anxiety
Electroacupuncture (EA) is often advocated for depression and sleep disorders but its efficacy remains uncertain. The aim of this study was, therefore, to “assess the efficacy and safety of EA as an alternative therapy in improving sleep quality and mental state for patients with insomnia and depression.”
A 32-week patient- and assessor-blinded, randomized, sham-controlled clinical trial (8-week intervention plus 24-week follow-up) was conducted from September 1, 2016, to July 30, 2019, at 3 tertiary hospitals in Shanghai, China. Patients were randomized to receive
- EA treatment and standard care,
- sham acupuncture (SA) treatment and standard care,
- standard care only as control.
Patients in the EA or SA groups received a 30-minute treatment 3 times per week (usually every other day except Sunday) for 8 consecutive weeks. All treatments were performed by licensed acupuncturists with at least 5 years of clinical experience. A total of 6 acupuncturists (2 at each center; including X.Y. and S.Z.) performed EA and SA, and they received standardized training on the intervention method before the trial. The regular acupuncture method was applied at the Baihui (GV20), Shenting (GV24), Yintang (GV29), Anmian (EX-HN22), Shenmen (HT7), Neiguan (PC6), and SanYinjiao (SP6) acupuncture points, with 0.25 × 25-mm and 0.30 × 40-mm real needles (Wuxi Jiajian Medical Device Co, Ltd), or 0.30 × 30-mm sham needles (Streitberger sham device [Asia-med GmbH]).
For patients in the EA group, rotating or lifting-thrusting manipulation was applied for deqi sensation after needle insertion. The 2 electrodes of the electrostimulator (CMNS6-1 [Wuxi Jiajian Medical Device Co, Ltd]) were connected to the needles at GV20 and GV29, delivering a continuous wave based on the patient’s tolerance. Patients in the SA group felt a pricking sensation when the blunt needle tip touched the skin, but without needle insertion. All indicators of the nearby electrostimulator were set to 0, with the light switched on. Standard care (also known as treatment as usual or routine care) was used in the control group. Patients receiving standard care were recommended by the researchers to get regular exercise, eat a healthy diet, and manage their stress level during the trial. They were asked to keep the regular administration of antidepressants, sedatives, or hypnotics as well. Psychiatrists in the Shanghai Mental Health Center (including X.L.) guided all patients’ standard care treatment and provided professional advice when a patient’s condition changed.
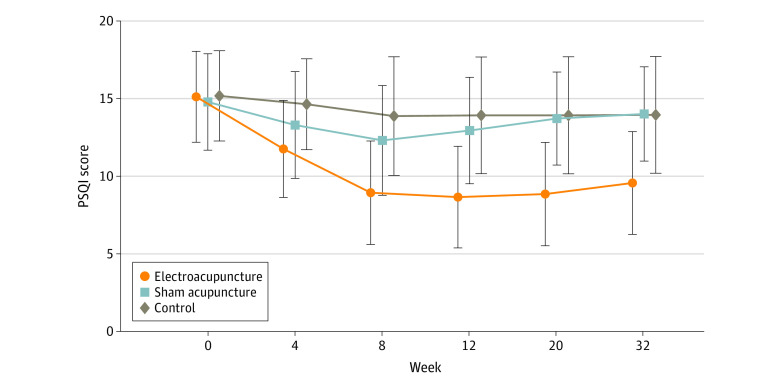
The primary outcome was change in Pittsburgh Sleep Quality Index (PSQI) from baseline to week 8. Secondary outcomes included PSQI at 12, 20, and 32 weeks of follow-up; sleep parameters recorded in actigraphy; Insomnia Severity Index; 17-item Hamilton Depression Rating Scale score; and Self-rating Anxiety Scale score.
