alternative medicine
I usually take ‘market reports’ with a pinch of salt. Having said that, this document makes some rather interesting predictions:
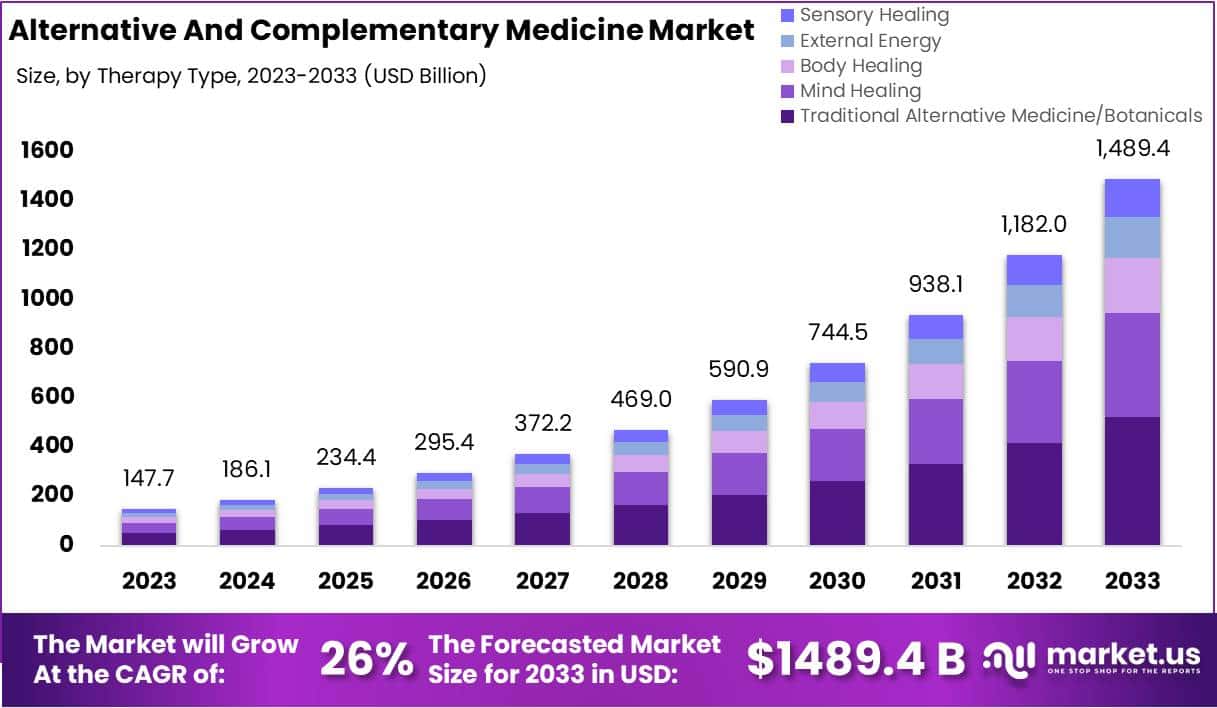
The size of the market for so-called alternative medicine (SCAM) is projected to expand from USD 147.7 billion in 2023 to approximately USD 1489.4 billion by the year 2033. This projection indicates a remarkable Compound Annual Growth Rate (CAGR) of 26% over the forecast period.
The market for SCAM is experiencing significant growth, fueled by increasing consumer interest in natural and holistic health solutions. This trend reflects a broader shift in societal attitudes towards health and wellness, emphasizing preventive care and natural health practices.
The market’s dynamics are influenced by various factors, including consumer preferences, regulatory standards, and evolving perceptions of health and wellness. As the popularity of these alternative therapies grows, it is crucial for individuals to consult with healthcare professionals to ensure that these non-conventional approaches are safely and effectively incorporated into their overall health regimen. The increasing acceptance of SCAM underscores a collective move towards more personalized and holistic healthcare solutions, resonating with today’s health-conscious consumers.
