anxiety
There are many patients in general practice with health complaints that cannot be medically explained. Some of these patients attribute their problems to dental amalgam.
This study examined the cost-effectiveness of the removal of amalgam fillings in patients with medically unexplained physical symptoms (MUPS) attributed to amalgam compared to usual care, based on a prospective cohort study in Norway.
Costs were determined using a micro-costing approach at the individual level. Health outcomes were documented at baseline and approximately two years later for both the intervention and the usual care using EQ-5D-5L. Quality-adjusted life year (QALY) was used as the main outcome measure. A decision analytical model was developed to estimate the incremental cost-effectiveness of the intervention. Both probabilistic and one-way sensitivity analyses were conducted to assess the impact of uncertainty on costs and effectiveness.
In patients who attributed health complaints to dental amalgam and fulfilled the inclusion and exclusion criteria, amalgam removal was associated with a modest increase in costs at the societal level as well as improved health outcomes. In the base-case analysis, the mean incremental cost per patient in the amalgam group was NOK 19 416 compared to the MUPS group, while the mean incremental QALY was 0.119 with a time horizon of two years. Thus, the incremental costs per QALY of the intervention were NOK 162 680, which is usually considered to be cost-effective in Norway. The estimated incremental cost per QALY decreased with increasing time horizons, and amalgam removal was found to be cost-saving over both 5 and 10 years.
The authors concluded that this study provides insight into the costs and health outcomes associated with the removal of amalgam restorations in patients who attribute health complaints to dental amalgam fillings, which are appropriate instruments to inform health care priorities.
The group sizes were 32 and 28 respectively. This study was thus almost laughably small and therefore cannot lead to firm conclusions of any type. In this contest, a recent systematic review might be relevant; it concluded as follows:
On the basis of the available RCTs, amalgam restorations, if compared with resin-based fillings, do not show an increased risk for systemic diseases. There is still insufficient evidence to exclude or demonstrate any direct influence on general health. The removal of old amalgam restorations and their substitution with more modern adhesive restorations should be performed only when clinically necessary and not just for material concerns. In order to better evaluate the safety of dental amalgam compared to other more modern restorative materials, further RCTs that consider important parameters such as long and uniform follow up periods, number of restorations per patient, and sample populations representative of chronic or degenerative diseases are needed.
Similarly, a review of the evidence might be informative:
Since more than 100 years amalgam is successfully used for the functional restoration of decayed teeth. During the early 1990s the use of amalgam has been discredited by a not very objective discussion about small amounts of quicksilver that can evaporate from the material. Recent studies and reviews, however, found little to no correlation between systemic or local diseases and amalgam restorations in man. Allergic reactions are extremely rare. Most quicksilver evaporates during placement and removal of amalgam restorations. Hence it is not recommended to make extensive rehabilitations with amalgam in pregnant or nursing women. To date, there is no dental material, which can fully substitute amalgam as a restorative material. According to present scientific evidence the use of amalgam is not a health hazard.
Furthermore, there is evidence that the removal of amalgam fillings is not such a good idea. One study, for instance, showed that the mercury released by the physical action of the drill, the replacement material and especially the final destination of the amalgam waste can increase contamination levels that can be a risk for human and environment health.
As dental amalgam removal does not seem risk-free, it is perhaps unwise to remove these fillings at all. Patients who are convinced that their amalgam fillings make them ill might simply benefit from assurance. After all, we also do not re-lay electric cables because some people feel they are the cause of their ill-health.
You haven’t heard of religious/spiritual singing and movement as a treatment for mental health?
Me neither!
But it does exist. This review explored the evidence of religious/spiritual (R/S) singing and R/S movement (dynamic meditation and praise dance), in relation to mental health outcomes.
After registering with PROSPERO (CRD42020189495), a systematic search of three major databases (CINAHL, MEDLINE, and PsycINFO) was undertaken using predetermined eligibility criteria. Reference lists of identified papers and additional sources such as Google Scholar were searched. The quality of studies was assessed using the Mixed Method Appraisal Tool (MMAT). Data were extracted, tabulated, and synthesized according to the Preferred Reporting Items for Systematic Reviews (PRISMA) guidelines.
