We all know that there is a plethora of interventions for and specialists in low back pain (chiropractors, osteopaths, massage therapists, physiotherapists etc., etc.); and, depending whether you are an optimist or a pessimist, each of these therapies is as good or as useless as the next. Today, a widely-publicised series of articles in the Lancet confirms that none of the current options is optimal:
Almost everyone will have low back pain at some point in their lives. It can affect anyone at any age, and it is increasing—disability due to back pain has risen by more than 50% since 1990. Low back pain is becoming more prevalent in low-income and middle-income countries (LMICs) much more rapidly than in high-income countries. The cause is not always clear, apart from in people with, for example, malignant disease, spinal malformations, or spinal injury. Treatment varies widely around the world, from bed rest, mainly in LMICs, to surgery and the use of dangerous drugs such as opioids, usually in high-income countries.
The Lancet publishes three papers on low back pain, by an international group of authors led by Prof Rachelle Buchbinder, Monash University, Melbourne, Australia, which address the issues around the disorder and call for worldwide recognition of the disability associated with the disorder and the removal of harmful practices. In the first paper, Jan Hartvigsen, Mark Hancock, and colleagues draw our attention to the complexity of the condition and the contributors to it, such as psychological, social, and biophysical factors, and especially to the problems faced by LMICs. In the second paper, Nadine Foster, Christopher Maher, and their colleagues outline recommendations for treatment and the scarcity of research into prevention of low back pain. The last paper is a call for action by Rachelle Buchbinder and her colleagues. They say that persistence of disability associated with low back pain needs to be recognised and that it cannot be separated from social and economic factors and personal and cultural beliefs about back pain.
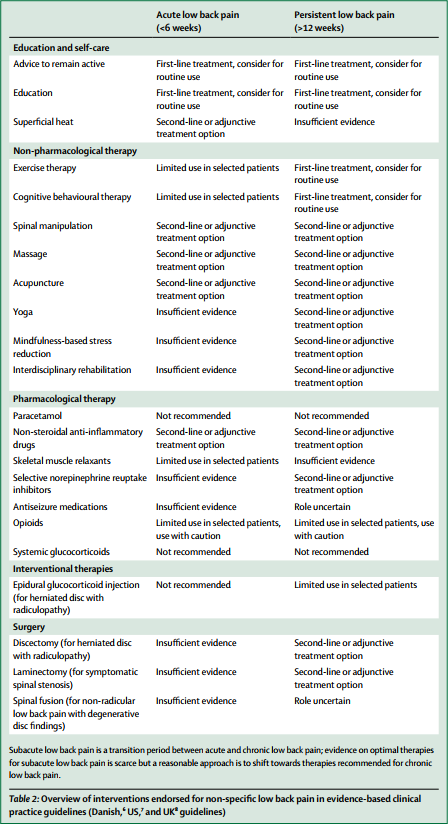
Overview of interventions endorsed for non-specific low back pain in evidence-based clinical practice guidelines (Danish, US, and UK guidelines)
In this situation, it makes sense, I think, to opt for a treatment (amongst similarly effective/ineffective therapies) that is at least safe, cheap and readily available. This automatically rules out chiropractic, osteopathy and many others. Exercise, however, does come to mind – but what type of exercise?
The aim of this meta-analysis of randomized controlled trials was to gain insight into the effectiveness of walking intervention on pain, disability, and quality of life in patients with chronic low back pain (LBP) at post intervention and follow ups.
Six electronic databases (PubMed, Science Direct, Web of Science, Scopus, PEDro and The Cochrane library) were searched from 1980 to October 2017. Randomized controlled trials (RCTs) in patients with chronic LBP were included, if they compared the effects of walking intervention to non-pharmacological interventions. Pain, disability, and quality of life were the primary health outcomes.
Nine RCTs were suitable for meta-analysis. Data was analysed according to the duration of follow-up (short-term, < 3 months; intermediate-term, between 3 and 12 months; long-term, > 12 months). Low- to moderate-quality evidence suggests that walking intervention in patients with chronic LBP was as effective as other non-pharmacological interventions on pain and disability reduction in both short- and intermediate-term follow ups.
The authors concluded that, unless supplementary high-quality studies provide different evidence, walking, which is easy to perform and highly accessible, can be recommended in the management of chronic LBP to reduce pain and disability.
I know – this will hardly please the legions of therapists who earn their daily bread with pretending their therapy is the best for LBP. But healthcare is clearly not about the welfare of the therapists, it is/should be about patients. And patients should surely welcome this evidence. I know, walking is not always easy for people with severe LBP, but it seems effective and it is safe, free and available to everyone.
