Monthly Archives: August 2018
The aim of palliative care is to improve quality of life for patients with serious illnesses by treating their symptoms, often in situations where all the possible causative therapeutic options have been exhausted. In many palliative care settings, complementary and alternative medicine (CAM) is used for this purpose. In fact, this is putting it mildly; my impression is that CAM seems to have flooded palliative care. The question is therefore whether this approach is based on sufficiently good evidence.
This review was aimed at evaluating the available evidence on the use of CAM in hospice and palliative care and to summarize their potential benefits. The researchers conducted thorough literature searches and located 4682 studies of which 17 were identified for further evaluation. The therapies considered included:
- acupressure,
- acupuncture,
- aromatherapy massage,
- breathing,
- hypnotherapy,
- massage,
- meditation,
- music therapy,
- reflexology,
- reiki.
Many studies demonstrated a short-term benefit in symptom improvement from baseline with CAM, although a significant benefit was not found between groups.
The authors concluded that CAM may provide a limited short-term benefit in patients with symptom burden. Additional studies are needed to clarify the potential value of CAM in the hospice or palliative setting.
When reading research articles in CAM, I often have to ask myself: ARE THEY TAKING THE MIKEY?
??? “Many studies demonstrated a short-term benefit in symptom improvement from baseline with CAM, although a significant benefit was not found between groups.” ???
Really?!?!?
Controlled clinical trials are only about comparing the outcomes between the experimental and the control groups (and not about assessing improvements from baseline which can be [and often is] unrelated to any effect caused by the treatment per se). Therefore, within-group changes are irrelevant and should not even deserve a mention in the abstract. Thus the only finding worth reporting in the abstract is this:
No significant benefit was found.
It follows that the above conclusions are totally out of line with the data.
They should, according to what the researchers report in their abstract, read something like this:
CAM HAS NO PROVEN BENEFIT IN PALLIATIVE CARE. ITS USE IN THIS AREA IS THEREFORE HIGHLY PROBLEMATIC.
Music therapy is the use of music for therapeutic purposes. Several forms of music therapy exist. They can consist of a patient listening to live or recorded music, or of patients participating in performing music. Music therapy is usually employed to complement other treatments; it is never a curative or causal approach and mostly aimed at inducing relaxation and enhancing physical and emotional well-being, or at promoting motor and communication skills.
There is a paucity of rigorous studies assessing the effectiveness of music therapy for specific condition, not least due to methodological obstacles and funding issues. Several systematic reviews of clinical studies have nevertheless emerged and results are generally encouraging. As for hypertension, the evidence is contradictory whether passive listening to music works. One review concluded that Music may improve systolic blood pressure and should be considered as a component of care of hypertensive patients. And another review revealed a trend towards a decrease in blood pressure in hypertensive patients who received music interventions, but failed to establish a cause-effect relationship between music interventions and blood pressure reduction.
A new study might bring more clarity:
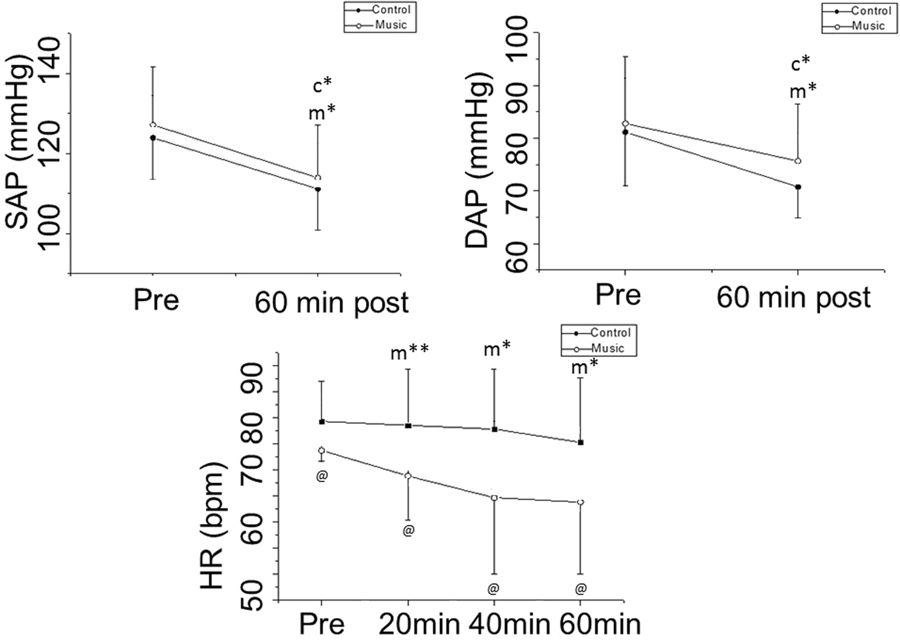
Its authors evaluated the effect of musical auditory stimulus associated with anti-hypertensive medication on heart rate (HR) autonomic control in hypertensive subjects. They included in this trial 37 well-controlled hypertensive patients designated for anti-hypertensive medication. Heart rate variability (HRV) was calculated from the HR monitor recordings of two different, randomly sorted protocols (control and music) on two separate days. Patients were examined in a resting condition 10 minutes before medication and 20 minutes, 40 minutes and 60 minutes after oral anti-hypertensive medications. Music was played throughout the 60 minutes after medication with the same intensity for all subjects in the music protocol.