In 2023, Traditional Alternative Medicine/Botanicals led the market, capturing a 35.2% share, which reflects a strong consumer inclination towards these treatments. Dietary Supplements were prominent in the market, securing a 25.1% share in 2023, which underscores the high consumer demand for nutritional aids. Direct Sales were the most favored distribution channel, accounting for 43.2% of the market share in 2023, which indicates their significant impact on guiding consumer purchases. Pain Management was the predominant application area, holding a 24.9% market share in 2023, propelled by the growing acknowledgment of non-pharmacological treatment options. Adults represented a substantial portion of the market, making up 62.33% in 2023, signifying a marked preference for SCAM therapies within this age group. Europe stood out as the market leader, claiming a 42.6% share in 2023, a position supported by widespread acceptance, governmental backing, and an increasing elderly population. The regions of North America and Asia-Pacific are highlighted as areas with potential, signaling opportunities for market expansion beyond the European stronghold in the upcoming years.
Leading Market Players Are:
- Columbia Nutritional
- Nordic Nutraceuticals
- Ramamani Iyengar Memorial Yoga Institute
- The Healing Company Ltd.
- John Schumacher Unity Woods Yoga Centre
- Sheng Chang Pharmaceutical Company
- Pure encapsulations LLC.
- Herb Pharm
- AYUSH Ayurvedic Pte Ltd.
Recent developments:
- In December 2023, Adoratherapy launched the Alkemie Chakra Healing Line, an aromatherapy range aimed at harmonizing the seven chakras.
- Coworth Park introduced the Hebridean Sound Treatment in October 2023, merging traditional Hebridean sounds with guided meditation to offer a novel, restorative wellness experience.
- The World Health Organization released draft guidelines in September 2023 for the safe, effective application of traditional medicines.
- Telehealth services, expanding significantly in August 2023, have broadened the reach of SCAM, enhancing patient access to these treatments.
According to its authors, this study‘s objective was to demonstrate that acupuncture is beneficial for decreasing the risk of ischaemic stroke in patients with rheumatoid arthritis (RA).
The investigation was designed as a propensity score-matched cohort nationwide population-based study. Patients with RA diagnosed between 1 January 1997 and 31 December 2010, through the National Health Insurance Research Database in Taiwan. Patients who were administered acupuncture therapy from the initial date of RA diagnosis to 31 December 2010 were included in the acupuncture cohort. Patients who did not receive acupuncture treatment during the same time interval constituted the no-acupuncture cohort. A Cox regression model was used to adjust for age, sex, comorbidities, and types of drugs used. The researchers compared the subhazard ratios (SHRs) of ischaemic stroke between these two cohorts through competing-risks regression models.
After 1:1 propensity score matching, a total of 23 226 patients with newly diagnosed RA were equally subgrouped into acupuncture cohort or no-acupuncture cohort according to their use of acupuncture. The basic characteristics of these patients were similar. A lower cumulative incidence of ischaemic stroke was found in the acupuncture cohort (log-rank test, p<0.001; immortal time (period from initial diagnosis of RA to index date) 1065 days; mean number of acupuncture visits 9.83. In the end, 341 patients in the acupuncture cohort (5.95 per 1000 person-years) and 605 patients in the no-acupuncture cohort (12.4 per 1000 person-years) experienced ischaemic stroke (adjusted SHR 0.57, 95% CI 0.50 to 0.65). The advantage of lowering ischaemic stroke incidence through acupuncture therapy in RA patients was independent of sex, age, types of drugs used, and comorbidities.
The authors concluded that this study showed the beneficial effect of acupuncture in reducing the incidence of ischaemic stroke in patients with RA.
It seems obvious that the editors of ‘BMJ Open’, the peer reviewers of the study and the authors are unaware of the fact that the objective of such an investigeation is not to to demonstrate that acupuncture is beneficial but to test whether acupuncture is beneficial. Starting a study with the intention to to show that my pet therapy works is akin to saying: “I am intending to mislead you about the value of my intervention”.
One needs therefore not be surprised that the authors of the present study draw very definitive conclusions, such as “acupuncture therapy is beneficial for ischaemic stroke prevention”. But every 1st year medical or science student should know that correlation is not the same as causation. What the study does, in fact, show is an association between acupuncture and stroke. This association might be due to dozens of factors that the ‘propensity score matching’ could not control. To conclude that the results prove a cause effect relationship is naive bordering on scientific misconduct. I find it most disappointing that such a paper can pass all the hurdles to get published in what pretends to be a respectable journal.
