This study investigated whether vitamin D and marine-derived long-chain omega 3 fatty acids reduce autoimmune disease risk. A nationwide, randomized, double-blind, placebo-controlled trial with a two-by-two factorial design was conducted in the US. In total, 25 871 participants (12 786 men ≥50 years and 13 085 women ≥55 years at enrollment) took part.
Participants were given
- vitamin D (2000 IU/day),
- matched placebo,
- omega 3 fatty acids (1000 mg/day),
- matched placebo.
Participants self-reported all incident autoimmune diseases from baseline to a median of 5.3 years of follow-up; these diseases were confirmed by extensive medical record review. Cox proportional hazard models were used to test the effects of vitamin D and omega 3 fatty acids on autoimmune disease incidence. The primary endpoint was all incident autoimmune diseases confirmed by medical record review: rheumatoid arthritis, polymyalgia rheumatica, autoimmune thyroid disease, psoriasis, and all others.
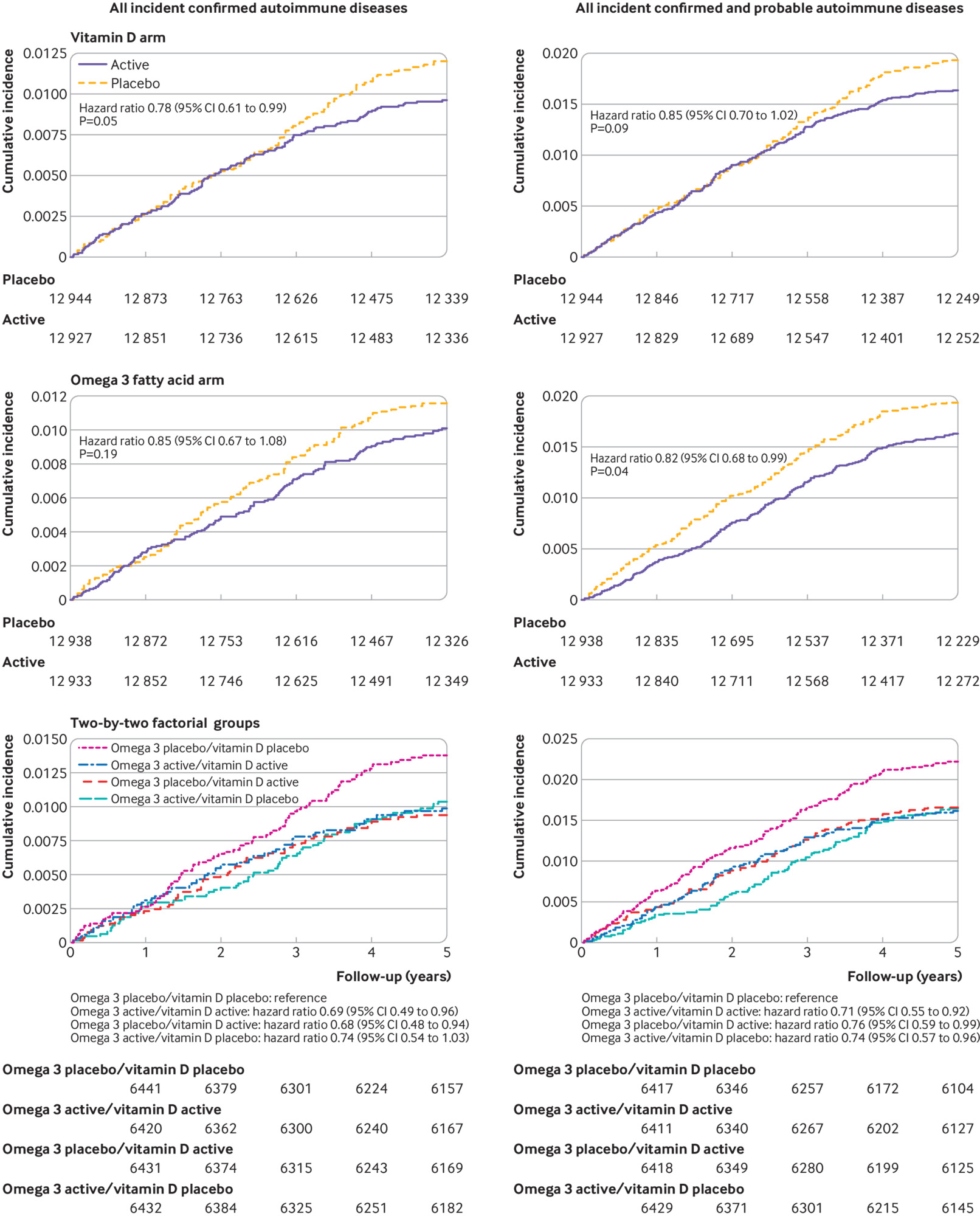
Participants were followed for a median of 5.3 years. 18 046 self-identified as non-Hispanic white, 5106 as black, and 2152 as other racial and ethnic groups. The mean age was 67.1 years. For the vitamin D arm, 123 participants in the treatment group and 155 in the placebo group had a confirmed autoimmune disease (hazard ratio 0.78, 95% confidence interval 0.61 to 0.99, P=0.05). In the omega 3 fatty acids arm, 130 participants in the treatment group and 148 in the placebo group had a confirmed autoimmune disease (0.85, 0.67 to 1.08, P=0.19). Compared with the reference arm (vitamin D placebo and omega 3 fatty acid placebo; 88 with confirmed autoimmune disease), 63 participants who received vitamin D and omega 3 fatty acids (0.69, 0.49 to 0.96), 60 who received only vitamin D (0.68, 0.48 to 0.94), and 67 who received only omega 3 fatty acids (0.74, 0.54 to 1.03) had confirmed autoimmune disease.
