bias
The state of acupuncture research has long puzzled me. The first thing that would strike who looks at it is its phenomenal increase:
- Until around the year 2000, Medline listed about 200 papers per year on the subject.
- From 2005, there was a steep, near-linear increase.
- It peaked in 2020 when we had a record-breaking 20515 acupuncture papers currently listed in Medline.
Which this amount of research, one would expect to get somewhere. In particular, one would hope to slowly know whether acupuncture works and, if so, for which conditions. But this is not the case.
On the contrary, the acupuncture literature is a complete mess in which it gets more and more difficult to differentiate the reliable from the unreliable, the useful from the redundant, and the truth from the lies. Because of this profound confusion, acupuncture fans are able to claim that their pet-therapy is demonstrably effective for a wide range of conditions, while skeptics insist it is a theatrical placebo. The consumer might listen in bewilderment.
Yesterday (18/1/2021), I had a quick (actually, it was not that quick after all) look into what Medline currently lists in terms of new acupuncture research published in 2021 and found a few other things that are remarkable:
- There were already 100 papers dated 2021 (today, there were even 118); that corresponds to about 5 new articles per day and makes acupuncture one of the most research-active areas of so-called alternative medicine (SCAM).
- Of these 100 papers, only 7 were clinical trials (CTs). In my view, clinical trials would be more important than any other type of research on acupuncture. To see that they amount to just 7% of the total is therefore disappointing.
- Twelve papers were systematic reviews (SRs). It is odd, I find, to see almost twice the amount of SRs than CTs.
- Eighteen papers referred to protocols of studies of SRs. In particular protocols of SRs are useless in my view. It seems to me that the explanation for this plethora of published protocols might be the fact that Chinese researchers are extremely keen to get papers into Western journals; it is an essential boost to their careers.
- Seven papers were surveys. This multitude of survey research is typical for all types of SCAM.
- Twenty-four articles were on basic research. I find basic research into an ancient therapy of questionable clinical use more than a bit strange.
- The rest of the articles were other types of publications and a few were misclassified.
- The vast majority (n = 81) of the 100 papers were authored exclusively by Chinese researchers (and a few Korean). In view of the fact that it has been shown repeatedly that practically all acupuncture studies from China report positive results and that data fabrication seems rife in China, this dominance of China could be concerning indeed.
Yes, I find all this quite concerning. I feel that we are swamped with plenty of pseudo-research on acupuncture that is of doubtful (in many cases very doubtful) reliability. Eventually, this will create an overall picture for the public that is misleading to the extreme (to check the validity of the original research is a monster task and way beyond what even an interested layperson can do).
And what might be the solution? I am not sure I have one. But for starters, I think, that journal editors should get a lot more discerning when it comes to article submissions from (Chinese) acupuncture researchers. My advice to them and everyone else:
if it sounds too good to be true, it probably is!
Professor Andreas Michalsen is the clinical director of the department of naturopathy in a Berlin hospital. He seems most keen to represent the scientific side of so-called alternative medicine in Germany. He has published several (fairly uncritical) books on SCAM and numerous papers in the medical literature. I had a look at those papers and hope you agree that Michalsen should join the other extraordinary experts in THE ALTERNATIVE MEDICINE HALL OF FAME:
- Jennifer Jacobs (homeopath, US)
- Jenise Pellow (homeopath, South Africa)
- Adrian White (acupuncturist, UK)
- Michael Frass (homeopath, Austria)
- Jens Behnke (research officer, Germany)
- John Weeks (editor of JCAM, US)
- Deepak Chopra (entrepreneur, Us)
- Cheryl Hawk (US chiropractor)
- David Peters (osteopathy, homeopathy, UK)
- Nicola Robinson (TCM, UK)
- Peter Fisher (homeopathy, UK)
- Simon Mills (herbal medicine, UK)
- Gustav Dobos (various, Germany)
- Claudia Witt (homeopathy, Germany and Switzerland)
- George Lewith (acupuncture, UK)
- John Licciardone (osteopathy, US)
My Medline search on 10/1/2021 for ‘Michalsen A, clinical trial’, generated 69 hits. Below I list the key conclusions of the 47 SCAM studies that were published in English by Andreas Michalsen et al:
- In this explorative pilot trial, an increase of HRV (more parasympathetic dominance and overall higher HRV) after ten weeks of yoga in school in comparison to regular school sports was demonstrated, showing an improved self-regulation of the autonomic nervous system. (pilot)
- Results showed a contrast between the high agreement of the consented final diagnosis and disagreement on certain diagnostic details.
- A single session of leech therapy is more effective over the short term in lowering the intensity of pain over the short term and in improving physical function and quality of life over the intermediate term.
- Short term fasting during chemotherapy is well tolerated and appears to improve QOL and fatigue during chemotherapy. Larger studies should prove the effect of STF as an adjunct to chemotherapy. (pilot)
- Administering verum (a complex homeopathic drug) resulted in a statistically significantly greater improvement of the Cough Assessment Score than the placebo. The tolerability was good and not inferior to that of the placebo.
- Ayurvedic treatment is beneficial in reducing knee OA symptoms.
- We did not find any clinically relevant differences between groups in this controlled clinical pilot trial of 8 wk of intermittent fasting in healthy volunteers.
- We found positive effects for both groups, which however were more pronounced in the Ayurvedic group. The conversational and counseling techniques in the Ayurvedic group offered more opportunities for problem description by patients as well as patient-centered practice and resource-oriented recommendations by the physician.
- Results of this study suggest that prolonged fasting is feasible and might have beneficial clinical effects. (pilot)
- This clinical trial indicates comparable efficacy of the herbal combination and antibiotic, although non-inferiority was not proved. However, the results and lessons learned are important for the planning of future trials.
- Thus, cycles of a 5-day fasting-mimiking diet are safe, feasible, and effective in reducing markers/risk factors for aging and age-related diseases.
- Ayurvedic external treatment is effective for pain-relief in chronic low back pain in the short term.
- Focused meditation and self-care exercise lead to comparable, symptomatic improvements in patients with chronic low back pain.
- This randomized trial found no effects of yoga on health-related quality of life in patients with colorectal cancer. Given the high attrition rate and low intervention adherence, no definite conclusions can be drawn from this trial.
- The Alexander Technique was not superior to local heat application in treating chronic non-specific neck pain.
- In conclusion, meditation may support chronic pain patients in pain reduction and pain coping.
- The herbal preparation of myrrh, chamomile extract and coffee charcoal is well tolerated and shows a good safety profile. We found first evidence for a potential efficacy non-inferior to the gold standard therapy mesalazine, which merits further study of its clinical usefulness in maintenance therapy of patients with ulcerative colitis.
- Yoga was more effective in relieving chronic nonspecific neck pain than a home-based exercise program. Yoga reduced neck pain intensity and disability and improved health-related quality of life. Moreover, yoga seems to influence the functional status of neck muscles, as indicated by improvement of physiological measures of neck pain.
- In this preliminary trial, yoga appears to be an effective treatment in chronic neck pain with possible additional effects on psychological well-being and QOL. (pilot)
- These results suggest that Gua Sha may be an effective treatment for patients with chronic neck and low back pain.
- The data indicate that during needle insertion high dose acupuncture stimulation leads to a higher increase of sympathetic nerve activity than low dose stimulation independent of personality. After needle insertion subjects who tend to augment incoming stimuli might show a lack of psychological relaxation when receiving high dose stimulation.
- In patients with METS, phlebotomy, with consecutive reduction of body iron stores, lowered BP and resulted in improvements in markers of cardiovascular risk and glycemic control.
- The present study gives preliminary evidence that healing clay jojoba oil facial masks can be effective treatment for lesioned skin and mild acne vulgaris.
- In a laboratory setting, an electroacupuncture procedure was as effective as a single dose of an orally administered opiate in reducing experimentally induced ischaemic pain.
