alternative medicine
Apparently, Hahnemann gave a lecture on the subject of veterinary homeopathy in the mid-1810s. Ever since, homeopathy has been used for treating animals. Von Boennighausen was one of the first influential proponents of veterinary homeopathy. However, veterinary medical schools tended to reject homoeopathy, and the number of veterinary homeopaths remained small. In the 1920ies, veterinary homoeopathy was revived in Germany. Members of the “Studiengemeinschaft für tierärztliche Homöopathie” (Study Group for Veterinary Homoeopathy) which was founded in 1936 started to investigate this approach systematically.
Today, veterinary homeopathy is still popular in some countries. Prince Charles has become a prominent advocate who claims to treat his own life stock with homeopathy. In many countries, veterinary homeopaths have their own professional organisations. Elsewhere, however, veterinarians are banned from practicing homeopathy. In the UK, only veterinarians are allowed to use homeopathy on animals (but anyone regardless of background can use it on human patients) and there is a British Academy of Veterinary Homeopathy. In the US, homeopathic vets are organised in the Academy of Veterinary Homeopathy.
If this sounds promising, we should not forget that, as discussed so often on this blog, homeopathy lacks plausibility the evidence for veterinary homeopathy fails to be positive (see for instance here). But, hold on, there is a new study, perhaps it will change everything?
This ‘study‘ was aimed at providing an initial insight into the existing prerequisites on dairy farms for the use of homeopathy (i.e. the consideration of homeopathic principles) and on homeopathic treatment procedures (including anamnesis, clinical examination, diagnosis, selection of a remedy, follow-up checks, and documentation) on 64 dairy farms in France, Germany and Spain.
The use of homeopathy was assessed via a standardised questionnaire during face-to-face interviews. The results revealed that homeopathic treatment procedures were applied very heterogeneously and differed considerably between farms and countries. Farmers also use human products without veterinary prescription as well as other prohibited substances.
The authors of this ‘study’ concluded that the subjective treatment approach using the farmers’ own criteria, together with their neglecting to check the outcome of the treatment and the lack of appropriate documentation is presumed to substantially reduce the potential for a successful recovery of the animals from diseases. There is, thus, a need to verify the effectiveness of homeopathic treatments in farm practices based on a lege artis treatment procedure and homeopathic principles which can be achieved by the regular monitoring of treatment outcomes and the prevailing rate of the disease at herd level. Furthermore, there is a potential risk to food safety due to the use of non-veterinary drugs without veterinary prescription and the use of other prohibited substances.
So did this ‘study’ change the evidence on veterinary homeopathy?
Sadly not!
This ‘study’ is hardly worth the paper it is printed on.
Who conceives such nonsense?
And who finances such an investigation?
The answer to the latter question is one of the few provided by the authors: This project has received funding from the European Union’s Seventh Framework Programme for research, technological development and demonstration under Grant Agreement No 311824 (IMPRO).
Time for a constructive suggestion! Could the European Union’s Seventh Framework Programme with their next research project in veterinary homeopathy please evaluate the question why farmers in the EU are allowed to use disproven therapies on defenceless animals?
An abstract from the recent ‘2nd OFFICIAL SIPS CONFERENCE ON PLACEBO STUDIES’ caught my attention. It is not available on-line; therefore let me reproduce it here in full:
The role of placebo effects in mindfulness-based analgesia 1. Jonathan Davies. University of Sydney, Sydney, NSW, Australia. 2. Louise Sharpe. University of Sydney, Sydney, NSW, Australia. 3. Melissa Day. University of Queensland, Brisbane, QLD, Australia. 4. Ben Colagiuri. University of Sydney, Sydney, NSW, Australia.
