Monthly Archives: January 2018
This survey assessed chiropractic (DC) and naturopathic “doctors”‘ (ND) knowledge, attitudes, and behaviour with respect to the pediatric patients in their practice. Cross-sectional surveys were developed in collaboration with DC and ND educators. Surveys were sent to randomly selected DCs and NDs in Ontario, Canada in 2004, and a national online survey was conducted in 2014. Data were analyzed using descriptive statistics, t-tests, non-parametric tests, and linear regression.
Response rates for DCs were n = 172 (34%) in 2004, n = 553 (15.5%) in 2014, and for NDs, n = 171 (36%) in 2004, n = 162 (7%) in 2014. In 2014, 366 (78.4%) of DCs and 83 (61%) of NDs saw one or more paediatric patients per week. Paediatric training was rated as inadequate by most respondents in both 2004 and 2014, with most respondents (n = 643, 89.9%) seeking post-graduate training by 2014. About half of DCs (51.7% in 2004, 49.2% in 2014) and one fifth of NDs (21% in 2004 and 23% in 2014) reported they received no hands-on clinical paediatric training. Only a minority of practitioners felt their hands-on paediatric training was adequate (somewhat or very) for their needs: DCs: 10.6% in 2004, 15.6% in 2014; NDs: 10% in 2004 and 19% in 2014. Respondents’ comfort in treating children and youth is based on experience and post-graduate training. Both DCs and NDs that see children and youth in their practices address a broad array of paediatric health concerns, from well child care and preventative health, to mild and serious illness.
The authors included two ‘case studies’ of conditions frequently treated by DCs and NDs:
Case study 1: colic
DC practitioners’ primary treatment focus (314 respondents) would be to use spinal manipulation (78.3%) if physical assessment suggests utility, diet changes (14.6% for child, 6.1% for mom if breast feeding), and massage (16.9%). ND practitioners (95 respondents) would assess and treat primarily with diet changes (62% for child including prescribing probiotics; 48% for mom if breast feeding), homeopathy (46%), weak herbal or tea preparations (19%), and use topical castor oil (packs or massage) (18%). In 2014, 65.9% of DCs and 59% of NDs believe (somewhat or very much) that concurrent treatment by a medical practitioner would be of benefit; 64.0% of DCs and 60% of NDs would refer the patient to another health care practitioner (practitioner type not specified).
Case study 2: acute otitis media
In 2014, almost all practitioners identified this as otitis media (in 2004, the DCs had a profession-specific question); DCs were more cautious about the value of their care for it relative to the NDs (DCs, 46.2% care will help patient very much, NDs, 95%). For treatment, DCs would primarily use spinal manipulation (98.5%) if indicated after assessment, massage (19.5%), dietary modifications (17.6%), and 3.8% would specifically refer to an MD for an antibiotic prescription. ND-preferred treatments were NHP products (79%), dietary modifications (66%), ear drops (60%), homeopathic remedies (18%), and 10% would prescribe antibiotics right away or after a few days. In 2014, 86.3% of DCs and 75% of NDs believe the patient would benefit (somewhat or very much) from concurrent treatment by a conventional medical practitioner; 81.7% of DCs and 58% of NDs would refer the patient to another health care provider.
The authors concluded that although the response rate in 2014 is low, the concerns identified a decade earlier remain. The majority of responding DCs and NDs see infants, children, and youth for a variety of health conditions and issues, but self-assess their undergraduate paediatric training as inadequate. We encourage augmented paediatric educational content be included as core curriculum for DCs and NDs and suggest collaboration with institutions/organizations with expertise in paediatric education to facilitate curriculum development, especially in areas that affect patient safety.
I find these data positively scary:
- Despite calling themselves ‘doctors’, they are nothing of the sort.
- DCs and NCs are not adequately educated or trained to treat children.
- They nevertheless often do so, presumably because this constitutes a significant part of their income.
- Even if they felt confident to be adequately trained, we need to remember that their therapeutic repertoire is wholly useless for treating sick children effectively and responsibly.
- Therefore, harm to children is almost inevitable.
