bias
Today is the start of chiropractic awareness week 2022. On this occasion the BCA states most categorically: First and foremost, chiropractic is a statutorily regulated healthcare profession, supported by evidence, which offers a safe form of treatment for patients with a range of conditions. Here I am tempted to cite my friend Simon Singh:
THEY HAPPILY PROMOTE BOGUS TREATMENTS
I am, of course, particularly impressed by the BCA’s assurance of safety. In my view, the safety issue needs to be addressed more urgently than any other in the realm of chiropractic. So, to make a meaningful contribution to the current chiropractic awareness week, I conducted a few Medline searches to identify all publications of 2022 on chiropractic/spinal manipulation risks.
This is what I found:
Objective: Patients can be at risk of carotid artery dissection and ischemic stroke after cervical chiropractic manipulation. However, such risks are rarely reported and raising awareness can increase the safety of chiropractic manipulations.
Case report: We present two middle-aged patients with carotid artery dissection leading to ischemic stroke after receiving chiropractic manipulation in Foshan, Guangdong Province, China. Both patients had new-onset pain in their necks after receiving chiropractic manipulations. Excess physical force during chiropractic manipulation may present a risk to patients. Patient was administered with recombinant tissue plasminogen activator after radiological diagnoses. They were prescribed 100 mg and clopidogrel 75 mg daily for 3 months as dual antiplatelet therapy. There were no complications over the follow-up period.
Conclusion: These cases suggest that dissection of the carotid artery can occur as the result of chiropractic manipulations. Patients should be diagnosed and treated early to achieve positive outcomes. The safety of chiropractic manipulations should be increased by raising awareness about the potential risks.
Spontaneous intracranial hypotension (SIH) still remains an underdiagnosed etiology of new-onset headache. Important risk factors include chiropractic manipulation (CM). We present a case of a 36-year-old Filipino woman who presented with severe bifrontal and postural headache associated with dizziness, vomiting, and doubling of vision. A cranial computed tomography scan was done which showed an acute subdural hematoma (SDH) at the interhemispheric area. Pain medications were given which afforded minimal relief. On history, the headaches occurred 2 weeks after cervical CM. Cranial and cervical magnetic resonance imaging revealed findings supportive of intracranial hypotension and neck trauma, respectively. The patient improved with conservative management. We found 12 articles on SIH and CM after a systematic review of literature. Eleven patients (90.9%) initially presented with orthostatic headache. Eight patients (66.7%) were initially treated conservatively but only 5 (62.5%) had complete recovery. Recovery was achieved within 14 days from start of supportive therapy. Among the 3 patients who failed conservative treatment, 2 underwent non-directed epidural blood patch and one required neurosurgical intervention. This report highlights that a thorough history is warranted in patients with new onset headache. A history of CM must be actively sought. The limited evidence from the case reports showed that patients with SIH and SDH but with normal neurologic examination and minor spinal pathology can be managed conservatively for less than 2 weeks. This review showed that conservative treatment in a closely monitored environment may be an appropriate first line treatment.
Introduction: Cranio-cervical artery dissection (CeAD) is a common cause of cerebrovascular events in young subjects with no clear treatment strategy established. We evaluated the incidence of major adverse cardiovascular events (MACE) in CeAD patients treated with and without stent placement.
Methods: COMParative effectiveness of treatment options in cervical Artery diSSection (COMPASS) is a single high-volume center observational, retrospective longitudinal registry that enrolled consecutive CeAD patients over a 2-year period. Patients were ≥ 18 years of age with confirmed extra- or intracranial CeAD on imaging. Enrolled participants were followed for 1 year evaluating MACE as the primary endpoint.
Results: One-hundred ten patients were enrolled (age 53 ± 15.9, 56% Caucasian, and 50% male, BMI 28.9 ± 9.2). Grade I, II, III, and IV blunt vascular injury was noted in 16%, 33%, 19%, and 32%, respectively. Predisposing factors were noted in the majority (78%), including sneezing, carrying heavy load, chiropractic manipulation. Stent was placed in 10 (10%) subjects (extracranial carotid n = 9; intracranial carotid n = 1; extracranial vertebral n = 1) at the physician’s discretion along with medical management. Reasons for stent placement were early development of high-grade stenosis or expanding pseudoaneurysm. Stented patients experienced no procedural or in-hospital complications and no MACE between discharge and 1 year follow up. CeAD patients treated with medical management only had 14% MACE at 1 year.
Conclusion: In this single high-volume center cohort of CeAD patients, stenting was found to be beneficial, particularly with development of high-grade stenosis or expanding pseudoaneurysm. These results warrant confirmation by a randomized clinical trial.