Background: Mindfulness meditation can reduce pain both in experimental and clinical settings, though it is not known to what extent mindfulness-specific vs placebo-like expectancy effects account for these changes. This study aimed to: 1. establish whether placebo effects contribute to mindfulness-mediated analgesia; and 2. identify putative cognitive mechanisms responsible for placebo- vs mindfulness-mediated analgesia. Methods: We compared the effects of focussed-attention mindfulness training (6 x 20 min), sham mindfulness, and a no-treatment in a double-blind RCT for experimental heat pain. Sham mindfulness instructions lacked the ‘active ingredients’ of the real training but were matched on all other contextual factors. Results: Both real and sham mindfulness training led to greater pain tolerance relative to no treatment, but there was no difference between the real and sham training. This was accompanied by increased expectancy, beliefs, and pain-related cognitive processes in the two mindfulness groups relative to no treatment, but again there were no differences between real and sham training on these outcomes. There were no effects on pain intensity, pleasantness or threshold. Conclusion: These findings suggest that mindfulness training – at least those involving focused-attention – may lead to improved pain tolerance via the placebo effect rather than any specific mindfulness-related mechanisms. Potential mediators of these effects will be discussed.

I find this study remarkable in two ways:
- It shows that, with a bit of fantasy, ingenuity and will, one can design and use sham procedures even in clinical trials of mind/body therapies.
- Its results suggest that, if one does control for placebo effects, these treatments may not prove to be more than a placebo therapy.
What implications might this have for clinical practice?
Mindfulness is currently hugely popular. It would not be surprising, if the news that it might rely purely on placebo effects would calm down the enthusiasm about this treatment. Many might ask, does it matter? As long as patients benefit, the mechanism of action seems irrelevant. This, of course, is an interesting debate which we have had on this blog many times before.
What do you think?
Yesterday, I had the honour and pleasure to present to the UK press my new book entitled ‘ALTERNATIVE MEDICINE, A CRITICAL ASSESSMENT OF 150 MODALITIES’ (see also my previous post). The SCIENCE MEDIA CENTRE had invited me to do a ‘media briefing’ on the occasion of its publication. I did this by outlining the background around so-called alternative medicine (SCAM) and explaining the concept of the new book which essentially is – as its title indicates – to provide concise and critical assessments of 150 modalities.
In the course of my short presentation, I mentioned the following exotic modalities in order to show that my book goes beyond the ‘usual suspects’ of acupuncture, chiropractic, etc.:
- BERLIN WALL
- COLLOIDAL SILVER
- PALEO DIET
- PLACENTOPHAGY
- URINE THERAPY
- CUPPING
- GUA SHA
- LYMPH DRAINAGE
- SLAPPING THERAPY
- VISCERAL OSTEOPATHY
- JOHREI HEALING
- LEECH THERAPY
- NEURAL THERAPY
- ZERO BALANCE
- APPLIED KINESIOLOGY
- IRIDOLOGY
- LIVE BLOOD ANALYSIS
- PULSE DIAGNOSIS
- RADIONICS
As it turned out, the journalists present found the BERLIN WALL remedy the most fascinating aspect of my talk. And this is clearly reflected in today’s articles covering the event:
The DAILY TELEGRAPH published an article much in the same vein, and so did THE SUN and the EXPRESS (not available on line). The only UK newspaper I have seen so far going beyond the Berlin Wall topic is THE DAILY MAIL. The paper mentions several other so-called alternative medicines (SCAMs) that consumers need to be protected from, in my view.
Interestingly, none of the articles mentioned that my new book is not an exercise in debunking. During my presentation, I made the point that several of my assessments of 150 modalities do arrive at positive conclusions for therapies that demonstrably generate more good than harm.
I also tried to point out to the journalists that SCAM includes a range of diagnostic techniques. None of them are valid which means that they present a real danger to consumers through false-positive and false-negative diagnoses. In particular the latter scenario can cost lives.
All in all, I did enjoy yesterday’s press briefing very much. I am aware of the fact that, in the realm of SCAM, the press have a most important role to play. Consumers rarely consult their doctor when deciding to use SCAM; frequently they go by what they read in the papers.