Among the 270 patients (194 women [71.9%] and 76 men [28.1%]; mean [SD] age, 50.3 [14.2] years) included in the intention-to-treat analysis, 247 (91.5%) completed all outcome measurements at week 32, and 23 (8.5%) dropped out of the trial. The mean difference in PSQI from baseline to week 8 within the EA group was -6.2 (95% CI, -6.9 to -5.6). At week 8, the difference in PSQI score was -3.6 (95% CI, -4.4 to -2.8; P < .001) between the EA and SA groups and -5.1 (95% CI, -6.0 to -4.2; P < .001) between the EA and control groups. The efficacy of EA in treating insomnia was sustained during the 24-week postintervention follow-up. Significant improvement in the 17-item Hamilton Depression Rating Scale (-10.7 [95% CI, -11.8 to -9.7]), Insomnia Severity Index (-7.6 [95% CI, -8.5 to -6.7]), and Self-rating Anxiety Scale (-2.9 [95% CI, -4.1 to -1.7]) scores and the total sleep time recorded in the actigraphy (29.1 [95% CI, 21.5-36.7] minutes) was observed in the EA group during the 8-week intervention period (P < .001 for all). No between-group differences were found in the frequency of sleep awakenings. No serious adverse events were reported.
The result of the blinding assessment showed that 56 patients (62.2%) in the SA group guessed wrongly about their group assignment (Bang blinding index, −0.4 [95% CI, −0.6 to −0.3]), whereas 15 (16.7%) in the EA group also guessed wrongly (Bang blinding index, 0.5 [95% CI, 0.4-0.7]). This indicated a relatively higher degree of blinding in the SA group.
The authors concluded that, in this randomized clinical trial of EA treatment for insomnia in patients with depression, quality of sleep improved significantly in the EA group compared with the SA or control group at week 8 and was sustained at week 32.
This trial seems rigorous, it has a sizable sample size, uses a credible placebo procedure, and is reported in sufficient detail. Why then am I skeptical?
- Perhaps because we have often discussed how untrustworthy acupuncture studies from China are?
- Perhaps because I fail to see a plausible mechanism of action?
- Perhaps because the acupuncturists could not be blinded and thus might have influenced the outcome?
- Perhaps because the effects of sham acupuncture seem unreasonably small?
- Perhaps because I cannot be sure whether the acupuncture or the electrical current is supposed to have caused the effects?
- Perhaps because the authors of the study are from institutions such as the Shanghai Municipal Hospital of Traditional Chinese Medicine, the Department of Acupuncture and Moxibustion, Huadong Hospital, Fudan University, Shanghai,
- Perhaps because the results seem too good to be true?
If you have other and better reasons, I’d be most interested to hear them.
I was fascinated to find a chiropractor who proudly listed ‘the most common conditions chiropractors help kids with‘:
- Vision problems
- Skin conditions
- Bedwetting
- Sinus problems
- ADD/ADHD
- Stomachaches
- Asthma
- Allergies
- Loss of hearing
- Ear Infections
- Hip, leg, or foot pain
- Constipation
- Poor coordination
- Breastfeeding difficulties
- Arm, hand, or shoulder pain
- Anxiety and nervousness
- Colic
- Scoliosis
The birth process, even under normal conditions, is frequently the first cause of spinal stress. After the head of the child appears, the physician grabs the baby’s head and twists it around in a figure eight motion, lifting it up to receive the lower shoulder and then down to receive the upper shoulder. This creates significant stress on the spine of the baby.
“Spinal cord and brain stem traumas often occur during the process of birth but frequently escape diagnosis. Infants often experience lasting neurological defects. Spinal trauma at birth is essentially attributed to longitudinal traction, especially when this force is combined with flexion and torsion of the spinal axis during delivery.” ~Abraham Towbin, MD
Growth patterns suggest the potential for neurological disorders is most critical from birth to two years of age, as this time is the most dynamic and important phase of postnatal brain development. Over sixty percent of all neurological development occurs after birth in the child’s first year of life. This is why it is so important to bring your child to a local pediatric chiropractor to have them checked and for your child to get a chiropractic adjustment during the first year of their life. Lee Hadley MD states “Subluxation alone is a rational reason for Pediatric Chiropractic care throughout a lifetime from birth.”