The results showed analogous response of systolic and diastolic arterial pressure in both protocols. HR decreased 60 minutes after medication in the music protocol, while it remained unchanged in the control protocol. The effects of anti-hypertensive medication on SDNN (Standard deviation of all normal RR intervals), LF (low frequency, nu), HF (high frequency, nu) and alpha-1 scale were more intense in the music protocol. Blood pressure readings showed no significant differences between the two groups.
The authors concluded that musical auditory stimulus increased HR autonomic responses to anti-hypertensive medication in well-controlled hypertensive subjects.
So, there were some acute effects on HRV. But what is the clinical relevance of this effect? I am not sure, and the authors tell us little about this.
Crucially, there was no effect on blood pressure. But the study design might have been ill-suited for detecting one. I think that a much simpler trial with two parallel groups of untreated hypertensives would have been more efficient for this purpose.
As a music-lover, I would like to believe that music can be used therapeutically. Yet, for hypertensives, I find it difficult to see how this could work. Even if passive listening to music had an anti-hypertensive effect, could it be employed in clinical routine? I somehow doubt it; we can hear music for a while, but our daily activities would largely prohibit doing it for prolonged periods (and most likely it would become a nuisance after a while and would put our pressure up rather than down – think of the background music that bothers us in some shops, for instance). And how would it work when we sleep, a time during which blood pressure control can be vital?
As a music-lover, I would also argue that listening to music can be pleasantly relaxing – presumably, the anti-hypertensive effect observed in some trials relies on this effect. But surely, it can also have the opposite effect. If I strongly dislike a piece of music, I might increase my blood pressure. If a piece moves me deeply, it could easily do the same. It is probably only a certain type of music that induces relaxation; and, to make it even more complex, this type might differ from person to person.
So, is music therapy potentially a usable anti-hypertensive?
Somehow, I don’t think so!
About 7 months ago, I contacted a German journalist who I knew and trusted to tell her about the incredible quackery-promotion performed by Germany’s institutes of adult education, the ‘Volkshochschulen‘ (VHSs). After I had been invited to give a few lectures for the VHSs, I had conducted some preliminary research and realised that, nationwide, they run hundreds of courses promoting the worst types of quackery.
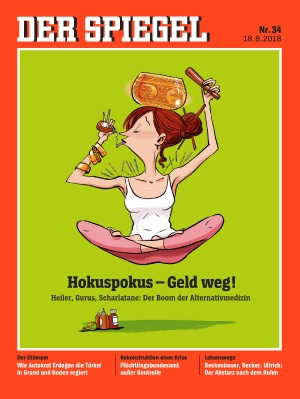
My journalist friend, Veronika Hackenbroch, who works for DER SPIEGEL liked the idea of conducting an in-depth investigation into the matter. What it revealed became the centre-piece of a theme issue published today. Here is its title page:
In a nutshell, the key finding is that every 5th course offered by the VHSs in the area of healthcare is steeped in woo. Considering that their funding comes mainly from the public purse, this is intolerable. When asked why they offer so much quackery, some heads of local VHSs said that they are not competent to evaluate the science; they simply assume that, if doctors in Germany use these treatments – specifically homeopathy – and if the public wants to learn about them, they have to offer them.
When I first heard this argument, it made me speechless. It has some undeniable logic behind it. The heads of VHSs are not medical experts. Thus, they cannot do their own research or evaluations. To just follow what the doctors must therefore seem reasonable to them.
So, where is the crux of the problem?