In this context, I find it noteworthy that, during the last years, the UK press have become considerably more sceptical. Not so long ago, most UK journalists used to praise SCAM like the best thing since sliced bread; today this attitude has laudably shifted towards a more rational stance. I am sure that the excellent work of the SCIENCE MEDIA CENTRE has played a crucial part in this positive development.
The ‘College of Medicine and Integrated Health’ (CMIH) has been the subject of several previous blog posts (see for instance here, here and here). Recently, they have come up with something new that, in my view, deserves a further comment.
The new ‘SELF CARE TOOL KIT’ began, according to the CMIH, in 2009 with a national multi-centre project commissioned by the UK Department of Health, to consider the best way to integrate self care into family practice. The project involved two large family health centres and two university departments. One output was the Self Care Library (SCL).
The Self Care Library (SCL) is an online patient resource providing free evidence-based information about self-care. The funding for the SCL did, however, not survive, and the facility was assigned to the CMIH. Thanks to funding from ‘Pukka Herbs Vitamins, Herbal Remedies & Health Supplements‘, the CMIH was able to transfer the content and to begin updating entries. Simon Mills, the coordinator of the original project who is now employed by Pukka, has led this transformation and helped the College set up the new parent portal, Our Health Directory.
The Self Care Toolkit is thus the new SCL. All concerned with this project are experienced in clinical practice and can separate the theory from real life needs. We all have academic lives as well so can be hard-nosed with the evidence base as well.
_______________________________________________________________
The above text is essentially based on the information provided by the CMIH. A few critical remarks and clarifications might therefore be in order:
- What does ‘separate the theory from real life needs’ mean? Does it mean that the scientific evidence can be interpreted liberally (see below)?
- Is it a good idea to have a commercial sponsor for such a project?
- Is it wise that the main person in charge is on the payroll of a manufacturer of dietary supplements?
- Is there any oversight to minimise undue bias and prevent the public from being misled?
- Is it really true that all people involved have academic lives? Simon Mills (who once was a member of my team) has no longer an academic appointment, as far as I know.
But, you are right, these are perhaps mere trivialities. Let’s see what the ‘Self Care Tool Kit’ actually delivers. I have chosen the entry on DEPRESSION to check its validity. Here it is:
_______________________________________________________________
It isn’t likely that taking extra vitamins will make much difference to low mood or depression. It is true that many people don’t get quite enough B, C and D vitamins in their food. And it’s also true that the brain and nervous system need these vitamins. Because they don’t get stored in the body, our daily diet has to supply them. Research has shown that people with low blood levels of the B vitamin folic acid are more likely to be depressed and less likely to do well on anti-depressant medicines. So, if you are eating a very poor diet, taking extra vitamins just might help. It’s also worth remembering that alcohol, refined sugars, nicotine and caffeine all take these vitamins out of the body. Yet most people who feel depressed probably won’t benefit from taking vitamins alone. To ensure that you get a good balance of these vitamins, try to eat more whole-foods, fruits, vegetables, nuts and seeds.
Some people say that taking high doses of vitamin C (1-2 g and more a day) helps lift their mood. There is a little research to support this and none showing that high doses of vitamin C actually help clinical depression. Vitamin C levels fall after surgery or inflammatory disease. The body needs more vitamin C when coping with stress, pregnancy and breast feeding. Aspirin, tetracycline and contraceptive pills take vitamin C out of the body. Smokers also need extra vitamin C because nicotine removes it. Fresh fruit and vegetables are the best sources of vitamin C.
Doctors are increasingly concerned about low vitamin D, especially in the Asian community. A lack of vitamin D can lead to depression. Oily fish and dairy products are good sources of vitamin D, and sunlight helps the body make vitamin D. Do you get enough sunshine and eat a good diet? It is estimated that worldwide over 1 billion people get too little vitamin D.
Evidence
Taking supplements of vitamins B and D might help some people, whose diet is poor, but more research is needed.
