical journals.
The UK ‘Advertising Standards Authority‘ (ASA) received a complaint about an advertisement that stated:
“Homeopathy is used throughout the world to keep healthy … People in the UK have been using it to successfully help with migraine, anxiety, chronic pain, woman’s [sic] health issues, depression, eczema, chronic fatigue, asthma, IBS, rheumatoid arthritis, and many other conditions”.
The ‘Good Thinking Society‘ had challenged whether:
- the ad discouraged essential treatment for conditions for which medical supervision should be sought, namely migraines, chronic pain, women’s health issues, depression, asthma, rheumatoid arthritis; and
- the claim “People in the UK have been using [homeopathy] to successfully help with anxiety, chronic pain … eczema, chronic fatigue syndrome … IBS” was misleading and could be substantiated.
The response of the ASA has just been published. Here are the key excerpts from the ASA’s assessment:
1. Upheld
The CAP Code required that marketers must not discourage essential treatment for conditions for which medical supervision should be sought. For example, they must not offer specific advice on, diagnosis or treatment for such conditions unless that advice, diagnosis or treatment was conducted under the supervision of a suitably qualified medical professional. Among other conditions, the ad referred to “migraines”, “chronic pain”, “woman’s [sic] health issues”, “depression”, “asthma”, and “rheumatoid arthritis”, which we considered were conditions for which medical supervision should be sought, and therefore advice, diagnosis or treatment must be conducted under the supervision of a suitably qualified medical professional. We noted that the practice was run by a GMC-registered GP, who we considered was a suitably qualified health professional. However, the individual homeopaths were not registered and did not hold the same qualifications. Therefore, Homeopathy UK had not shown that all treatment and diagnoses conducted at the practice would be conducted under the supervision of a suitably qualified medical professional. Because Homeopathy UK had not supplied evidence that treatment would always be carried out by a suitably qualified health professional, and because reference to the conditions listed in the ad could discourage consumers from seeking essential treatment under the supervision of a suitably qualified health professional, we concluded that the ad had breached the Code.
On that point the ad breached CAP Code (Edition 12) rule 12.2 (Medicines, medical devices, health-related products and beauty products).
2. Upheld
We considered that consumers would understand the claim “People in the UK have been using [homeopathy] to successfully help with anxiety, chronic pain … eczema, chronic fatigue syndrome … IBS” to mean that homeopathy could be used to successfully treat those conditions … when we reviewed the evidence provided by Homeopathy UK, we considered that the studies provided did not meet the standard of evidence we required for the types of claims being made, both in terms of adequacy and relevance…
On that point the ad breached CAP Code (Edition) rules 3.1 (Misleading advertising), 3.7 (Substantiation) and 12.1 (Medicines, medical devices, health-related products and beauty products).
Action
The ad must not appear again in the form complained about. We told Homeopathy UK to ensure their future marketing communications did not to refer to conditions for which advice should be sought from suitably qualified health professionals. We also told them to ensure they did not make claims for homeopathy unless they were supported with robust evidence.
_____________________________
Am I reading this correctly?
The ASA seems to be saying that homeopaths are not suitably qualified health professionals and, as no therapeutic claims are supported by robust evidence, that claims for homeopathy are improper.
You may not like it, but we do seem to live in the age of the ‘alternative truth’. It might necessitate reconsidering some of our definitions. A lie, for instance, was formerly defined as making an untrue statement with intent to deceive. Does that definition need to be revised in the age of the ‘alternative truth’?
Laura Kuenssberg, the political editor of the BBC, seems to think so. She recently published an interesting new definition of a lie: “… outright lying … is relatively rare. It is too easily found out. Only one senior politician still in the game has ever privately told me something that was utterly, entirely, and completely untrue.” She wrote this in an article about our PM, Boris Johnson who, by old standards, would probably qualify as a habitual liar. And as the BBC political editor cannot easily call him that, she conveniently moved the goal post and defined a lie to be something “utterly, entirely, and completely untrue”.
So, here we have it, the age of alternative truths has redefined the lie!
But I am not starting to write political rants – tempting though it often is – there is enough to rant about in so-called alternative medicine (SCAM). The questions I asked myself are these: how does SCAM measure up to the new Kuenssberg definition, and how gullible have we become?
Let’s play a little game to find out, shall we?
I provide 10 statements commonly used by the SCAM fraternity, and I ask you to consider which of them is “utterly, entirely, and completely untrue”.
- Chiropractic manipulations have been proven to do more good than harm.
- Acupuncture is effective for chronic pain.