- To this, we must add the risk of incompetent advice from CDs and NDs – just think of immunisations.
The only conclusion I can draw is this: chiropractors and naturopaths should keep their hands off our kids!
Can conventional therapy (CT) be combined with herbal therapy (CT + H) in the management of Alzheimer’s disease (AD) to the benefit of patients? This was the question investigated by Chinese researchers in a recent retrospective cohort study funded by grants from China Ministry of Education, National Natural Science Foundation of China, Beijing Municipal Science and Technology Commission, and Beijing Municipal Commission of Health and Family Planning.
In total, 344 outpatients diagnosed as probable dementia due to AD were collected, who had received either CT + H or CT alone. The GRAPE formula was prescribed for AD patients after every visit according to TCM theory. It consisted mainly (what does ‘mainly’ mean as a description of a trial intervention?) of Ren shen (Panax ginseng, 10 g/d), Di huang (Rehmannia glutinosa, 30 g/d), Cang pu (Acorus tatarinowii, 10 g/d), Yuan zhi (Polygala tenuifolia, 10 g/d), Yin yanghuo (Epimedium brevicornu, 10 g/d), Shan zhuyu (Cornus officinalis, 10 g/d), Rou congrong (Cistanche deserticola, 10 g/d), Yu jin (Curcuma aromatica, 10 g/d), Dan shen (Salvia miltiorrhiza, 10 g/d), Dang gui (Angelica sinensis, 10 g/d), Tian ma (Gastrodia elata, 10 g/d), and Huang lian (Coptis chinensis, 10 g/d), supplied by Beijing Tcmages Pharmaceutical Co., LTD. Daily dose was taken twice and dissolved in 150 ml hot water each time. Cognitive function was quantified by the mini-mental state examination (MMSE) every 3 months for 24 months.
The results show that most of the patients were initially diagnosed with mild (MMSE = 21-26, n = 177) and moderate (MMSE = 10-20, n = 137) dementia. At 18 months, CT+ H patients scored on average 1.76 (P = 0.002) better than CT patients, and at 24 months, patients scored on average 2.52 (P < 0.001) better. At 24 months, the patients with improved cognitive function (△MMSE ≥ 0) in CT + H was more than CT alone (33.33% vs 7.69%, P = 0.020). Interestingly, patients with mild AD received the most robust benefit from CT + H therapy. The deterioration of the cognitive function was largely prevented at 24 months (ΔMMSE = -0.06), a significant improvement from CT alone (ΔMMSE = -2.66, P = 0.005).

The authors concluded that, compared to CT alone, CT + H significantly benefited AD patients. A symptomatic effect of CT + H was more pronounced with time. Cognitive decline was substantially decelerated in patients with moderate severity, while the cognitive function was largely stabilized in patients with mild severity over two years. These results imply that Chinese herbal medicines may provide an alternative and additive treatment for AD.
Conclusions like these render me speechless – well, almost speechless. This was nothing more than a retrospective chart analysis. It is not possible to draw causal conclusions from such data.
Why?
Because of a whole host of reasons. Most crucially, the CT+H patients were almost certainly a different and therefore non-comparable population to the CT patients. This flaw is so elementary that I need to ask, who are the reviewers letting such utter nonsense pass, and which journal would publish such rubbish? In fact, I can be used for teaching students why randomisation is essential, if we aim to find out about cause and effect.
Ahhh, it’s the BMC Complement Altern Med! I think the funders, editors, reviewers, and authors of this paper should all go and hide in shame.