- In the presence of modern treatments, complementary prescription of comprehensive lifestyle modification has no impact on coronary artery calcium progression but sustainable benefit for blood pressure, heart rate and the need of anti-ischemic medication is demonstrated.
- A single course of leech therapy was effective in relieving pain in the short-term and improved disability in intermediate-term. Leeches might be considered as an additional option in the therapeutic approach to lateral epicondylitis.
- Gua sha has beneficial short-term effects on pain and functional status in patients with chronic neck pain.
- Alterations in short-chain fatty acids were found in terms of significant changes to increased acetate levels in the fasting group.
- In this first study on the efficacy of cantharidin blisters, a clinically relevant pain-relieving short-term effect on lumbar spinal stenosis was observed.
- We conclude that cupping therapy may be effective in relieving the pain and other symptoms related to CTS.
- A single course of leech therapy is effective in relieving pain, improving disability and QoL for at least 2 months.
- The high effect sizes indicate that repeated rhythmic embrocation with Solum Oil may improve mood, pain perception (sensory PPS), and the ability to cope with pain (affective PPS) in patients with chronic low back pain.
- The data indicate, that verum acupuncture and sham acupuncture might have a beneficial influence on the autonomic nervous system in migraineurs with a reduction of the LF power of HRV related to the clinical effect. This might be due to a reduction of sympathetic nerve activity. VA and SA induce different effects on the high-frequency component of HRV, which seem, however, not to be relevant for the clinical outcome in migraine.
- Gua Sha increases microcirculation local to a treated area, and that increase in circulation may play a role in local and distal decrease in myalgia. Decrease in myalgia at sites distal to a treated area is not due to distal increase in microcirculation. There is an unidentified pain-relieving biomechanism associated with Gua Sha.
- These results are consistent with possible short-term benefits of a comprehensive lifestyle modification program on some aspects of quality-of-life and emotional well-being, but no effects were discernable 12 months after completion of therapy.
- In the presence of modern treatments, comprehensive lifestyle modification provides no additional benefits on progression of atherosclerosis but improves autonomic function, angina, and QOL with concomitant reduced need of medication. These responses are more pronounced in GNB3*825T allele carriers.
- Neither Mediterranean diet nor fasting treatments affect the microbiologically assessed intestinal flora and sIgA levels in patients with RA and FM.
- Women suffering from mental distress participating in a 3-month Iyengar yoga class show significant improvements on measures of stress and psychological outcomes.
- Adoption of a Mediterranean diet by patients with medically treated CAD has no effect on markers of inflammation and metabolic risk factors.
- A comprehensive lifestyle modification and stress management program did not improve psychological outcomes in medically stable CAD patients. The program did appear to confer psychological benefits for women but not men. Further trials should investigate gender-related differences in coronary patient responses to behavioral interventions.
- Mind-body therapy may improve quality of life in patients with UC in remission, while no effects of therapy on clinical or physiological parameters were found, which may at least in part be related to selective patient recruitment.
- Leech therapy helps relieve symptoms in patients with osteoarthritis of the knee.
- A home-based hydrotherapeutic thermal treatment program improves quality of life, heart-failure-related symptoms and heart rate response to exercise in patients with mild chronic heart failure. The results of this investigation suggest a beneficial adaptive response to repeated brief cold stimuli in addition to enhanced peripheral perfusion due to thermal hydrotherapy in patients with chronic heart failure.
- This open pilot study demonstrates that along with a decrease in sleep arousals a 1-week fasting period promotes the quality of sleep and daytime performance in non-obese subjects.
- Periarticular application of 4 leeches led to rapid relief of pain with sustained improvement after 4 weeks in the absence of major complications.
- Short-term fasting in inpatients with pain and stress syndromes is safe and well tolerated, concomitant mineral supplements have no additive benefit.
- The results suggest that the cardiovascular response during whole-body infrared-A irradiation is accompanied by significant changes in autonomic cardiac regulation: A significant decrease of low-frequency power corresponding to depressed vagal activity results in an increase of Iow/high-frequency ratio. During serial hyperthermias the acute response is diminished suggesting an adaption of the autonomic response to hyperthermia.
This list is impressive in several ways: very few SCAM researchers managed to publish 47 Medline-listed clinical studies, and nobody I know has ever conducted clinical trials of so many different SCAMs in so many different medical conditions. They include:
- Acupuncture
- Alexander technique
- Ayrurvedic medicine
- Blood letting
- Cupping
- Diet
- Embrocation
- Fasting
- Gua cha
- Herbal medicine
- Homeopathy
- Hydrotherapy
- Hyperthermia
- Meditation
- Mind/body therapies
- Leeching
- Life style modification
- Yoga
While this is astounding, another fact is even more baffling: with just 2 or 3 exceptions, all these studies yield postive results. Whatever Michalsen touches turns to gold! And if it doesn’t, he spins the findings such that the conclusions are at least partly positive; see for instance No 14, 33, 36, 40 or 41 in the above list.
WELCOME TO THE ALTERNATIVE MEDICINE HALL OF FAME PROFESSOR MICHALSEN!
So-called alternative medicine (SCAM) is, as we all know, an umbrella term. Under this umbrella, we find hundreds of different modalities that have little in common with each other. Here I often focus on:
- homeopathy,
- chiropractic,
- acupuncture,
- herbal medicine.
There are uncounted others, and in my recent book, I published critical evaluations 150 of them. But for the moment, let’s keep to the 4 SCAMs listed above.
What strikes me regularly is that many SCAM enthusiasts do seem to appreciate my critical assessments of SCAM; for instance:
- When I point out that the assumptions of homeopathy fly in the face of science, most SCAM enthusiasts agree.
- When I point out that chiropractic spinal manipulations might not be safe, most SCAM enthusiasts agree.
- When I point out that acupuncture is not a panacea, most SCAM enthusiasts agree.
- When I point out that herbal remedies can interact with prescribed drugs, most SCAM enthusiasts agree.
Most but not all!
- Those who find my criticism of homeopathy unfair are the homeopaths and their proponents.
- Those who find my criticism of chiropractic unfair are the chiropractors and their proponents.
- Those who find my criticism of acupuncture unfair are the acupuncturists and their proponents.
- Those who find my criticism of herbal medicine unfair are the herbalists and their proponents.
Hardly ever does a herbalist defend homeopathy’s weird assumptions; rarely does an acupuncturist tell me that I am too harsh with the chiropractors; never have I heard a chiropractor complain that my criticism of acupuncture is unjustified.
Entirely obvious?
Perhaps!
But I find it nevertheless curious, because my critical stance is always the same. I do not change it for this or that form of SCAM (I would also not change it for conventional medicine, but I leave it to those who have more specific expertise to do the criticising). I have no axe to grind against any particular SCAM. All I do is point out flaws in their logic, limitations in their studies, gaps in the evidence. All I do is provide my honest interpretation of the evidence.
It really seems to me that everyone appreciates my honesty, until I start being honest with them.
And this is why I find it curious. Homeopaths, chiropractors, acupuncturists, herbalists and all the other types of SCAM practitioners like to be seen on the side of science, evidence, critical thinking and progress. This, I suppose, is good for the (self) image; it might even help the delusion that they are all evidence-based. But as soon as someone applies science, evidence, critical thinking and progress to their very own little niche within SCAM, they stop liking it and start aggressing the critic.
I suppose this is entirely obvious as well?
Perhaps!
But it also exposes the double standard that is so deeply ingrained in SCAM.
Dr Jennifer Jacobs is a homeopaths from the US. She is a family physician and a clinical assistant professor in epidemiology at the University of Washington School of Public Health and Community Medicine. She received her MD degree from Wayne State University and a Masters in Public Health from the University of Washington.