Seven of the 259 identified articles met inclusion criteria. Three studies considered R/S singing, while four considered R/S movement. In R/S movements, three studies considered dynamic meditation while one investigated praise dance. Although moderate to poor in quality, included studies indicated a positive trend for the effectiveness of R/S singing and movement in dealing with mental health concerns.
The authors concluded that, while R/S singing and R/S movement (praise dance and dynamic meditation) may be of value as mental health strategies, findings of the review need to be considered with caution due to methodological constraints. The limited number and poor quality of included studies highlight the need for further quality research in these R/S practices in mental health.
I am glad the authors caution us not to take their findings seriously. To be honest, I was not in danger of making this mistake. Neither do I feel the need for further research in this area. Mental health is a serious issue, and personally, I think we should research it not by conducting ridiculous studies of implausible modalities.
PS
I do not doubt that the experience of singing or movement can help in certain situations. However, I have my doubts about religious/spiritual singing and movement therapy.
The present study investigated the impact of a purposefully designed Islamic religion-based intervention on reducing depression and anxiety disorders among Muslim patients using a randomised controlled trial design. A total of 62 Muslim patients (30 women and 32 men) were divided by gender into two groups, with each group assigned randomly to either treatment or control groups. The participants who received the Islamic-based intervention were compared to participants who received the control intervention.
The Islamic-Based Intervention that was applied to the two experimental groups (i.e. one male, one female) has several components. These components were based on moral and religious concepts and methods, including moral confession, repentance, insight, learning, supplication, seeking Allah’s mercy, seeking forgiveness, remembrance of Allah, patience, trust in Allah, self-consciousness, piety, spiritual values, and moral principles. The techniques implemented in the intervention included the art of asking questions, clarifying, listening, interacting, summarising, persuading, feedback, empathy, training practice, reflecting feelings, discussion, and dialogue, lecturing, brainstorming, reinforcement, modeling, positive self-talk, evaluation, homework, practical applications, activation games (play through activities), emotional venting, stories, presentation, correction of thoughts, and relaxation. The two control groups (i.e. one male, one female) received the energy path program provided by the Al-Nour Centre. This program aimed to enhance self-confidence and modify people’s behavior with anxiety disorders, depression, and obsessive-compulsive disorder. Both interventions comprised 30 sessions over 30 h; two sessions were conducted per week, and each session lasted for 60 min (one hour). The duration of the intervention was 15 weeks.
Taylor’s manifest anxiety scale and Steer and Beck’s depression scale were used for examining the effects on depression and anxiety levels. The results revealed that the Islamic intervention significantly reduced anxiety levels in women and depression levels in men compared to the typical care control groups.
The authors concluded that religious intervention played a vital role in lowering the patients’ level of anxiety among women and depression among men. In general, religious practices prevent individuals from becoming subject to mental disorders, i.e. anxiety and depression.
The authors comment that the Islamic religion-based intervention (RSAFI) significantly reduced the levels of depression and anxiety among the participants. Also, there was a substantial improvement in the patients’ general health after the intervention. They were satisfied and believed that everything happening to them was destined by Allah. These results could be attributed to the different intervention practices that relied on the guidance of the Holy Quran and Sunnah. For instance, Saged et al. (2020) confirmed that the Holy Quran significantly impacts healing patients who suffer from physical, psychological, and mental disorders. In this respect, Moodley et al. (2018) concluded that having faith in Allah offers a relatively quick approach to healing patients suffering from heartache and depression. This goes hand in hand because the recitation of the Quran and remembrance of Allah help patients feel relaxed and peaceful. Muslims believe that the Quran is the word of Allah and that Allah’s words exert a significant impact on the healing of mental health patients, as, ultimately, Almighty Allah is the one who cures illnesses.