Personally, I intend to use this study as a good example for drawing the wrong conclusions on seemingly rigorous research.
An article entitled “Homeopathy for worm infestations in children’s” caught my eye. Here is the un altered abstract:
Unusual sorts of worms can be there in a child’s stomach and may initiate several health complications such as pain, infection etc. To treat worm infections, one must identify about various categories of worms, and after understanding the kind of infection induced by the worm’s the treatment for the babies or children can planned. There are various Homeopathic medicines available which be used to treat worm infections without any side effects on the health of the children’s. In this paper we have discussed how the worm infection has been treated at our homeopathic research institute.
In the paper itself, the author, Dr. AK Dwivedi (Professor and H.O.D, Department of Physiology and Biochemistry, SKRP Guajarati Medical College, Indore, Madhya Pradesh, India), explains:
Homeopathic do not take care of just the disease, but is prescribed on the base of physical, emotional and genetic condition of a person. Homeopathic medicines act on both the mental and physical levels of individuals. Homeopathy is a natural and mild system of medicines that utilizes minute doses of well-researched remedies to improve the body’s natural curing procedure. Homeopathic medicines originate from substances that come’s from plants, minerals & animals.
The author’s conclusion is equally impressive:
On the basis of our research and after analysing the patients after medication we have found that homeopathy can completely cure the worm infection, If the dosages are properly prescribed and taken on that basis of investigation reports from time to time under guidance of experienced Homeopathic Physician worm infection can be treated with homeopathy effectively.
Yes, this level of incompetence could be quite funny! But sadly, it is also quite concerning. Most worm infestations are easily treated with effective conventional therapies. Untreated, they can have serious consequences. To advocate homeopathy – which is of course ineffective – is irresponsible, unethical and arguably criminal, in my view.
There are many variations of acupuncture. Electroacupuncture (EA) and Laseracupuncture (LA) are but two examples both of which are commonly used. However, it remains uncertain whether LA is as effective as EA. This study aimed to compare EA and LA head to head in dysmenorrhea.
A crossover, randomized clinical trial was conducted. EA or LA was applied to selected acupuncture points. Participants were randomized into two sequence treatment groups who received either EA or LA twice per week in luteal phase for 3 months followed by 2-month washout, then shifted to other groups (sequence 1: EA > LA; sequence 2: LA > EA). Outcome measures were heart rate variability (HRV), prostaglandins (PGs), pain, and quality-of-life (QoL) assessment (QoL-SF12). We also compared the effect of EA and LA in low and high LF/HF (low frequency/high frequency) status.
43 participants completed all treatments. Both EA and LA significantly improved HRV activity and were effective in reducing pain (Visual Analog Scale [VAS]; EA: p < 0.001 and LA: p = 0.010) and improving QoL (SF12: EA: p < 0.001, LA, p = 0.017); although without intergroup difference. EA reduced PGs significantly (p < 0.001; δ p = 0.068). In low LF/HF, EA had stronger effects than LA in increasing parasympathetic tone in respect of percentage of successive RR intervals that differ by more than 50 ms (pNN50; p = 0.053) and very low-frequency band (VLF; p = 0.035).
The authors concluded that there is no significant difference between EA and LA in improving autonomic nervous system dysfunction, pain, and QoL in dysmenorrhea. EA is prominent in PGs changing and preserving vagus tone in low LF/HF; yet LA is noninvasive for those who have needle phobia. Whether LA is equivalent with EA and the mechanism warrants further study.
Looking at the affiliations of the authors, one might expect that they should be able to design a meaningful study:
- 1Division of Hemato-Oncology, Department of Internal Medicine, Branch of Zhong-Zhou, Taipei City Hospital, Taipei, Taiwan.
- 2Institute of Traditional Medicine, National Yang-Ming Chiao Tung University, Taipei, Taiwan.