Jennifer is foremost famous for the homeopathic childhood diarhoea studies, but does that justify her joining THE ALTERNATIVE MEDICINE HALL OF FAME with its 15 current members who managed the impossible feast of never publishing a negative conclusion about their pet SCAM:
- Jenise Pellow (homeopath, South Africa)
- Adrian White (acupuncturist, UK)
- Michael Frass (homeopath, Austria)
- Jens Behnke (research officer, Germany)
- John Weeks (editor of JCAM, US)
- Deepak Chopra (entrepreneur, Us)
- Cheryl Hawk (US chiropractor)
- David Peters (osteopathy, homeopathy, UK)
- Nicola Robinson (TCM, UK)
- Peter Fisher (homeopathy, UK)
- Simon Mills (herbal medicine, UK)
- Gustav Dobos (various, Germany)
- Claudia Witt (homeopathy, Germany and Switzerland)
- George Lewith (acupuncture, UK)
- John Licciardone (osteopathy, US)
A Medline search generated 25 papers of hers on homeopathy. Here are the key findings of the … that report original data on the effectiveness of homeopathy (clinical trials or reviews):
- If and when conventional medicine runs out of options for treating epidemic diseases, homeopathy could be seen as an attractive alternative, but only if there is viable experimental evidence of its success.
- The homeopathic syrup appeared to be effective in reducing the severity of cold symptoms in the first day after beginning treatment.
- …the medicines prescribed in individualised homeopathy may have small, specific, treatment effects.
- Homeopathic ear drops may be effective in reducing the use of antibiotics in children with AOM managed with a delayed antibiotic approach.
- This study suggests that homeopathic ear drops were moderately effective in treating otalgia in children with AOM and may be most effective in the early period after a diagnosis of AOM. Pediatricians and other primary health care providers should consider homeopathic ear drops a useful adjunct to standard therapy.
- The homeopathic combination therapy tested in this study did not significantly reduce the duration or severity of acute diarrhea in Honduran children. Further study is needed to develop affordable and effective methods of using homeopathy to reduce the global burden of childhood diarrhea.
- This pilot study provides no evidence to support a therapeutic effect of individually selected homeopathic remedies in children with ADHD. A therapeutic effect of the homeopathic encounter is suggested and warrants further evaluation.
- Small sample size precludes definitive answers, but results from this preliminary trial suggest that homeopathy may be of value in the treatment of menopausal symptoms and improving quality of life, especially in those women not on tamoxifen.
- The results from these studies confirm that individualized homeopathic treatment decreases the duration of acute childhood diarrhea and suggest that larger sample sizes be used in future homeopathic research to ensure adequate statistical power. Homeopathy should be considered for use as an adjunct to oral rehydration for this illness.
- These results suggest that a positive treatment effect of homeopathy when compared with placebo in acute otitis media cannot be excluded and that a larger study is justified.
- These results are consistent with the finding from the previous study that individualized homeopathic treatment decreases the duration of diarrhea and number of stools in children with acute childhood diarrhea.
- The statistically significant decrease in the duration of diarrhea in the treatment group suggests that homeopathic treatment might be useful in acute childhood diarrhea. Further study of this treatment deserves consideration.
Next to Claudia Witt, Jennifer might be the researcher who has published the most clinical trials of homeopathy with positive conclusions (don’t be jealous Michael Frass, you might be in third place!). Attentive readers have probably noticed, she also published a negative trial with a negative conclusion (No 6) and a negative trial with a not so negative conclusion (No 7). The negative study almost cost her the place in the HALL OF FAME. But let’s be generous, and let’s consider the TRUSTWORTHINESS INDEX which, in her case, is still well and safely in the untrustworthy region. Therefore, I hope we all agree: Jenifer does deserve a place in THE ALTERNATIVE MEDICINE HALL OF FAME.
WELCOME JENNIFER!
I was alerted to an article in which some US doctors, including the famous Andrew Weil, promote the idea that so-called alternative medicine (SCAM) has a lot to offer for people recovering from Covid-19 infections. There would be a lot to argue about their recommendations, but today I will not go into this (I find it just too predictable how SCAM proponents try to promote SCAM on the basis of flimsy evidence; perhaps I am suffering from ‘BS for Covid fatigue’?). What did, however, strike me in their paper was a definition of INTEGRATIVE MEDICINE (IM) that I had not yet come across:
Integrative medicine is defined as healing-oriented medicine that takes account of the whole person, including all aspects of lifestyle. It emphasizes the therapeutic relationship between practitioner and patient, is informed by evidence, and makes use of all appropriate therapies.
Ever since the term IM became fashionable, there have been dozens of definitions of the term (almost as though IM proponents were not quite sure themselves what they were promoting). And ever since I first heard about IM, I felt it was a thinly disguised attempt to smuggle unproven treatments into the routine of evidence-based medicine (EBM). In 2002, I published my 1st comment on the subject. In it, I warned that IM must not become an excuse for using every conceivable untested treatment under the banner of holism. Nineteen years on, this is exactly what has happened, and one definition of IM after the next is soaked in platitudes, falsehoods and misunderstandings.
So, let’s see how reasonable this new definition is. I will try to do this by briefly discussing each element of the two sentences.
- IM is healing-oriented medicine: this is a transparently daft platitude. Does anyone know a medicine that is not oriented towards healing? Healing is the process of becoming well again, especially after a cut or other injury, or of making someone well again. Healing is what medicine has always been and always be aimed at. In other words, it is not something that differentiates IM from other forms of healthcare.
- IM takes account of the whole person: This is the little holistic trick that IM proponents like to adopt. It implies that normal medicine or EBM is not holistic. This implication is wrong. Any good medicine is holistic, and if a sector of healthcare fails to account for the whole person, we need to reform it. (Here are the conclusions of an editorial I published in 2007 entitled ‘Holistic heath care?‘: good health care is likely to be holistic but holistic health care, as it is marketed at present, is not necessarily good. The term ‘holistic’ may even be a ‘red herring’ which misleads patients. What matters most is whether or not any given approach optimally benefits the patient. This goal is best achieved with effective and safe interventions administered humanely — regardless of what label we put on them.) Creating a branch of medicine that, like IM, pretends to have a monopoly on holism can only hinder this process.
- IM includes all aspects of lifestyle: really, all of them? This is nonsense! Good physicians take into account the RELEVANT lifestyles of their patients. If, for instance, my patient with intermittent claudication is a postman, his condition would affect him differently from a patient who is a secretary. But all lifestyles? No! I fear this ‘over the top’ statement merely indicates that those who have conceived it have difficulties differentiating the important from the trivial.
- IM emphasizes the therapeutic relationship: that’s nice! But so do all other physicians (except perhaps pathologists). As medical students, we were taught how to do it, some physicians wrote books about it (remember Balint?), and many of us ran courses on the subject. Some conventional clinicians might even feel insulted by the implication that they do not emphasize the therapeutic relationship. Again, the IM brigade take an essential element of good healthcare as their monopoly. It almost seems to be a nasty habit of theirs to highjack a core element of healthcare and declare it as their invention.
- IM is informed by evidence: that is brilliant, finally there emerges a real difference between IM and EBM! While proper medicine is BASED on evidence, IM is merely INFORMED by it. The difference is fundamental, because it allows IM clinicians to use any un- or disproven SCAM. The evidence for homeopathy fails to show that it is effective? Never mind, IM is not evidence-based, it is evidence-informed. IM physiciance know homeopathy is a placebo therapy (if not they would be ill-informed which would make them unethical), but they nevertheless use homeopathy (try to find an IM clinic that does not offer homeopathy!), because IM is not EBM. IM is evidence-informed!
- IM makes use of all appropriate therapies: and the last point takes the biscuit. Are the IM fanatics honestly suggesting that conventional doctors use inappropriate therapies? Does anyone know a branch of health care where clinicians systematically employ therapies that are not appropriate? Appropriate means suitable or right for a particular situation or occasion. Are IM practitioners the only ones who use therapies that are suitable for a particular situation? This last point really does count on anyone falling for IM not to have the slightest ability to think analytically.
