Fish oil (omega-3 PUFA) preparations are today extremely popular and amongst the best-researched dietary supplement. During the 1970s, two Danish scientists, Bang and Dyerberg, remarked that Greenland Eskimos had a baffling lower prevalence of coronary artery disease than mainland Danes. They also noted that their diet contained large amounts of seal and whale blubber and suggested that this ‘Eskimo-diet’ was a key factor in the lower prevalence. Subsequently, a flurry of research stared to investigate the phenomenon, and it was shown that the ‘Eskimo-diet’ contained unusually high concentrations of omega-3 polyunsaturated fatty acids from fish oils (seals and whales feed predominantly on fish).
Initial research also demonstrated that the regular consumption of fish oil has a multitude of cardiovascular and anti-inflammatory effects. This led to the promotion of fish oil supplements for a wide range of conditions. Meanwhile, many of these encouraging findings have been overturned by more rigorous studies, and the enthusiasm for fish oil supplements has somewhat waned. But now, a new paper has come out with surprising findings.
The objective of this meta-analysis was to evaluate the association of anxiety symptoms with omega-3 PUFA treatment compared with controls in varied populations.
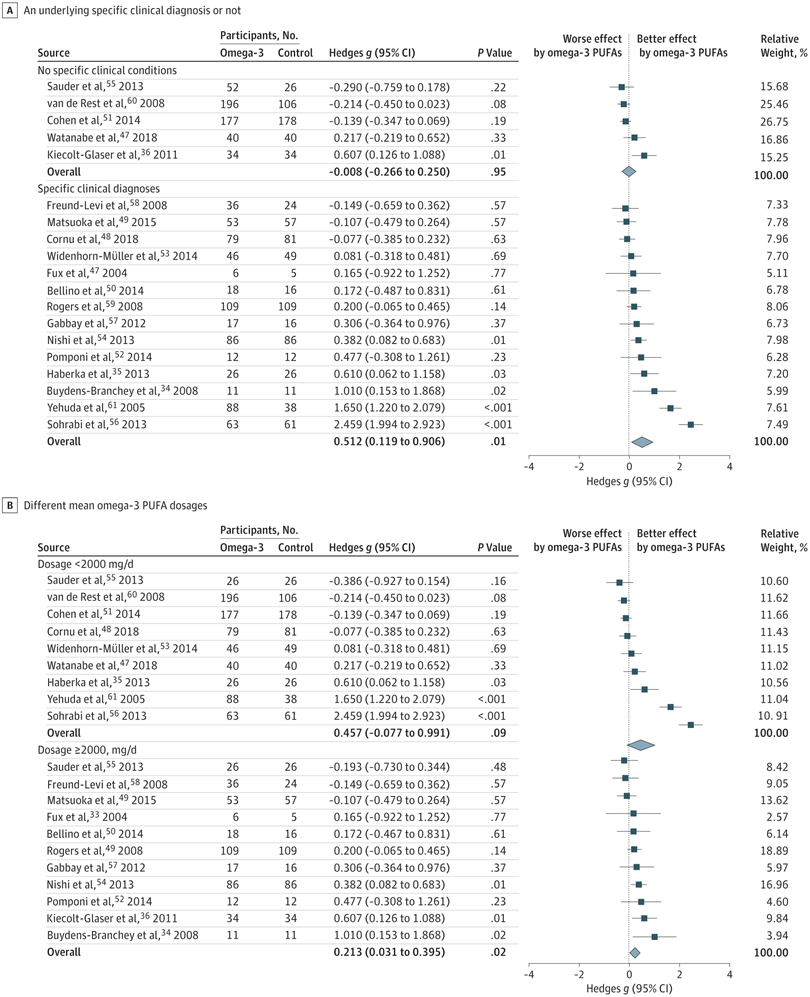
A search was performed of clinical trials assessing the anxiolytic effect of omega-3 PUFAs in humans, in either placebo-controlled or non–placebo-controlled designs. Of 104 selected articles, 19 entered the final data extraction stage. Two authors independently extracted the data according to a predetermined list of interests. A random-effects model meta-analysis was performed. Changes in the severity of anxiety symptoms after omega-3 PUFA treatment served as the main endpoint.