Background: Manipulation and mobilisation for low back pain are presented in an evidence-based manner with regard to mechanisms of action, indications, efficacy, cost-effectiveness ratio, user criteria and adverse effects. Terms such as non-specific or specific are replaced by the introduction of “entities” related to possible different low back pain forms.
Efficacy: MM is effective for acute and chronic low back pain in terms of pain relief, recovery of function and relapse prevention. It is equally effective but less risky compared to other recommended therapies. MM can be used alone in acute cases and not only in the case of chronic low back pain where it is always and necessarily part of a multimodal therapy programme, especially in combination with activating measures. The users of MM should exclusively be physician specialists trained according to the criteria of the German Medical Association (Bundesärztekammer) with an additional competence in manual medicine or appropriately trained certified therapists. The application of MM follows all rules of Good Clinical Practice.
Adverse effects: Significant adverse effects of MM for low back pain are reported in the international literature with a frequency of 1 per 50,000 to 1 per 3.7 million applications, i.e. MM for low back pain is practically risk-free and safe if performed according to the rules of the European Training Requirements of the UEMS.
Studies have reported that mild adverse events (AEs) are common after manual therapy and that there is a risk of serious injury. We aimed to assess the safety of Chuna manipulation therapy (CMT), a traditional manual Korean therapy, by analysing AEs in patients who underwent this treatment. Patients who received at least one session of CMT between December 2009 and March 2019 at 14 Korean medicine hospitals were included. Electronic patient charts and internal audit data obtained from situation report logs were retrospectively analysed. All data were reviewed by two researchers. The inter-rater agreement was assessed using the Cohen’s kappa coefficient, and reliability analysis among hospitals was assessed using Cronbach’s Alpha coefficient. In total, 2,682,258 CMT procedures were performed in 289,953 patients during the study period. There were 50 AEs, including worsened pain (n = 29), rib fracture (n = 11), falls during treatment (n = 6), chest pain (n = 2), dizziness (n = 1), and unpleasant feeling (n = 1). The incidence of mild to moderate AEs was 1.83 (95% confidence interval [CI] 1.36-2.39) per 100,000 treatment sessions, and that of severe AEs was 0.04 (95% CI 0.00-0.16) per 100,000 treatment sessions. Thus, AEs of any level of severity were very rare after CMT. Moreover, there were no instances of carotid artery dissection or spinal cord injury, which are the most severe AEs associated with manual therapy in other countries.
_______________________________
This is not too bad after all!
Five papers are clearly better than nothing.
What conclusions might be drawn from my mini-review?
I think it might be safe to say:
- There is not much but at least some research going on in this area.
- The risks of chiropractic/spinal manipulation are real and are being recognized.
- BUT NOT BY CHIROPRACTORS! The most remarkable feature of the 5 papers, I think, is that none originates from a chiropractic team.
Thus, allow me to make a suggestion to chiropractors worldwide: Instead of continuing with HAPPILY PROMOTING BOGUS TREATMENTS, what about using the ‘chiropractic awareness week’ to raise awareness of the urgent necessity to research the safety of your treatments?
No 10-year follow-up study of so-called alternative medicine (SCAM) for lumbar intervertebral disc herniation (LDH) has so far been published. Therefore, the authors of this paper performed a prospective 10-year follow-up study on the integrated treatment of LDH in Korea.
One hundred and fifty patients from the baseline study, who initially met the LDH diagnostic criteria with a chief complaint of radiating pain and received integrated treatment, were recruited for this follow-up study. The 10-year follow-up was conducted from February 2018 to March 2018 on pain, disability, satisfaction, quality of life, and changes in a herniated disc, muscles, and fat through magnetic resonance imaging.
Sixty-five patients were included in this follow-up study. Visual analogue scale score for lower back pain and radiating leg pain were maintained at a significantly lower level than the baseline level. Significant improvements in Oswestry disability index and quality of life were consistently present. MRI confirmed that disc herniation size was reduced over the 10-year follow-up. In total, 95.38% of the patients were either “satisfied” or “extremely satisfied” with the treatment outcomes and 89.23% of the patients claimed their condition “improved” or “highly improved” at the 10-year follow-up.
The authors concluded that the reduced pain and improved disability was maintained over 10 years in patients with LDH who were treated with nonsurgical Korean medical treatment 10 years ago. Nonsurgical traditional Korean medical treatment for LDH produced beneficial long-term effects, but future large-scale randomized controlled trials for LDH are needed.
This study and its conclusion beg several questions:
WHAT DID THE SCAM CONSIST OF?