Safety
Very high doses of vitamins and minerals can upset the body and cause side-effects. Get medical advice if you intend to take large doses. To ensure that you get a good balance of these vitamins, try to eat more whole-foods, fruits, vegetables, nuts and seeds.
Cost
If your diet is poor and you don’t get into the sun, ask your doctor about a vitamin D blood test. If it’s normal, there’s no point in taking vitamin D. If it’s low, your GP will prescribe it for you or you can buy a vitamin D supplement.
___________________________________________________________________
In my view, this text begs several questions:
1) Am I right in thinking that phraseology such as the one below will encourage patients suffering from depression to try the supplements mentioned?
- people with low blood levels of the B vitamin folic acid are more likely to be depressed and less likely to do well on anti-depressant medicines..
- Some people say that taking high doses of vitamin C (1-2 g and more a day) helps lift their mood…
- There is a little research to support this and none showing that high doses of vitamin C actually help clinical depression…
- A lack of vitamin D can lead to depression.
- Taking supplements of vitamins B and D might help some people…
- … your GP will prescribe it for you or you can buy a vitamin D supplement.
2) How does that tally with the latest evidence? For instance:
- No significant reduction in depression was seen after vitamin D supplementation compared to placebo
- No additional effects from nutritional supplementation were detected
- Adding vitamin C to citalopram did not increase the efficacy of citalopram in MDD patients.
3) The CMIH state: ‘This site gives you information NOT medical advice.’ But, in view of the actual text above, is this true?
4) Depression is a life-threatening condition. Is there a risk that patients trust the CMHI’s (non-) advice and commit suicide because of its ineffectiveness?
5) Do Pukka, the sponsor of all this, happen to supply most of the self care remedies promoted in the ‘Self Care Tool Kit’?
The answer to the last question, I am afraid, is YES!
Before a scientific paper gets published in a journal, it is submitted to the process of peer-review. Essentially, this means that the editor sends it to 2 or 3 experts in the field asking them to review the submission. Reviewers usually do not get any reward for this, yet the task they are asked to do can be tedious, difficult and time-consuming. Therefore, most reviewers think carefully before accepting it.
My friend Timothy Caulfield was recently invited by a medical journal to review a study of homeopathy. Here is his response to the editor as posted on Twitter:
I find myself regularly in similar situations. Yet, I have never responded in this way. Here is what I normally do:
- I have a look at the journal itself. If it is one of those SCAM publications, I tend to politely reject the invitation because, in my experience, their review process is farcical and not worth the effort. All too often it has happened that I reviewed a paper that was of very poor quality and thus recommended rejecting it. Yet the editor ignored my expert opinion and published the article nevertheless. This is why, several years ago, I decided enough is enough and no longer consider investing my time is such frustrating work.
- If the journal is of decent standing, I would have a look at the submission the editor sent me. If it makes any sense at all I would consider reviewing it (obviously depending on whether I have the time and the expertise).
- If a decent journal invites me to review a nonsensical paper (I assume that was the case Timothy referred to), I find myself in the same position as my friend Timothy. But, contrary to Timothy, I normally take the trouble to write a critical review of a nonsensical submission. Why? The reason is simple: if I don’t do it, the editor will simply send it to another reviewer. Many journals allow authors to suggest reviewers of their choice. Thus, the editor might send the submission next to the person suggested by the author who most likely will write a favourable review, thus hugely increasing the chances that the paper will be published in a decent journal.
On this blog, we have seen repeatedly that even top journal occasionally publish rubbish papers. Perhaps they do so because well-intentioned experts react in the way my friend Timothy did above (as he failed to tell us what journal invited him, I might be wrong).
If we want pseudoscience to disappear, we are fighting a lost battle. It will always rear its ugly head in third class journals. This is lamentable, but perhaps not so disastrous: by publishing little else than rubbish, these SCAM journals discredit themselves and will eventually be read only by pseudoscientists.
But we can do our bit to get rid of pseudoscience in decent journals. For this to happen, I think, rational thinkers need to accept invitations from such journals and do a proper review. And, of course, they can add to it a sentence or two about the futility of reviewing nonsense.