This is the title of an editorial by Alan Schmukler. You probably remember him; I have featured him before, for instance here, here, and here. This is what was recently on Schmukler’s mind (I have added a few references referring to comments of mine added below):
England’s National Health Service (NHS) is proposing that NHS doctors no longer be permitted to prescribe homeopathic remedies [1]… They claim lack of evidence for effectiveness. Anyone who’s been remotely conscious the last 10 years will see this as a pretext. Homeopathy is practiced by board certified physicians in clinics and hospitals around the world [2]. The massive Swiss review of homeopathy, found it effective, safe and economical, and the Swiss incorporated homeopathy into their national health care system [3]…
The reason given for banning homeopathy and these nutrients is a lie. Why would the NHS ban safe, effective and affordable healing methods? [4] Without these methods, all that is left are prescription drugs. Apparently, someone at the NHS has an interest in pushing expensive prescription drugs [5], rather than safer and cheaper alternatives. That someone, also wishes to deny people freedom of choice in medicine [6]. I say “someone”, because organizations don’t make decisions, people do. Who is that someone? In looking for a suspect, we might ask, who is the chief executive of the organization? Who introduced this plan and is promoting it? Who at the NHS has the political clout? Who was it that recently declared: “Homeopathy is a placebo and a misuse of scarce NHS funds which could better be devoted to treatments that work”.
The quote is from Simon Stevens, NHS England’s chief executive. He got the job in 2014, after ten years as a top executive at UnitedHealth, the largest health insurance company in America. His past work experiences and current activities show that he favors privatization [7]. That would make him an odd choice to run a healthcare system based on socialized medicine. In fact, he has been moving the NHS towards privatization and the corporate, profit based American model. [8] The last thing a privatizer in healthcare would want, are non-proprietary medicines, for which you can’t charge exorbitant fees [9]. Banning homeopathy on the NHS is just one small part of a larger plan to maximize corporate profits by letting corporations own and control the health care system [10]. Before they can do this, they have to eliminate alternative methods of treatment.
Personally, I think Schmukler is wrong – here is why:
1 The current argument is not about what doctors are permitted to do, but about what the NHS should do with our tax money.
2 Argumentum ad populum
3 Oh dear! Anyone who uses this report as evidence must be desperate – see for instance here.
4 Why indeed? Except highly dilute homeopathic remedies are pure placebos.
5 Maybe ‘someone’ merely wants to use effective medications rather than placebos.
6 Freedom of choice is a nonsense, if it is not guided by sound evidence – see here.
7 No, that’s Jeremy Hunt! But in any case privatisation might be more profitable with homeopathy – much higher profit margins without any investment into R&D.
8 No, this is Hunt again!
9 Homeopathic remedies are ideal for making vast profits: no research, no development, no cost for raw material, etc., etc.
10 I am sure Boiron et al would not mind stepping into the gap.
I very much look forward to the next outburst of Alan Schmukler and hope he will manage to think a bit clearer by then.
We have discussed the NHMRC report on homeopathy several times – see, for instance, here, here and here. Perhaps understandably, homeopaths have great difficulties accepting its negative findings, and have complained about it ever since it was published. Now, a very detailed and well-researched analysis has become available of both the report and its criticism. Here I take the liberty to copy and (clumsily) translate its conclusions; if you can read German, I highly recommend studying the full document.
START OF MY TRANSLATION
The criticism of the NHMRC review is very voluminous and highlights many different aspects of the background, the methodology, the execution and the unwanted results from a homeopathic perspective. The very engaging discussions in the general public about this document and its flaws are, however, relatively meaningless: the NHMRC arrives at exactly the same conclusions as the employee of the Homeopathic Research Institute (HRI), Mathie, in his reviews of 2014 and 2017.
In both reviews, Mathie evaluated a total of 107 primary studies and found only 2 trials that could be rated as qualitatively good, that is to say constituting reliable evidence. Mathie did upgrade 2 further studies to the category of reliable evidence, however, this was in violation of the procedures proscribed in the study protocol.
The criticism of the NHMRC review was not able to make a single valid rebuttal. No condition could be identified for which homeopathy is clearly superior to placebo. This is all the more important, as Mathie avoided the mistakes that constituted the most prominent alleged criticisms of the NHMRC report.
- Since Mathie and most of his co-authors are affiliated with organisations of homeopathy, an anti-homeopathy bias can be excluded.
- Mathie conducted classic reviews and even differentiated between individualised and non-individualised homeopathy.
- Mathie did not exclude studies below a certain sample size.
Yet, in both reviews, he draws the same conclusion.
In view of the truly independent replications of an employee of the HRI, we can be sure that there are, in fact, no solid proofs for the effectiveness of homeopathy. The claim of a strong efficacy, equivalent to conventional medicines, that is made by homeopathy’s advocates is therefore not true.