The answer is not provided in the paper; instead, the authors refer to 3 previous articles where they claim to have published the treatment schedule:
The treatment package included herbal medicine, acupuncture, bee venom pharmacopuncture and Chuna therapy (Korean spinal manipulation). Treatment was conducted once a week for 24 weeks, except herbal medication which was taken twice daily for 24 weeks; (1) Acupuncture: frequently used acupoints (BL23, BL24, BL25, BL31, BL32, BL33, BL34, BL40, BL60, GB30, GV3 and GV4)10 ,11 and the site of pain were selected and the needles were left in situ for 20 min. Sterilised disposable needles (stainless steel, 0.30×40 mm, Dong Bang Acupuncture Co., Korea) were used; (2) Chuna therapy12 ,13: Chuna is a Korean spinal manipulation that includes high-velocity, low-amplitude thrusts to spinal joints slightly beyond the passive range of motion for spinal mobilisation, and manual force to joints within the passive range; (3) Bee venom pharmacopuncture14: 0.5–1 cc of diluted bee venom solution (saline: bee venom ratio, 1000:1) was injected into 4–5 acupoints around the lumbar spine area to a total amount of 1 cc using disposable injection needles (CPL, 1 cc, 26G×1.5 syringe, Shinchang medical Co., Korea); (4) Herbal medicine was taken twice a day in dry powder (2 g) and water extracted decoction form (120 mL) (Ostericum koreanum, Eucommia ulmoides, Acanthopanax sessiliflorus, Achyranthes bidentata, Psoralea corylifolia, Peucedanum japonicum, Cibotium barometz, Lycium chinense, Boschniakia rossica, Cuscuta chinensis and Atractylodes japonica). These herbs were selected from herbs frequently prescribed for LBP (or nerve root pain) treatment in Korean medicine and traditional Chinese medicine,15 and the prescription was further developed through clinical practice at Jaseng Hospital of Korean Medicine.9 In addition, recent investigations report that compounds of C. barometz inhibit osteoclast formation in vitro16 and A. japonica extracts protect osteoblast cells from oxidative stress.17 E. ulmoides has been reported to have osteoclast inhibitive,18 osteoblast-like cell proliferative and bone mineral density enhancing effects.19 Patients were given instructions by their physician at treatment sessions to remain active and continue with daily activities while not aggravating pre-existing symptoms. Also, ample information about the favourable prognosis and encouragement for non-surgical treatment was given.
The traditional Korean spinal manipulations used (‘Chuna therapy’ – the references provided for it do NOT refer to this specific way of manipulation) seemed interesting, I thought. Here is an explanation from an unrelated paper:
Chuna, which is a traditional manual therapy practiced by Korean medicine doctors, has been applied to various diseases in Korea. Chuna manual therapy (CMT) is a technique that uses the hand, other parts of the doctor’s body or other supplementary devices such as a table to restore the normal function and structure of pathological somatic tissues by mobilization and manipulation. CMT includes various techniques such as thrust, mobilization, distraction of the spine and joints, and soft tissue release. These techniques were developed by combining aspects of Chinese Tuina, chiropratic, and osteopathic medicine.[13] It has been actively growing in Korea, academically and clinically, since the establishment of the Chuna Society (the Korean Society of Chuna Manual Medicine for Spine and Nerves, KSCMM) in 1991.[14] Recently, Chuna has had its effects nationally recognized and was included in the Korean national health insurance in March 2019.[15]
This almost answers the other questions I had. Almost, but not quite. Here are two more:
- The authors conclude that the SCAM produced beneficial long-term effects. But isn’t it much more likely that the outcomes their uncontrolled observations describe are purely or at least mostly a reflection of the natural history of lumbar disc herniation?
- If I remember correctly, I learned a long time ago in medical school that spinal manipulation is contraindicated in lumbar disc herniation. If that is so, the results might have been better, if the patients of this study had not received any SCAM at all. In other words, are the results perhaps due to firstly the natural history of the condition and secondly to the detrimental effects of the SCAM the investigators applied?
If I am correct, this would then be the 4th article reporting the findings of a SCAM intervention that aggravated lumbar disc herniation.
PS
I know that this is a mere hypothesis but it is at least as plausible as the conclusion drawn by the authors.
Ginseng plants belong to the genus Panax and include:
- Panax ginseng (Korean ginseng),
- Panax notoginseng (South China ginseng),
- and Panax quinquefolius (American ginseng).
They are said to have a range of therapeutic activities, some of which could render ginseng a potential therapy for viral or post-viral infections. Ginseng has therefore been used to treat fatigue in various patient groups and conditions. But does it work for chronic fatigue syndrome (CFS), also often called myalgic encephalomyelitis (ME)? This condition is a complex, little-understood, and often disabling chronic illness for which no curative or definitive therapy has yet been identified.