I am sure Timothy and I both want to eliminate pseudoscience as much as possible. In other words, we are in agreement about the aim, yet we differ in our approach. The question is: which is more effective?
… Many proponents of so-called alternative medicine (SCAM) are keen to point out that, while mainstream medicine may be good at treatment of diseases, particularly acute conditions, SCAM’s forte lies in the prevention of disease. Patients seem to have intuitively accepted this notion; a recent survey suggest that more than 50% of those Americans who use SCAM do so not to treat ailments but to remain healthy, i.e. to prevent disease and illness. If one looks closer at the evidence for or against SCAM’s role in disease prevention, one is stunned by the contrast of firmly held beliefs and the lack of reliable evidence to support them…
… Unfortunately the subject is more complex than normally appreciated within SCAM. Until we have convincing data, it is not possible to state with confidence that a given form of SCAM is effective in preventing a given condition. It follows
- that we now should prepare to carry out the much needed (but difficult) research related
to preventative, - that we should be cautious and abstain from overstating the largely unproven role of SCAM in the prevention of disease and illness.

These lines were written by me and published exactly 20 years ago. As far as I can see, very little has changed since.
- SCAM providers continue to make big claims about disease prevention.
- Many consumers continue to believe them.
- And the evidence continues to be absent or flimsy.
It follows, I fear, that charlatans who advocate their SCAM as a means to prevent disease are dishonestly defrauding the public.
I do hope that someone disagrees with me and shows me the evidence proving me wrong!
As reported on this blog, the Spanish minister of health want to change the EU law that governs homeopathy. Now the INH has taken action in support of this idea:
THE COMMENT
… the Spanish government … no longer wants to accept the medicinal status of homeopathy, wants to ban homeopathy from pharmacies and has already “discontinued” the first batch of homoeopathics which could not present a valid proof of efficacy upon request. England is currently performing a complete “blacklisting”, i.e. a process that means the end of any registration for homeopathic medication with a drug authority.
The EU Medicines Directive does not regulate in detail how exactly the member states deal with homeopathy in health care. However, it does fix two key points: It includes homeopathy in its definition of a medical drug and obliges the states to regulate a simplified registration procedure for homeopathy instead of the usual drug approval. If one seriously wants to dispute the status of homeopathic medicinal products (and thus their privileges), one cannot completely ignore EU law.
Spain knows that. At various levels (including that of the government), there are efforts to achieve a revision of the EU directive on medicinal products in the field of homeopathy. These efforts need support. The INH has therefore addressed the following letter to German MEPs, which is initially intended to provide basic information on the facts of the case and support Spain’s position in the expected discussion. This seems all the more necessary as the European homeopathic manufacturers and associations have for a long time maintained a lobby organisation directly in Brussels, which apparently has quite good material and personnel resources and whose task is to exert direct influence “on the spot”. We do not have such resources, but we do have the facts. And who knows – perhaps one or the other national government will even join Spain and become active in the EU?
_________________________________________________________________
THE LETTER TO ALL GERMAN MEPs
7 August 2019
Homeopathy in the EU Medicines Directive
Dear Madam / Sir,
The European Medicines Directive (Directive 2001/83/EC of the European Parliament and of the Council of 6 November 2001 on the Community code relating to medicinal products for human use, Official Journal of the European Community L 311, 28.11.2001) classifies homeopathic preparations as medicinal products and requires national governments to establish a simplified registration procedure outside the otherwise prescribed rules for marketing authorisation for pharmaceutical remedies.
However, the consensus of the worldwide scientific community has long since classified homeopathy as a specifically ineffective sham therapy, the spread and “popularity” of which have completely different bases than those of medical relevance (evidence). In many countries, this insight is now gaining acceptance. It will be in the well-understood interest of the public’s health to take consequences of this. The misguiding of the public that homeopathy is a form of therapy expressly recognised by the legislator and therefore endowed with the credit of efficacy and harmlessness may not be continued.