- 3Department of Traditional Medicine, Branch of Yang-Ming, Taipei City Hospital, Taipei, Taiwan.
- 4Department of Traditional Medicine, Branch of Kunming, Taipei City Hospital, Taipei, Taiwan.
- 5Department of Gynecology and Obstetrics, Branch of Yang-Ming, Taipei City Hospital, Taipei, Taiwan.
Sadly, this assumption is evidently mistaken.
The trial certainly does not show what they claim and neither had it ever the chance to show anything relevent. A clinical trial is comparable to a mathematical equation. It can be solved, if it has one unkown; it cannot produce a result, if it has two unknowns.
The efficacy of EA and LA for dysmenorrhea are both unknown. A comparative study with two unknowns cannot produce a meaningful result. EA and LA did not both improve autonomic nervous system dysfunction, pain, and QoL in dysmenorrhea but most likely they both had no effect. What caused the improvement was not the treatment per se but the ritual, the placebo effect, the TLC or other non-specific factors. The maginal differences in other parameters are meaningless; they are due to the fact that – as an equivalence trial – the study was woefully underpowered and thus open to coincidental differences.
Clinical trials should be about contributing to our knowledge and not about contributing to confusion.
Here is the abstract of a recent article that I find worrying:
In 2020, severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) challenged the world with a global outbreak that led to millions of deaths worldwide. Coronavirus disease 2019 (COVID-19) is the symptomatic manifestation of this virus, which can range from flu-like symptoms to utter clinical complications and even death. Since there was no clear medicine that could tackle this infection or lower its complications with minimal adverse effects on the patients’ health, the world health organization (WHO) developed awareness programs to lower the infection rate and limit the fast spread of this virus. Although vaccines have been developed as preventative tools, people still prefer going back to traditional herbal medicine, which provides remarkable health benefits that can either prevent the viral infection or limit the progression of severe symptoms through different mechanistic pathways with relatively insignificant side effects. This comprehensive review provides scientific evidence elucidating the effect of 10 different plants against SARS-CoV-2, paving the way for further studies to reconsider plant-based extracts, rich in bioactive compounds, into more advanced clinical assessments in order to identify their impact on patients suffering from COVID-19.
The conclusions of this paper read as follows:
…since these 10 herbs hold distinct bioactive compounds with significant properties in vitro and with remarkable benefits to human health, it is possible to prevent SARS-CoV-2 infection and reduce its symptomatic manifestations by consuming any of these 10 plants according to the recommended dose. The diversity in bioactive molecules between the different plants exerts various effects through different mechanisms at once, which makes it more potent than conventional synthetic drugs. Nonetheless, more studies are needed to highlight the clinical efficacy of these extracts and spot their possible side effects on patients, especially those with comorbidities who take multiple conventional drugs.
I should point out that the authors fail to offer a single reliable trial that would prove or even imply that any of the 10 herbal remedies can effectively treat or prevent COVID infections (to the best of my knowledge, no such studies exist). Laguage like “it is possible to prevent SARS-CoV-2 infection and reduce its symptomatic manifestations” is therefore not just misleading but highly dangerous and deeply unethical. Sadly, such evidence-free claims abound in herbal medicine.
I think the journal editor, the peer-reviewer, the authors and their universities ( University of Tripoli in Lebanon, American University of the Middle East, Egaila in Kuwait, University of Balamand, Kalhat, Tripoli in Lebanon, Lebanese University, Tripoli in Lebanon, Aix-Marseille Université in France) should be ashamed to produce such dangerous rubbish.
Acute Otitis Media (AOM) is one of the most common acute infections in children and often injudiciously treated by antibiotics. Homeopathy has been claimed to work but is it really effective?
This open label, randomized, controlled, parallel arm trial was conducted on children (aged 0–12 years), suffering from AOM. The primary outcome was changes in Tympanic Membrane Examination scale (TMES) and Acute Otitis Media-Severity of Symptoms (AOM-SOS) scale, time to improvement in pain through Facial Pain Scale-Revised (FPS-R) over 10 days. The need for antibiotics in both groups and the recurrence of subsequent episodes of AOM over 12 months were also compared.