This systematic review aimed to assess the current state of evidence regarding ginseng for CFS. Multiple databases were searched from inception to October 2020. All data was extracted independently and in duplicates. Outcomes of interest included the effectiveness and safety of ginseng in patients with CFS.
A total of two studies enrolling 68 patients were deemed eligible: one randomized clinical trial and one prospective observational study. The certainty of evidence in the effectiveness outcome was low and moderate in both studies, while the safety evidence was very low as reported from one study.
The authors concluded that the study findings highlight a potential benefit of ginseng therapy in the treatment of CFS. However, we are not able to draw firm conclusions due to limited clinical studies. The paucity of data warrants limited confidence. There is a need for future rigorous studies to provide further evidence.
To get a feeling of how good or bad the evidence truly is, we must of course look at the primary studies.
The prospective observational study turns out to be a mere survey of patients using all sorts of treatments. It included 155 subjects who provided information on fatigue and treatments at baseline and follow-up. Of these subjects, 87% were female and 79% were middle-aged. The median duration of fatigue was 6.7 years. The percentage of users who found a treatment helpful was greatest for coenzyme Q10 (69% of 13 subjects), dehydroepiandrosterone (DHEA) (65% of 17 subjects), and ginseng (56% of 18 subjects). Treatments at 6 months that predicted subsequent fatigue improvement were vitamins (p = .08), vigorous exercise (p = .09), and yoga (p = .002). Magnesium (p = .002) and support groups (p = .06) were strongly associated with fatigue worsening from 6 months to 2 years. Yoga appeared to be most effective for subjects who did not have unclear thinking associated with fatigue.
The second study investigated the effect of Korean Red Ginseng (KRG) on chronic fatigue (CF) by various measurements and objective indicators. Participants were randomized to KRG or placebo group (1:1 ratio) and visited the hospital every 2 weeks while taking 3 g KRG or placebo for 6 weeks and followed up 4 weeks after the treatment. The fatigue visual analog score (VAS) declined significantly in each group, but there were no significant differences between the groups. The 2 groups also had no significant differences in the secondary outcome measurements and there were no adverse events. Sub-group analysis indicated that patients with initial fatigue VAS below 80 mm and older than 50 years had significantly greater reductions in the fatigue VAS if they used KRG rather than placebo. The authors concluded that KRG did not show absolute anti-fatigue effect but provided the objective evidence of fatigue-related measurement and the therapeutic potential for middle-aged individuals with moderate fatigue.
I am at a loss in comprehending how the authors of the above-named review could speak of evidence for potential benefit. The evidence from the ‘observational study’ is largely irrelevant for deciding on the effectiveness of ginseng, and the second, more rigorous study fails to show that ginseng has an effect.
So, is ginseng a promising treatment for ME?
I doubt it.
A multi-disciplinary research team assessed the effectiveness of interventions for acute and subacute non-specific low back pain (NS-LBP) based on pain and disability outcomes. For this purpose, they conducted a systematic review of the literature with network meta-analysis.
They included all 46 randomized clinical trials (RCTs) involving adults with NS-LBP who experienced pain for less than 6 weeks (acute) or between 6 and 12 weeks (subacute). Non-pharmacological treatments (eg, manual therapy) including acupuncture and dry needling or pharmacological treatments for improving pain and/or reducing disability considering any delivery parameters were included. The comparator had to be an inert treatment encompassing sham/placebo treatment or no treatment. The risk of bias was
- low in 9 trials (19.6%),
- unclear in 20 (43.5%),
- high in 17 (36.9%).
At immediate-term follow-up, for pain decrease, the most efficacious treatments against an inert therapy were:
- exercise (standardised mean difference (SMD) -1.40; 95% confidence interval (CI) -2.41 to -0.40),
- heat wrap (SMD -1.38; 95% CI -2.60 to -0.17),
- opioids (SMD -0.86; 95% CI -1.62 to -0.10),
- manual therapy (SMD -0.72; 95% CI -1.40 to -0.04).
- non-steroidal anti-inflammatory drugs (NSAIDs) (SMD -0.53; 95% CI -0.97 to -0.09).
Similar findings were confirmed for disability reduction in non-pharmacological and pharmacological networks, including muscle relaxants (SMD -0.24; 95% CI -0.43 to -0.04). Mild or moderate adverse events were reported in the opioids (65.7%), NSAIDs (54.3%), and steroids (46.9%) trial arms.
The authors concluded that NS-LBP should be managed with non-pharmacological treatments which seem to mitigate pain and disability at immediate-term. Among pharmacological interventions, NSAIDs and muscle relaxants appear to offer the best harm-benefit balance.