END OF MY TRANSLATION
And here is the original German text:
Die Kritik an dem Review des NHMRC ist sehr umfangreich und beleuchtet sehr viele verschiedene Facetten über das Umfeld, die Methodik und die Durchführung sowie das aus Sicht der Homöopathen unerwünschte Ergebnis selbst. Die in der Öffentlichkeit sehr engagierte Diskussion um diese Arbeit und ihre möglichen Unzulänglichkeiten sind jedoch relativ bedeutungslos: Das NHMRC kommt zu genau dem gleichen Ergebnis wie Mathie als Mitarbeiter des HRI in seinen in 2014 und 2017 veröffentlichten systematischen Reviews:
Insgesamt hat Mathie in beiden Reviews 107 Einzelstudien untersucht und fand nur zwei Studien, die als qualitativ gut („low risk of bias“), also als zuverlässige Evidenz betrachtet werden können. Mathie hat zwar vier weitere Studien zur zuverlässigen Evidenz aufgewertet, was allerdings im Widerspruch zu den üblichen Vorgehensweisen steht und im Studienprotokoll nicht vorgesehen war.
Die Kritik am Review des NHMRC hat keinen einzigen Punkt fundiert widerlegen können. Man konnte keine Indikation finden, bei der sich die Homöopathie als klar über Placebo hinaus wirksam erwiesen hätte. Diese Punkte sind umso bedeutsamer, weil Mathie die am NHMRC hauptsächlich kritisierten Fehler nicht gemacht hat:
- Als Mitarbeiter des HRI und mit Autoren, die überwiegend für Homöopathie-affine Organisationen arbeiten, ist eine Voreingenommenheit gegen die Homöopathie auszuschließen.
- Mathie hat klassische Reviews ausgeführt, sogar getrennt zwischen einzelnen Ausprägungen (individualisierte Homöopathie und nicht-individualisierte Homöopathie).
- Mathie hat keine Größenbeschränkung der Studien berücksichtigt.
Er kommt aber dennoch zweimal zum gleichen Ergebnis wie das NHMRC.
Angesichts der wirklich als unabhängig anzusehenden Bestätigung der Ergebnisse des NHMRC durch einen Mitarbeiter des Homeopathy Research Institute kann man sicher davon ausgehen, dass es tatsächlich keine belastbaren Wirkungsnachweise für die Homöopathie gibt und dass die von ihren Anhängern behauptete starke, der konventionellen Medizin gleichwertige oder gar überlegene Wirksamkeit der Homöopathie nicht gegeben ist.
I do apologise for my clumsy translation and once again encourage those who can to study the detailed original in full.
My conclusion of this (and indeed of virtually all criticism of homeopathy) is that homeopaths are just as unable to accept criticism as an evangelic believer is going to accept any rational argument against his belief. In other words, regardless of how convincing the evidence, homeopaths will always dismiss it – or, to put it in a nutshell: HOMEOPATHY IS A CULT.
The title of this post is a statement recently made in an article by Mike Adams in ‘Alternative Medicine News’:
The cancer industry goes to great lengths to deny patients access to any information that they might use to prevent, treat or cure cancer without requiring expensive (and highly toxic) medical interventions. That’s what makes the BMJ documentation of this curcumin cancer cure so astonishing: In years past, the BMJ never would have even tolerated the publishing of such a scientific assessment. So what changed? In truth, the evidence of natural cures for cancer is now so overwhelming that even the BMJ cannot remain in a state of denial without appearing to be hopelessly out of touch with scientific reality.
The story is based on one single patient who apparently was cured of cancer using curcumin (turmeric). The case was also recently (3/1/18) featured on BBC’s ‘YOU AND YOURS’ (http://www.bbc.co.uk/programmes/b09k0ng7) in a similarly uncritical way: no expert was asked to provide an evidence-based assessment and bring some reason into the discussion. Even the DAILY FAIL reported about the story, and predictably, critical assessment had to make way for sensationalism.
So what?