Intention-to-treat analysis was performed on 222 children; Homeopathy (n = 117) (H-group), Allopathy (A-group) (n = 105). There was a statistically significant reduction of scores in H-group compared with A-group at each time point: at day 3 (mean diff. ± sd: 1.71 ± 0.19; 95% CI: 1.34 to 2.07; p = 0.0001), at day 7 (mean diff. ± sd: 1.29 ± 0.24; 95% CI: 0.82 to 1.76; p = 0.0001) and at day 10 (mean diff. ± sd: 1.23 ± 0.25; 95% CI = 0.74 to 1.71; p = 0.0001) favoring homeopathy. Clinical failure by the third day of treatment was observed in 11% and 24% of children in H-group vs A-group (OR: 0.03; 95% CI: 0.001 to 0.52; p = 0.03). None of the children in the H-group required antibiotics, whereas 14 children in the A-group did.
The authors concluded that both therapies seemed to produce comparable effects and appeared safe. The study consolidated the findings observed during a pilot study, i.e., homeopathy is non-inferior to allopathy in managing AOM in children and antibiotics in children can be avoided.
This study was published in the journal ‘Homeopathy’ and originates from the Central Council for Research in Homeopathy, New Delhi, India. Sadly, I do not have the full text of the paper and cannot therefore scrutinize it adequately.
Let me just mention these three facts:
- The journal ‘Homeopathy’ never publishes negative results.
- Indian researchers of homeopathy publish as good as no negative results.
- As far as I can see, the Central Council for Research in Homeopathy, New Delhi, has never published a negative result.
These points do, of course, not necessarily mean that the study is false-positive, but they do not inspire me with confidence. In any case, it seems wise to insist on better evidence. To render it credible, we would need:
- Several rigorous RCTs that test homeopathy for AOM against placebo.
- If (and only then) they show that homeopathy is better than placebo, at least one independent replication of the present study.
As the biological plausibility of all this is close to zero, the chances that this will happen are also zero.
Traditional herbal medicine (THM) is frequently used in pediatric populations. This is perticularly true in many low-income countries. Yet THM has been associated with a range of adverse events, including liver toxicity, renal failure, and allergic reactions. Despite these concerns, its impact on multi-organ dysfunction syndrome (MODS) risk has so far not been thoroughly investigated.
This study aimed to investigate the incidence and predictors of MODS in a pediatric intensive care unit (PICU) in Ethiopia, with a focus on the association between THM use and the risk of MODS. It was designed as a single-center prospective cohort study conducted at a PICU in the university of Gondar Comprehensive Specialized hospital, Northwest Ethiopia. The researchers enrolled eligible patients aged one month to 18 years admitted to the PICU during the study period. Data on demographic characteristics, medical history, clinical and laboratory data, and outcome measures using standard case record forms, physical examination, and patient document reviews. The predictors of MODS were assessed using Cox proportional hazards models, with a focus on the association between traditional herbal medicine use and the risk of MODS.
A total of 310 patients were included in the final analysis, with a median age of 48 months and a male-to-female ratio of 1.5:1. The proportion and incidence of MODS were 30.96% (95% CI:25.8, 36.6) and 7.71(95% CI: 6.10, 9.40) per 100-person-day observation respectively. Renal failure (17.74%), neurologic failure (15.16%), and heart failure (14.52%) were the leading organ failures identified. Nearly one-third of patients (32.9%) died in the PICU, of which 59.8% had MODS. The rate of mortality was higher in patients with MODS than in those without. The Cox proportional hazards model identified renal disease (AHR = 6.32 (95%CI: 3.17,12.61)), intake of traditional herbal medication (AHR = 2.45, 95% CI:1.29,4.65), modified Pediatric Index of Mortality 2 (mPIM 2) score (AHR = 1.54 (95% CI: 1.38,1.71), and critical illness diagnoses (AHR = 2.68 (95% CI: 1.77,4.07)) as predictors of MODS.