This short analysis confirms yet again that IM is little more than a smokescreen behind which IM advocates try to smuggle nonsense into routine healthcare. The fact that, during the last two decades, the definition constantly changed, while no half decent definition emerged suggests that they themselves don’t quite know what it is. They like moving the goal post but seem unsure in which direction. And their latest attempt to define IM indicates to me that IM advocates might not be the brightest buttons in the drawer.
So sorry, I have been neglecting THE ALTERNATIVE MEDICINE HALL OF FAME of late. I was reminded of its existence when writing my post about Adrian White the other day. Reading the kind comments I received on it, I not only decided to make Adrian an honorary member (for his latter part of his career as an acupuncture researcher, but also to reactivate the idea of the HALL OF FAME in more general terms. And in the course of doing just this, I noticed that I somehow forgot to admit Prof Michael Frass, an omission which I regret and herewith rectify. A warm welcome to both!
In case you are unaware what THE ALTERNATIVE MEDICINE HALL OF FAME is, let me explain: it is a group of researchers who manage to go through (part of) their professional life researching their particular SCAM without ever publishing a negative conclusion about it, or who have other outstanding merits in misleading the public about so-called alternative medicine (SCAM). As of today, we thus have the following experts in the HALL:
Adrian White (acupuncturist, UK)
Michael Frass (homeopath, Austria)
Jens Behnke (research officer, Germany)
John Weeks (editor of JCAM, US)
Deepak Chopra (entrepreneur, Us)
Cheryl Hawk (US chiropractor)
David Peters (osteopathy, homeopathy, UK)
Nicola Robinson (TCM, UK)
Peter Fisher (homeopathy, UK)
Simon Mills (herbal medicine, UK)
Gustav Dobos (various, Germany)
Claudia Witt (homeopathy, Germany and Switzerland)
George Lewith (acupuncture, UK)
John Licciardone (osteopathy, US)
I must say, this is an assembly of international SCAM experts to be proud of – even if I say so myself!
The new member I am proposing to admit today is Dr Jenice Pellow. She is a lecturer in the Department of Complementary Medicine at the University of Johannisburg and already once featured on this blog. But now it seems time to admit this relatively little-known researcher into my HALL OF FAME. Dr Pellow has 11 Medline-listed papers on so-called alternative medicine (SCAM). Allow me to show you some key findings from their abstracts:
- Complementary and alternative medicine (CAM) offers parents various treatment options for this condition [ADHD], including dietary modifications, nutritional supplementation, herbal medicine, and homeopathy. CAM appears to be most effective when prescribed holistically and according to each individual’s characteristic symptoms.
- The homeopathic medicine reduced the sensitivity reaction of cat allergic adults to cat allergen, according to the SPT. Future studies are warranted to further investigate the effect of Cat saliva and Histaminum and their role as a potential therapeutic option for this condition.
- Findings suggest that daily use of the homeopathic complex does have an effect over a 4-wk period on physiological and cognitive arousal at bedtime as well as on sleep onset latency in PI sufferers. Further research on the use of this complex for PI is warranted before any definitive conclusions can be drawn.
- The homeopathic complex used in this study exhibited significant anti-inflammatory and pain-relieving qualities in children with acute viral tonsillitis. No patients reported any adverse effects. These preliminary findings are promising; however, the sample size was small and therefore a definitive conclusion cannot be reached. A larger, more inclusive research study should be undertaken to verify the findings of this study.
- …results suggest the homeopathic complex, together with physiotherapy, can significantly improve symptoms associated with CLBP due to OA.
- This small study showed the potential benefits of individualized homeopathic treatment of binge eating in males, decreasing both the frequency and severity of binging episodes.
- There have been numerous trials and pharmacological studies of specific herbal preparations related to the treatment of low sexual desire.
- Most of the evaluated medicinal plants showed evidence of efficacy in relieving menstrual pain in at least one RCT.
- Results indicated that most participants made use of both complementary and conventional medicines for their infant’s colic; the most commonly used complementary medicine products were homeopathic remedies, probiotics and herbal medicines.
- Promising evidence for the following single supplements were found [for allergic rhinitis]: apple polyphenols, tomato extract, spirulina, chlorophyll c2, honey, conjugated linoleic acid, MSM, isoquercitrin, vitamins C, D and E, as well as probiotics. Combination formulas may also be beneficial, particularly specific probiotic complexes, a mixture of vitamin D3, quercetin and Perilla frutescens, as well as the combination of vitamin D3 and L. reuteri.
- Despite a reported lack of knowledge regarding complementary medicine and limited personal use, participants had an overall positive attitude towards complementary medicine.
I admit that 11 papers in 7 years is not an overwhelming output for a University lecturer. However, please do consider the fact that all of them – particularly the ones on homeopathy which is be the particular focus of Jenice (after all, she is a homeopath) – chime a happy tune for SCAM. I therefore think that Jenice should be admitted to THE ALTERNATIVE MEDICINE HALL OF FAME and hope you agree.
Welcome to ALTERNATIVE MEDICINE HALL OF FAME, Jenice!
As though the UK does not have plenty of organisations promoting so-called alternative medicine (SCAM)! Obviously not – because a new one is about to emerge.
In mid-January, THE COLLEGE OF MEDICINE AND INTEGRATED HEALTH (COMIH) will launch the Integrated Medicine Alliance bringing together the leaders of many complementary health organisations to provide patients, clinicians and policy makers with information on the various complementary modalities, which will be needed in a post COVID-19 world, where:
- patient choice is better respected,
- requirements for evidence of efficacy are more proportionate to the seriousness of the disease and the safety of the intervention,
- and where benefit versus risk are better balanced.
We already saw this in 2020 with the College advocating from the very beginning of the year that people should think about taking Vitamin D, while the National Institute for Clinical Excellence continued to say the evidence was insufficient, but the Secretary of State has now supported it being given to the vulnerable on the basis of the balance between cost, benefit and safety.
Elsewhere we learn more about the Integrated Medicine Alliance (IMA):
The IMA is a group of organisations and individuals that have been brought together for the purpose of encouraging and optimising the best use of complementary therapies alongside conventional healthcare for the benefit of all.
The idea for this group was conceived by Dr Michael Dixon in discussion with colleagues associated with the College of Medicine, and the initial meeting to convene the group was held in February 2019.
The group transitioned through a number of titles before settling on the ‘Integrated Medicine Alliance’ and began work on developing a patient leaflet and a series of information sheets on the key complementary therapies.
It was agreed that in the first instance the IMA should exist under the wing of the College of Medicine, but that in the future it may develop into a formal organisation in its own right, but inevitably maintaining a close relationship with the College of Medicine.
The IMA also offers ‘INFORMATION SHEETS’ on the following modalities:
- Acupuncture
- Alexander Technique
- Aromatherapy
- Herbal Medicine
- Homeopathy
- Hypnotherapy
- Massage
- Naturopathy
- Reflexology
- Reiki
- Tai Chi
- Yoga Therapy
I find those leaflets revealing. They tell us, for example that the Reiki practitioner channels universal energy through their hands to help rebalance each of the body’s energy centres, known as chakras. About homeopathy, we learn that a large corpus of evidence has accumulated which stands the most robust tests of modern science. And about naturopathy, we learn that it includes ozone therapy but is perfectly safe.
Just for the fun of it – and free of charge – let me try to place a few corrections here:
- Reiki healers use their hands to perform what is little more than a party trick.
- The universal energy they claim to direct does not exist.
- The body does not have energy centres.
- Chakras are a figment of imagination.
- The corpus of evidence on homeopathy is by no means large.
- The evidence is flimsy.
- The most robust tests of modern science fail to show that homeopathy is effective beyond placebo.
- Naturopathy is a hotchpotch of treatments most of which are neither natural nor perfectly safe.
One does wonder who writes such drivel for the COMIH, and one shudders to think what else the IMA might be up to.