When discussing the limitations of their study, the authors state that the sample of this study was limited to the patients with anxiety and depression disorders at the Al-Nour Centre in Kuala Lumpur, so the results cannot be generalized to other samples. Furthermore, the treatment of anxiety was restricted to females, whereas the treatment of depression was restricted to males. Additionally, the selection of females and males as samples for the study was based on their pre-measurement of anxiety and depression, which serve as self-report measures.
The authors seem to be unconcerned about the fact that the 2 interventions (verum and control) were clearly distinguishable and their patients thus were not blinded (and neither were the evaluators). This obviously means that the observed effect might have nothing at all to do with the Islamic-Based Intervention but could be entirely due to expectation and persuasion.
Why might the authors not even bother to discuss such an obvious possibility?
A look at their affiliations might provide the answer:
- 1Academy of Islamic Studies, University of Malaya, 50603, Kuala Lumpur, Malaysia. [email protected].
- 2Academy of Islamic Studies, University of Malaya, 50603, Kuala Lumpur, Malaysia.
- 3Faculty of Education, Universiti Teknologi Malaysia, Johor, Malaysia.
- 4Faculty of Education, University of Malaya, 50603, Kuala Lumpur, Malaysia.
- 5Islamic Banking and Finance, International Islamic University Malaysia, Selangor, Malaysia.
- 6Department of Hadith and Associated Sciences, Nourah Bint Abdulrahman University, Riyadh, Saudi Arabia.
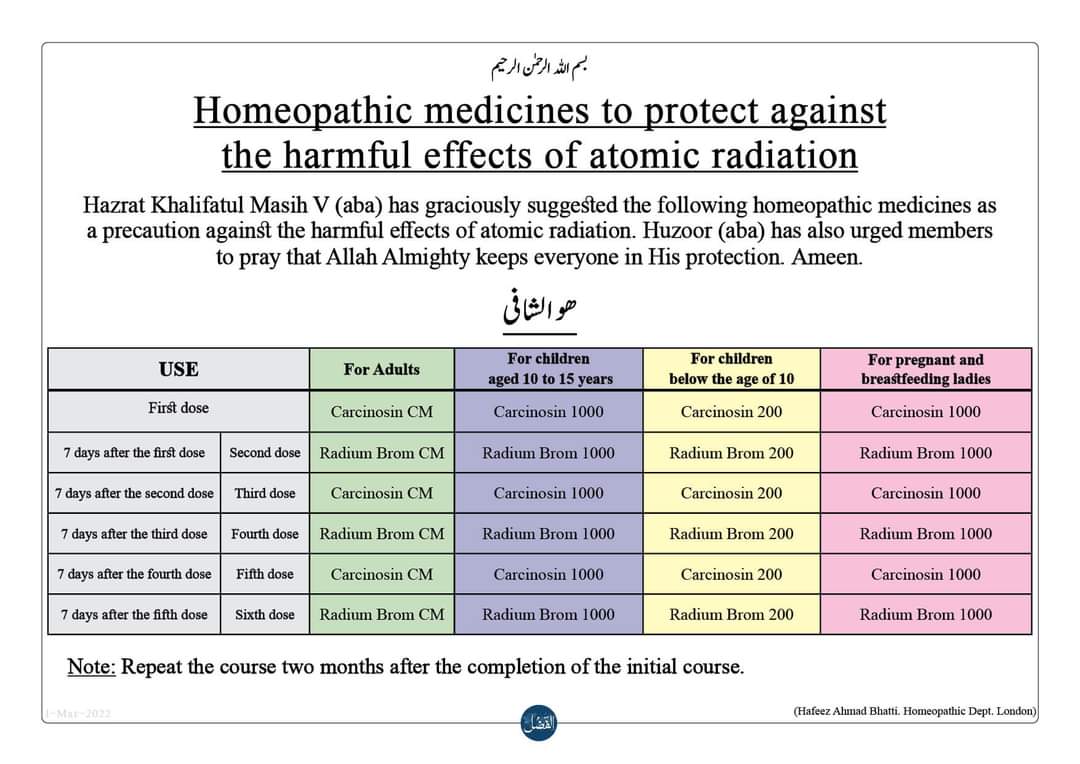
Yes, the fear of nuclear radiation has gripped the minds of many consumers. And who would blame them? We are all frightened of Putin’s next move. There is plenty of uncertainty. But, let me assure you, there is one certainty:
Homeopathy does not help against the effects of nuclear radiation.
