Monthly Archives: December 2022
Yesterday, the post brought me a nice Christmas present. For many months, I had been working on updating and extending a book of mine. Then there were some delays at the publisher, but now it is out – what a delight!
The previous edition contained my evidence-based assessments of 150 alternative modalities (therapies and diagnostic techniques). This already was by no means an easy task. The new edition has 202 short, easy-to-understand, and fully-referenced chapters, each on a different modality. I am quite proud of the achievement. Let me just show you the foreword to the new edition:
Alternative medicine is full of surprises. For me, a big surprise was that the first edition of this book was so successful that I was invited to do a second one. I do this, of course, with great pleasure.
So, what is new? I have made two main alterations. Firstly, I updated the previous text by adding new evidence where it had emerged. Secondly, I added many more modalities—52, to be exact.
To the best of my knowledge, this renders the new edition of this book the most comprehensive reference text on alternative medicine available to date. It informs you about the nature, proven benefits, and potential risks of 202 different diagnostic methods and therapeutic interventions from the realm of so-called alternative medicine. If you use this information wisely, it could save you a lot of money. One day, it might even save your life.
I hope you enjoy using this book as much as I enjoyed writing it.
Like the first edition, the book is not about promoting so-called alternative medicine (SCAM) nor about the opposite. It is about evaluating SCAM critically but fairly. In other words, each subject had to be researched and the evidence for or against it explained such that a layperson will comprehend it. This proved to be a colossal task.
The end result will not please the many believers in SCAM, I am afraid. Yet, I hope it will suit those who realize that, in healthcare, progress is generated not through belief but through critical evaluation of the evidence.
Earlier this year, I started the ‘WORST PAPER OF 2022 COMPETITION’. As a prize, I am offering the winner (that is the lead author of the winning paper) one of my books that best fits his/her subject. I am sure this will overjoy him or her. I hope to identify about 10 candidates for the prize, and towards the end of the year, I let my readers decide democratically on who should be the winner. In this spirit of democratic voting, let me suggest to you entry No 9. Here is the unadulterated abstract:
Background
With the increasing popularity of traditional Chinese medicine (TCM) by the global community, how to teach basic knowledge of TCM to international students and improve the teaching quality are important issues for teachers of TCM. The present study was to analyze the perceptions from both students and teachers on how to improve TCM learning internationally.
Methods
A cross-sectional national survey was conducted at 23 universities/colleges across China. A structured, self-reported on-line questionnaire was administered to 34 Chinese teachers who taught TCM course in English and to 1016 international undergraduates who were enrolled in the TCM course in China between 2017 and 2021.
Results
Thirty-three (97.1%) teachers and 900 (88.6%) undergraduates agreed Chinese culture should be fully integrated into TCM courses. All teachers and 944 (92.9%) undergraduates thought that TCM had important significance in the clinical practice. All teachers and 995 (97.9%) undergraduates agreed that modern research of TCM is valuable. Thirty-three (97.1%) teachers and 959 (94.4%) undergraduates thought comparing traditional medicine in different countries with TCM can help the students better understand TCM. Thirty-two (94.1%) teachers and 962 (94.7%) undergraduates agreed on the use of practical teaching method with case reports. From the perceptions of the undergraduates, the top three beneficial learning styles were practice (34.3%), teacher’s lectures (32.5%), case studies (10.4%). The first choice of learning mode was attending to face-to-face teaching (82.3%). The top three interesting contents were acupuncture (75.5%), Chinese herbal medicine (63.8%), and massage (55.0%).
Conclusion
To improve TCM learning among international undergraduates majoring in conventional medicine, integration of Chinese culture into TCM course, comparison of traditional medicine in different countries with TCM, application of the teaching method with case reports, and emphasization of clinical practice as well as modern research on TCM should be fully considered.