The authors point out that previous published systematic reviews on spinal manipulation, exercise, and heat wrap did overlap with theirs: exercise (eg, motor control exercise, McKenzie exercise), heat wrap, and manual therapy (eg, spinal manipulation, mobilization, trigger points or any other technique) were found to reduce pain intensity and disability in adults with acute and subacute phases of NS-LBP.
I would add (as I have done so many times before) that the best approach must be the one that has the most favorable risk/benefit balance. Since spinal manipulation is burdened with considerable harm (as discussed so many times before), exercise and heat wraps seem to be preferable. Or, to put it bluntly:
if you suffer from NS-LBP, see a physio and not osteos or chiros!
Yes, Today is ‘WORLD SLEEP DAY‘ and you are probably in bed hoping this post will put you back to sleep.
This study aimed to synthesise the best available evidence on the safety and efficacy of using moxibustion and/or acupuncture to manage cancer-related insomnia (CRI).
The PRISMA framework guided the review. Nine databases were searched from its inception to July 2020, published in English or Chinese. Randomised clinical trials (RCTs) of moxibustion and or acupuncture for the treatment of CRI were selected for inclusion. The methodological quality was assessed using the method suggested by the Cochrane collaboration. The Cochrane Review Manager was used to conduct a meta-analysis.
Fourteen RCTs met the eligibility criteria; 7 came from China. Twelve RCTs used the Pittsburgh Sleep Quality Index (PSQI) score as continuous data and a meta-analysis showed positive effects of moxibustion and or acupuncture (n = 997, mean difference (MD) = -1.84, 95% confidence interval (CI) = -2.75 to -0.94, p < 0.01). Five RCTs using continuous data and a meta-analysis in these studies also showed significant difference between two groups (n = 358, risk ratio (RR) = 0.45, 95% CI = 0.26-0.80, I 2 = 39%).
The authors concluded that the meta-analyses demonstrated that moxibustion and or acupuncture showed a positive effect in managing CRI. Such modalities could be considered an add-on option in the current CRI management regimen.
Even at the risk of endangering your sleep, I disagree with this conclusion. Here are some of my reasons:
- Chinese acupuncture trials invariably are positive which means they are as reliable as a 4£ note.
- Most trials were of poor methodological quality.
- Only one made an attempt to control for placebo effects.
- Many followed the A+B versus B design which invariably produces (false-) positive results.
- Only 4 out of 14 studies mentioned adverse events which means that 10 violated research ethics.
Sorry to have disturbed your sleep!
This review assessed the magnitude of reporting bias in trials assessing homeopathic treatments and its impact on evidence syntheses.
A cross-sectional study and meta-analysis. Two persons independently searched Clinicaltrials.gov, the EU Clinical Trials Register and the International Clinical Trials Registry Platform up to April 2019 to identify registered homeopathy trials. To determine whether registered trials were published and to detect published but unregistered trials, two persons independently searched PubMed, Allied and Complementary Medicine Database, Embase and Google Scholar up to April 2021. For meta-analyses, the authors used random effects models to determine the impact of unregistered studies on meta-analytic results.
The investigators reported the proportion of registered but unpublished trials and the proportion of published but unregistered trials. They also assessed whether primary outcomes were consistent between registration and publication
Since 2002, almost 38% of registered homeopathy trials have remained unpublished, and 53% of published randomised controlled trials (RCTs) have not been registered. Retrospective registration was more common than prospective registration. Furthermore, 25% of primary outcomes were altered or changed compared with the registry. Although we could detect a statistically significant trend toward an increase of registrations of homeopathy trials (p=0.001), almost 30% of RCTs published during the past 5 years had not been registered.
A meta-analysis stratified by registration status of RCTs revealed substantially larger treatment effects of unregistered RCTs (SMD: −0.53, 95% CI −0.87 to −0.20) than registered RCTs (SMD: −0.14, 95% CI −0.35 to 0.07).
The authors concluded that registration of published trials was infrequent, many registered trials were not published and primary outcomes were often altered or changed. This likely affects the validity of the body of evidence of homeopathic literature and may overestimate the true treatment effect of homeopathic remedies.
An obvious investigation to do (why did I not have this idea?)!
And a finding that will surprise few (except fans of homeopathy who will, of course, dispute it).
The authors also mention that reporting biases are likely to have a substantial impact on the estimated treatment effect of homeopathy. Using data from a highly cited meta-analysis of homeopathy RCTs, our example showed that unregistered trials yielded substantially larger treatment effects than registered trials. They also caution that, because of the reporting biases identified in their analysis, effect estimates of meta-analyses of homeopathy trials might substantially overestimate the true treatment effect of homeopathic remedies and need to be interpreted cautiously.