But this indisputable fact has never stopped a homeopath.
Many of them are currently trying to persuade us that homeopathy can protect us. Here, for example, is something I found on Twitter:
But there is more, much more. If you go on the Internet, you find dozens of websites making wild claims. Here is just one example:
Homeopathic remedies as a preventive for adults
To be taken on an annual or bi-annual basis:
Week 1: Carcinosin in CM potency
Week 2: Radium Bromide in CM potency
Week 3: Carcinosin in CM potency
Week 4: Radium Bromide in CM potency
Week 5: Carcinosin in CM potency
Week 6: Radium Bromide in CM potency
Homeopathic remedies as a preventive for children (13 years old)
100
To be taken on an annual or bi-annual basis:
Week 1: Carcinosin in 1000 potency
Week 2: Radium Bromide in 1000 potency
Week 3: Carcinosin in 1000 potency
Week 4: Radium Bromide in 1000 potency
Week 5: Carcinosin in 1000 potency
Week 6: Radium Bromide in 1000 potency.
___________________________
Ridiculous? YES
Irresponsible? YES
Dangerous? YES
It’s high time to stop this nonsense!
Stress is associated with a multitude of physical and psychological health impairments. To tackle these health disorders, over-the-counter (OTC) products like Neurodoron® are popular since they are considered safe and tolerable. One tablet of this anthroposophic remedy contains the following active ingredients:
- 83.3 mg Aurum metallicum praeparatum trituration (trit.) D10,
- 83.3 mg Kalium phosphoricicum trit. D6,
- 8.3 mg Ferrum-Quarz trit. D2.
Experience reports and first studies indicate that Neurodoron® is efficient in the treatment of stress-associated health symptoms. “To confirm this” (!!!), a non-interventional study (NIS) with pharmacies was conducted.
The NIS was planned to enroll female and male patients who suffered from nervous exhaustion with symptoms caused by acute and/or chronic stress. The main outcome measures were characteristic stress symptoms, stress burden, and perceived stress. Further outcome measures included perceived efficacy and tolerability of the product as assessed by the patients and collection of adverse drug reactions (ADRs). A study duration of about 21 days with a recommended daily dose of 3–4 tablets was set.
In total, 279 patients were enrolled at 74 German pharmacies. The analyzed set (AS) included 272 patients (mean age 44.8 ± 14.4 years, 73.9% female). 175 patients of the AS completed the NIS. During the study, all stress symptoms declined significantly (total score 18.1 vs. 12.1 (of max. 39 points), < 0.0001). Furthermore, a reduction of stress burden (relative difference in stress burden, VAS = −29.1%, < 0.0001) was observed. For most patients, perceived stress was reduced at the study end (PSQ total score decreased in 70.9% of the patients). 75.9% of the study population rated the product efficacy as “good” or “very good” and 96.6% rated its tolerability as “good” or “very good.” One uncritical ADR was reported.
The authors concluded that this study adds information on the beneficial effects of Neurodoron® in self-medication. The results from this NIS showed a marked reduction in stress burden and perceived stress, along with an excellent safety profile of the medicinal product (MP) Neurodoron®. Further trials are required to confirm these results.
I beg to differ!
The study had no control group and therefore one cannot possibly attribute any of the observed changes to the anthroposophic remedy. They are more likely to be due to:
- the natural history of the condition,
- regression towards the mean,
- a placebo effects,
- other treatments administered during the trial period.
Sadly, the authors discuss none of these possibilities in their paper.