As our children continue to grow, the daily stresses can have a negative impact on an ever growing body. During the first few years of life, an infant often falls while learning to walk or can fall while tumbling off a bed or other piece of furniture. Even the seemingly innocent act of playfully tossing babies up in the air and catching them often results in a whiplash-like trauma to the spine, making it essential to get your baby checked by a pediatric chiropractor every stage of his/her development as minor injuries can present as major health concerns down the road if gone uncorrected.
______________________________
On the Internet, similar texts can be found by the hundreds. I am sure that many new parents are sufficiently impressed by them to take their kids to a chiropractor. I have yet to hear of a single case where the chiropractor then checked out the child and concluded: “there is nothing wrong; your baby does not need any therapy.” Chiropractors always find something – not something truly pathological, but something to mislead the parent and to earn some money.
Often the treatment that follows turns out to be a prolonged and thus expensive series of sessions that almost invariably involve manipulating the infant’s fragile and developing spine. There is no compelling evidence that this approach is effective for anything. In addition, there is evidence that it can do harm, sometimes even serious harm.
And that’s the reason why I have mentioned this topic before and intend to continue doing so in the future:
- There is hardly a good reason for adults to consult a chiropractor.
- There is no reason to take a child to a chiropractor.
- There are good reasons for chiropractors to stop treating children.
But let’s be a bit more specific. Let’s deal with the above list of indications on the basis of the reliable evidence:
- Vision problems – no sound evidence that chiropractic manipulations are effective.
- Skin conditions – no sound evidence that chiropractic manipulations are effective.
- Bedwetting – some evidence that chiropractic manipulations are ineffective.
- Sinus problems – no sound evidence that chiropractic manipulations are effective.
- ADD/ADHD – some evidence that chiropractic manipulations are ineffective.
- Stomachaches – no sound evidence that chiropractic manipulations are effective.
- Asthma – some evidence that chiropractic manipulations are ineffective.
- Allergies – no sound evidence that chiropractic manipulations are effective.
- Loss of hearing – no sound evidence that chiropractic manipulations are effective.
- Ear Infections – some evidence that chiropractic manipulations are ineffective.
- Hip, leg, or foot pain – no sound evidence that chiropractic manipulations are effective.
- Constipation – no sound evidence that chiropractic manipulations are effective.
- Poor coordination – no sound evidence that chiropractic manipulations are effective.
- Breastfeeding difficulties – no good evidence that chiropractic manipulations are effective.
- Arm, hand, or shoulder pain – no sound evidence that chiropractic manipulations are effective.
- Anxiety and nervousness – no sound evidence that chiropractic manipulations are effective.
- Colic – some evidence that chiropractic manipulations are ineffective.
- Scoliosis – no sound evidence that chiropractic manipulations are effective.
I rest my case.
This study aimed to evaluate the number of craniosacral therapy sessions that can be helpful to obtain a resolution of the symptoms of infantile colic and to observe if there are any differences in the evolution obtained by the groups that received a different number of Craniosacral Therapy sessions at 24 days of treatment, compared with the control group which did not received any treatment.
Fifty-eight infants with colic were randomized into two groups:
- 29 babies in the control group received no treatment;
- babies in the experimental group received 1-3 sessions of craniosacral therapy (CST) until symptoms were resolved.
Evaluations were performed until day 24 of the study. Crying hours served as the primary outcome measure. The secondary outcome measures were the hours of sleep and the severity, measured by an Infantile Colic Severity Questionnaire (ICSQ).
Statistically significant differences were observed in favor of the experimental group compared to the control group on day 24 in all outcome measures:
- crying hours (mean difference = 2.94, at 95 %CI = 2.30-3.58; p < 0.001);
- hours of sleep (mean difference = 2.80; at 95 %CI = – 3.85 to – 1.73; p < 0.001);
- colic severity (mean difference = 17.24; at 95 %CI = 14.42-20.05; p < 0.001).