I think, it lies in the vicious circle that inevitable unfolds such a situation:
- some people like homeopathy (or other bogus treatments),
- therefore, they ask their doctors to provide it,
- therefore, some doctors offer it,
- therefore, the VHSs feel they can promote if,
- therefore, people like homeopathy (or other bogus treatments).
This circle has no beginning and no end; it just turns and turns. And it is difficult to stop, not least because it is driven by the relentless promotion of interested parties, such as the manufacturers of woo. Yet, if we want to make progress and are serious about improving healthcare, we have to try stopping it!
But how?
Through providing information and fighting misinformation (of course, some rules and regulations would help as well).
That’s exactly what we tried to do – thank you Veronika Hackenbroch!
I am truly saddened and shocked to hear that Peter Fisher has died. Apparently, he was cycling to work on 15 August, when, at 9.30 am, he was hit and fatally injured by a lorry. The Faculty of Homeopathy published the following statement:
The Faculty of Homeopathy has to announce with great sadness, news of the death of the Faculty President, Dr Peter Fisher in a road accident near the Royal London Hospital for Integrated Medicine (RLHIM), London, UK, on the morning of 15th August 2018.
Dr Fisher was Director of Research at the hospital, Europe’s largest centre for integrative medicine. He was also Physician to Her Majesty Queen Elizabeth II. He was previously Honorary Consultant Rheumatologist at King’s College Hospital. He was also one of the world leaders in homeopathic research, and will be sorely missed not only by his family and UK friends and colleagues but around the whole world.
A graduate of Cambridge University and a Fellow of the Royal College of Physicians and the Faculty of Homeopathy, he was a widely published expert in rheumatology and forms of complementary and alternative medicine. Dr Fisher chaired the World Health Organisation’s working group on homeopathy and was a member of WHO’s Expert Advisory Panel on Traditional and Complementary Medicine. He was awarded the Albert Schweitzer Gold Medal of the Polish Academy of Medicine in 2007.
Further detail will appear on the website in due course.
______________________________________________________________
This is how Peter described himself on the Bupa website:
I specialise in homeopathy and other forms of complementary medicine, integrated with conventional treatment, for rheumatological complaints including osteoarthritis, rheumatoid arthritis and soft tissue syndromes such as Fibromyalgia. Also for skin conditions including eczema and psoriasis and a range of general medical problems. I accept both NHS and Private referrals.
I am Associate Clinical Director and Director of Research at the Royal London Hospital for Integrated Medicine, Europe’s largest centre for integrative medicine.
I am also Physician to Her Majesty The Queen.
I was previously Honorary Consultant Rheumatologist at King’s College Hospital. I am a graduate of Cambridge University and a Fellow of the Royal College of Physicians and of the Faculty of Homeopathy. I am accredited as a specialist in both homeopathy and rheumatology.
_____________________________________________________________________
I knew Peter well. We first met when we both served on a EU committee on homeopathy in Brussels for several years. I do not think that I exaggerate, if I say that we became friends. I did respect him for his relatively prudent stance on many things related to homeopathy. For instance, he was an outspoken critic of the anti-vaxx attitude of many of his fellow homeopaths. We even have two publications together:
Complementary medicine must be research led and evidence based.
He was also a contributor of my book ‘HOMEOPATHY, A CRITICAL APPRAISAL‘ where he co-authored a chapter on homeopathic pathogenetic trials which contained the sentence, ” It is not possible to reach a definitive conclusion regarding the true effects of homeopathic medicines in healthy volunteers...”
And, in 2015, we published a BMJ ‘head to head’ together where we outlined our differences regarding homeopathy:
Should doctors recommend homeopathy?
It is no secret to regular readers of this blog that, lately, we disagreed on many things. In the course of these differences, our friendship regrettably fell apart.
I am nevertheless deeply saddened to hear of this tragic accident.
I know, I have reported about the risks of chiropractic manipulations many times before. But I will continue to do so, because the subject is important and mentioning it might save lives.
The purpose of this study from the US was to determine the frequency of patients seen at a single institution who were diagnosed with a cervical vessel dissection related to chiropractic neck manipulation. The researchers identified cases through a retrospective chart review of patients seen between April 2008 and March 2012 who had a diagnosis of cervical artery dissection following a recent chiropractic manipulation. Relevant imaging studies were reviewed by a board-certified neuroradiologist to confirm the findings of a cervical artery dissection and stroke. The investigators also conducted telephone interviews to ascertain the presence of residual symptoms in the affected patients.