In other words, the few reviews suggesting that homeopathy works beyond placebo (and are thus celebrated by homeopaths) are most likely false-positive. And the many reviews showing that homeopathy does not work would demonstrate this fact even clearer if the reporting bias had been accounted for.
Or, to put it bluntly:
The body of evidence on homeopathy is rotten to the core and therefore not reliable.
Vaccine hesitancy is currently recognized by the WHO as a major threat to global health. During the COVID-19 pandemic, there has been a growing interest in the role of social media in the propagation of false information and fringe narratives regarding vaccination. Using a sample of approximately 60 billion tweets, Danish investigators conducted a large-scale analysis of the vaccine discourse on Twitter. They used methods from deep learning and transfer learning to estimate the vaccine sentiments expressed in tweets, then categorize individual-level user attitudes towards vaccines. Drawing on an interaction graph representing mutual interactions between users, They analyzed the interplay between vaccine stances, interaction network, and the information sources shared by users in vaccine-related contexts.
The results show that strongly anti-vaccine users frequently share content from sources of a commercial nature; typically sources that sell alternative health products for profit. An interesting aspect of this finding is that concerns regarding commercial conflicts of interests are often cited as one of the major factors in vaccine hesitancy.
The authors furthermore demonstrate that the debate is highly polarized, in the sense that users with similar stances on vaccination interact preferentially with one another. Extending this insight, the authors provide evidence of an epistemic echo chamber effect, where users are exposed to highly dissimilar sources of vaccine information, enforcing the vaccination stance of their contacts.
The authors concluded that their findings highlight the importance of understanding and addressing vaccine mis- and disinformation in the context in which they are disseminated in social networks.
In the article, the authors comment that their findings paint a picture of the vaccine discourse on Twitter as highly polarized, where users who express similar sentiments regarding vaccinations are more likely to interact with one another, and tend to share contents from similar sources. Focusing on users whose vaccination stances are the positive and negative extremes of the spectrum, we observe relatively disjoint ‘epistemic echo chambers’ which imply that members of the two groups of users rarely interact, and in which users experience highly dissimilar ‘information landscapes’ depending on their stance. Finally, we find that strongly anti-vaccine users much more frequently share information from actors with a vested commercial interest in promoting medical misinformation.
One implication of these findings is that online (medical) misinformation may present an even greater problem than previously thought, because beliefs and behaviors in tightly knit, internally homogeneous communities are more resilient, and provide fertile ground for fringe narratives, while mainstream information is attenuated. Furthermore, such polarization of communities may become self-perpetuating, because individuals avoid those not sharing their views, or because exposure to mainstream information might further entrench fringe viewpoints.
On Amazon, someone commented as follows on my biography of Prince Charles:
… Dr. Ernst goes on digressions that mostly seem intended to make Prince Charles look bad. There’s a long chapter on Laurens van der Post, who influenced Prince Charles as a youth, and a lot about somewhat unsavory things he did. So what? …
This made me think. I read the chapter again and find it hard to agree with the comment. To me, this chapter is a short (~2000 words) and essential part of the book. Judge for yourself; here are a few excerpts from it: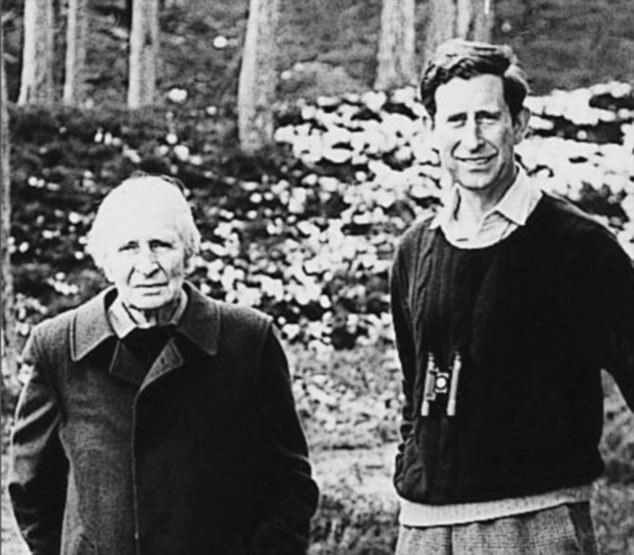
“It seemed to have been a union of mutual needs, between a Prince longing to find meaning in his existence and a storyteller who could weave apparent answers out of thin air.” Laurence van der Post was oozing charm and charisma and sensed that “for the Prince, there was a missing dimension”, as Jonathan Dimbleby put it. By 1975, the two men had formed such a close rapport that van der Post felt able to counsel him about spiritual matters, urging him to explore the ‘old world of the spirit’ and ‘the inward way’ towards truth and understanding. Van der Post suggested the two make a seven week journey into the Kalahari desert. This, he believed, would introduce Charles to the spirit world. Preparations were made in 1977 but, in the end, the plan had to be abandoned. Instead, the two later went to Kenya where they spent 5 days of long walks and “intense conversation”.