Also, the differences between the groups ≤ 2 CST sessions (n = 19), 3 CST sessions (n = 10), and control (n = 25) were statistically significant on day 24 of the treatment for crying, sleep and colic severity outcomes (p < 0.001).
The authors concluded that babies with infantile colic may obtain a complete resolution of symptoms on day 24 by receiving 2 or 3 CST sessions compared to the control group, which did not receive any treatment.
Why do SCAM researchers so often have no problem leaving the control group of patients in clinical trials without any treatment at all, while shying away from administering a placebo? Is it because they enjoy being the laughingstock of the science community? Probably not.
I suspect the reason might be that often they know that their treatments are placebos and that their trials would otherwise generate negative findings. Whatever the reasons, this new study demonstrates three things many of us already knew:
- Colic in babies always resolves on its own but can be helped by a placebo response (e.g. via the non-blinded parents), by holding the infant, and by paying attention to the child.
- Flawed trials lend themselves to drawing the wrong conclusions.
- Craniosacral therapy is not biologically plausible and most likely not effective beyond placebo.
Bioenergy (or energy healing) therapies are among the popular alternative treatment options for many diseases, including cancer. Many studies deal with the advantages and disadvantages of bioenergy therapies as an addition to established treatments such as chemotherapy, surgery, and radiation in the treatment of cancer. However, a systematic overview of this evidence is thus far lacking. For this reason, German authors reviewed and critically examined the evidence to determine what benefits the treatments have for patients.
In June 2022, a systematic search was conducted searching five electronic databases (Embase, Cochrane, PsychInfo, CINAHL and Medline) to find studies concerning the use, effectiveness, and potential harm of bioenergy therapies including the following modalities:
- Reiki,
- Therapeutic Touch,
- Healing Touch,
- Polarity Therapy.
From all 2477 search results, 21 publications with a total of 1375 patients were included in this systematic review. The patients treated with bioenergy therapies were mainly diagnosed with breast cancer. The main outcomes measured were:
- anxiety,
- depression,
- mood,
- fatigue,
- quality of life (QoL),
- comfort,
- well-being,
- neurotoxicity,
- pain,
- nausea.
The studies were predominantly of moderate quality and, for the most part, found no effect. In terms of QoL, pain, and nausea, there were some positive short-term effects of the interventions, but no long-term differences were detectable. The risk of side effects from bioenergy therapies appears to be relatively small.
The authors concluded that considering the methodical limitations of the included studies, studies with high study quality could not find any difference between bioenergy therapies and active (placebo, massage, RRT, yoga, meditation, relaxation training, companionship, friendly visit) and passive control groups (usual care, resting, education). Only studies with a low study quality were able to show significant effects.
Energy healing is as popular as it is implausible. What these ‘healers’ call ‘energy’ is not how it is defined in physics. It is an undefined, imagined entity that exists only in the imagination of its proponents. So why should it have an effect on cancer or any other condition?
My team conducted 2 RCT of energy healing (pain and warts); both failed to show positive effects. And here is what I stated in my recent book about energy healing for any ailment:
Energy healing is an umbrella term for a range of paranormal healing practices. Their common denominator is the belief in a mystical ‘energy’ that can be used for therapeutic purposes.
- Forms of energy healing have existed in many ancient cultures. The ‘New Age’ movement has brought about a revival of these ideas, and today energy healing systems are amongst the most popular alternative therapies in the US as well as in many other countries. Popular forms of energy healing include those listed above. Each of these are discussed and referenced in separate chapters of this book.
- Energy healing relies on the esoteric belief in some form of ‘energy’ which is distinct from the concept of energy understood in physics and refers to some life force such as chi in Traditional Chinese Medicine, or prana in Ayurvedic medicine.
- Some proponents employ terminology from quantum physics and other ‘cutting-edge’ science to give their treatments a scientific flair which, upon closer scrutiny, turns out to be but a veneer of pseudo-science.