We hear about such nonsense almost every day!
True, but this case is different; it is based on a publication in the highly-respected BMJ (well, actually, it was the ‘BMJ CASE REPORTS’ and not the BMJ, as reported). Here is the article:
START OF QUOTE
A woman aged 57 years was initially diagnosed with monoclonal gammopathy of undetermined significance (MGUS) in 2007 following an incidental finding of M-protein (18 g/L) during investigation for hypertension.
Within 15 months, the patient had rapidly progressed to ISS stage 3 myeloma with M-protein 49 g/L, urinary protein 1.3 g/24-hour, Bence-Jones protein 1.0 g/24-hour, Hb 9.7 g/dL and increasing back pain. She initially declined antimyeloma treatment but 6 months later, following vertebral collapse at T5 and T12, started cyclophosphamide, thalidomide and dexamethasone (CTD) treatment. However, after a week, the patient was admitted with idiosyncratic syndrome including hyponatraemia, a fall in albumin and worsening of blood counts. She received red cell transfusion and her electrolyte abnormalities were carefully corrected.
Although there was evidence of a response to CTD (M-protein 34 g/L), bortezomib and dexamethasone treatment was initiated as an alternative, but this was discontinued after three cycles due to progressive disease (M-protein 49 g/L). The patient was then treated with lenalidomide and dexamethasone with the aim of reducing disease burden prior to high-dose therapy and autologous stem cell transplantation. Treatment was frequently interrupted and dose adjusted to account for neutropenia and despite a minor response after six cycles (starting M-protein 47 g/L, finishing M-protein 34 g/L), in October 2009, she proceeded with stem cell mobilisation. However, neither cyclophosphamide nor plerixafor/GCSF priming were successful. A bone marrow biopsy revealed 50% myeloma cells and a course of CTD was restarted with cautious titration of thalidomide.
The patient achieved a partial response with CTD retreatment over the course of 17 cycles (M-protein 13 g/L) with no further episodes of idiosyncratic syndrome. However, attempts to harvest stem cells in February 2011 and again there months later, both failed. By then, her M-protein had risen to 24 g/L and the patient was too neutropenic to be considered for a clinical trial.
At this point, the patient began a daily regime of oral curcumin complexed with bioperine (to aid absorption), as a single dose of 8 g each evening on an empty stomach. A few months later, she also embarked on a once-weekly course of hyperbaric oxygen therapy (90 min at 2 ATA) which she has maintained ever since. Her paraprotein levels gradually declined to a nadir of 13 g/L, her blood counts steadily improved and there was no evidence of further progressive lytic bone disease.
Outcome and follow-up
The patient continues to take oral curcumin 8 g daily without further antimyeloma treatment. Over the last 60 months, her myeloma has remained stable with minimal fluctuation in paraprotein level, her blood counts lie within the normal range and she has maintained good quality of life throughout this period. Repeat bone imaging in 2014 identified multiple lucencies <1 cm in the right hip and degenerative changes in both hips, but these were attributed to osteoarthritis rather than the myeloma. Recent cytogenetic analysis revealed she had no abnormal cytogenetics by fluorescent in situ hybridisation.
Discussion
A small but significant number of myeloma patients consume dietary supplements in conjunction with conventional treatment primarily to help cope with the side effects of treatment, manage symptoms and enhance general well-being. Few, if any, use dietary supplementation as an alternative to standard antimyeloma therapy. Here, we describe a case in which curcumin has maintained long-term disease control in a multiply-relapsed myeloma patient. To the best of our knowledge, this is the first report in which curcumin has demonstrated an objective response in progressive disease in the absence of conventional treatment.
Curcumin is a polyphenol derived from the perennial herb Curcuma longa (turmeric) and has, for centuries, been used as a traditional Indian medicine. Several reports published over the two decades have claimed various health benefits of curcumin and this has led to its increasing popularity as a dietary supplement to prevent or treat a number of different diseases.
The biological activity of curcumin is indeed remarkable. It is a highly pleiotropic molecule which possesses natural antioxidant, anti-inflammatory, antiseptic and analgesic properties. More recently, it has demonstrated antiproliferative effects in a wide variety of tumour cells including myeloma cells and exerts its antiproliferative effects through multiple cellular targets that regulate cell growth and survival.