Of the 141 patients with cervical artery dissection, 12 had documented chiropractic neck manipulation prior to the onset of the symptoms that led to medical presentation. The 12 patients had a total of 16 cervical artery dissections. All 12 patients developed symptoms of acute stroke. All strokes were confirmed with magnetic resonance imaging or computerized tomography. The researchers obtained follow-up information on 9 patients, 8 of whom had residual symptoms and one of whom died as a result of his injury.
The authors concluded that, in this case series, 12 patients with newly diagnosed cervical artery dissection(s) had recent chiropractic neck manipulation. Patients who are considering chiropractic cervical manipulation should be informed of the potential risk and be advised to seek immediate medical attention should they develop symptoms.
Cerebellar and spinal cord injuries related to cervical chiropractic manipulation were first reported in 1947. By 1974, there were 12 reported cases. Non-invasive imaging has since greatly improved the diagnosis of cervical artery dissection and of stroke, and cervical artery dissection is now recognized as pathogenic of strokes occurring in association with chiropractic manipulation.
The authors also point out that another institution had previously described 13 stroke cases after chiropractic manipulation. The patients at both institutions were relatively young and incurred substantial residual morbidity. A single patient at each institution died. If these findings are representative of other institutions across the United States, the incidence of stroke secondary to chiropractic manipulation may be higher than supposed. To assess this problem further, a randomized prospective cohort study could establish the relative risk of chiropractic manipulation of the cervical spine resulting in a cervical artery dissection. But such a study may be methodologically prohibitive. More feasible would be a case-control study in which patients who had experienced cervical artery dissection were matched with subjects who had not incurred such injuries. Comparing the groups’ odds of having received chiropractic manipulation demonstrated that spinal manipulative therapy is an independent risk factor for vertebral artery dissection and is highly suggestive of a causal association.
I very much agree with the authors when they sate that until the actual level of risk from chiropractic manipulation is known, patients with neck pain may be better served by equally effective passive physical therapy exercises.
In other words: there is very little reason to recommend chiropractic care for neck pain (or any other condition).
Kinesiology tape KT is fashionable, it seems. Gullible consumers proudly wear it as decorative ornaments to attract attention and show how very cool they are.
Am I too cynical?
Perhaps.
But does KT really do anything more?
A new trial might tell us.
The aim of this study was to investigate whether adding kinesiology tape (KT) to spinal manipulation (SM) can provide any extra effect in athletes with chronic non-specific low back pain (CNLBP).
Forty-two athletes (21males, 21females) with CNLBP were randomized into two groups of SM (n = 21) and SM plus KT (n = 21). Pain intensity, functional disability level and trunk flexor-extensor muscles endurance were assessed by Numerical Rating Scale (NRS), Oswestry pain and disability index (ODI), McQuade test, and unsupported trunk holding test, respectively. The tests were done before and immediately, one day, one week, and one month after the interventions and compared between the two groups.
After treatments, pain intensity and disability level decreased and endurance of trunk flexor-extensor muscles increased significantly in both groups. Repeated measures analysis, however, showed that there was no significant difference between the groups in any of the evaluations.
The authors, physiotherapists from Iran, concluded that the findings of the present study showed that adding KT to SM does not appear to have a significant extra effect on pain, disability and muscle endurance in athletes with CNLBP. However, more studies are needed to examine the therapeutic effects of KT in treating these patients.
Regular readers of my blog will be able to predict what I have to say about this study design: A+B versus B is not a meaningful test of anything. I used to claim that it cannot possibly produce a negative result – and yet, here it seems to have done exactly that!
How come?
The way I see it, there are two possibilities to explain this:
- the KT has a mildly negative effect on CNLBP; thus the expected positive placebo-effect was neutralised to result in a null-effect overall;
- the study was under-powered such that the true inter-group difference could not manifest itself.
I think the second possibility is more likely, but it does really not matter at all. Because the only lesson we can learn from this trial is this: inadequate study designs will hardly ever generate anything worthwhile.
And this is, I think, a lesson that would be valuable for many researchers.
_______________________________________________________________________
Reference
Comparing spinal manipulation with and without Kinesio Taping® in the treatment of chronic low back pain.
I have often cautioned my readers about the ‘evidence’ supporting acupuncture (and other alternative therapies). Rightly so, I think. Here is yet another warning.