I am impressed with this paper mainly because to me it does not make any sense at all. To be blunt, I find it farcically nonsensical. What precisely? Everything:
- the research question,
- the methodology,
- the conclusion
- the write-up,
- the list of authors and their affiliations: Department of Chinese Integrative Medicine, Women’s Hospital, School of Medicine, Zhejiang University, Hangzhou, China, Department of Traditional Chinese Medicine, School of Basic Medicine, Qingdao University, Qingdao, China, Department of Chinese Integrative Medicine, The Second Affiliated Hospital of Kunming Medical University, Kunming, China, Department of Traditional Chinese Medicine, The Affiliated Hospital of Xuzhou Medical University, Xuzhou, China, Department of Traditional Chinese Medicine, Medical College, China Three Gorges University, Yichang, China, Basic Teaching and Research Department of Acupuncture and Moxibustion, College of Traditional Chinese Medicine, Xinjiang Medical University, Urumqi, China, Institute of Integrative Medicine, Dalian Medical University, Dalian, China, Department of Chinese and Western Medicine, Chongqing Medical University, Chongqing, China, Department of Chinese and Western Medicine, North Sichuan Medical College, Nanchong, China, Department of Chinese and Western Medicine, School of Medicine, Xiamen University, Xiamen, China, School of Traditional Chinese Medicine, Capital Medical University, Beijing, China, School of Traditional Chinese Medicine, Southern Medical University, Guangzhou, China, Department of Traditional Chinese Medicine, The First Affiliated Hospital of Soochow University, Suzhou, China, Department of Traditional Chinese Medicine, School of Medicine, Xiamen University, Xiamen, China, Department of Chinese Medicine/Department of Chinese Integrative Medicine, The First Affiliated Hospital of Anhui Medical University, Hefei, China, Department of Traditional Chinese Medicine, Shengjing Hospital Affiliated to China Medical University, Shenyang, China, Department of Acupuncture, Affiliated Hospital of Jiangsu University, Zhenjiang, China, Teaching and Research Section of Traditional Chinese Medicine, The Second Affiliated Hospital of Soochow University, Suzhou, China, Department of Traditional Chinese Medicine, The Second Affiliated Hospital of Harbin Medical University, Harbin, China, Department of Chinese Medicine, The First Affiliated Hospital of Anhui Medical University, Hefei, China, Department of Chinese Medicine, The First Affiliated Hospital of Kunming Medical University, Kunming, China, Department of Traditional Chinese Medicine, Shengli Clinical Medical College of Fujian Medical University, Fuzhou, China, Department of Chinese Medicine, The First Affiliated Hospital of Jinzhou Medicine University, Jinzhou, China, Department of Integrated Traditional and Western Medicine, The First Affiliated Hospital of Harbin Medical University, Harbin, China, Department of Chinese Medicine, The Second Affiliated Hospital of Guangzhou Medical University, Guangzhou, China, Department of Traditional Chinese Medicine, The First Affiliated Hospital of Fujian Medical University, Fuzhou, China.
- the journal that had this paper peer-reviewed and published.
But what impressed me most with this paper is the way the authors managed to avoid even the slightest hint of critical thinking. They even included a short paragraph in the discussion section where they elaborate on the limitations of their work without ever discussing the true flaws in the conception and execution of this extraordinary example of pseudoscience.
Is acupuncture more than a theatrical placebo? Acupuncture fans are convinced that the answer to this question is YES. Perhaps this paper will make them think again.
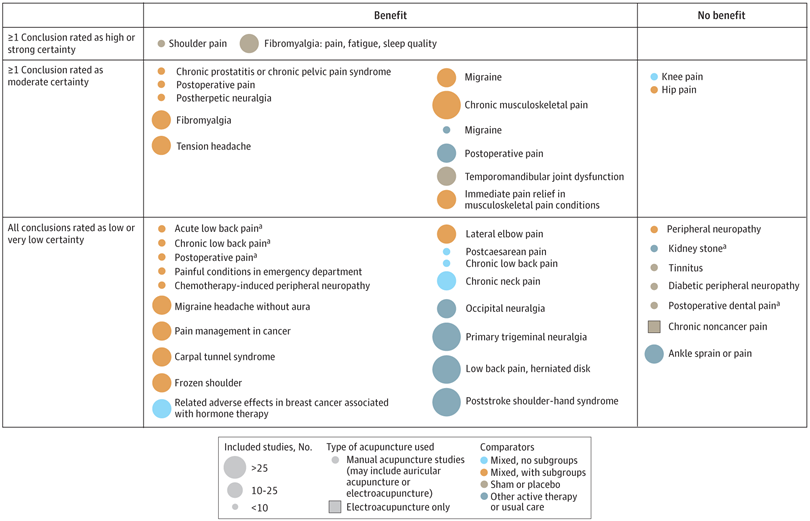
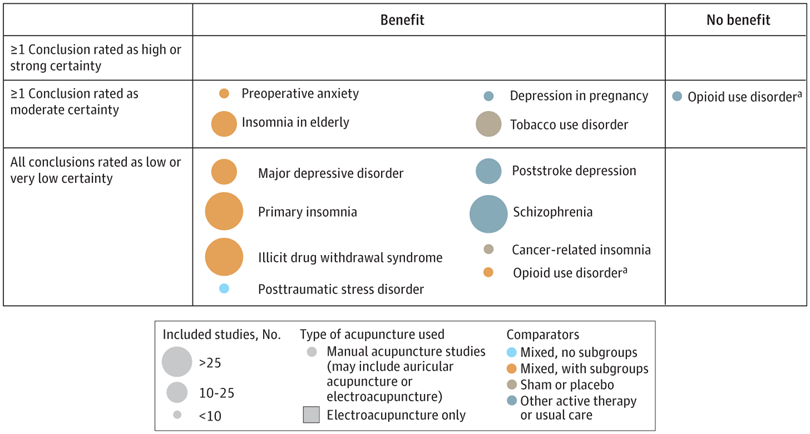