In view of this, I am tempted to rephrase their conclusions as follows:
This study adds no valuable information on the effects of Neurodoron® in self-medication. The results from this NIS showed what utter nonsense the Weleda marketing team is capable of producing in an attempt to boost sales.
PS
These declarations of the 4 study authors and the sponsorship are revealing, I thought:
RH and CS are employees of Weleda AG, Germany. JH and KS work for daacro GmbH & Co. KG, a clinical research organization, Germany. The authors declare that there are no conflicts of interest.
This study was financed by the pharmaceutical company Weleda AG, Arlesheim, the employer of RH and CS. Weleda commissioned the CRO daacro for their contribution to the manuscript.
Bioresonance is an alternative therapeutic and diagnostic method employing a device developed in Germany by Scientology member Franz Morell in 1977. The bioresonance machine was further developed and marketed by Morell’s son-in-law Erich Rasche and is also known as ‘MORA’ therapy (MOrell + RAsche). Bioresonance is based on the notion that one can diagnose and treat illness with electromagnetic waves and that, via resonance, such waves can influence disease on a cellular level.
On this blog, we have discussed the idiocy bioresonance several times (for instance, here and here). My favorite study of bioresonance is the one where German investigators showed that the device cannot even differentiate between living and non-living materials. Despite the lack of plausibility and proof of efficacy, research into bioresonance continues.
The aim of this study was to evaluate if bioresonance therapy can offer quantifiable results in patients with recurrent major depressive disorder and with mild, moderate, or severe depressive episodes.
The study included 140 patients suffering from depression, divided into three groups.
- The first group (40 patients) received solely bioresonance therapy.
- The second group (40 patients) received pharmacological treatment with antidepressants combined with bioresonance therapy.
- The third group (60 patients) received solely pharmacological treatment with antidepressants.
The assessment of depression was made using the Hamilton Depression Rating Scale, with 17 items, at the beginning of the bioresonance treatment and the end of the five weeks of treatment.
The results showed a statistically significant difference for the treatment methods applied to the analyzed groups (p=0.0001). The authors also found that the therapy accelerates the healing process in patients with depressive disorders. Improvement was observed for the analyzed groups, with a decrease of the mean values between the initial and final phase of the level of depression, of delta for Hamilton score of 3.1, 3.8 and 2.3, respectively.
The authors concluded that the bioresonance therapy could be useful in the treatment of recurrent major depressive disorder with moderate depressive episodes independently or as a complementary therapy to antidepressants.
One could almost think that this is a reasonably sound study. But why did it generate such a surprising result?
When reading the full paper, the first thing one notices is that it is poorly presented and badly written. Thus there is much confusion and little clarity. The questions keep coming until one comes across this unexpected remark: the study was a retrospective study…
This explains some of the confusion and it certainly explains the surprising results. It remains unclear how the patients were selected/recruited but it is obvious that the groups were not comparable in several ways. It also becomes very clear that with the methodology used, one can make any nonsense look effective.
In the end, I am left with the impression that mutton is being presented as lamb, even worse: I think someone here is misleading us by trying to convince us that an utterly bogus therapy is effective. In my view, this study is as clear an example of scientific misconduct as I have seen for a long time.
This systematic review examined the efficacy of acupressure on depression. Literature searches were performed on PubMed, PsycINFO, Scopus, Embase, MEDLINE, and China National Knowledge (CNKI). Randomized clinical trials (RCTs) or single-group trials in which acupressure was compared with various control methods or baseline (i.e. no treatment) in people with depression were included. Data were synthesized using a random-effects or a fixed-effects model to analyze the impacts of acupressure treatment on depression and anxiety in people with depression. The primary outcome measures were depression symptoms quantified by various means. Subgroups were created, and meta-regression analyses were performed to explore which factors are relevant to the greater or lesser effects of treating symptoms. 