In total, 1203 participants with omega-3 PUFA treatment and 1037 participants without omega-3 PUFA treatment showed an association between clinical anxiety symptoms among participants with omega-3 PUFA treatment compared with control arms. Subgroup analysis showed that the association of treatment with reduced anxiety symptoms was significantly greater in subgroups with specific clinical diagnoses than in subgroups without clinical conditions. The anxiolytic effect of omega-3 PUFAs was significantly better than that of controls only in subgroups with a higher dosage (at least 2000 mg/d) and not in subgroups with a lower dosage (<2000 mg/d).
The authors concluded that this review indicates that omega-3 PUFAs might help to reduce the symptoms of clinical anxiety. Further well-designed studies are needed in populations in whom anxiety is the main symptom.
I think this is a fine meta-analysis reporting clear results. I doubt that this paper truly falls under the umbrella of alternative medicine, but fish oil is a popular food supplement and should be mentioned on this blog. Of course, the average effect size is modest, but the findings are nevertheless intriguing.

Indeed, Dr. Ernst, the difference here is the sound biochemical background supporting the action of PUFA Omega – 3 and the absolute absence of any philosophical or religious pseudo-scientific concepts.
The chiral opposite of homeopathy and else.
yes, of course
So according to you even when science proves something works – it still may not work –
Reading through this website it is extremely bias
Makes me wonder who your sponsors are?? and how much you are paid to write your opinions!
I cant wait for your big long winded scientific karate do type style defence that states the whole world is wrong except… you! Or will it be I’m too cool to answer with … whatever! Or perhaps you may look for a spelling error, or gramatical mistake to zone in on… Not everyone thinks your a legend… Theres a whole bunch of us that think your a brainwasshed idi*t…
Will you rant about your reply or will you sit and think about it… Perhaps write a whole post about how someone disagreed with your naive mind…
I find it difficult and useless to discuss with people foaming from their mouths
I guess that proves not everyone agrees with the disinformation you promote. It’s quite refreshing to hear someone have a dig at you… Some of the baloney you write it’s no wonder.
always nice to know there is a fan out there!
toybas said:
Who do you think they are and how much he’s paid? But who are your sponsors and how much are you paid to write your drivel here?
Tobyas,
“So according to you even when science proves something works – it still may not work”
The review quoted here doesn’t prove that anything works, it suggests that omega-3 fatty acids may have some benefit in anxiety and that this is worth investigating further. It is quite common to read this sort of conclusion in medical papers, and I certainly wouldn’t regard this as enough to base my practice on (not that I treat anxiety – I am an oncologist). But as more evidence accumulates practice changes in line with it (or should do).
You’re an oncologist… You mean you kill people for a living… 2-3% efficacy rate.. . Everyone wonders how people like you sleep at night?
not everyone, just people like you who evidently have not understood a thing
Chemo kills everyone knows that except fake scientists like you and your groupies cause your all in denial… Gotta pay those mortgage repayments hey!
I think you are sick and need help
@Prof. Ernst
I am beginning to doubt your otherwise admirable policy of accepting (almost?) all comments, even the belligerent ones.
Even if the person behind “Geoff” has shown himself to be an irrelevant idiot and should be allowed on occasion to reaffirm this himself, this level of defamatory, hurtful excrement* is not what I would consider necessary to leave on display.
*Referring to: Geoff on Friday 28 September 2018 at 16:13
I ban people AFTER they sufficiently demonstrated that they are unable to make meaningful contributions and merely insult other. with him/her, this stage is approaching very fast.
Geoff,
I’m sorry not to have answered your post more promptly, but unfortunately I was in hospital this afternoon having cancer treatment myself and not feeling very well. Not chemotherapy today but one of the newer targeted therapies. However, I have had both chemotherapy and radiotherapy myself. Throughout my career I have always felt that I should treat my patients how I would want my family and indeed myself treated. Now I have been the patient for the past two years, and I have no reason to feel that I should have been doing anything differently in my practice.
I am grateful to my own doctors as I don’t think it is very likely that I would still be here to post on this forum without their help, or without the research that provides the eivdence that they base their treatment on.