A new analysis mapped the systematic reviews, conclusions, and certainty or quality of evidence for outcomes of acupuncture as a treatment for adult health conditions. Computerized search of PubMed and 4 other databases from 2013 to 2021. Systematic reviews of acupuncture (whole body, auricular, or electroacupuncture) for adult health conditions that formally rated the certainty, quality, or strength of evidence for conclusions. Studies of acupressure, fire acupuncture, laser acupuncture, or traditional Chinese medicine without mention of acupuncture were excluded. Health condition, number of included studies, type of acupuncture, type of comparison group, conclusions, and certainty or quality of evidence. Reviews with at least 1 conclusion rated as high-certainty evidence, reviews with at least 1 conclusion rated as moderate-certainty evidence and reviews with all conclusions rated as low- or very low-certainty evidence; full list of all conclusions and certainty of evidence.
A total of 434 systematic reviews of acupuncture for adult health conditions were found; of these, 127 reviews used a formal method to rate the certainty or quality of evidence of their conclusions, and 82 reviews were mapped, covering 56 health conditions. Across these, there were 4 conclusions that were rated as high-certainty evidence and 31 conclusions that were rated as moderate-certainty evidence. All remaining conclusions (>60) were rated as low- or very low-certainty evidence. Approximately 10% of conclusions rated as high or moderate-certainty were that acupuncture was no better than the comparator treatment, and approximately 75% of high- or moderate-certainty evidence conclusions were about acupuncture compared with a sham or no treatment.
Three evidence maps (pain, mental conditions, and other conditions) are shown below
The authors concluded that despite a vast number of randomized trials, systematic reviews of acupuncture for adult health conditions have rated only a minority of conclusions as high- or moderate-certainty evidence, and most of these were about comparisons with sham treatment or had conclusions of no benefit of acupuncture. Conclusions with moderate or high-certainty evidence that acupuncture is superior to other active therapies were rare.
These findings are sobering for those who had hoped that acupuncture might be effective for a range of conditions. Despite the fact that, during recent years, there have been numerous systematic reviews, the evidence remains negative or flimsy. As 34 reviews originate from China, and as we know about the notorious unreliability of Chinese acupuncture research, this overall result is probably even more negative than the authors make it out to be.
Considering such findings, some people (including the authors of this analysis) feel that we now need more and better acupuncture trials. Yet I wonder whether this is the right approach. Would it not be better to call it a day, concede that acupuncture generates no or only relatively minor effects, and focus our efforts on more promising subjects?
An international team of researchers described retracted papers originating from paper mills, including their characteristics, visibility, and impact over time, and the journals in which they were published. The term paper mill refers to for-profit organizations that engage in the large-scale production and sale of papers to researchers, academics, and students who wish to, or have to, publish in peer-reviewed journals. Many paper mill papers included fabricated data.
All paper mill papers retracted from 1 January 2004 to 26 June 2022 were included in the study. Papers bearing an expression of concern were excluded. Descriptive statistics were used to characterize the sample and analyze the trend of retracted paper mill papers over time, and to analyze their impact and visibility by reference to the number of citations received.