- Homeopathy is supported by sound evidence.
- Homeopathic remedies act as nano-particles.
- Natural means safe.
- Integrative medicine is in the best interest of patients.
- Chiropractic subluxations do exist.
- Detox is a concept that makes sense.
- SCAM practitioners treat the root causes of disease.
- SCAM is cost-effective.
Next, please count the number of statements that are “utterly, entirely, and completely untrue”. This will give you a figure between 0 and 10. I propose that it can be used as a measure of gullibility.
I suggest the following grading:
- 10 – 8 = not gullible
- 7 – 5 = gullible
- 4 – 2 = very gullible
- 1 – 0 = dangerously gullible.
And here you have the ‘Edzard Ernst measure of gullibility’!
Many people believe that homeopathy is essentially plant-based – but they are mistaken! Homeopathic remedies can be made from anything: Berlin wall, X-ray, pus, excrement, dental plaque, mobile phone rays, poisons … anything you can possibly think of. So, why not from vaccines?
This is exactly what a pharmacist specialized in homeopathy thought.
It has been reported that the ‘Schloss-Apotheke’ in Koblenz, Germany offered for sale a homeopathic remedy made from the Pfizer vaccine. This has since prompted not only the Chamber of Pharmacists but also the Paul Ehrlich Institute and Pfizer to issue statements. On Friday (30/4/2021) morning, the pharmacy had advertised homeopathic remedies based on the Pfizer/Biontech vaccine. The Westphalia-Lippe Chamber of Pharmacists then issued an explicit warning against it. “We are stunned by this,” said a spokesman. The offer has since disappeared from the pharmacy’s website.
Pfizer vaccine. This has since prompted not only the Chamber of Pharmacists but also the Paul Ehrlich Institute and Pfizer to issue statements. On Friday (30/4/2021) morning, the pharmacy had advertised homeopathic remedies based on the Pfizer/Biontech vaccine. The Westphalia-Lippe Chamber of Pharmacists then issued an explicit warning against it. “We are stunned by this,” said a spokesman. The offer has since disappeared from the pharmacy’s website.
On Friday afternoon, the manufacturer of the original vaccine also intervened. The Paul Ehrlich Institute released a statement making it clear that a vaccine is only safe “if it is administered in accordance with the marketing authorization.”
The Schloss-Apotheke had advertised the product in question with the following words:
“We have Pfizer/BioNTech Covid-19-Vaccine in potentized form up to D30 as globules or dilution (for discharge) in stock.”
The chamber of pharmacists countered with a warming under the heading “Facts instead of Fake News” on Facebook and Instagram:
“Whatever they might contain: These remedies are no effective protection against Covid-19.”
Pharmacy manager, Annette Eichele, of the Schloss-Apotheke claimed she had not sold homeopathic Corona vaccines and stressed that effective vaccines of this kind do not exist. According to Eichele, only an additional “mini drop” of the original Biontech vaccine had been used and “highly potentized” and prepared homeopathically. According to Eichele, Corona vaccinations that had already been administered were thus to have a “better and more correct effect with this supplementary product, possibly without causing side effects … but this is not scientifically proven”. The homeopathic product had been produced only on customer request and had been sold less than a dozen times in the past weeks. Ten grams of the remedy were sold for about 15 Euros. On Twitter, Eichele stated: „Wir haben nichts Böses getan, wir wollten nur Menschen helfen!“ (We have done nothing evil, we only wanted to help people). I am reminded yet again of Bert Brecht who observed:
“The opposite of good is not evil but good intentions”.
Many chiropractors seem to view the present pandemic as a business opportunity and make no end of false claims to attract customers. This has now been outlawed in the US. Medscape reported that a US district court will decide whether a chiropractor who is charged with 10 counts of making false marketing claims related to COVID-19 will be the first person convicted under a new federal law.
On his website, chiropractor ‘Dr.’ Eric Neptune advertises his services as follows:
Have you ever been told by your medical doctor that you or a member of your family had a specific disease, syndrome, or sickness? Did your doctor then recommend a drug or surgery to fix the issue, or tell you that you would have to live with it for the rest of your life? If so, you are not alone!
Nepute Wellness Center is unlike any medical clinic you may have been to. The clinic team is focused on finding and fixing the CAUSE of your problem vs. seeking out and treating only the SYMPTOMS. Nepute Wellness Center is equipped with state-of-the-art diagnostic equipment and testing, as well as medical doctors, nurses, and chiropractors who have been uniquely trained to treat your whole body, regardless of age, and return your body to a healthy balance so that it can heal itself the way God intended.