I was criticised for not referencing this article in a recent post on adverse effects of spinal manipulation. In fact the commentator wrote: Shame on you Prof. Ernst. You get an “E” for effort and I hope you can do better next time. The paper was published in a third-class journal, but I will nevertheless quote the ‘key messages’ from this paper, because they are in many ways remarkable.
- Adverse events from manual therapy are few, mild, and transient. Common AEs include local tenderness, tiredness, and headache. Other moderate and severe adverse events (AEs) are rare, while serious AEs are very rare.
- Serious AEs can include spinal cord injuries with severe neurological consequences and cervical artery dissection (CAD), but the rarity of such events makes the provision of epidemiological evidence challenging.
- Sports-related practice is often time sensitive; thus, the manual therapist needs to be aware of common and rare AEs specifically associated with spinal manipulative therapy (SMT) to fully evaluate the risk-benefit ratio.
The author of this paper is Aleksander Chaibi, PT, DC, PhD who holds several positions in the Norwegian Chiropractors’ Association, and currently holds a position as an expert advisor in the field of biomedical brain research for the Brain Foundation of the Netherlands. I feel that he might benefit from reading some more critical texts on the subject. In fact, I recommend my own 2020 book. Here are a few passages dealing with the safety of SMT:
Relatively minor AEs after SMT are extremely common. Our own systematic review of 2002 found that they occur in approximately half of all patients receiving SMT. A more recent study of 771 Finish patients having chiropractic SMT showed an even higher rate; AEs were reported in 81% of women and 66% of men, and a total of 178 AEs were rated as moderate to severe. Two further studies reported that such AEs occur in 61% and 30% of patients. Local or radiating pain, headache, and tiredness are the most frequent adverse effects…
A 2017 systematic review identified the characteristics of AEs occurring after cervical spinal manipulation or cervical mobilization. A total of 227 cases were found; 66% of them had been treated by chiropractors. Manipulation was reported in 95% of the cases, and neck pain was the most frequent indication for the treatment. Cervical arterial dissection (CAD) was reported in 57%, and 46% had immediate onset symptoms. The authors of this review concluded that there seems to be under-reporting of cases. Further research should focus on a more uniform and complete registration of AEs using standardized terminology…
In 2005, I published a systematic review of ophthalmic AEs after SMT. At the time, there were 14 published case reports. Clinical symptoms and signs included:
- central retinal artery occlusion,
- nystagmus,
- Wallenberg syndrome,
- ptosis,
- loss of vision,
- ophthalmoplegia,
- diplopia,
- Horner’s syndrome…
Vascular accidents are the most frequent serious AEs after chiropractic SMT, but they are certainly not the only complications that have been reported. Other AEs include:
- atlantoaxial dislocation,
- cauda equina syndrome,
- cervical radiculopathy,
- diaphragmatic paralysis,
- disrupted fracture healing,
- dural sleeve injury,
- haematoma,
- haematothorax,
- haemorrhagic cysts,
- muscle abscess,
- muscle abscess,
- myelopathy,
- neurologic compromise,
- oesophageal rupture
- pneumothorax,
- pseudoaneurysm,
- soft tissue trauma,
- spinal cord injury,
- vertebral disc herniation,
- vertebral fracture…
In 2010, I reviewed all the reports of deaths after chiropractic treatments published in the medical literature. My article covered 26 fatalities but it is important to stress that many more might have remained unpublished. The cause usually was a vascular accident involving the dissection of a vertebral artery (see above). The review also makes the following important points:
- … numerous deaths have been associated with chiropractic. Usually high-velocity, short-lever thrusts of the upper spine with rotation are implicated. They are believed to cause vertebral arterial dissection in predisposed individuals which, in turn, can lead to a chain of events including stroke and death. Many chiropractors claim that, because arterial dissection can also occur spontaneously, causality between the chiropractic intervention and arterial dissection is not proven. However, when carefully evaluating the known facts, one does arrive at the conclusion that causality is at least likely. Even if it were merely a remote possibility, the precautionary principle in healthcare would mean that neck manipulations should be considered unsafe until proven otherwise. Moreover, there is no good evidence for assuming that neck manipulation is an effective therapy for any medical condition. Thus, the risk-benefit balance for chiropractic neck manipulation fails to be positive.
- Reliable estimates of the frequency of vascular accidents are prevented by the fact that underreporting is known to be substantial. In a survey of UK neurologists, for instance, under-reporting of serious complications was 100%. Those cases which are published often turn out to be incomplete. Of 40 case reports of serious adverse effects associated with spinal manipulation, nine failed to provide any information about the clinical outcome. Incomplete reporting of outcomes might therefore further increase the true number of fatalities.
- This review is focussed on deaths after chiropractic, yet neck manipulations are, of course, used by other healthcare professionals as well. The reason for this focus is simple: chiropractors are more frequently associated with serious manipulation-related adverse effects than osteopaths, physiotherapists, doctors or other professionals. Of the 40 cases of serious adverse effects mentioned above, 28 can be traced back to a chiropractor and none to a osteopath. A review of complications after spinal manipulations by any type of healthcare professional included three deaths related to osteopaths, nine to medical practitioners, none to a physiotherapist, one to a naturopath and 17 to chiropractors. This article also summarised a total of 265 vascular accidents of which 142 were linked to chiropractors. Another review of complications after neck manipulations published by 1997 included 177 vascular accidents, 32 of which were fatal. The vast majority of these cases were associated with chiropractic and none with physiotherapy. The most obvious explanation for the dominance of chiropractic is that chiropractors routinely employ high-velocity, short-lever thrusts on the upper spine with a rotational element, while the other healthcare professionals use them much more sparingly.
Another review summarised published cases of injuries associated with cervical manipulation in China. A total of 156 cases were found. They included the following problems:
- syncope (45 cases),
- mild spinal cord injury or compression (34 cases),
- nerve root injury (24 cases),
- ineffective treatment/symptom increased (11 cases),
- cervical spine fracture (11 cases),
- dislocation or semi-luxation (6 cases),
- soft tissue injury (3 cases),
- serious accident (22 cases) including paralysis, deaths and cerebrovascular accidents.
Manipulation including rotation was involved in 42% of all cases. In total, 5 patients died…
To sum up … chiropractic SMT can cause a wide range of very serious complications which occasionally can even be fatal. As there is no AE reporting system of such events, we nobody can be sure how frequently they occur.
[references from my text can be found in the book]This is an analysis that I have long hesitated to conduct. The reason for my hesitation is simple: some people might think it is vindictive, revengeful or ad hominem. After reflecting about it for years, I have now decided to go ahead with it (sorry, it’s a bit lengthy). This case study is not meant to be vindictive, but offers an important insight into the power of conflicts of interest in SCAM that are not financial but ideological. I think it is crucial that people are aware of and consider such conflicts carefully, and I can’t see how else I might demonstrate my point so plainly.
Dr Adrian White was a co-worker of mine for about 10 years. He became a trusted colleague, my ‘right hand’ man and even my deputy at my Exeter department. When I discovered that my trust had been misplaced, I did not prolong his contract (I will not dwell on this episode, those who are interested find it in my memoir). Adrian then got a senior research fellowship with Prof John Campbell (not my favourite colleague at Exeter) at the department of general practice where he continued his research on acupuncture for about 10 more years largely unsupervised.
Adrian had been an acupuncturist body and soul (in fact, I had never before met anyone so utterly convinced of the value of this therapy). When he joined my team, he was scientifically naive, and we spent many month trying to teach him how to think like a scientist. Initially, he found it very difficult to think critically about acupuncture. Later, I thought the problem was under control. Yet, most of his research in my department was guided by me and tightly supervised (i.e. I made sure that out studies were testing rather than promoting SCAM, and that our reviews were critical assessments of the existing evidence).
Thus there exist two separate and well-documented periods of a pro-acupuncture researcher:
- 10 years guided by me and members of my team;
- 10 years largely unsupervised.