The authors concluded that the incidence of MODS was high. Renal disease, THM use, mPIM 2 scores, and critical illness diagnoses were independent predictors of MODS. A more than twofold increase in the risk of MODS was seen in patients who used TMH. Healthcare providers should be aware of risks associated with THM, and educate caregivers about the potential harms of these products. Future studies with larger sample sizes and more comprehensive outcome measures are needed.
I do fully agree with the authors about the high usage of herbal and other so-called alternative medicines by children. We have shown that, in the UK the average one-year prevalence rate was 34% and the average lifetime prevalence was 42%. We have furthermore shown that the evidence base for these treatments in children is weak, even more so than for general populations. Finally, we can confirm that adverse effects are far from rare and often serious.
It is therefore high time, I think, that national regulators do more to protect children from SCAM practitioners who are at best uncritical about their treatments and at worse outright dangerous.
Jennifer Jacobs started publishing peer-reviewed papers on homeopathy in the early 1990s. This happens to be around the same time as I did. So, we both have about 30 years of research into homeopathy behind us.
Jennifer just authored a paper entitled “Thirty Years of Homeopathic Research – Lessons Learned“. Here is its abstract:
Conducting double-blind randomized controlled trials is difficult, even in the allopathic medical system. Doing so within the paradigm of classical homeopathy is even more challenging. More than thirty years of experience in carrying out such trials has taught me much about the pitfalls to avoid as well as the factors that can lead to success. The initial steps of putting together a research protocol, securing funding, and obtaining human subjects’ approval can be daunting. After that comes developing questionnaires and surveys, hiring study personnel, and recruitment of subjects. The actual implementation of the research comes with its own set of possible missteps. Sample size determination, entry criteria, as well as type, frequency and duration of treatment are all crucial. Finally, statistical analysis must be performed to a high standard and a manuscript prepared to submit for publication. Even then there can be one or more manuscript revisions to make, based on feedback from reviewers, before a study is actually published. The entire process can take at least two years and is usually much longer.
Mistakes at any one of these steps can damage the outcome, as well as the impact of the study. With examples from my body of research, I will discuss some of the things that I wish I had done differently, as well as those that turned out to be correct. Homeopathic research is held to a much higher standard than conventional trials. Any flaws in study design, implementation, and analysis can be used by critics to negate the results. I am hopeful that the next generation of homeopathic researchers will learn from my experiences and carry on with great success.
Jennifer’s example motivated me to follow suit and contribute some very brief thoughts about my 30 years of homeopathy research and the lessons I have learnt:
Conducting double-blind randomized controlled trials is difficult in any area of medicine. Yet these types of studies are by far the best way to find out which treatments work and which don’t. Therefore, they need doing, regardless of the obstacles they may pose.
In homeopathy, we now have a large body of such trials. Sadly, not all of them are reliable. Those that are, according to accepted criteria, tend to fail to show that homeopathy works better than a placebo. Understandably, homeopaths are disappointed with this overall result and have made numerous attempts to invalidate it.
The main problem with research into homeopathy is not the research methodology. It is well established for clinical trials and can be easily modified to fit all the demands made by individualised treatment or other pecularities that may apply to homeopathy. The main problem is the homeopath who finds it impossible to accept the truth, namely that highly diluted homeopathic remedies are pure placebos and any observed benefits of homeopathy are due to non-specific effects such as the empathetic encounter or a placebo response.
The lesson to be learned from the past is that, in medicine, even the most obsessive belief, conviction or wishful thinking will eventually have to give way to the scientific evidence. In the case of homeopathy, this process has taken an extraordinary amount of time and effort but, finally, we are almost there and the writing is on the wall for everyone to see.
Two resumes of 30 years of work, research and experience!
And what a difference between them!
Who do you think gets closer to the truth,
Jennifer or I?
Of all the forms of so-called alternative medicine (SCAM), Reiki is amongst the least plausible. It is a form of paranormal or ‘energy healing’ popularised by Japanese Mikao Usui (1865–1926). Reiki is based on the assumptions of Traditional Chinese Medicine and the existence of ‘chi’, the life-force that is assumed to determine our health.