I am really not sure where you get the figure of a 2 – 3% efficacy rate for oncology treatment. What sort of treatment? What sort of cancer? How are you defining efficacy? I don’t know any oncologist who would advocate a treatment that had such a low chance of working. Even phase I trials of previously untested drugs in terminally ill patients can do better than that.
Yes, I have watched people die from treatment that I have given them, and it isn’t very nice. Any intervention that affects the body sufficiently to modify the natural history of a disease will have unwanted effects, and when the disease is something like cancer, the drugs, radiotherapy, surgery etc. which are strong enough to be effective can have devastating side-effects in some cases. But we know what the side-effects are and how frequent, we know how to mitigate them, we explain them to our patients so that we can obtain proper informed consent before undertaking treatment, and we are continually researching into ways that they can be reduced. In general, the most toxic treatments are reserved for situations where we expect to achieve a long-term cure; where the aim is to control incurable disease a milder approach is required. And however bad the treatment can be, uncontrolled cancer is much worse.
Perhaps you are referring to incurable diseases, such as the one that I have. For these, the long-term survival rates are very poor, whatever you do. But in the shorter term, conventional, evidence-based treatment can improve quality of life, and, yes, survival, even if it can’t work miracles.
I will tell you the story of my father, who was diagnosed with metastatic stomach cancer just over twenty years ago. For various reasons it was difficult to diagnose (it was diffusely infiltrating the stomach wall – we call this linitus plastica – and didn’t show up on any of the endoscopies). By the time we knew what we were dealing with he had lost a lot of weight and was very frail; personally I had doubts about whether he was fit for chemotherapy. Nevertheless he insisted that he wanted to give it a go, and moreover that he wanted to go into a clinical trial. Although he lived in Wiltshire he was referred to a cancer centre 90 miles away in London (where I happened to be working at the time, and indeed where I am having my own treatment now) and was randomised between two different chemotherapy regimens, one of them being the standard treatment at the time, the other being a variation on it. He coped with his treatment much better than I expected, and even seemed to regard his trips to London as days out, since all the nurses made a great fuss of him (he was very charming) and his old girlfriends who lived nearby came to visit him in hospital. Within a month he was visibly stronger, and by the time he had completed his eighteen weeks of chemotherapy he was well enough to take himself off to Cambridge for an old university reunion, to go to a wedding and dance the night away, and more importantly to spend quality time with his family, which was treasured by him and by all of us. Roughly eight months after he completed his treatment, the cancer came back and started to progress rapidly; he was dead within a few weeks. But we had all had a great year with him which we would not have had otherwise. Also he had the satisfaction of knowing that he was contributing to knowledge that would help those who came after him.
I have faced this situation many times with my own patients, and I have not wanted to deny them the chance that was so precious to my own family. However, I know that his response was unusually good, and I have never made any unrealistic promises of what I could achieve. It has always been my policy to pull out as soon as possible if treatment was not working, to minimise the unwanted and potentially debilitating effects of chemotherapy.
For me, it is awkward that frequent hospital visits for treatment, consultations and scans, together with infections as a result of immunosuppression (more from my cancer than from treatment) make it difficult to plan things and impossible to work. It is frustrating that I am tired out walking the dog and I can’t wield a chainsaw any longer, let alone work (mainly as a result of tumours in my spine). I hate it that I have lost my sense of smell and the enjoyment of food and wine that goes with it (as a result of a parainfluenza infection, cancer-related, not treatment-related; the effects of chemotherapy on the immune system predispose to a different type of infection). Nevertheless I have a good quality of life and I am enjoying the bonus time that conventional medicine has been able to grant me so far, and I am indeed hoping for another useful year or two.
People like me sleep at night because we are honest with ourselves about what we can and can’t do, we know we can’t achieve miracles, but we know that we are making the lives of our patients a little bit better. Not all of them, and we don’t know in advance who will benefit the most from treatment, but the majority of them will benefit, even if it is only pain relief from radiotherapy. Indeed, I think one of the most valuable things that I have been able to do is to help my patients to understand what is happening to them, so that they are in a position to decide what to do next.