What could be more tempting than to compare Adrian’s output during these two periods?
To do this, I looked up all of Adrian’s 120 publications on acupuncture and selected those 52 articles that generated factual new data (mostly clinical trials or systematic reviews). As it happens, they are numerically distributed almost equally within the two periods. The endpoints for my analysis were the directions of the conclusions of his papers. I therefore extracted, dated, and rated the 52 articles as follows:
- P = positive from the point of view of an acupuncture advocate,
- N = negative from the point of view of an acupuncture advocate.
- P/N = not clearly pointing in either direction.
To render this exercise transparent (occasionally, I was not entirely sure about my ratings), I copied all the 52 conclusions and provided links to the original papers so that anyone inferested is able to check easily.
Here are my findings. Articles 1 – 27 were published AFTER Adrian had left my department; articles 28 – 52 are his papers from the time while he worked with me.
- A definitive three-arm trial is feasible. Further follow-up reminders, minimum data collection and incentives should be considered to improve participant retention in the follow-up processes in the standardised advice and exercise booklet arm. (2016) P/N
- The available evidence suggests that adding acupuncture to symptomatic treatment of attacks reduces the frequency of headaches. Contrary to the previous findings, the updated evidence also suggests that there is an effect over sham, but this effect is small. The available trials also suggest that acupuncture may be at least similarly effective as treatment with prophylactic drugs. Acupuncture can be considered a treatment option for patients willing to undergo this treatment. As for other migraine treatments, long-term studies, more than one year in duration, are lacking. (2016) P
- The available results suggest that acupuncture is effective for treating frequent episodic or chronic tension-type headaches, but further trials – particularly comparing acupuncture with other treatment options – are needed. (2016) P
- Acupuncture during pregnancy appears to be associated with few AEs when correctly applied. (2014) P
- Although pooled estimates suggest possible short-term effects there is no consistent, bias-free evidence that acupuncture, acupressure, or laser therapy have a sustained benefit on smoking cessation for six months or more. However, lack of evidence and methodological problems mean that no firm conclusions can be drawn. Electrostimulation is not effective for smoking cessation. Well-designed research into acupuncture, acupressure and laser stimulation is justified since these are popular interventions and safe when correctly applied, though these interventions alone are likely to be less effective than evidence-based interventions. (2014) P
- The current evidence suggests that acupuncture may have some effects on drug dependence that have been missed because of choice of outcome in many previous studies, and future studies should use outcomes suggested by clinical experience. Body points and electroacupuncture, used in the original clinical observation, justify further research. (2013) P
- Acceptability is very high and may be maximised by taking a number of factors into account: full information should be provided before treatment begins; flexibility should be maintained in the appointment system and different levels of contact between fellow patients should be fostered; sufficient space and staffing should be provided and single-sex groups used wherever possible. (2012) P
- This is the first evaluation of nurse-led group (multibed) acupuncture clinics for patients with knee osteoarthritis to include a 2 year follow-up. It shows the practicability of offering a low-cost acupuncture service as an alternative to knee surgery and the service’s success in providing long-term symptom relief in about a third of patients. Using realistic assumptions, the cost consequences for the local commissioning group are an estimated saving of £100 000 a year. Sensitivity analyses are presented using different assumptions. (2012) P
- There is no consistent, bias-free evidence that acupuncture, acupressure, laser therapy or electrostimulation are effective for smoking cessation, but lack of evidence and methodological problems mean that no firm conclusions can be drawn. Further, well designed research into acupuncture, acupressure and laser stimulation is justified since these are popular interventions and safe when correctly applied, though these interventions alone are likely to be less effective than evidence-based interventions. (2011) P/N
- Eight (8) of 10 international acupuncture experts were able to reach consensus on the syndromes, symptoms, and treatment of postmenopausal women with hot flashes. The syndromes were similar to those used by practitioners in the ACUFLASH clinical trial, but there were considerable differences between the acupuncture points. This difference is likely to be the result of differences in approach of training schools, and whether it is relevant for clinical outcomes is not well understood. (2011) P
- 70% of those patients eligible to participate volunteered to do so; all participants had clinically identified MTrPs; a 100% completion rate was achieved for recorded self-assessment data; no serious adverse events were reported as a result of either intervention; and the end of treatment attrition rate was 17%. A phase III study is both feasible and clinically relevant. This study is currently being planned. (2010) P
- In conclusion, the results from all studies are in agreement with the hypothesis that acupuncture needling relieves hot flushes. There are few data however supporting the hypothesis that the effect of acupuncture is point specific. Future research should investigate whether there is a biological effect of needling on hot flushes or not, whether tailored treatment is superior to standardised treatment, and ways of delivering treatment that causes least discomfort and least cost. (2010) P
- Acupuncture can contribute to a more rapid reduction in vasomotor symptoms and increase in health-related quality of life in postmenopausal women but probably has no long-term effects. (2010) P
- within the context of this pilot study, the sham acupuncture intervention was found to be a credible control for acupuncture. This supports its use in a planned, definitive, randomised controlled trial on a similar whiplash injured population. (2009) N/P
- factors other than the TCM syndrome diagnoses and the point selection may be of importance regarding the outcome of the treatment. (2009) N/P
- Acupuncture plus self-care can contribute to a clinically relevant reduction in hot flashes and increased health-related quality of life in postmenopausal women. (2009) P
- the authors conclude that acupuncture could be a valuable non-pharmacological tool in patients with frequent episodic or chronic tension-type headaches. (2009) P
- there is consistent evidence that acupuncture provides additional benefit to treatment of acute migraine attacks only or to routine care. There is no evidence for an effect of ‘true’ acupuncture over sham interventions, though this is difficult to interpret, as exact point location could be of limited importance. Available studies suggest that acupuncture is at least as effective as, or possibly more effective than, prophylactic drug treatment, and has fewer adverse effects. Acupuncture should be considered a treatment option for patients willing to undergo this treatment. (2009) P
- We have conducted the first survey of the effects of provision of acupuncture in UK general practice, using data provided by the NHS, and uncovered a wide variation in the availability of the service in different areas. We have been unable to demonstrate any consistent differences in the prescribing or referral rates that could be due to the use of acupuncture in these practices. The wide variation in the data means that if such a trend exists, a very large survey would be needed to identify it. However, we discovered inaccuracies and variations in presentation of data by the PCTs which have made the numerical input, and hence our results, unreliable. Thus the practicalities of access to data and the problems with data accuracy would preclude a nationwide survey. (2008) P
- In conclusion, there is limited evidence deriving from one study that deep needling directly into myofascial trigger points has an overall treatment effect when compared with standardised care. Whilst the result of the meta-analysis of needling compared with placebo controls does not attain statistically significant, the overall direction could be compatible with a treatment effect of dry needling on myofascial trigger point pain. However, the limited sample size and poor quality of these studies highlights and supports the need for large scale, good quality placebo controlled trials in this area. (2009) P