A total of 14 RCTs (1439 participants) were identified. Analysis of the between-group showed that acupressure was effective in reducing depression [Standardized mean differences (SMDs) = -0.58, 95%CI: -0.85 to -0.32, P < 0.0001] and anxiety (SMD = -0.67, 95%CI: -0.99 to -0.36, P < 0.0001) in participants with mild-to-moderate primary and secondary depression. Subgroup analyses suggested that acupressure significantly reduced depressive symptoms compared with different controlled conditions and in participants with different ages, clinical conditions, and duration of intervention. Adverse events, including hypotension, dizziness, palpitation, and headache, were reported in only one study.
The authors concluded that the evidence of acupressure for mild-to-moderate depressive symptoms was significant. Importantly, the findings should be interpreted with caution due to study limitations. Future research with a well-designed mixed method is required to consolidate the conclusion and provide an in-depth understanding of potential mechanisms underlying the effects.
I think that more than caution is warranted when interpreting these data. In fact, it would have been surprising if the meta-analyses had NOT generated an overall positive result. This is because in several studies there was no attempt to control for the extra attention or the placebo effect of administering acupressure. In most of the trials where this had been taken care of (i.e. patient-blinded, sham-controlled studies), there were no checks for the success of blinding. Thus it is possible, even likely that many patients correctly guessed what treatment they received. In turn, this means that the outcomes of these trials were also largely due to placebo effects.
Overall, this paper is therefore a prime example of a biased review of biased primary studies. The phenomenon can be aptly described by the slogan:
RUBBISH IN, RUBBISH OUT!
Recently, there has been a flurry of research interest in mindfulness – one could almost call it hype! Not that this is reflected in loads of rigorous trials, rather it manifests itself by an unprecedented amount of systematic reviews on mindfulness being published.
I conducted a Medline search on 8/2/2022 for meta-analyses of mindfulness. It resulted in no less than 9 such papers. Here are their conclusions:
- This meta-analysis suggests that SOF is a moderately effective evidence-based practice for reducing disruptive behavior.
- In conclusion, both mindfulness interventions showed robust evidence on anxiety symptoms in pretest-posttest periods compared to control groups. Few studies and lack of evidence of follow-up periods were the main limitations found.
- Memory specificity did not significantly differ from baseline to post-treatment for either MBCT and Control interventions.
- Although this review was limited by search strategies and most of the included studies were of low quality, it still provided some tentative support for PSIs for the treatment of TOPFA women.
- Meta-regression results showed that some heterogeneity in effect size could be accounted for by intervention dosage, study population, and study design. Our findings quantify MBIs’ potential for improving immune function and thus impacting somatic disorders.
- Mindfulness interventions somewhat improved depression in emerging adults. Because primary researchers did not report the adverse effects, mindfulness interventions should be used with caution. Future researchers might study the adverse effects of mindfulness interventions as well as the long-term effects.
- The effect of MBIs on pain in cancer patients was demonstrated in our analysis, albeit with small effect sizes. High-quality RCTs are needed to verify the efficacy of MBIs on cancer patients or survivors with pain complaints. Future trials should take into account the specific pain outcome measures (pain intensity or pain interference), the approach of intervention provision (clinic-based or remote MBI, group or individual practice), the duration and frequency of interventions and the comparators (passive or active control arms).
- This meta-analysis found that MBIs had beneficial effects on mental health such as psychological distress and wellbeing in nurses.
- Because MBIs show promise across some PICOS, future RCTs and meta-analyses should build on identified strengths and limitations of this literature.
This amounts to about two systematic reviews/meta-analyses per week!
And what do these papers tell us?
If you are an advocate of mindfulness, you probably conclude that your pet therapy is supported by reasonably sound evidence. If, however, you think a little more critically, you would probably see that the evidence is far from strong. The effect size is usually small and of doubtful clinical relevance. This is, I think, important because clinical trials of mindfulness cannot easily control for placebo effects (there is no adequate placebo that would allow patients to be blinded). Therefore, the small effects that do emerge in systematic reviews/meta-analyses are most likely the result of a placebo response and not due to mindfulness per se.