In this respect, the Kingdom of Spain is already campaigning for an amendment to European pharmaceutical law, which not only grants homeopathic preparations the status of medicinal products by definition, but also grants them the additional privilege of registration (see also http://www.europarl.europa.eu/doceo/document/E-8-2018-004948-ASW_EN.html). This special legal framework has no objective justification, as the EASAC – as official advisor to the EU institutions – clearly stated in its statement of 20.09.2017 (https://easac.eu/publications/details/homeopathic-products-and-practices/).
In the interest of a science-based, honest and patient-oriented health policy, also on behalf of the German Consumer Association e.V. and its regional associations, we ask you to support a revision of the Medicines Directive in the sense described, in order to clear the way for appropriate national regulations under Community law.
You can inform yourself about the scientific status of homeopathy on the (multilingual) website of our association: www.network-homeopathy.info .
Yours sincerely
For the Information Network Homeopathy
Dr. Natalie Grams – Dr. Ing. Norbert Aust – Dr. Christian Lübbers
__________________________________________________________________
IF YOU FEEL LIKE SUPPORTING THIS INITIALIVE, PLEASE WRITE TO YOUR MEP.
We have looked at curcumin several (tumeric) times before (see here, here and here). It seems to have a fascinating spectrum of pharmacological activities. But do they translate into clinical usefulness? To answer this question, we obviously need clinical trials. Unfortunately, not many have become available. Here are two recent studies:
Due to the potential benefits of curcumin in the ischemic heart disease, this study was performed to evaluate whether pretreatment with curcumin may reduce myocardial injury following elective percutaneous coronary intervention (PCI). A randomized clinical trial was performed on 110 patients undergoing elective PCI. The intervention group (n = 55) received a single dose of 480 mg nanomicelle curcumin orally and the standard treatment before PCI, while the control group (n = 55) received only the standard treatment., Serum concentrations of CK-MB and troponin I was measured before, 8 and 24 h after the procedure to assess myocardial damage during PCI. The results showed that the raise of CK-MB in curcumin group was half of the control group (4 vs. 8 cases) but was not significant. There were no significant differences in CK-MB levels at 8 (P = .24) and 24 h (P = .37) after PCI between the curcumin and the control group. No significant difference was also found in troponin I levels at 8 (P = 1.0) and 24 h (P = .35) after PCI between the groups. This study did not support the potential cardioprotective benefit of curcumin against pre-procedural myocardial injury in patients undergoing elective PCI.

Ground and mashed turmeric
Inflammation along with oxidative stress has an important role in the pathophysiology of unstable angina which leads to acute myocardial infarction, arrhythmias and eventually heart failure. Curcumin has anti-inflammatory and anti-oxidant effects and thereby, it may reduce cardiovascular complications. This randomized controlled trial aimed to investigate the effects of curcumin on the prevention of atrial and ventricular arrhythmias and heart failure in patients with unstable angina.
Materials and Methods:
Forty patients with unstable angina who met the trial inclusion and exclusion criteria, participated in this double-blind randomized clinical trial. The patients were randomized into two groups: curcumin (80 mg/day for 5days) and placebo (80 mg/day for 5days). Cardiac function was evaluated by two-dimensional echocardiography devices at baseline (immediately after hospitalization) and 5 days after the onset of the trial. Atrial and ventricular arrhythmias were recorded by Holter monitors in cardiology ward, Ghaem academic hospital, Mashhad, Iran. Progression to heart failure, myocardial infarction, and pulmonary and cardiopulmonary resuscitation events as well as mortality were recorded daily throughout the study.
Results:
There were no significant differences between the two groups in atrial and ventricular arrhythmias (p=0.2), and other echocardiographic parameters (Ejection fraction, E, A, E/A ratio, Em, and pulmonary artery pressure) at baseline and five days after the start of the trial.
Conclusion:
Nanocurcumin administered at the dose of 80 mg/day for five days had no effect in the incidence of cardiovascular complications in patients with unstable angina.
