Low back pain (LBP) is influenced by interrelated biological, psychological, and social factors, however current back pain management is largely dominated by one-size fits all unimodal treatments. Team based models with multiple provider types from complementary professional disciplines is one way of integrating therapies to address patients’ needs more comprehensively.
This parallel-group randomized clinical trial conducted from May 2007 to August 2010 aimed to evaluate the relative clinical effectiveness of 12 weeks of monodisciplinary chiropractic care (CC), versus multidisciplinary integrative care (IC), for adults with sub-acute and chronic LBP. The primary outcome was pain intensity and secondary outcomes were disability, improvement, medication use, quality of life, satisfaction, frequency of symptoms, missed work or reduced activities days, fear-avoidance beliefs, self-efficacy, pain coping strategies, and kinesiophobia measured at baseline and 4, 12, 26 and 52 weeks. Linear mixed models were used to analyze outcomes.
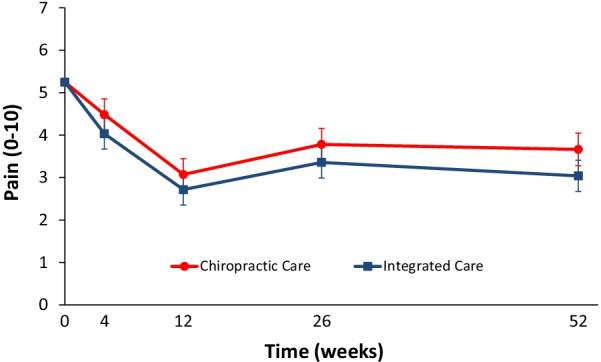
In total, 201 participants were enrolled. The largest reductions in pain intensity occurred at the end of treatment and were 43% for CC and 47% for IC. The primary analysis found IC to be significantly superior to CC over the 1-year period (P = 0.02). The long-term profile for pain intensity which included data from weeks 4 through 52, showed a significant advantage of 0.5 for IC over CC (95% CI 0.1 to 0.9; P = 0.02; 0 to 10 scale). The short-term profile (weeks 4 to 12) favored IC by 0.4, but was not statistically significant (95% CI – 0.02 to 0.9; P = 0.06). There was also a significant advantage over the long term for IC in some secondary measures (disability, improvement, satisfaction, and low back symptom frequency), but not for others (medication use, quality of life, leg symptom frequency, fear-avoidance beliefs, self-efficacy, active pain coping, and kinesiophobia). No serious adverse events resulted from either of the interventions.
The authors concluded that participants in the IC group tended to have better outcomes than the CC group, however, the magnitude of the group differences was relatively small. Given the resources required to successfully implement multidisciplinary integrative care teams, they may not be worthwhile, compared to monodisciplinary approaches like chiropractic care, for treating LBP.
The obvious question is: what were the exact treatments used in both groups? The authors provide the following explanations:
All participants in the study received 12 weeks of either monodisciplinary chiropractic care (CC) or multidisciplinary team-based integrative care (IC). CC was delivered by a team of chiropractors allowed to utilize any non-proprietary treatment under their scope of practice not shown to be ineffective or harmful including manual spinal manipulation (i.e., high velocity, low amplitude thrust techniques, with or without the assistance of a drop table) and mobilization (i.e., low velocity, low amplitude thrust techniques, with or without the assistance of a flexion-distraction table). Chiropractors also used hot and cold packs, soft tissue massage, teach and supervise exercise, and administer exercise and self-care education materials at their discretion. IC was delivered by a team of six different provider types: acupuncturists, chiropractors, psychologists, exercise therapists, massage therapists, and primary care physicians, with case managers coordinating care delivery. Interventions included acupuncture and Oriental medicine (AOM), spinal manipulation or mobilization (SMT), cognitive behavioral therapy (CBT), exercise therapy (ET), massage therapy (MT), medication (Med), and self-care education (SCE), provided either alone or in combination and delivered by their respective profession. Participants were asked not to seek any additional treatment for their back pain during the intervention period. Standardized forms were used to document the details of treatment, as well as adverse events. It was not possible to blind patients or providers to treatment due to the nature of the study interventions. Patients in both groups received individualized care developed by clinical care teams unique to each intervention arm. Care team training was conducted to develop and support group dynamics and shared clinical decision making. A clinical care pathway, designed to standardize the process of developing recommendations, guided team-based practitioner in both intervention arms. Evidence based treatment plans were based on patient biopsychosocial profiles derived from the history and clinical examination, as well as baseline patient rated outcomes. The pathway has been fully described elsewhere [23]. Case managers facilitated patient care team meetings, held weekly for each intervention group, to discuss enrolled participants and achieve treatment plan recommendation consensus. Participants in both intervention groups were presented individualized treatment plan options generated by the patient care teams, from which they could choose based on their preferences.