My advice to patients is therefore to walk (slowly and cautiously) to the office of their preferred therapist, have a little rest there (say hello to the staff perhaps) and then walk straight back home.

As written on page 8 of the Lancet Low Back Pain Series 2, “Improved and better integrated education of health-care professionals could support implementation of best practice for low back pain..and create new and innovative strategies for practice. Examples of such support include, the integrated education of medical doctors with Chiropractors in Denmark..”
yes… and?
Which begs the question as to why anyone would want to spend time and trouble studying ‘chiropractic’, which its devisor D D Palmer stated was a ‘different system from medicine’, rather than medicine.
And quite what the point might be of offering ‘integrated’ education in two quite different systems.
Practitioners who have gone down the ‘chiropractic’ path, for whatever reason, should do their best to overcome the ‘sunk cost fallacy’ and retrieve their careers by training as physiotherapists or councillors.
As a surgeon I never operated for ‘low back pain’ – but did so to remove pressure crushing, and defunctioning, a nerve root (neuropraxia or neurotemesis).
And I only used MRI to indicate where I should operate, not whether I should.
(i.e. After I had decided surgical attention was indicated on clinical grounds.)
Without very clear indications indeed for surgery, ‘Ernst’s Exercises’ will suffice, and be cost effective.
RR, you must be very rare amongst your colleagues in regard to surgery and MRI’s. I applaud your management, it is (or was) very safe. But how many of your colleagues (especially in the U.S.) reach for the MRI referral pad at the slight hint of low back pain, “Just to see what the problem really is”. How many reach for the opiate prescription as first choice before trying all the safer methods of treatment? I would suggest that this over-management has cost us millions of wasted dollars/pounds, far in excess of what is reasonable.
You may be right.
I do not know.
But that’s a tu quoque logical fallacy, and a red herring.
Do not compare bad medicine with chiropractic. They’re much the same!
And that’s the point.
Richard,
Why integrate?
Based on the opinion of the Lancet Low Back Pain Series Working Group, here are the reasons to integrate.
1. Develop best practice.
2. Help break down professional barriers.
3. Develop a common language.
4. Create new and innovative strategies for practice.
1 Is what conventional medicine constantly strives to do.
2. There would be no ‘barrier’ if students contemplating ‘chiropractic’ qualified in medicine. As I did.
3. Medicine is practised by those with many languages. ‘Twas ever thus.
4. See 1 above.
To which consider:
(i) That adding cow pie to apple pie does not make apple pie better.
(ii) That DD Palmer always intended chiropractic to be different from medicine.
Enjoy your career as best you may, but please don’t harm mine.
With respect to the establishment of Australia’s Macquarie University private hospital and medical school without the initial requested removal of the universities long established Centre for Chiropractic. It is time for the integration of both health disciplines so innovative management of spinal pain and health can be more effectively pursued.
innovative management of spinal pain by the chiropractic profession?
could you please list some of the innovations chiropractors have contributed to this field in the last 12o years?
other that falsely calling themselves ‘Dr’, I mean.
EE, who can use the title “Dr”?
Vetinarians?
Medical Practitioners?
Dentists?
Physiotherapists?
Chiropractors?
Osteopaths?
Doctors of Philosophy?
Doctors of Science?
Doctors of Divinity?
Doctors of Law?
In the UK, anyone can use the title ‘Dr’. Or ‘Lord’ as in Sutch.
Some dentists do – though why they are not proud enough to use ‘Dentist’ (Dn), is for them to explain.
Unless a registered medical practitioner or qualified PhD, why would anyone want to use ‘doctor’, unless to mislead and defraud?
E.E., In looking at the recommendations for the treatment of common low back pain, could you please list some of the innovations physiotherapists, orthopaedic surgeons and the pharmaceutical industry have contributed to this field in the last 12o years
no, I asked first
1.Digital Motion X-ray https://www.dmxworks.com/
2. Chiropractic biophysics spinal remodelling traction and mirror image spinal manipulation procedures. https://idealspine.com/
3. Instrument-based manipulation as opposed to just manual manipulation. http://neuromechanical.com/
4. My own research on the development of a new method of traction called SMAT (Supine Mid Abdominal Traction)
http://www.cjaonline.com.au/index.php/cja/article/view/184
1 show me the evidence that this is a chiro innovation
2 I don’t consider this an innovation worth writing home about
3 I don’t consider this an innovation worth writing home about
4 I don’t consider this an innovation worth writing home about
Write to DMX and find out for yourself.
normally, it is the one who makes a claim who ought to substantiate it – or did i get that wrong too?