Van der Post urged Charles to play “a dynamic and as yet unimagined role to suit the future shape of a fundamentally reappraised and renewed modern society”, a reappraisal that would be “so widespread and go so deep that it will involve a prolonged fight for all that is good and creative in the human imagination.” An aspect of this fight, he claimed, would be “to restore the human being to a lost natural aspect of his own spirit; to restore his relevance for life and his love of nature, and to draw closer to the original blueprint and plan of life…”
Laurence left an interview for posthumous publication; in it, he expressed his hope that Charles would never become king, as this would imprison him, it would be more important that Charles continues to be a great prince. “He’s been brought up in a terrible way … He’s a natural Renaissance man, a man who believes in the wholeness and totality of life … Why should it be that if you try to contemplate your natural self that you should be thought to be peculiar?”
“For 20 years they had most intimate conversations and correspondence … with a steady flow of reassurance and encouragement, political and diplomatic advice, memoranda, draft speeches and guidance for reading”. Van der Post introduced Charles to the teachings of Carl Jung and his concept of the ‘collective unconscious’ that binds all humans together regardless whether they are Kalahari bushmen or princes. On the behest of van der Post, Charles began to record his dreams which van der Post then interpreted according to Jung’s theories. In the late 1970s van der Post tried to convince Charles to give up all his duties and withdraw from the world completely in search for an ‘inner world truth’. This plan too was aborted.
All biographers agree that van der Post was the strongest intellectual influence of Charles’ life.
- Charles sought van der Post’s advice and spiritual guidance on numerous occasions.
- When William was born, he made van der Post his godfather.
- When Charles’ marriage to Diana ran into difficulties, the couple was counselled by van der Post.
- Charles invited Laurence regularly to Highgrove, Sandringham and Balmoral.
- Charles visited van der Post on his deathbed.
- After Laurence’s death, Charles created a series of annual lectures hosted in van der Post’s memory which he hosted in St James’ Palace.
…
…
…
Charles’ notions about medicine were unquestionably inspired by van der Post. Laurence. He, for instance, bemoaned the inadequacy of conventional medicine and wrote: “Even if doctors did … use dreams and their decoding as an essential part of their diagnostic equipment and perhaps could confront cancer at the point of entry, how are they to turn it aside, unless they are humble enough to keep their instruments in their cases and look for some new form of navigation over an uncharted sea of the human spirit?” As we will see in the next chapters, van der Post’s influence shines through in many of Charles’ speeches. Moreover, it contributed to the attitude of many critical observers towards Charles. Christopher Hitchens is but one example for many:
“We have known for a long time that Prince Charles’ empty sails are so rigged as to be swelled by any passing waft or breeze of crankiness and cant. He fell for the fake anthropologist Laurens van der Post. He was bowled over by the charms of homeopathic medicine. He has been believably reported as saying that plants do better if you talk to them in a soothing and encouraging way… The heir to the throne seems to possess the ability to surround himself—perhaps by some mysterious ultramagnetic force?—with every moon-faced spoon-bender, shrub-flatterer, and water-diviner within range.”
The following chapters will show that Hitchens might not have been far off the mark.
___________________________
Yes, I do feel that the chapter is essential for the book. It explains how Charles’ love affair with alternative medicine got started and why it would become so intense and durable. Without it, the reader would not be able to understand the rest of the book. Moreover, it is important to demonstrate that van der Post was a charlatan and an accomplished liar. This is relevant because, in later life, Charles’ skill to choose adequate advisors was often wanting.
Stress is associated with a multitude of physical and psychological health impairments. To tackle these health disorders, over-the-counter (OTC) products like Neurodoron® are popular since they are considered safe and tolerable. One tablet of this anthroposophic remedy contains the following active ingredients:
- 83.3 mg Aurum metallicum praeparatum trituration (trit.) D10,
- 83.3 mg Kalium phosphoricicum trit. D6,
- 8.3 mg Ferrum-Quarz trit. D2.
Experience reports and first studies indicate that Neurodoron® is efficient in the treatment of stress-associated health symptoms. “To confirm this” (!!!), a non-interventional study (NIS) with pharmacies was conducted.
The NIS was planned to enroll female and male patients who suffered from nervous exhaustion with symptoms caused by acute and/or chronic stress. The main outcome measures were characteristic stress symptoms, stress burden, and perceived stress. Further outcome measures included perceived efficacy and tolerability of the product as assessed by the patients and collection of adverse drug reactions (ADRs). A study duration of about 21 days with a recommended daily dose of 3–4 tablets was set.