Reiki practitioners believe that, with their hands-on healing method, they can transfer ‘healing energy’ to a patient which, in turn, stimulates the self-healing properties of the body. They assume that the therapeutic effects of this technique are obtained from a ‘universal life energy’ that provides strength, harmony, and balance to the body and mind.
Despite its implausibility, Reiki is used for a very wide range of conditions. Some people are even convinced that it has positive effects on sexuality. But is that really so?
This randomised clinical trial was aimed at finding out. Specifically, its authors wanted to determine the effect of Reiki on sexual function and sexual self-confidence in women with sexual distress*. It was was conducted with women between the ages of 15–49 years who were registered at a family health center in the eastern region of Turkey and had sexual distress.
The sample of the study consisted of 106 women, 53 in the experimental group and 53 in the control group. Women in the experimental group received Reiki once a week for four weeks, while no intervention was applied to those in the control group. Data were collected using the Female Sexual Distress Scale-Revised (FSDS-R), the Arizona Sexual Experiences Scale (ASEX), and the Sexual Self-confidence Scale (SSS).
The levels of sexual distress, sexual function, and sexual self-confidence of women in both groups were similar before the intervention, and the difference between the groups was not statistically significant (p > 0.05). After the Reiki application, the FSDS-R and ASEX mean scores of women in the experimental group significantly decreased, while their SSS mean score significantly increased, and the difference between the groups was statistically significant (p < 0.05).
The authors concluded that Reiki was associated with reduced sexual distress, positive outcomes in sexual functions, and increase sexual self-confidence in women with sexual distress. Healthcare professionals may find Reiki to positively enhance women’s sexuality.
Convinced?
I hope not!
The study has the most obvious of all design flaws: it does not control for a placebo effect, nor the effect of empaty/sympathy received from the therapist, nor the negative impact of learning that you are in the control group and will thus not receive any treatment or attention.
To me, it is obvious that these three factors combined must be able to bring about the observed outcomes. Therefore, I suggest to re-write the conclusions as follows:
The intervention was associated with reduced sexual distress, positive outcomes in sexual functions, and increase sexual self-confidence in women with sexual distress. Considering the biological plausibility of a specific effect of Reiki, the most likely cause for the outcome are non-specific effects of the ritual.
*[Sexual distress refers to persistent, recurrent problems with sexual response, desire, orgasm or pain that distress you or strain your relationship with your partner. Yes, I had to look up the definition of that diagnosis.]
Yes, I often moan about the abundance of poor-quality prevalence surveys that we are confronted with when scanning the literaturee on so-called alternative medicine (SCAM), e.g.:
- The survey mania in so-called alternative medicine prevents progress
- A truly homeopathic survey
- A new survey of CAM-use (or is it a promotion for more nonsense on the NHS?)
- A new chiropractic survey seems to avoid all the potentially embarrassing questions
- Survey-mania in alternative medicine: a fruitless, misleading and counter-productive distraction
Here is another example that recently appeared on my screen and that allows me to explain (yet again) why these surveys are such a waste of space:
The Use of Traditional and Complementary Medicine Among Patients With Multiple Sclerosis in Morocco
Let’s assume the survey is done perfectly (a condition that most are very far from meeting). If the information generated by such a perfect survey were worthwhile, we would also need to consider possible mutations that would be just as relevant:
- We have just over 200 nations (other than Morocco) on the planet.
- I assume there are about 1000 conditions (other than multiple sclerosis) for which SCAM is used.
- There are, I estimate, 100 different definitions of SCAM (other than ‘traditional and complementary medicine’) that all include different modalities.
So, this alone would make 20 000 000 surveys that would be important enough to get published. But that’s not all. The usage and nature of SCAM change fairly quickly. That means we would need these 20 million surveys to be repeated every 2 to 3 years to be up-to-date.
For all this, we would need, I estimate, 200 000 research groups doing the work and about 20 000 SCAM journals to publish their results.
I think we can agree that this would be a nonsensical effort for producing millions of papers reaching dramatic conclusions that read something like this:
Our survey shows that patients suffering from xy living in yz use much SCAM. This level of popularity suggests that SCAM is much appreciated and needs to be made available more widely and free of charge.
I rest my case.