Regarding instrument-based manipulation. contact Dr Gunzberg, the editor of the European Spine Journal and ask him about his collaborative research with chiropractors regarding this topic.
!! I imagined Mr Epstein would cite some serious articles, even if only published in chiropractic journals, but…
1. The references cited by Wikipedia indeed indicate this is not a chiropractic innovation.
2. The lengthy account of this on the linked website contains no formal reference citations to supporting evidence.
3. This is the famous ‘activator’, a tarted-up version of a spring-loaded automatic centre punch. For connoisseurs of chiropractic hilarity you can watch examples of this wonderful device in action here and here and here.
4. This is a case report: ‘research’ with N=1.
Is there any remote possibility Mr Epstein might recognize just how pathetic his response is?
I would not hold my breath
“both health disciplines” I think not. One is a discipline supported by developing knowledge and research, the other is a magical belief system based on nonsense extricated from his fundament by a con man.
@ME…Another chimera from a chimerical “professional”.
Positing oneself as indispensable into all matters which benefit you (and likely you alone) was always the arena of the priest….seems DCs, PTs, ATCs and others of that ilk see the robust pecuniary reward of selling religion to the masses i.e. “bring me your pain and I’ll “treat-it-away””.
“…and create new, innovative strategies…” LOL…..just like 150,000 DCs over 123 years have done? PTs, DCs and ATCs have been suggesting “eventually we’ll stumble upon something that works” but never hesitate charging for all the shit that don’t
Having just re-read, and with the intention of innumerable ‘re-reads’….More Harm Than Good, I can’t quite wrap my brain around how amazing, succinct, insightful and THOROUGH it is!!
It is brilliant in all regards….not the least of which is your ability to create understanding from otherwise typically overwhelming topics e.g. statistics, ethics etc. Bravo!
If anyone has ever contemplated “alternative medicine”, at any level, and has NOT bought this book then shame on them and: “you deserve to get swindled’!!
It’s easy to recognize the blog-contributors here who HAVE NOT and WILL NOT read this book….. They are blind and need to remain blind for their own selfish reasons.
now, that’s a nice compliment!
but most of the praise must go to my co-author Kevin Smith who is brilliant.
can we tempt you to put this comment on the book’s Amazon site? PLEASE!
@ Michael
You are a physio?
Yes, he is, plus the ex-husband of a chiropractor.
I see that the “shake, bake and fake” of modern physiotherapy is not even considered as an option for treatment.
any idea about this?
http://www.nejm.org/doi/full/10.1056/NEJM199911043411903
and a commentary about it:
http://www.nejm.org/doi/full/10.1056/NEJM200003163421112
A+B is usually more than B alone.
Osteopaths often advise against drugs.
Until osteopathy became regulated in some countries, New Zealand and Australia for example, there were three types of osteopaths.
1) American trained, who had a very similar qualification to medical practitioners.
2). U.K., N.Z. Australian trained who had a similar qualification to chiropractors, but always better qualifications than physiotherapists.
3). Totally untrained, with no formal qualifications who did a few weekend courses in how to “crunch spines” and were than able to call themselves osteopaths as there was no regulation governing this.
It is incorrect for you to use the professional designation “osteopath” without defining which group they belong to.
whatever
Edzard … unfortunately you are right. The preliminary medical exam in the US has no effect for to stop US osteopathic physicians D.O. to support the old ideas of drugless healing by advertising Cranial Osteopathy and to call medication ‘a poisoning’ in general… but there is the same problem all over the world. The preliminary exam doesn’t stop physicians from practising CAM.
GibleyGibley … and don’t forget the Swiss osteopaths with GDK diploma. Their training is according to the WHO benchmarks for training in osteopathy. The exam in Switzerland is done according to the law and to fixed regulations and subjects by officially adviced Swiss state physicians and contains embryology as a core subject !! to proof that they understand the details of the ‘involuntary mechanism’ (iatromechanic plus vitalism).
Like a knight in ‘Monty Python and the Holy Grail’ I would ask you now: “What do you mean with ‘osteopath’ – an US osteopathic physician D.O. or an European / Commonwealth osteopathic manipulator Dr. (ost) or M.Sc. (ost) or B.Sc. (ost) or …
In direct relation to The Lancet series on Low Back Pain, the President of the British Chiropractic Association appears to be overselling chiropractic on Channel 5 news tonight:
https://www.facebook.com/AECCUniversityCollege/videos/vb.283166808463426/1596663297113764/?type=3&theater
Not that anyone is likely to be surprised.