This systematic review assessed the clinical effectiveness of acupuncture in the treatment of postpartum depression (PPD). Nine trials involving 653 women were selected. A meta-analysis demonstrated that the acupuncture group had a significantly greater overall effective rate compared with the control group. Moreover, acupuncture significantly increased oestradiol levels compared with the control group. Regarding the HAMD and EPDS scores, no difference was found between the two groups. The Chinese authors concluded that acupuncture appears to be effective for postpartum depression with respect to certain outcomes. However, the evidence thus far is inconclusive. Further high-quality RCTs following standardised guidelines with a low risk of bias are needed to confirm the effectiveness of acupuncture for postpartum depression.
What a conclusion!
What a review!
What a journal!
What evidence!
Let’s start with the conclusion: if the authors feel that the evidence is ‘inconclusive’, why do they state that ‘acupuncture appears to be effective for postpartum depression‘. To me this does simply not make sense!
Such oddities are abundant in the review. The abstract does not mention the fact that all trials were from China (published in Chinese which means that people who cannot read Chinese are unable to check any of the reported findings), and their majority was of very poor quality – two good reasons to discard the lot without further ado and conclude that there is no reliable evidence at all.
The authors also tell us very little about the treatments used in the control groups. In the paper, they state that “the control group needed to have received a placebo or any type of herb, drug and psychological intervention”. But was acupuncture better than all or any of these treatments? I could not find sufficient data in the paper to answer this question.
Moreover, only three trials seem to have bothered to mention adverse effects. Thus the majority of the studies were in breach of research ethics. No mention is made of this in the discussion.
In the paper, the authors re-state that “this meta-analysis showed that the acupuncture group had a significantly greater overall effective rate compared with the control group. Moreover, acupuncture significantly increased oestradiol levels compared with the control group.” This is, I think, highly misleading (see above).
Finally, let’s have a quick look at the journal ‘Acupuncture in Medicine’ (AiM). Even though it is published by the BMJ group (the reason for this phenomenon can be found here: “AiM is owned by the British Medical Acupuncture Society and published by BMJ”; this means that all BMAS-members automatically receive the journal which thus is a resounding commercial success), it is little more than a cult-newsletter. The editorial board is full of acupuncture enthusiasts, and the journal hardly ever publishes anything that is remotely critical of the wonderous myths of acupuncture.
My conclusion considering all this is as follows: we ought to be very careful before accepting any ‘evidence’ that is currently being published about the benefits of acupuncture, even if it superficially looks ok. More often than not, it turns out to be profoundly misleading, utterly useless and potentially harmful pseudo-evidence.
Reference
Acupunct Med. 2018 Jun 15. pii: acupmed-2017-011530. doi: 10.1136/acupmed-2017-011530. [Epub ahead of print]
Effectiveness of acupuncture in postpartum depression: a systematic review and meta-analysis.
Li S, Zhong W, Peng W, Jiang G.
It has been shown repeatedly that a ‘conspiracy mentality’ is associated with usage of alternative medicine. But perhaps alternative medicine is itself a conspiracy theory in disguise?
One of the questions I invariably get after a public lecture is the one about alternative medicine being the victim of some sort of sinister plot. This notion can take various shapes and forms:
- The scientific establishment prevents the public from fully benefitting from the effects of alternative medicine.
- The pharmaceutical industry suppresses the good news about alternative treatments.
- The funding agencies refuse to fund research into alternative medicine.
- The media are bent on defaming alternative medicine.
- The regulators do not allow alternative medicine to thrive as much as it would deserve.
- The medical profession is afraid that the benefits of alternative medicine become better known.
I could go on, but I am sure you get the picture.
The amazing thing is that I hear such arguments not just from fanatic proponents of alternative medicine, but also from more reasonable people. These sentiments seem to be entirely common and seemingly logical arguments. Most people I meet seem to believe them at least to some degree.
Having heard them so often, I do wonder: Can one explain alternative medicine as a conspiracy theory?
A conspiracy theory is an erroneous and often difficult to falsify notion that tries to explain a set of circumstances as the result of a secret plot by usually powerful conspirators, while ignoring obvious alternative explanations. The very concept of alternative medicine assumes that there are valuable therapies that conventional healthcare does not allow in its realm.
The reasons for the secret plot that prevents them to be included in conventional healthcare are rarely named by enthusiasts of alternative medicine. So, what are they?
- Professional jealousy?
- Financial interests?
- Lack of interest?
- Lack of caring?
According to proponents of alternative medicine who I have asked, they consist of a mixture of all of these possibilities. And all of these possibilities are, in a way, consistent with alternative medicine being based on a conspiracy theory.