- We conclude that limited evidence supports acupuncture use in treating pregnancy-related pelvic and back pain. Additional high-quality trials are needed to test the existing promising evidence for this relatively safe and popular complementary therapy. (2008) P
- Acupuncture appears to offer symptomatic improvement to some patients with fibromyalgia in a tertiary clinic who have failed to respond to other treatments. In view of its safety, further acupuncture research is justified in this population. (2007) P
- It is speculated that optimal results from acupuncture treatment for osteoarthritis of the knee may involve: climatic factors, particularly high temperature; high expectations of patients; minimum of four needles; electroacupuncture rather than manual acupuncture, and particularly, strong electrical stimulation to needles placed in muscle; and a course of at least 10 treatments. These factors offer some support to criteria for adequate acupuncture used in the recent review. In addition, ethnic and cultural factors may influence patients’ reporting of their symptoms, and different versions of an outcome measure are likely to differ in their sensitivity – both factors which may lead to apparent rather than real differences between studies. The many variables in a study are likely to be more tightly controlled in a single centre study than in multicentre studies. (2007) P
- Any effects of acupressure on smoking withdrawal, as an adjunct to the use of NRT and behavioural intervention, are unlikely to be detectable by the methods used here and further preliminary studies are required before the hypothesis can be tested. (2007) P
- Auricular acupuncture appears to be effective for smoking cessation, but the effect may not depend on point location. This calls into question the somatotopic model underlying auricular acupuncture and suggests a need to re-evaluate sham controlled studies which have used ‘incorrect’ points. Further experiments are necessary to confirm or refute these observational conclusions. (2006) P
- Acupuncture that meets criteria for adequate treatment is significantly superior to sham acupuncture and to no additional intervention in improving pain and function in patients with chronic knee pain. Due to the heterogeneity in the results, however, further research is required to confirm these findings and provide more information on long-term effects. (2007) P
- There is no consistent evidence that acupuncture, acupressure, laser therapy or electrostimulation are effective for smoking cessation, but methodological problems mean that no firm conclusions can be drawn. Further research using frequent or continuous stimulation is justified. (2006) N/P
- Acupuncture is not superior to sham treatment for recovery in activities of daily living and health-related quality of life after stroke, although there may be a limited effect on leg function in more severely affected patients. (2005) N
- The evidence from controlled trials is insufficient to conclude whether acupuncture is an effective treatment for depression, but justifies further trials of electroacupuncture. (2005) N
- Acupuncture effectively relieves chronic low back pain. No evidence suggests that acupuncture is more effective than other active therapies. (2005) N/P
- In view of the small number of studies and their variable quality, doubt remains about the effectiveness of acupuncture for gynaecological conditions. Acupuncture and acupressure appear promising for dysmenorrhoea, and acupuncture for infertility, and further studies are justified. (2003) N
- In conclusion, the results suggest that the procedure using the new device is indistinguishable from the same procedure using real needles in acupuncture naïve subjects, and is inactive, where the specific needle sensation (de qi) is taken as a surrogate measure of activity. It is therefore a valid control for acupuncture trials. The findings also lend support to the existence of de qi, a major concept underlying traditional Chinese acupuncture. (2002) N/P
- There is no clear evidence that acupuncture, acupressure, laser therapy or electrostimulation are effective for smoking cessation. (2002) N
- Collectively, these data imply that acupuncture is superior to various control interventions, although there is insufficient evidence to state whether it is superior to placebo. (2002) N/P
- In conclusion, the incidence of adverse events following acupuncture performed by doctors and physiotherapists can be classified as minimal; some avoidable events do occur. Acupuncture seems, in skilled hands, one of the safer forms of medical intervention. (2001) N/P
- Based on the evidence of rigorous randomised controlled trials, there is no compelling evidence to show that acupuncture is effective in stroke rehabilitation. Further, better-designed studies are warranted. (2001) N
- Although it has already been demonstrated that severe adverse events seem to be uncommon in standard practice, many serious cases of negligence have been found in the present review, suggesting that training system for acupuncturists (including medical doctors) should be improved and that unsupervised self-treatment should be discouraged. (2001) N
- Direct needling of myofascial trigger points appears to be an effective treatment, but the hypothesis that needling therapies have efficacy beyond placebo is neither supported nor refuted by the evidence from clinical trials. Any effect of these therapies is likely because of the needle or placebo rather than the injection of either saline or active drug. Controlled trials are needed to investigate whether needling has an effect beyond placebo on myofascial trigger point pain. (2001) N/P
- Although the incidence of minor adverse events associated with acupuncture may be considerable, serious adverse events are rare. Those responsible for establishing competence in acupuncture should consider how to reduce these risks. (2001) N
- In conclusion, this study does not provide evidence that this form of acupuncture is effective in the prevention of episodic tension-type headache. (2000) N
- The present study provides no strong evidence to support the hypothesis that the acupuncture point SP6 is more tender in women and in men. Recommendations for further investigations are discussed. (2000) N
- Acupuncture has not been demonstrated to be efficacious as a treatment for tinnitus on the evidence of rigorous randomized controlled trials. (2000) N
- We conclude that acupuncture continues to be associated with occasional, serious adverse events and fatalities. These events have no geographical limits. Most of these events are due to negligence. Everyone concerned with setting standards, delivering training, and maintaining competence in acupuncture should familiarise themselves with the lessons to be learnt from these untoward events. (2000) N
- Overall, the existing evidence suggests that acupuncture has a role in the treatment of recurrent headaches. However, the quality and amount of evidence is not fully convincing. There is urgent need for well-planned, large-scale studies to assess effectiveness and efficiency of acupuncture under real life conditions. (1999) N/P
- While the frequency of adverse effects of acupuncture is unknown and they may be rare, knowledge of normal anatomy and anatomical variations is essential for safe practice and should be reviewed by regulatory bodies and those responsible for training courses. (1999) N
- In conclusion, the hypothesis that acupuncture is efficacious in the treatment of neck pain is not based on the available evidence from sound clinical trials. Further studies are justified. (1999) N
- Even though all studies are in accordance with the notion that acupuncture is effective for temporomandibular joint dysfunction, this hypothesis requires confirmation through more rigorous investigations. (1999) N
- Acupuncture is not free of risks. All adverse events reported in 1997 would have been avoidable. The absolute number of cases is small, but the degree of underreporting remains unknown. (1999) N
- This form of electroacupuncture is no more effective than placebo in reducing nicotine withdrawal symptoms. (1998) N
- Acupuncture was shown to be superior to various control interventions, although there is insufficient evidence to state whether it is superior to placebo. (1998) N/P
- Considerable variation was observed in the scores awarded by the acupuncture experts. (1998) N
- It is therefore concluded that, according to the data published to date, the evidence that acupuncture is a useful adjunct for stroke rehabilitation is encouraging but not compelling. More and better trials are required to clarify this highly relevant issue. (1996) N
The results are remarkable (particularly considering that one would not expect unbiased studies or reviews of acupuncture to generate plenty of positive conclusions):
0 times N, 5 times N/P, 22 times P – after Adrian had left my department,
17 times N, 7 times N/P, 0 times P – while Adrian worked in my department.
From these figures, it is tempting to calculate the ratios for both periods of negative : positive conclusions:
zero versus infinite
If that is not impressive, I don’t know what is!