If you are tired of trying to treat your symptoms using prescription and over-the-counter pills, or even considering surgery, then Nepute Wellness Center may be right for you! Or like many, you want to be proactive with your health and prevent sickness and disease before you begin to suffer any symptoms, allowing you to live the full life you deserve, then make Nepute Wellness Center your partner in health!
Already over a year ago, Eric Nepute, the owner of Quickwork, based in St. Louis, Missouri, managed to make headlines. He had recorded a video that racked up more than 21 million views and suggested that drinking tonic water would prevent COVID-19 infections. Now, Mr. Neptune is the first person charged by the Federal Trade Commission (FTC) under the new COVID- 19 Consumer Protection Act. His company which has several locations in St. Louis County advertised its vitamin D and zinc products on social media and the internet as drugs that could treat or prevent COVID-19 claiming that their products are “more effective than the available COVID-19 vaccines”.
The FTC warned Nepute’s company in May 2020 about making unsubstantiated claims for other products regarding efficacy against COVID-19 and advised him to immediately stop making claims that were not supported by scientific evidence. However, Nepute seemed undeterred.
The FTC is seeking to fine Nepute and Quickwork up to US$43,792 for each violation of the COVID-19 Consumer Protection Act. In addition, the FTC seeks to bar the company from making health claims unless they are true and can be substantiated by scientific evidence.
Through his attorney, Neptune told the local NBC TV news affiliate, “I feel that I have not done anything wrong. I encourage everyone to live a healthy lifestyle during this unprecedented time. My attorneys are reviewing the complaint and I have no further comments at this time.”
In 2008, the British Chiropractic Association sued Simon Singh because he disclosed that they were promoting chiropractic for infant colic. The BCA lost the case, plenty of money, and all its reputation. Ever since the issue is a very sore point for chiropractic pride. The data show that Simon was quite correct in stating that they are happily promoting bogus treatments without a jot of evidence. Here for instance is my systematic review:
Some chiropractors claim that spinal manipulation is an effective treatment for infant colic. This systematic review was aimed at evaluating the evidence for this claim. Four databases were searched and three randomised clinical trials met all the inclusion criteria. The totality of this evidence fails to demonstrate the effectiveness of this treatment. It is concluded that the above claim is not based on convincing data from rigorous clinical trials.
But chiropractors steadfastly refuse to accept defeat and keep on trying to find positive results. Now Danish chiropractors have made another attempt.
The purpose of this study is to evaluate the effect of chiropractic care on infantile colic. This multicenter, single-blind randomized controlled trial was conducted in four Danish chiropractic clinics, 2015–2019. Information was distributed in the maternity wards and by maternal and child health nurses. Children aged 2–14 weeks with unexplained excessive crying were recruited through home visits and randomized (1:1) to either chiropractic care or control group. Both groups attended the chiropractic clinic twice a week for 2 weeks. The intervention group received chiropractic care, while the control group was not treated. The parents were not present in the treatment room and unaware of their child’s allocation.
The primary outcome was change in daily hours of crying before and after treatment. Secondary outcomes were changes in hours of sleep, hours being awake and content, gastrointestinal symptoms, colic status and satisfaction. All outcomes were based on parental diaries and a final questionnaire.
Of 200 recruited children, 185 completed the trial (treatment group n = 96; control group n = 89). Duration of crying in the treatment group was reduced by 1.5 h compared with 1 h in the control group (mean difference − 0.6, 95% CI − 1.1 to − 0.1; P = 0.026), but when adjusted for baseline hours of crying, age, and chiropractic clinic, the difference was not significant (P = 0.066). The proportion obtaining a clinically important reduction of 1 h of crying was 63% in the treatment group and 47% in the control group (p = 0.037), and NNT was 6.5. We found no effect on any of the secondary outcomes.

The authors concluded that excessive crying was reduced by half an hour in favor of the group receiving chiropractic care compared with the control group, but not at a statistically significant level after adjustments. From a clinical perspective, the mean difference between the groups was small, but there were large individual differences, which emphasizes the need to investigate if subgroups of children, e.g. those with musculoskeletal problems, benefit more than others from chiropractic care.
This seems to be a rigorous trial. However, I don’t quite understand why the authors even mention that, before adjusting, the results seemed to favor chiropractic. This only makes a squarely negative study look positive! Why would anyone want to do that? Could this perhaps hint at a reason for this odd behavior? “The study was primarily funded by the Foundation for Chiropractic Research and Postgraduate Education.”