When I ask people why they believe in these theories, they cannot produce any solid evidence for their beliefs. This does not surprise me because, as far as I can see, there is no evidence to support them: they are erroneous. In turn, this means that one important criterium for conspiracy theory is being met.
Another characteristic of conspiracy theories is that they cannot easily been proven to be false. None of the above-listed reasons are, in fact, difficult to falsify.
A final characteristic of conspiracy theories is that its proponents are ignoring obvious alternative explanations.
WHY ARE ALTERNATIVE THERAPIES NOT ADMITTED INTO THE REALM OF CONVENTIONAL MEDICINE?
Simply because they are not supported by sufficiently strong evidence for generating more good than harm.
So, yes, to some extent alternative medicine even is a conspiracy theory in disguise.
How often do we hear this sentence: “I know, because I have done my research!” I don’t doubt that most people who make this claim believe it to be true.
But is it?
What many mean by saying, “I know, because I have done my research”, is that they went on the internet and looked at a few websites. Others might have been more thorough and read books and perhaps even some original papers. But does that justify their claim, “I know, because I have done my research”?
The thing is, there is research and there is research.
The dictionary defines research as “The systematic investigation into and study of materials and sources in order to establish facts and reach new conclusions.” This definition is helpful because it mentions several issues which, I believe, are important.
Research should be:
- systematic,
- an investigation,
- establish facts,
- reach new conclusions.
To me, this indicates that none of the following can be truly called research:
- looking at a few randomly chosen papers,
- merely reading material published by others,
- uncritically adopting the views of others,
- repeating the conclusions of others.
Obviously, I am being very harsh and uncompromising here. Not many people could, according to these principles, truthfully claim to have done research in alternative medicine. Most people in this realm do not fulfil any of those criteria.
As I said, there is research and research – research that meets the above criteria, and the type of research most people mean when they claim: “I know, because I have done my research.”
Personally, I don’t mind that the term ‘research’ is used in more than one way:
- there is research meeting the criteria of the strict definition
- and there is a common usage of the word.
But what I do mind, however, is when the real research is claimed to be as relevant and reliable as the common usage of the term. This would be a classical false equivalence, akin to putting experts on a par with pseudo-experts, to believing that facts are no different from fantasy, or to assume that truth is akin to post-truth.
Sadly, in the realm of alternative medicine (and alarmingly, in other areas as well), this is exactly what has happened since quite some time. No doubt, this might be one reason why many consumers are so confused and often make wrong, sometimes dangerous therapeutic decisions. And this is why I think it is important to point out the difference between research and research.
The following announcement was made by the NHS on 7 August 2018:
The Governing Body of Bristol, North Somerset and South Gloucestershire (BNSSG) Clinical Commissioning Group (CCG) today approved changes that mean NHS funded homeopathy will only be available in exceptional circumstances in the area. The changes will mean the CCG’s Individual Funding Request (IFR) Panel would need a clinician to set out why the patient is clinically exceptional before treatment could be provided.
The decision comes after the publication of a report, which took evidence from local people, clinicians, patient groups, providers of homeopathic treatments and national guidelines.
CCG Clinical Chair Dr Jonathan Hayes said, “We are working hard to become an evidence-informed organisation because we need to make the best use of all resources to offer treatment and care to the widest range of people. The decision on homeopathy funding today is a step towards this and brings us in line with national guidelines.”
It is estimated that 41 patients receiving NHS funded homeopathic consultations in the area cost the local NHS £109,476 in the 2017/2018 financial year.
END OF QUOTE

The move is the result of 4 years of excellent work by the GOOD THINKING SOCIETY, a charity dedicate to the promotion of rational thinking.
Michael Marshall, its Project Director, said: “We are very pleased to see the Bristol CCGs take this decision to cease funding for homeopathy – every other CCG across the country has made it clear that homeopathic remedies are no better than placebo and such there is simply no place for homeopathy on the NHS.
“With the end to homeopathy funding in Bristol, the region joins NHS bodies across the rest the country in recognising that homeopathy is not a valid use of limited NHS resources. There is now no CCG in England where homeopathic pills or consultations can be routinely funded with NHS money – instead, funding can be directed towards treatments that have been shown to actually work.”
Does that not call for a knighthood for Mr Marshall?
One would have thought so!
Who will tell Prince Charles to get the ball rolling?
And while we are all waiting for the big event, you might as well donate a few £s to this truly splendid charity.
Please be generous!!!