Looking just at the positive and the negative papers over the years:
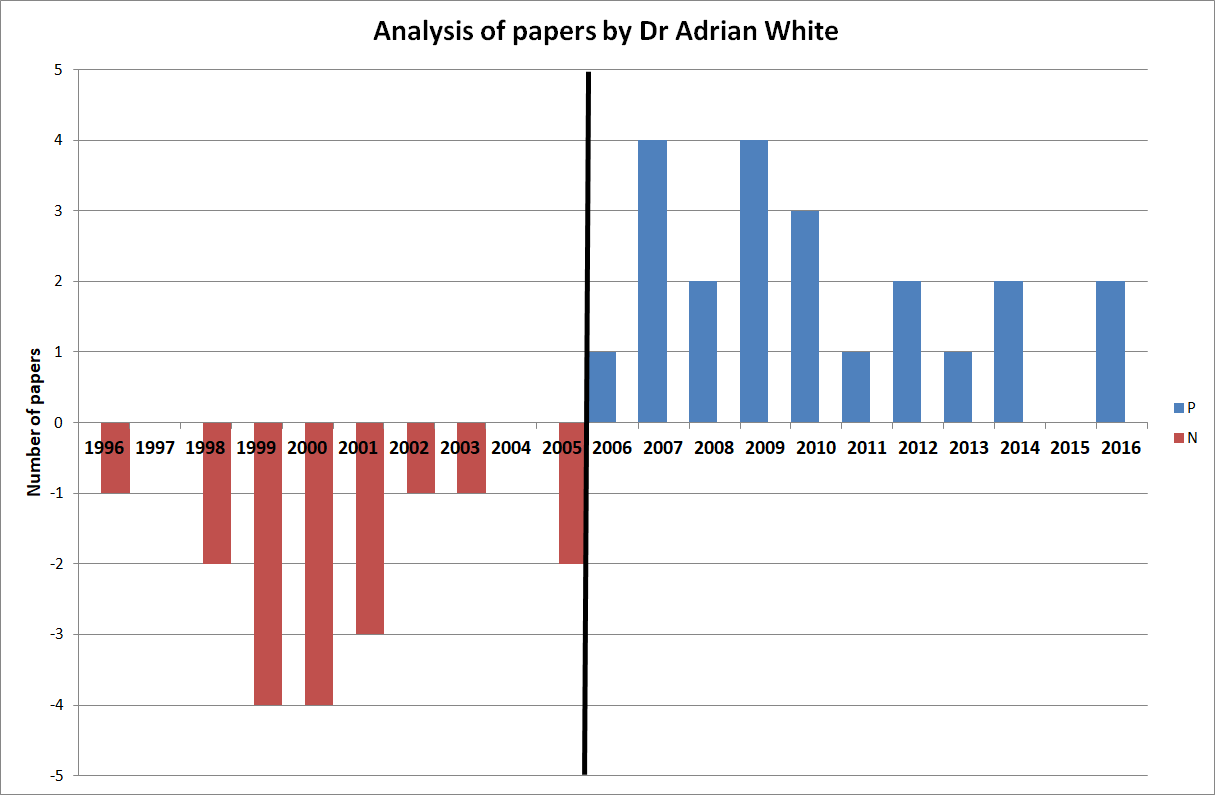 One could discuss these papers in more detail, but I think this is hardly necessary. Just a few highlights perhaps: look at articles No 5, 20 and 27 for examples of turning an essentially negative finding into a positive conclusion. Notice that Adrian conducted a clinical trial of acupuncture for smoking cessation (No 49) while working with me and later published uncritical positive reviews on the subject. Does this not indicate that he distrusted his own study because it had not generated the result he had hoped for?
One could discuss these papers in more detail, but I think this is hardly necessary. Just a few highlights perhaps: look at articles No 5, 20 and 27 for examples of turning an essentially negative finding into a positive conclusion. Notice that Adrian conducted a clinical trial of acupuncture for smoking cessation (No 49) while working with me and later published uncritical positive reviews on the subject. Does this not indicate that he distrusted his own study because it had not generated the result he had hoped for?
Of course, my analysis is merely a case study and therefore my findings are not generalisable. However, in my personal experience, the described phenomenon is by no means an exception in SCAM research. I have observed similar phenomena over and over again. Just look at the ALTERNATIVE MEDICINE HALL OF FAME that I created for this blog:
- John Weeks (editor of JCAM)
- Deepak Chopra (US entrepreneur)
- Cheryl Hawk (US chiropractor)
- David Peters (osteopathy, homeopathy, UK)
- Nicola Robinson (TCM, UK)
- Peter Fisher (homeopathy, UK)
- Simon Mills (herbal medicine, UK)
- Gustav Dobos (various, Germany)
- Claudia Witt (homeopathy, Germany and Switzerland)
- George Lewith (acupuncture, UK)
- John Licciardone (osteopathy, US)
But Adrian’s case might be unique because it allows us to make a longitudinal observation over two decades. And it suggests to me that an ideological bias can (and often is) so strong and indistructable that is re-emerges as soon as it is no longer kept under strict control.
I have long suspected that ideological conflicts of interest have a much more powerful influence in SCAM research than financial ones. Such an overpowering influence might even be characteristic to much of SCAM research. And because it can be so dominant, it seems important to know about. People reading research need to be aware that it originates from a biased source, and funders who finance research would be wise to think twice about supporting researchers who are likely to generate findings that are biased and therefore false-positive. In the final analysis, such research is worse than no research at all.
There are of course 2 types of osteopaths: the US osteopaths who are very close to real doctors, and the osteopaths from all other countries who are practitioners of so-called alternative medicine. This post, as all my posts on this subject, is about the latter category.
I was alerted to a paper entitled ‘Osteopathy under scrutiny’. It goes without saying that I thought it relevant; after all, scrutinising so-called altermative medicine (SCAM), such as osteopathy is one of the aims of this blog. The article itself is in German, but it has an English abstract:
Osteopathic medicine is a medical specialty that enjoys a high level of recognition and increasing popularity among patients. High-quality education and training are essential to ensure good and safe patient treatment. At a superficial glance, osteopathy could be misunderstood as a myth; accurately considered, osteopathic medicine is grounded in medical and scientific knowledge and solid theoretical and practical training. Scientific advances increasingly confirm the empirical experience of osteopathy. Although more studies on its efficacy could be conducted, there is sufficient evidence for a reasonable application of osteopathy. Current scientific studies show how a manually executed osteopathic intervention can induce tissue and even cellular reactions. Because the body actively responds to environmental stimuli, osteopathic treatment is considered an active therapy. Osteopathic treatment is individually applied and patients are seen as an integrated entity. Because of its typical systemic view and scientific interpretation, osteopathic medicine is excellently suited for interdisciplinary cooperation. Further work on external evidence of osteopathy is being conducted, but there is enough knowledge from the other pillars of evidence-based medicine (EBM) to support the application of osteopathic treatment. Implementing careful, manual osteopathic examination and treatment has the potential to cut healthcare costs. To ensure quality, osteopathic societies should be intimately involved and integrated in the regulation of the education, training, and practice of osteopathic medicine.
This does not sound as though the authors know what scutiny is. In fact, the abstract reads like a white-wash of quackery. Why might this be so? To answer this question, we need to look no further than to the ‘conflicts of interest’ where the authors state (my translation): K. Dräger and R. Heller state that, in addition to their activities as further education officers/lecturers for osteopathy (Deutsche Ärztegesellschaft für Osteopathie e. V. (DÄGO) and the German Society for Osteopathic Medicine e. V. (DGOM)) there are no conflicts of interest.
But, to tell you the truth, the article itself is worse, much worse that the abstract. Allow me to show you a few quotes (all my [sometimes free] translations).
- Osteopathic medicine is a therapeutic method based on the scientific findings from medical research.
- [The osteopath makes] diagnostic and therapeutic movements with the hands for evaluating limitations of movement. Thereby, a blocked joint as well as a reduced hydrodynamic or vessel perfusion can be identified.
- The indications of osteopathy are comparable to those of general medicine. Osteopathy can be employed from the birth of a baby up to the palliative care of a dying patient.
- Biostatisticians have recognised the weaknesses of RCTs and meta-analyses, as they merely compare mean values of therapeutic effects, and experts advocate a further evidence level in which statictical correlation is abandonnened in favour of individual causality and definition of cause.
- In ostopathy, the weight of our clinical experience is more important that external evidence.
- Research of osteopathic medicine … the classic cause/effect evaluation cannot apply (in support of this statement, the authors cite a ‘letter to the editor‘ from 1904; I looked it up and found that it does in no way substantiate this claim)
- Findings from anatomy, embryology, physiology, biochemistry and biomechanics which, as natural sciences, have an inherent evidence, strengthen in many ways the plausibility of osteopathy.
- Even if the statistical proof of the effectiveness of neurocranial techniques has so far been delivered only in part, basic research demonstrates that the effects of traction or compression of bogily tissue causes cellular reactions and regulatory processes.
What to make of such statements? And what to think of the fact that nowhere in the entire paper even a hint of ‘scrutiny’ can be detected? I don’t know about you, but for me this paper reflects very badly on both the authors and on osteopathy as a whole. If you ask me, it is an odd mixture of cherry-picking the evidence, misunderstanding science, wishful thinking and pure, unadulterated bullshit.
You urgently need to book into a course of critical thinking, guys!