- The ‘energy’ that energy healers refer to is not measurable and lacks biological plausibility.
- Considering its implausibility, energy healing has attracted a surprisingly high level of research activity. Its findings are discussed in the respective chapters of each of the specific forms of energy healing.
- Generally speaking, the methodologically best trials of energy healing fail to demonstrate that it generates effects beyond placebo.
- Even though energy healing is per se harmless, it can do untold damage, not least because it significantly undermines rational thought in our societies.
As you can see, I do not entirely agree with my German friends on the issue of harm. I think energy healing is potentially dangerous and should be discouraged.
One should never assume that one has seen everything so-called alternative medicine (SCAM) has to offer. New interventions pop up all the time. The ingenuity of the SCAM entrepreneur is limitless. Here is a particularly audacious innovation:
Aura sprays deliver healing gemstone energies to your body, emotions, memory, and mind via your aura.
They give you:
- Instant relief from negative, harmful, or unwanted energies.
- Support that you cannot get from herbs and medicines.
- Deep nourishment to help you overcome weakness and depletion.
And you can choose from an entire range: 
7-Color-Ray Diamond Spray $34.95 – $89.95
Energy Clearing Spray $24.95 – $59.95
Electromagnetic Radiation EMR Clearing $24.95 – $59.95
Sparkler Diamond Spray $34.95
I was particularly fascinated by the EMR spray and found further relevant information about it:
Electromagnetic radiation (EMR) floods our environment and is potentially harmful. GEMFormulas’ EMR Clearing spray clears this energetic toxin from the body and teaches it to become immune. This is essential if we are to thrive in a modern world.
Use this spray to help clear your body and aura of harmful electromagnetic radiation frequencies, which can weaken tissue, inhibit cellular function, and interfere with normal energy flows in the body.
**Harmful electromagnetic radiation is emitted by computers, cell phones, motors, microwave ovens, and other electrical appliances.**
Use When You Are Feeling:
- Weakened in the vicinity of electromagnetic fields.
- Dermatological symptoms such as redness, tingling, and burning sensations.
- Symptoms typical of EHS (Electromagnetic Hypersensitivity) such as fatigue, tiredness, concentration difficulties, dizziness, nausea, heart palpitations, and digestive disturbances.
- A range of non-specific, medically unexplained symptoms.
And When You Want to:
- Become more resilient to the effects of potentially harmful EMR.
- Build immunity to EMR, heal from damage caused by EMR, and protect yourself from further EMR damage.
- Clear harmful EMR residues from your body and aura.
- Maximize your health potential.
Ideal For People Who:
- Work with computers all day long.
- Live near sources of high electromagnetic radiation.
- Suspect they have Electromagnetic Hypersensitivity (EHS).
- Plan to become pregnant.
- Are trying to heal from another affliction.
Additional Benefits: Clear Therapeutic Gemstones and Crystals
You can also use the spray to clear electromagnetic radiation that therapeutic gemstone necklaces naturally accumulate during normal wear in areas of high electromagnetic fields, when stored too close to computers or other electronic devices, and when worn while you are holding a cell phone.
I am tempted!
Not that I plan to become pregnant but I am trying to heal from another affliction: gullibility.
Seriously: how can anyone fall for such nonsense???
But obviously, some people do and pay good money to ruthless con artists (if you look on the Internet, there are dozens of firms offering such quackery).
Even after 30 years of research, so-called alternative medicine (SCAM) has a sheer inexhaustible ability to amaze me.
Cannabis use is a frequently-discussed subject, not just in the realm of so-called alternative medicine (SCAM). In general, SCAM advocates view it as an herbal medicine and recommend it for all sorts of conditions. They also often downplay the risks associated with cannabis use. Yet, these risks might be substantial.
Cannabis potency, defined as the concentration of Δ9-tetrahydrocannabinol (THC), has increased internationally, which could increase the risk of adverse health outcomes for cannabis users. The first systematic review of the association of cannabis potency with mental health and addiction was recently published in ‘The Lancet Psychiatry’.