In total, 1182 retracted paper mill papers were identified. The publication of the first paper mill paper was in 2004 and the first retraction was in 2016; by 2021, paper mill retractions accounted for 772 (21.8%) of the 3544 total retractions. Overall, retracted paper mill papers were mostly published in journals of the second highest Journal Citation Reports quartile for impact factor (n=529 (44.8%)) and listed four to six authors (n=602 (50.9%)). Of the 1182 papers, almost all listed authors of 1143 (96.8%) paper mill retractions came from Chinese institutions, and 909 (76.9%) listed a hospital as a primary affiliation. 15 journals accounted for 812 (68.7%) of 1182 paper mill retractions, with one journal accounting for 166 (14.0%). Nearly all (n=1083, 93.8%) paper mill retractions had received at least one citation since publication, with a median of 11 (interquartile range 5-22) citations received.
The authors concluded that papers retracted originating from paper mills are increasing in frequency, posing a problem for the research community. Retracted paper mill papers most commonly originated from China and were published in a small number of journals. Nevertheless, detected paper mill papers might be substantially different from those that are not detected. New mechanisms are needed to identify and avoid this relatively new type of misconduct.
China encourages its researchers to publish papers in return for money and career promotions. Furthermore, medical students at Chinese universities are required to produce a scientific paper in order to graduate. Paper mills openly advertise their services on the Internet and maintain a presence on university campuses. The authors of this analysis reference another recent article (authored by two Chinese researchers) that throws more light on the problem:
This study used data from the Retraction Watch website and from published reports on retractions and paper mills to summarize key features of research misconduct in China. Compared with publicized cases of falsified or fabricated data by authors from other countries of the world, the number of Chinese academics exposed for research misconduct has increased dramatically in recent years. Chinese authors do not have to generate fake data or fake peer reviews for themselves because paper mills in China will do the work for them for a price. Major retractions of articles by authors from China were all announced by international publishers. In contrast, there are few reports of retractions announced by China’s domestic publishers. China’s publication requirements for physicians seeking promotions and its leniency toward research misconduct are two major factors promoting the boom of paper mills in China.
As the authors of the new analysis point out: “Fraudulent papers have negative consequences for the scientific community and the general public, engendering distrust in science, false claims of drug or device efficacy, and unjustified academic promotion, among other problems.” On this blog, I have often warned of research originating from China (some might even think that this is becoming an obsession of mine but I do truly think that this is very important). While such fraudulent papers may have a relatively small impact in many areas of healthcare, their influence in the realm of TCM (where the majority of research comes from China) is considerable. In other words, TCM research is infested by fraud to a degree that prevents drawing meaningful conclusions about the value of TCM treatments.
I feel strongly that it is high time for us to do something about this precarious situation. Otherwise, I fear that in the near future no respectable scientist will take TCM seriously.
It has been reported that a naturopath from the US who sold fake COVID-19 immunization treatments and fraudulent vaccination cards during the height of the coronavirus pandemic has been sentenced to nearly three years in prison. Juli A. Mazi pleaded guilty last April in federal court in San Francisco to one count of wire fraud and one count of false statements related to health care matters. Now District Judge Charles R. Breyer handed down a sentence of 33 months, according to Joshua Stueve, a spokesperson for the U.S. Department of Justice. Mazi, of Napa, was ordered to surrender to the Bureau of Prisons on or before January 6, 2023.
The case is the first federal criminal fraud prosecution related to fraudulent Centers for Disease Control and Prevention vaccination cards for COVID-19, according to the U.S. Department of Justice. In August, Breyer denied Mazi’s motion to withdraw her plea agreement after she challenged the very laws that led to her prosecution. Mazi, who fired her attorneys and ended up representing herself, last week filed a letter with the court claiming sovereign immunity. Mazi said that as a Native American she is “immune to legal action.”
She provided fake CDC vaccination cards for COVID-19 to at least 200 people with instructions on how to complete the cards to make them look like they had received a Moderna vaccine, federal prosecutors said. She also sold homeopathic pellets she fraudulently claimed would provide “lifelong immunity to COVID-19.” She told customers that the pellets contained small amounts of the virus and would create an antibody response. Mazi also offered the pellets in place of childhood vaccinations required for attendance at school and sold at least 100 fake immunization cards that said the children had been vaccinated, knowing the documents would be submitted to schools, officials said. Federal officials opened an investigation against Mazi after receiving a complaint in April 2021 to the Department of Health and Human Services Office of Inspector General hotline.