Back pain should not be ignored in its early stages, proper tests must be done and appropriate medicine must be taken prescribed by the doctor to relief pain. People waste a lot of money on irrelevant medicine and therapies that does not cure their disease.
I am suggesting:
Don’t walk home but insist on a proper diagnostic procedure because there could be some pathologies like osteoporothic fractures or bone cancer or a meningeoma or other severe ilnesses which cannot be treated by walking at all …
before
” ….walking straight back home again…”
I would insist on a detailed medical checkup by following the medical guidlines. Why?
Look here:
https://www.nejm.org/doi/full/10.1056/NEJMicm1714206
She had symtoms FOR THREE MONTHS progressing and it took her THREE MONTH until a proper medical investigation was carried out …
I had a similar case wuth meningeoma
I had a similar case suffering from meningeoma and her physicist (Dr. med.) whom I called was not willing to send her to the MRI when she went to him after my call.
She reported to me alternating sensations for 3 minutes warm after 15 minutes cold a.s.o. AND as the one lower leg became cold the other became warm and this was alternating too every 10 to 15 minutes. I palpated this and it was true and her reflexes were weak but still there she could stand on her heels and toes but had light burning sensations tingling and numbness in both feet.
Because the physicist (Dr. med.) told her “this guy (he meant me) has no idea what he is talking about” (I am a Heilpraktiker) I sent her to the emergeny unit the next day and she had a 6 hours surgery at once ….
Uh, you do know EE that the Sitthipornvorakul, et al paper you mentioned on walking, that walking was compared mainly to PT based exercise, PT program or some type of patient education…and many of those papers used the A+B design…a design with which you seem to have an issue.
You did read the paper, right?
We all are at a staggering 84% chance of succumbing to back pain in our lifetime. which can interrupt our daily routine like a thoroughbred professional. But this pain needs to be catered to properly for reducing its propensity.
meaning?
we need effective treatments – but, at present, we hardly have any.
Here are some tips for relieving from lower back pain. Maintain a healthy weight, Keep your back muscles strong, Stretch your muscles, Focus on good posture, Lift properly, sleep well.
Any skeptics going to challenge these?
Back pain is a very sensitive issue for everyone. As a back pain sufferer dr. advice me have to lose my weight.
Here i got some effective suggestion like maintain ur weight, Stretch your muscles carefully, Focus on good posture, sleep well and therapist is a good option for sufferer
It’s a little more complicated than just loose weight or stretch some muscles. I don’t expect many to read these, but these papers may be of interest to those of us who actually deal with these patients on a daily basis.
Paraspinal
CONCLUSIONS: The results indicate atrophy in CLBP in the multifidus and paraspinal muscles but not in the erector spinae. No atrophy was shown in RLBP and ALBP. Fat infiltration did not occur in RLBP, but results in CLBP were inconsistent. No abnormalities in fiber type in the paraspinal muscles were found in CLBP.
http://www.painphysicianjournal.com/linkout?issn=1533-3159&vol=19&page=E985
Reflexes were evoked in each of the homonymous muscles with latencies and estimated conduction velocities compatible with being evoked by Ia muscle afferents and having a monosynaptic component. Short latency heteronymous excitatory reflex connections were observed in muscles on the ipsilateral side, whilst reflex responses in the contralateral muscles were inhibitory in response to the same stimulus. The latencies of the crossed responses were on average 9.1 ms longer than the ipsilateral excitatory responses. These results are in contrast to the crossed excitatory responses observed between the abdominal muscles and trapezius muscles on the opposite aspect of the trunk.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3324696/
Conclusion Even between symptomatic episodes, young individuals with a history of low back pain demonstrated altered recruitment of the deep fibers of lumbar multifidus in response to changing locomotor speed during walking turns.
http://digitalcommons.chapman.edu/pt_articles/43/
These findings suggest that abnormal segmental motion noted on kinetic MR images is closely associated with disc degeneration, FJO, and the pathological characteristics of interspinous ligaments, ligamentum flavum, and paraspinal muscles. Kinetic MR imaging in patients with mechanical back pain may prove a valuable source of information about the stability of the functional spine unit by measuring abnormal segmental motion and grading of radiographic parameters simultaneously.