Clinical trials are not a good tool for proving a negative; they rarely can prove that a therapy is totally useless. Therefore, we cannot be sure that the many fascinating pharmacological activities of curcumin do not, after all, translate into some clinical benefit. However, what we can say with a high degree of certainty is this: currently there is no good evidence to show that curcumin is effective in treating any human condition.
Perhaps there is a more general lesson here about herbal medicine. Many plants have exiting pharmacological activities such as anti-biotic or anti-cancer activity which can be shown in-vitro. These are then hyped by entrepreneurs and enthusiasts of so-called alternative medicine (SCAM). Such hype fools many consumers and is thus good for business. But in-vitro activity does not necessarily mean that the therapy is clinically useful. There are many reasons for this, e.g. toxicity, lack of absorption. The essential test is always the clinical trial.
IN-VIVO VERITAS!
It is hardly surprising that Gwyneth Paltrow’s obsession with so-called alternative medicine (SCAM) for the vagina is motivating women to try some of it. The consequences can be dramatic; not only for the wallet but also for the vagina!
Vaginal steaming made global headlines in 2015 after its promotion by celebrity Gwyneth Paltrow. One of many female genital modification practices currently on offer in Anglo-Western nations – practices both heavily promoted and critiqued – vaginal steaming is claimed to offer benefits for fertility and overall reproductive, sexual or even general health and wellbeing. We analysed a selection of online accounts of vaginal steaming to determine the sociocultural assumptions and logics within such discourse, including ideas about women, women’s bodies and women’s engagement with such ‘modificatory’ practices. Ninety items were carefully selected from the main types of website discussing vaginal steaming: news/magazines; health/lifestyle; spa/service providers; and personal blogs. Data were analysed using thematic analysis, within a constructionist framework that saw us focus on the constructions and rationalities that underpin the explicit content of the texts. Within an overarching theme of ‘the self-improving woman’ we identified four themes: (1) the naturally deteriorating, dirty female body; (2) contemporary life as harmful; (3) physical optimisation and the enhancement of health; and (4) vaginal steaming for life optimisation. Online accounts of vaginal steaming appear both to fit within historico-contemporary constructions of women’s bodies as deficient and disgusting, and contemporary neoliberal and healthist discourse around the constantly improving subject.
A recent case-report tells a cautionary tale. Here is its abstract:
BACKGROUND:
Vaginal steaming has gained increased popularity as a method to achieve empowerment by providing vaginal tightening and to “freshen” the vagina.
CASE:
A 62-year-old woman sustained second-degree burns following vaginal steaming in an attempt to reduce vaginal prolapse.
CONCLUSION:
Clinicians need to be aware of alternative treatments available to women so that counselling may mitigate any potential harm.
As the full paper is not available to me, I had to rely on another report for further information.
The woman had been suffering from a prolapsed vagina and had been led to believe the vaginal steaming could help avoid surgery. Spas advertising “v-steaming” claim it has been used throughout history in countries in Asia and Africa. They claim the practice, which is sometimes called Yoni steaming, acts to “detox” the vagina, can ease period pains, help with fertility and much more. Experts, however, warn that it can be dangerous and point out that there is no good evidence for the health claims being made.
Dr Vanessa Mackay, a consultant and spokeswoman for the Royal College of Obstetricians and Gynaecologists, says it is a “myth” that the vagina requires extensive cleaning or treatment. She recommends using plain, unperformed soaps on the external vulva area only. “The vagina contains good bacteria, which are there to protect it,” she said in a statement. “Steaming the vagina could affect this healthy balance of bacteria and pH levels and cause irritation, infection (such as bacterial vaginosis or thrush) and inflammation. It could also burn the delicate skin around the vagina (the vulva).”
Dr Magali Robert, who authored the case-report, said the injured woman attempted to steam her vagina on the advice of a traditional Chinese doctor. The woman, who gave permission for her case to be shared, sat over the boiling water for 20 minutes on two consecutive days before presenting at an emergency department with injuries. She sustained second-degree burns and had to delay reconstructive surgery while she healed.