In total, 279 patients were enrolled at 74 German pharmacies. The analyzed set (AS) included 272 patients (mean age 44.8 ± 14.4 years, 73.9% female). 175 patients of the AS completed the NIS. During the study, all stress symptoms declined significantly (total score 18.1 vs. 12.1 (of max. 39 points), < 0.0001). Furthermore, a reduction of stress burden (relative difference in stress burden, VAS = −29.1%, < 0.0001) was observed. For most patients, perceived stress was reduced at the study end (PSQ total score decreased in 70.9% of the patients). 75.9% of the study population rated the product efficacy as “good” or “very good” and 96.6% rated its tolerability as “good” or “very good.” One uncritical ADR was reported.
The authors concluded that this study adds information on the beneficial effects of Neurodoron® in self-medication. The results from this NIS showed a marked reduction in stress burden and perceived stress, along with an excellent safety profile of the medicinal product (MP) Neurodoron®. Further trials are required to confirm these results.
I beg to differ!
The study had no control group and therefore one cannot possibly attribute any of the observed changes to the anthroposophic remedy. They are more likely to be due to:
- the natural history of the condition,
- regression towards the mean,
- a placebo effects,
- other treatments administered during the trial period.
Sadly, the authors discuss none of these possibilities in their paper.
In view of this, I am tempted to rephrase their conclusions as follows:
This study adds no valuable information on the effects of Neurodoron® in self-medication. The results from this NIS showed what utter nonsense the Weleda marketing team is capable of producing in an attempt to boost sales.
PS
These declarations of the 4 study authors and the sponsorship are revealing, I thought:
RH and CS are employees of Weleda AG, Germany. JH and KS work for daacro GmbH & Co. KG, a clinical research organization, Germany. The authors declare that there are no conflicts of interest.
This study was financed by the pharmaceutical company Weleda AG, Arlesheim, the employer of RH and CS. Weleda commissioned the CRO daacro for their contribution to the manuscript.
Bioresonance is an alternative therapeutic and diagnostic method employing a device developed in Germany by Scientology member Franz Morell in 1977. The bioresonance machine was further developed and marketed by Morell’s son-in-law Erich Rasche and is also known as ‘MORA’ therapy (MOrell + RAsche). Bioresonance is based on the notion that one can diagnose and treat illness with electromagnetic waves and that, via resonance, such waves can influence disease on a cellular level.
On this blog, we have discussed the idiocy bioresonance several times (for instance, here and here). My favorite study of bioresonance is the one where German investigators showed that the device cannot even differentiate between living and non-living materials. Despite the lack of plausibility and proof of efficacy, research into bioresonance continues.
The aim of this study was to evaluate if bioresonance therapy can offer quantifiable results in patients with recurrent major depressive disorder and with mild, moderate, or severe depressive episodes.
The study included 140 patients suffering from depression, divided into three groups.
- The first group (40 patients) received solely bioresonance therapy.
- The second group (40 patients) received pharmacological treatment with antidepressants combined with bioresonance therapy.
- The third group (60 patients) received solely pharmacological treatment with antidepressants.
The assessment of depression was made using the Hamilton Depression Rating Scale, with 17 items, at the beginning of the bioresonance treatment and the end of the five weeks of treatment.
The results showed a statistically significant difference for the treatment methods applied to the analyzed groups (p=0.0001). The authors also found that the therapy accelerates the healing process in patients with depressive disorders. Improvement was observed for the analyzed groups, with a decrease of the mean values between the initial and final phase of the level of depression, of delta for Hamilton score of 3.1, 3.8 and 2.3, respectively.
The authors concluded that the bioresonance therapy could be useful in the treatment of recurrent major depressive disorder with moderate depressive episodes independently or as a complementary therapy to antidepressants.
One could almost think that this is a reasonably sound study. But why did it generate such a surprising result?
When reading the full paper, the first thing one notices is that it is poorly presented and badly written. Thus there is much confusion and little clarity. The questions keep coming until one comes across this unexpected remark: the study was a retrospective study…
This explains some of the confusion and it certainly explains the surprising results. It remains unclear how the patients were selected/recruited but it is obvious that the groups were not comparable in several ways. It also becomes very clear that with the methodology used, one can make any nonsense look effective.
In the end, I am left with the impression that mutton is being presented as lamb, even worse: I think someone here is misleading us by trying to convince us that an utterly bogus therapy is effective. In my view, this study is as clear an example of scientific misconduct as I have seen for a long time.