This is undoubtedly an interesting study. It begs many questions. The two that puzzle me most are:
- Why publish the results only 12 years after the trial was concluded? The authors provide a weak explanation, but I would argue that it is unethical to sit on a publicly funded study for so long.
- Why did the researchers not include a third group of patients who were treated by their GP like in normal routine?
The 2nd question is, I think, important because the findings could mostly be a reflection of the natural history of LBP. We can probably all agree that, at present, the optimal treatment for LBP has not been found. To me, the results look as though they indicate that it hardly matters how we treat LBP, the outcome is always very similar. If we throw the maximum amount of care at it, the results tend to be marginally better. But, as the authors admit, there comes a point where we have to ask, is it worth the investment?
Perhaps the old wisdom is not entirely wrong (old because I learned it at medical school some 50 years ago): make sure LBP patients keep as active as they can while trying to ignore their pain as best as they can. It’s not a notion that would make many practitioners of so-called alternative medicine (SCAM) happy – LBP is their No 1 cash cow! – but it would surely save huge amounts of public expenditure.

Your last advice is true and wise for most simple cases. I normally tell patients to wait 6 weeks before seeking care. On the other hand you have the pain specialists advising on intense early care prior to brain functional modulation in response to pain… more mud in the water
Basically what they found is that adding acupuncturists, psychologists, exercise therapists, massage therapists, and primary care physicians, with case managers coordinating care delivery in addition to chiropractic care doesn’t add much or any clinically significant change (but will add cost, risk and time) for subacute or chronic back pain.
I suppose this is to be expected since it appears to be a A+B design (kind of, as there is some overlap of services)
So, go to six providers or just one…a chiropractor?
“…make sure LBP patients keep as active as they can…”
Yes, often that is the goal. The question is….what, if any, interventions can help in that goal, or put another way, what is keeping the patient from being active? But that question is beyond the purpose of this blog.
“I suppose this is to be expected since”
REALLY?
if you expect this, why then do you add treatments other than manipulation to your therapeutic repertoire?
“it appears to be a A+B design (kind of, as there is some overlap of services)”
you might mean the ‘A+B vs B’ design
the thing about it that it ALWAYS generates a positive result which does not fit to you stating it “doesn’t add much or any clinically significant change”
“I suppose this is to be expected since”
REALLY?
if you expect this, why then do you add treatments other than manipulation to your therapeutic repertoire?
Research is showing that manual therapy plus exercise is better than either one alone. If research reveals that adding something else has additional benefit it should be added as the case indicates.
“it appears to be a A+B design (kind of, as there is some overlap of services)”
you might mean the ‘A+B vs B’ design
the thing about it that it ALWAYS generates a positive result which does not fit to you stating it “doesn’t add much or any clinically significant change”
Not really. Doing too much can have a negative effect and/or adding an intervention that negates or reverses a positive intervention.
“Doing too much can have a negative effect and/or adding an intervention that negates or reverses a positive intervention.”
which, of course, has nothing to do with the study named design.
It had to do with your comment:
“the thing about it that it ALWAYS generates a positive result.”
except that you quoted A+B BEFORE I commented.
OK, let’s go with your comment:
you might mean the ‘A+B vs B’ design
the thing about it that it ALWAYS generates a positive result
If this is true, the positive findings from the addition of these other interventions to CC were probably not due to the other interventions. Thus it appears they added no additional benefit.
are you daft?
they DID generate sign benefit!
just not very much
EE: they DID generate sign benefit!
yes, but was it simply because of the design of the study? You can’t seem to make up your mind.
EE: they DID generate sign benefit!
Now look at which ones were clinically significant.
Start with primary outcome of low back pain intensity (hint, Table 3)
thank you:
The long-term profile for pain intensity (0–10) which included data from weeks 4 through 52, showed a significant advantage of 0.5 for IC over CC (95% CI 0.1 to 0.9; P = 0.02)
“These findings suggest that the minimum clinically significant difference in patient-assigned NRS-11 pain scores is 1.41 (SD±1.05; 95% CI 1.28 to 1.54). Studies that report a change of less than 1.41 points may indicate statistical significance, but the findings may not have clinical significance.” Annals of Emergency Medicine Volume 44, Issue 4, Supplement, October 2004, Pages S86-S87.
thanks for confirming that you were mistaken. not easy for a chiro, I know.
Elaborate on what you think was my mistake regarding clinical significance.
Somebody has found a use for chiropractic at last. As its benefits are largely indistinguishable from placebo, it can be used as the placebo control in studies that want to assess the effectiveness of other interventions.
One cannot come to that conclusion using this paper.