Dr Robert, who works in pelvic medicine and reconstructive surgery in Calgary, said word of unconventional therapies like steaming can spread through channels like the internet and word-of-mouth. “Health care providers need to be aware of alternative therapies so that they can help women make informed choices and avoid potential harm,” she says in the article.
Many so-called alternative medicine (SCAM) traditions have their very own diagnostic techniques, unknown to conventional clinicians. Think, for instance, of:
- iridology,
- applied kinesiology,
- tongue diagnosis,
- pulse diagnosis,
- Kirlean photography,
- live blood cell analysis,
- the Vega test,
- dowsing.
(Those interested in more detail can find a critical assessment of these and other diagnostic SCAM methods in my new book.)
And what about homeopathy?
Yes, homeopathy is also a diagnostic method.
Let me explain.
According to Hahnemann’s classical homeopathy, the homeopath should not be interested in conventional diagnostic labels. Instead, classical homeopaths are focussed on the symptoms and characteristics of the patient. They conduct a lengthy history to learn all about them, and they show little or no interest in a physical examination of their patient or other diagnostic procedures. Once they are confident to have all the information they need, they try to find the optimal homeopathic remedy.
This is done by matching the symptoms with the drug pictures of homeopathic remedies. Any homeopathic drug picture is essentially based on what has been noted in homeopathic provings where healthy volunteers take a remedy and monitor all that symptoms, sensations and feelings they experience subsequently. Here is an example:
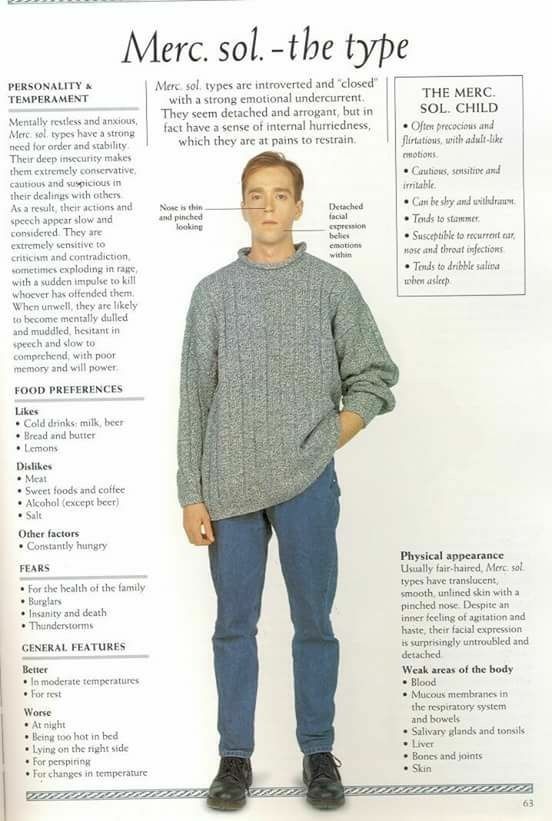 The perfect match is what homeopaths thrive to find with their long and tedious procedure of taking a history. And the perfectly matching homeopathic remedy is essentially the homeopathic diagnosis.
The perfect match is what homeopaths thrive to find with their long and tedious procedure of taking a history. And the perfectly matching homeopathic remedy is essentially the homeopathic diagnosis.
Now, here is the thing: most SCAM diagnostic techniques have been tested (and found to be useless), but homeopathy as a diagnostic tool has – as far as I know – never been submitted to any rigorous tests (if you know otherwise, please let me know). And this, of course, begs an important question: is it right – ethical, legal, moral – to use homeopathy without such evidence being available?
The simplest such test would be quite easy to conduct: one would send the same patient to 10 or 20 experienced homeopaths and see how many of them prescribe the same remedy.
Simple! But I shudder to think what such an experiment might reveal.