https://www.researchgate.net/publication/24427087_Kinetic_magnetic_resonance_imaging_analysis_of_abnormal_segmental_motion_of_the_functional_spine_unit_Clinical_article
Muscle attenuation varied by specific muscle (p < .001), was lower in older adults (p < .001), and was generally lower in women than in men (p < .001), although not in all muscles. Age-related differences in muscle attenuation varied with specific muscle (p < .001), with the largest age differences occurring in the paraspinal and abdominal muscles.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3605905/
CONCLUSION: The present findings show that there is selective ipsilateral atrophy of paraspinal muscles, specific to the symptomatic side, in patients with acute and chronic LBP. The reduction of the muscle CSA and increased fatty infiltration occurred synchronously, and the extent of change is significantly greater in chronic LBP in the ES muscle. Atrophy of the MF muscle appears to be at multiple levels but side specific in relation to symptoms in patients with chronic LBP, and the decreased muscle CSA may occur prior to fatty infiltration.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4743557/
CONCLUSIONS: Paraspinal fat infiltration, but not muscle CSA, was associated with high-intensity pain/disability and structural abnormalities in the lumbar spine. Although cause and effect cannot be determined from this cross-sectional study, longitudinal data will help to determine whether disabling low back pain and structural abnormalities of the spine are a cause or result of fat replacement of paraspinal muscles.
https://www.ncbi.nlm.nih.gov/m/pubmed/25828477/?i=2&from=%2F25947906%2Frelated
Patients with low back pain have a less refined position sense than healthy individuals, possibly because of an altered paraspinal muscle spindle afference and central processing of this sensory input. Furthermore, muscle vibration can be an interesting expedient for improving proprioception and enhancing local muscle control.
https://www.ncbi.nlm.nih.gov/pubmed/10767813
Among older adults with chronic LBP of at least moderate intensity, L5 multifidi muscle composition, but not size, may help to explain physical function.
https://www.ncbi.nlm.nih.gov/pubmed/27590444
Tendency of smaller trunk musculature CSA may be a cause or a result of chronic LBP. A unique pattern of larger CSA at L3-L4 and L4-L5 disc levels and smaller CSA at L5-S1 of Rectus abdominis muscles is observed in LBP patients compared to healthy persons. Differences in disc angles and CSA of disc at L3-L4 and L4-L5 levels between the two groups signify that these may be the predisposing factors leading to LBP due to abnormal load/stress transmission and precipitating early degenerative changes in the disc.
https://www.ncbi.nlm.nih.gov/pubmed/27421282
As a result, the degree of intramuscular fat infiltration seems to be affected by age, disc level, and muscle type. It seems to be more prominent in the extensor muscles, extending from lower to upper levels.
https://www.ncbi.nlm.nih.gov/pubmed/27497888
There was evidence for a negative association between cross-sectional area (CSA) of multifidus and LBP, but conflicting evidence for a relationship between erector spinae, psoas and quadratus lumborum CSA and LBP. Moreover, there was evidence to indicate multifidus CSA was predictive of LBP for up to 12 months in men, but insufficient evidence to indicate a relationship for longer time periods. While there was conflicting evidence for a relationship between multifidus fat infiltration and LBP, there was no or limited evidence for an association for the other paraspinal musculature. Conclusions This review found evidence that multifidus CSA was negatively associated with and predictive of LBP, up to 12 months but conflicting evidence for an association between erector spinae, psoas and quadratus lumborum CSA, and LBP. To further understand the role of the paraspinal musculature in LBP, there is a need for high quality cohort studies which extend over both the short and longer term.
https://www.ncbi.nlm.nih.gov/pubmed/28756299
Eleven studies were included. With 1 exception, all pooled results were significantly different statistically between groups, suggesting that paraspinal muscles are smaller in patients with chronic LBP than in control patients and on the symptomatic side of patients with chronic unilateral LBP. In patients with acute unilateral LBP, there was no significant difference between sides. A qualitative examination demonstrated a trend toward an increased effect size when outcome assessors were unblinded.
https://www.researchgate.net/publication/236056840_Multifidus_and_Paraspinal_Muscle_Group_Cross-Sectional_Areas_of_Patients_With_Low_Back_Pain_and_Controls_A_Systematic_Review_With_a_Focus_on_Blinding
so glad you master the copy and past task – now you can begin to contemplate what is cause and what is effect here
If you think it’s a simple cause and effect relationship, it indicates naivety on your part.
did I claim it to be simple?
“…now you can begin to contemplate what is cause and what is effect here.”
based upon your request, yes, simplicity is implied.
you have too much fantasy – but, I suppose as a chiro, you might need it.