The authors searched Embase, PsycINFO, and MEDLINE (from database inception to Jan 14, 2021). Included studies were observational studies of human participants comparing the association of high-potency cannabis (products with a higher concentration of THC) and low-potency cannabis (products with a lower concentration of THC), as defined by the studies included, with depression, anxiety, psychosis, or cannabis use disorder (CUD).
Of 4171 articles screened, 20 met the eligibility criteria:
- eight studies focused on psychosis,
- eight on anxiety,
- seven on depression,
- and six on CUD.
Overall, higher potency cannabis, relative to lower potency cannabis, was associated with an increased risk of psychosis and CUD. Evidence varied for depression and anxiety. The association of cannabis potency with CUD and psychosis highlights its relevance in healthcare settings, and for public health guidelines and policies on cannabis sales.
The authors concluded that standardisation of exposure measures and longitudinal designs are needed to strengthen the evidence of this association.
The fact that cannabis use increases the risk of psychosis has long been general knowledge. The notion that the risk increases with increased potency of cannabis seems entirely logical and is further supported by this systematic review. Perhaps it is time to educate the public and make cannabis users more aware of these risks, and perhaps it is time that SCAM proponents negate the harm cannabis can do.
The ‘My Resilience in Adolescence (MYRIAD) Trial’evaluated the effectiveness and cost-effectiveness of SBMT compared with teaching-as-usual (TAU).
MYRIAD was a parallel group, cluster-randomised controlled trial. Eighty-five eligible schools consented and were randomized 1:1 to TAU (43 schools, 4232 students) or SBMT (42 schools, 4144 students), stratified by school size, quality, type, deprivation, and region. Schools and students (mean (SD); age range=12.2 (0.6); 11–14 years) were broadly UK population-representative. Forty-three schools (n=3678 pupils; 86.9%) delivering SBMT, and 41 schools (n=3572; 86.2%) delivering TAU, provided primary end-point data. SBMT comprised 10 lessons of psychoeducation and mindfulness practices. TAU comprised standard social-emotional teaching. Participant-level risk for depression, social-emotional-behavioural functioning and well-being at 1 year follow-up were the co-primary outcomes. Secondary and economic outcomes were included.
 An analysis of the data from 84 schools (n=8376 participants) found no evidence that SBMT was superior to TAU at 1 year. Standardised mean differences (intervention minus control) were: 0.005 (95% CI −0.05 to 0.06) for risk for depression; 0.02 (−0.02 to 0.07) for social-emotional-behavioural functioning; and 0.02 (−0.03 to 0.07) for well-being. SBMT had a high probability of cost-effectiveness (83%) at a willingness-to-pay threshold of £20 000 per quality-adjusted life year. No intervention-related adverse events were observed.
An analysis of the data from 84 schools (n=8376 participants) found no evidence that SBMT was superior to TAU at 1 year. Standardised mean differences (intervention minus control) were: 0.005 (95% CI −0.05 to 0.06) for risk for depression; 0.02 (−0.02 to 0.07) for social-emotional-behavioural functioning; and 0.02 (−0.03 to 0.07) for well-being. SBMT had a high probability of cost-effectiveness (83%) at a willingness-to-pay threshold of £20 000 per quality-adjusted life year. No intervention-related adverse events were observed.
The authors concluded that the findings do not support the superiority of SBMT over TAU in promoting mental health in adolescence.
Even though the results are negative, MYRIAD must be praised for its scale and rigor, and for highlighting the importance of large, well-designed studies before implementing measures of this kind on a population basis. Co-author Tim Dalgliesh, director of the Cambridge Centre for Affective Disorders, said: “For policymakers, it’s not just about coming up with a great intervention to teach young people skills to deal with their stress. You also have to think about where that stress is coming from in the first place.”