My conclusion is therefore not nearly as positive as that of fans of mindfulness: the collective evidence suggests to me that the success of mindfulness relies mostly or even entirely on the placebo effect. And this means that even dozens of further systematic reviews are not going to advance our knowledge significantly. What is needed, I think, is a few truly rigorous studies aimed at determining whether the effects of mindfulness are specific or non-specific in nature. My prediction is that, once we have this evidence, the current hype around mindfulness will calm down.
Bach Flower Remedies are often mistaken for homeopathy. Yet they are quite different. They were invented about 100 years ago by Dr. Edward Bach (1886–1936), a doctor homeopath who had previously worked in the London Homeopathic Hospital. His remedies are clearly inspired by homeopathy; however, they are by no means the same because they do not follow the ‘like cures like’ principle and neither are they potentised. They are manufactured by placing freshly picked specific flowers or parts of plants in water which is subsequently mixed with alcohol, bottled, and sold. Like most homeopathic remedies, they are highly dilute and thus do not contain therapeutic concentrations of the plant printed on the bottle. In other words, flower remedies (or essences) are placebos. This does not stop enthusiasts to continue submitting them to clinical trials.
This study tested the effects of flower essence bouquets on the signs and symptoms of stress in nursing students. The study was designed as a randomized clinical trial, triple blind, with two groups (flower essence group and placebo group), carried out with 101 nursing students. Bach’s flower essences Cerato (Ceratostigma wilimottianum), Cherry Plum (Prunus cerasifera), Elm (Ulmus procera), Impatients (Impatiens glandulifera), Larch (Larix decidua), Olive (Olea europaea) and White Chestnut (Aesculus hippocastanum) were selected by the researcher based on the experience of attending nursing students on flower essence therapy. The formulas were prepared in a 30 ml amber glass bottle with a perforated cap with a white seal and bulbs, and labeled according to randomization (Group 1 or Group 2). The groups applied the treatments for 60 days at a dosage of 4 drops 4 times a day. The outcome was evaluated using the Baccaro Test and the Perceived Stress Scale applied at the beginning and at the end of the intervention.
The results demonstrated no significant difference between the groups in stress reduction (p > 0.05). Both groups showed a reduction in scale scores (p < 0.001) with a large effect size. There was an influence of the COVID-19 pandemic in the reduction of Baccaro Test scores.
The authors (who seem to have been advocates of Bach Flower Remedies) concluded that the intervention with flower essence therapy was not more effective than placebo in reducing stress signs and symptoms.
Is anyone surprised?
I am not!
Shiatsu is a (mostly) manual therapy that was popularised by Japanese Tokujiro Namikoshi (1905–2000). It developed out of the Chinese massage therapy, ‘tui na’. The word shiatsu means finger pressure in Japanese; however, a range of devices is also being promoted for shiatsu. The evidence that shiatsu is effective for any condition is close to non-existent.
This study aimed to investigate the effect of Shiatsu massage on agitation in mechanically ventilated patients.
A total of 68 mechanically ventilated patients were randomly assigned to two groups. Patients in the intervention group received three 5-minute periods of Shiatsu massage with a 2-minute break between them, while patients in the control group only received a touch on the area considered for the message. Data were collected before and after the intervention using the Richmond Agitation-Sedation Scale (RASS) and then analyzed.
The results showed that the level of agitation significantly decreased in the intervention group compared to the control group (p=.001).
The authors concluded that the application of shiatsu massage seems to be effective in managing agitation in mechanically ventilated patients. Further studies with greater sample size and longer follow-up period are needed to confirm the current findings.
It is good to see that, as far as I know for the first time, an attempt was made to control for placebo and other non-specific effects in a trial of shiatsu. However, in itself, the attempt is not convincing. What we need to know is whether the attempt was successful or not. Were the patients fully blinded and unable to tell the difference between verum and sham? From reading not just the abstract but the full paper, I do not get the impression that patients were successfully blinded. This means that the results might be entirely due to the effect of deblinding.