We know this, not only from seeing directly what effects our treatment is having, but from properly-conducted research, which forms the basis of what we do. We work in teams where every member is valued from what they can contribute. We submit ourselves to audit, so that we can see how well our practice stands up to local and national standards. We have regular meetings to discuss cases where things have not turned out as well as we had hoped, to see what can be learned. Where there are complaints, we try to understand why, and to try to resolve them to the satisfaction of all concerned, whatever that takes. We regularly undertake professional development in various forms, particularly to ensure that our practice is able to keep up with new knowledge.
I don’t know whether I have answered your question. From what you have said so far I fear that you will be none the wiser for my post, merely better-informed (to paraphrase Lord Birkenhead), but I hope other people reading this will take a more nuanced view.
Anyway, it has been a long day and I will not be able to sleep tonight if I don’t go to bed soon.
thank you Julian; I hope you have many more months of good quality life.
Wonderful and wise writing as ever, Julian. Will Geoff read this, understand this and feel suitably chastened? Probably not. Those of his ilk never do.
Prof. Ernst wrote:
It is good to see some comforting, albeit rather vague, news about fish oil, in light of the disappointing conclusions (that prof. Ernst also touched on) about the absent effects of Omega-3 on CVD and absent effects on dry eyes
Here in the north, fish oil has since prehistoric times been considered a life-giving sustenance. People were brought up drinking a good mouthful every morning. Many swore that it was what made them strong and healthy. The main benefit was and still is considered its supplementation of vitamin D, which is otherwise lacking due to the lack of sunlight most of the year. People here need extra vit. D, now most take it concentrated in pills.
But perhaps also because fats provide concentrated caloric energy that gives a slow, warming sustenance into the day. The taste is an acquired one 😉
This reminds me of another study I read about a few years ago. Unfortunately I don’t have the reference to hand, and this is going to have to be from memory.
The study arose from the SELECT trial, a large, prospective, double-blind, four-way cancer prevention trial exploring the potential benefits of selenium and vitamin E in reducing the risk of prostate cancer. The results were published a few years ago, and in fact showed that selenium had no effect, whereas vitamin E increased the risk of prostate cancer (not entirely surprising given that other trials have shown antioxidents to be carcinogenic, possibly due to interference with DNA-repair mechanisms).
Anyway, one thing the SELECT researchers did was to collect and store blood samples from their subjects, and to make them available for other studies. One such explored the relationship between omega-3 fatty acids and prostate cancer. What the investigators did was to identify individuals who developed prostate cancer over the course of the study, match them with controls who did not get cancer, and then measure levels of twelve different omega-3 fatty acids in their baseline blood samples. They found that for three of the fatty acids, higher levels correlated with subsequent development of prostate cancer. They concluded that omega-3 fatty acid supplementation may have a role in reducing prostate cancer risk.
To my mind there were a number of concerns regarding this study. First of all, although SELECT had been a randomised prospective trial, the omega-3 study was a retrospective case-control study with all the statistical shortcomings of this design. Secondly, looking at twelve different fatty acids and only finding correlations with three of them seems rather like data-dredging: if you look at enough different factors you will find some correlations purely by chance, and this approach certainly means that tests of statistical significance need to be interpreted with caution. Finally, the authors use serum fatty acid levels as a surrogate for dietary intake without giving any explanation of whether this is valid.
The biggest concern of all, of course, was how it was reported in the press. A number of my prostate cancer patients brought in cuttings from national newspapers saying that omega-3 fatty acids were useful against prostate cancer, and I had to spend a lot of time explaining why that didn’t necessarily mean that they should all be taking them. Though I wasn’t nearly as upset as I was when I came across an elderly man with lung cancer spending money that he couldn’t really afford from his meagre pension on omega-3 fatty acid supplements, on the recommendation of his GP who had read some daft article about their use intravenously at high doses in pancreatic cancer and really should have known better.
I am not against omega-3 fatty acids, but as your review shows, it is important to examine the evidence critically, and to read the literature carefully and not simply to accept the conclusions given in the abstract.
@Julian Money-Kyrle,
your kind and informed comments are much appreciated. Whenever I notice that you wrote a comment in this blog, I am looking forward to reading it.
Thank you for sharing your deep professional knowledge and your personal experience, I wish you all the best for your ongoing treatment.