“There had been some hope for an easy solution, especially for those who might develop depression,” says Til Wykes, head of the School of Mental Health and Psychological Sciences at the Institute of Psychiatry, Psychology, and Neuroscience, King’s College London. “There may be lots of reasons for developing depression, and these are probably not helped by mindfulness,” she says. “We need more research on other potential factors that might be modified, and perhaps this would provide a more targeted solution to this problem.”
Personally, I feel that mindfulness has been hyped in recent years. Much of the research that seemed to support it was less than rigorous. What is now needed is a realistic approach based on sound evidence and critical thinking.
HISC (HOMEOPATHY IN THE SUSSEX COMMUNITY) was formed in 2011 and has established effective partnerships with organisations that support those in need. Projects include working with domestic and sexual violence charities as well as supporting people recovering from long-term and enduring mental health illness issues. They enable vulnerable and marginalised members of the Sussex community to access low cost treatment with highly experienced homeopaths.
On 22 July, HISC made the following announcement:
Homeopathy in the Sussex Community (HISC) has been awarded a grant from The National Lottery Community Fund to provide homeopathy to survivors of domestic abuse and sexual violence.
HISC works in partnership with Sussex-based organisations; RISE, and Survivors Network, offering long-term and low-cost homeopathic support to women who have experienced abuse and sexual violence.
This grant will fund these projects for the next year, allowing HISC to build on the valuable work already being done and reaching even more vulnerable women who want access to homeopathic support.
Society Fellow Caroline Jurdon and Registered members Michael Bird, Therese Eriksen, Tara Lavelle and Jo Magowan have all worked on the project with colleagues from the wider community. HISC received one of the Society of Homeopath’s Community Clinic awards in 2018.
HISC also offer volunteering and sitting in opportunities for students.
_________________________
The ‘National Lottery Community Fund’ make the following points on their website:
- “Our funding is public money. This means that it cannot be used to give organisations an unlawful advantage.”
- “We fund projects that support people and communities across the UK to thrive.”
I would argue that, for the following reasons, the award is misplaced:
- Public money should not be wasted. It must be invested in projects that have a reasonable chance to do more good than harm.
- A broad consensus exists today that homeopathy has no effect beyond placebo. In fact, the NHS has stopped funding homeopathy and states that “there’s been extensive investigation of the effectiveness of homeopathy. There’s no good-quality evidence that homeopathy is effective as a treatment for any health condition.”
- Homeopathy can endanger lives. If people are misled into believing that it is effective and thus treat serious conditions with homeopathy, they needlessly prolong their suffering or, in the worst case scenario, hasten their death. Awards of the above nature can undoubtedly have this effect.
In my view, this means that the award given to HISC by the National Lottery Community Fund gives an unlawful advantage to an organisation promoting a bogus therapy. At best, it is a waste of public funds, at worst it causes serious harm.
Surely, women who have experienced abuse and sexual violence deserve better!
I recently looked at the list of best-sellers in homeopathy on Amazon. To my surprise, there were several books that were specifically focused on the homeopathic treatment of children. Since we had, several years ago, published a systematic review of this subject, these books interested me. Here is what Amazon tells us about them:
Homeopathic remedies are increasingly being used to treat common childhood ailments. They are safe, have no side effects or allergic reactions, are inexpensive and, above all, effective. In this guide, Dana Ullman explains what homeopathy is, how it works and how you can use it correctly to enhance your child’s health. He recommends remedies for more than 75 physical and emotional conditions, including: allergies, grief, anxiety, headaches, asthma, measles, bedwetting, nappy rash, bites and stings, shock, burns, sunburn, colic, teething, coughs and colds and travel sickness
Without doubt, this is the most comprehensive book on homeopathic pediatrics. Included is a complete guide to the correct use of homeopathy, recommended remedies for the treatment of more than seventy-five common physical, emotional, and behavioral conditions, and valuable information on the essential medicines that all parents should have in their home medicine kits
Tricia Allen, a qualified homeopath, offers a host of practical advice on how to treat illness using natural, homeopathic remedies. Homeopathy differs from conventional medicine in that it does not only alleviate the individual symptoms of an illness, but treats the underlying state to ensure that the disease does not return, something which rarely occurs when using traditional remedies. This guide gives you advice on; what homeopathy is and how to use it; each stage of childhood and how to deal with the complaints that occur at that time of a child’s development; the most common childhood illnesses, how to take your own steps to treating them, which homeopathic remedies to use and when to seek medical help and first aid.