_______________________
On her website, Mazi states this about herself:
Juli Mazi received her doctorate in Naturopathic Medicine from the National University of Natural Medicine in Portland, Oregon where she trained in the traditional medical sciences as well as ancient and modern modalities that rely on the restorative power of Nature to heal. Juli Mazi radiates the vibrant health she is committed to helping her patients achieve. Juli’s positive outlook inspires confidence; her deep well of calm puts people at immediate ease. The second thing they notice is that truly she listens. Dr. Mazi’s very presence is healing.
On this site, she also advocates all sorts of treatments and ideas which I would call more than a little strange, for instance, coffee enemas:
Using a coffee enema is a time-tested remedy for detoxification, but it is not without risks. If you are not careful, the process can cause internal burns. In addition, improperly brewed coffee can lead to electrolyte imbalances and dehydration, and coffee enemas are not recommended for pregnant women or young children.
To make coffee enemas safe and effective, always choose quality organic coffee. A coffee enema should be free of toxins and pesticides. Use a reusable enema kit with stainless steel or silicone hosing for safety. Moreover, do not use a soft plastic or latex enema bags. It is also essential to limit the length of time that the coffee spends in the container.
A coffee enema should be held for 12 to 15 minutes and then released in the toilet. You may repeat the process as necessary. Usually, the procedure should be done once or twice a day. However, if you are experiencing acute toxicity, you can use a coffee enema as often as needed. Make sure you have had a bowel movement before making the coffee enema. Otherwise, the process may be hindered.
Perhaps the most interesting thing on her website is her advertisement of the fact that her peers not just tolerate such eccentricities but gave Mazi an award for ‘BEST ALTERNATIVE HEALTH & BEST GENERAL PRACTITIONER’.
To me, this suggests that US ‘doctors of naturopathy’ and their professional organizations live on a different planet, a planet where evidence counts for nothing and dangerously misleading patients seems to be the norm.
I know, I have often posted nasty things about integrative medicine and those who promote it. Today, I want to make good for all my sins and look at the bright side.
Imagine you are a person convinced of the good that comes from so-called alternative medicine (SCAM). Imagine you believe it has stood the test of time, is natural, holistic, tackles the root problems of illness, etc., etc. Imagine you are such a person.
Your convictions made you support more research into SCAM because you feel that evidence is needed for it to be more generally accepted. So, you are keen to see more studies proving the efficacy of this or that SCAM in the management of this or that condition.
This, unfortunately, is where the problems start.
Not only is there not a lot of money and even fewer scientists to do this research, but the amount of studies that would need doing is monstrously big:
- There are hundreds of different types of SCAM.
- Each SCAM is advocated for hundreds of conditions.
Consequently, tens of thousands of studies are needed to only have one trial for each specific research question. This is tough for a SCAM enthusiast! It means he/she has to wait decades to see the light at the end of the tunnel.
But then it gets worse – much worse!
As the results of these studies come in, one after the other, you realize that most of them are not at all what you have been counting on. Many can be criticized for being of dismal quality and therefore inconclusive, and those that are rigorous tend to be negative.
Bloody hell! There you have been waiting patiently for decades and now you must realize that this wait did not take you anywhere near the goal that was so clear in your sight. Most reasonable people would give up at this stage; they would conclude that SCAM is a pipedream and direct their attention to something else. But not you! You are single-minded and convinced that SCAM is the future. Some people might even call you obsessed – obsessed and desperate.
It is out of this sense of desperation that the idea of integrative medicine was born. It is a brilliant coup that solves most of the insurmountable problems outlined above. All you need to do is to take the few positive findings that did emerge from the previous decades of research, find a political platform, and loudly proclaim:
SCAM does work.
Consumers like SCAM.
SCAM must be made available to all.
Consumers deserve the best of both worlds.
The future of healthcare evidently lies in integrated medicine.
Forgotten are all those irritating questions about the efficacy of this or that treatment. Now, it’s all about the big issue of wholesale integration of SCAM. Forgotten is the need for evidence – after all, we had decades of that! – now, the issue is no longer scientific, it is political.
And if anyone has the audacity to ask about evidence, he/she can be branded as a boring nit-picker. And if anyone doubts the value of integrated medicine, he/she will be identified as a politically incorrect dinosaur.
Mission accomplished!