The authors concluded that vitamin D supplementation for five years, with or without omega 3 fatty acids, reduced autoimmune disease by 22%, while omega 3 fatty acid supplementation with or without vitamin D reduced the autoimmune disease rate by 15% (not statistically significant). Both treatment arms showed larger effects than the reference arm (vitamin D placebo and omega 3 fatty acid placebo).
This is the best trial of dietary supplements that I have seen for a very long time. Yet, the authors caution: Because participants were older adults, the results might not generalize to autoimmune diseases that primarily have their onset in younger people. However, the pathogenesis of many of the specific autoimmune diseases observed (eg, rheumatoid arthritis and psoriasis) is similar in younger adults. The trial tested only one dose and formulation of each supplement. The relatively low number of participants with a confirmed diagnosis of most individual diseases, and the challenge of confirming diagnosis of autoimmune thyroid disease based on medical records, limited statistical power to detect an effect on individual disease outcomes and subgroups of a priori interest. Given the latency of autoimmune disease onset, longer follow-up could be informative, and participants are being followed in an open label extension study.
As regular readers know, I am not easily impressed – but today I am.

Not bad. Ideal would be to have vit d blood levels checked and be dosed to ideal levels. But of course it woulld be a lot harder to placebo control such a study.
In the UK, GP’s are advised NOT to test serum 25(OH)D levels unless they suspect there is a risk of rickets or other serious bone disorder. And because of this outdated and medically negligent ‘Government Approved’ attitude, many millions of folks are deficient in this multi-tasking, immunomodulating pre-hormone.
For the record, I maintain a minimum serum level of appx 140 nmol/L. Some years ago a GP in private practice warned me that my level was too high and in her words ‘”dangerously toxic.”
At the young age of 75 I would be highly embarrassed if I ever suffered a sore throat, never mind a viral infection. Concerned about your health? Time to get real as they say.
Dear Edzard, yes an interesting study …. but wait a moment! You might be in danger of softening your attitude towards those dreaded SCAM artists, even though Omega-3 fatty acids are considered by many alternative practitioners as being essential for our general wellbeing – including our immunity. I’m confused dot com.
” I’m confused dot com.”
I know, you’ve given plenty of evidence for that
i don’t think that anybody has said that Omega 3 fatty acids are not important for wellbeing, simply that so far there has been no evidence to support that contention, and that it is unsafe to promote any kind of health intervention in the absence of evidence. This new study constitutes evidence. Though its findings should not be unduly extrapolated.
The marker to observe with omega 3 requirements is the ratio to omega 6 intake. The more omega 6 intake, the more omega 3 is required to counter the omega 6 and maintain good health. Omega 6 fatty acids are inflammatory.
https://pubmed.ncbi.nlm.nih.gov/12442909/
Thank you for posting this!
I remember how vitamin D levels were talked about in the beginning of the pandemic. Seemed to have a role in hospitalization rate
Hmm p=0.05 corresponds to a false positive risk of 20 – 30% for an unbiased, well-powered comparison. In fact if the sample is very big, p=0.05 can even provide strong evidence for the null hypothesis (the Jeffreys-Lindley effect). Observing p=0.05 in an experiment with such a large number o people is profoundly unimpressive.
References
https://royalsocietypublishing.org/doi/10.1098/rsos.171085
and
https://www.tandfonline.com/doi/full/10.1080/00031305.2018.1529622
yes, the findings are not fully convincing,
but the study is excellent and exceptional, I think.
Well it seems to have been well-designed but badly analysed. The results could very easily have arisen by chance alone. The myth that p=0.05 enables you to claim a discovery dies very hard.
I get email alerts from New Scientist magazine, which I formerly subscribed to. Yesterday’s email alert highlighted this Study, so I’m pleased to see it commented upon here. I started taking a vitamin D3 supplement a few months ago, after reading one of the medical columns in a credible newspaper or magazine (I forget which) written by a very rational-toned GP who said that he took it. There was some suggestion floating around, some time ago, about a connection between low hours of quality sunlight in Scotland leading to lower levels of Vitamin D, and the high incidence here of Multiple Sclerosis.
The NHS website recommends taking a vitamin D supplement during the winter months so no need to wait for a medical columnist to write about it:
https://www.nhs.uk/conditions/vitamins-and-minerals/vitamin-d/
of course, our loony friends would probably dismiss this advice as “government approved” and ignore it on principle.
That’s interesting. Thank you, Zebra.
I worked in the Middle East for a year, and I miss the Saudi sunshine!
David,
I am a few weeks behind with New Scientist at the moment so I haven’t read what they have to say about this. However, I find that they aren’t always a reliable source of medical information. Most of the articles are written by science journalists (compared with Scientific American, where many of them are written by the researchers themselves), and although they have a scientific education they are mainly generalists without the specialist experience to appreciate the nuances in a medical paper. When it comes to reporting research involving new ideas or approaches to treatment they are almost as bad as the lay press in implying that something will soon be available fore patients when in reality it will be decades or more likely never.
Actually I have never understood why patients are so keen on having the latest treatment, which generally means something that hasn’t been tested very thoroughly, particularly when it comes to medical devices or surgery. In case anybody is wondering, I should add that the Covid vaccines have been tested very thoroughly indeed.
In the specific case of vitamin D, many people in Northern Europe are deficient, particularly at the end of the Winter, so a supplement is a good idea, though 25 mcg daily is usually plenty.
There’s a problem with vitamin D believers taking doses that are way more than the tolerable upper intake level, which in the USA is 4000 IU/day for adults. https://ods.od.nih.gov/factsheets/VitaminD-HealthProfessional/
People think, if some is good, then more is better.
So it’s a good idea to give a caution along with the positive evidence.