The Homeopathic Treatment of Children is indispensible at giving both a clear overall impression of the various major constitutional types, and also a detailed outline for reference at the end of each chapter. Not only does Paul Herscu draw from various sources (repertories and materia medica), he also adds indispensable original information from his successful practice.
______________________________
The fact that such books exist is perhaps not all that surprising. Yet, I do find the fact that they are among the best-selling books on homeopathy surprising – or to be more precise, I find it concerning.
Why?
Simple: children cannot give informed consent to the treatments they receive. Thus, consent is given for them by their parents or (I suspect often) not at all. This renders homeopathic treatment of children more problematic than that of fully competent adults.
Homeopathy has not been shown to be effective for any pediatric condition. I know Dana Ullman disagrees and claims it works for children’s allergies, grief, anxiety, headaches, asthma, measles, bedwetting, nappy rash, bites and stings, shock, burns, sunburn, colic, teething, coughs and colds, and travel sickness. Yet, these claims are not based on anything faintly resembling sound evidence! Our above-mentioned systematic review reached the following conclusion: “The evidence from rigorous clinical trials of any type of therapeutic or preventive intervention testing homeopathy for childhood and adolescence ailments is not convincing enough for recommendations in any condition.”
And what follows from this state of affairs?
I am afraid it is this:
Treating sick children with homeopathy amounts to child abuse.
Given the high prevalence of burdensome symptoms in palliative care (PC) and the increasing use of so-called alternative medicine (SCAM) therapies, research is needed to determine how often and what types of SCAM therapies providers recommend to manage symptoms in PC.
This survey documented recommendation rates of SCAM for target symptoms and assessed if, SCAM use varies by provider characteristics. The investigators conducted US nationwide surveys of MDs, DOs, physician assistants, and nurse practitioners working in PC.
Participants (N = 404) were mostly female (71.3%), MDs/DOs (74.9%), and cared for adults (90.4%). Providers recommended SCAM an average of 6.8 times per month (95% CI: 6.0-7.6) and used an average of 5.1 (95% CI: 4.9-5.3) out of 10 listed SCAM modalities. Respondents recommended mostly:
- mind-body medicines (e.g., meditation, biofeedback),
- massage,
- acupuncture/acupressure.
The most targeted symptoms included:
- pain,
- anxiety,
- mood disturbances,
- distress.
Recommendation frequencies for specific modality-for-symptom combinations ranged from little use (e.g. aromatherapy for constipation) to occasional use (e.g. mind-body interventions for psychiatric symptoms). Finally, recommendation rates increased as a function of pediatric practice, noninpatient practice setting, provider age, and proportion of effort spent delivering palliative care.
The authors concluded that to the best of our knowledge, this is the first national survey to characterize PC providers’ SCAM recommendation behaviors and assess specific therapies and common target symptoms. Providers recommended a broad range of SCAM but do so less frequently than patients report using SCAM. These findings should be of interest to any provider caring for patients with serious illness.
Initially, one might feel encouraged by these data. Mind-body therapies are indeed supported by reasonably sound evidence for the symptoms listed. The evidence is, however, not convincing for many other forms of SCAM, in particular massage or acupuncture/acupressure. So encouragement is quickly followed by disappointment.
Some people might say that in PC one must not insist on good evidence: if the patient wants it, why not? But the point is that there are several forms of SCAMs that are backed by good evidence for use in PC. So, why not follow the evidence and use those? It seems to me that it is not in the patients’ best interest to disregard the evidence in medicine – and this, of course, includes PC.