In vitro, curcumin prevents myeloma cell proliferation through inhibition of IL-6-induced STAT-3 phosphorylation and through modulation of the expression of NF-kB-associated proteins such as IkB〈,Bcl-2, Bcl-xL, cyclin D1 and IL-6 and apoptosis-related molecules including p53 and Bax. In other studies, curcumin was shown to circumvent resistance to dexamethasone, doxorubicin and melphalan as well as potentiate the effects of bortezomib, thalidomide and lenalidomide. Furthermore, curcumin-induced cell death was not influenced by myeloma molecular heterogeneity.
The antimyeloma effects of curcumin in the clinical setting however are less clear. Only one phase I/II study has evaluated curcumin treatment in myeloma patients. These patients were either asymptomatic, relapsed or had plateau phase disease. Treatment with curcumin downregulated the expression of NFkB, COX-2 and STAT3 in peripheral blood mononuclear cells, but no objective responses were observed in any subgroup of patients. This may be as a result of small sample size in this study, follow-up was limited to 3 months and clinical responses may have been observed with longer follow-up. However, downregulation of NFkB, COX-2 and STAT3 expression may not correlate with the clinical activity of curcumin and there may be further mechanisms of action that remain unclear, possibly through the modulation of another target. We would not be able to identify any patient-specific mechanisms of activity in this case study, as the patient has been taking curcumin for some time now and baseline bone marrow or peripheral blood samples are not available. However, in the setting of a clinical trial, it may be possible to use next-generation sequencing to help identify a mutation that may be a potential target for curcumin.
Another study examined its effects in preventing the progression of MGUS and smouldering myeloma to myeloma. The results showed that curcumin exerted a trace of biological activity with modest decreases in free light chain and paraprotein levels and a reduction in a marker of bone resorption with curcumin treatment, suggesting the therapeutic potential of curcumin in MGUS and smouldering myeloma. However, more studies are needed to address this further.
Whether such effects are observed in patients with active disease remains to be seen. The fact that our patient, who had advanced stage disease and was effectively salvaged while exclusively on curcumin, suggests a potential antimyeloma effect of curcumin. She continues to take daily curcumin and remains in a very satisfactory condition with good quality of life. This case provides further evidence of the potential benefit for curcumin in myeloma. We would recommend further evaluation of curcumin in myeloma patients in the context of a clinical trial.
END OF QUOTE
What should we make of this?
I think that much of the reporting around the story was grossly irresponsible. It is simply not possible to conclude that curcumin was the cause of the remission. It could be due to a whole host of other factors. And a case report is just an anecdote; it never can prove anything and can only be used to stimulate further research.
I fully agree with the authors of the case report: curcumin seems worthy of further investigation. But recommending it to patients for self-medication is vastly premature and quite simply dangerous, unethical and naïve bordering on stupid.
And, of course, the above-cited drivel of Mike Adams is just beyond the pale – the evidence for ‘alternative cancer cures‘ is very, very far from ‘overwhelming’; and the ‘cancer industry’ is doing what they can to determine whether turmeric or any other natural remedy can be used to treat cancer and other diseases.
If they are ever successful, the Adams of this world will shout ‘EXPLOITATION!!!’
If their endeavours are not successful, they will complain ‘CONSPIRACY!!!’
Yesterday, I heard my ‘good friend’ Dr Michael Dixon (see here, here and here, for example) talk on the BBC about the “new thing” in healthcare: social prescribing. He explained, for instance, that social prescribing could mean treating a diabetic not with medication but with auto-hypnosis and other alternative therapies. At that moment, I wasn’t even entirely sure what the term ‘social prescribing’ meant, I have to admit – so I did some reading.
What is social prescribing?
The UK ‘Social Prescribing Network‘ defines it thus:
Social Prescribing is a means of enabling GPs and other frontline healthcare professionals to refer patients to a link worker – to provide them with a face to face conversation during which they can learn about the possibilities and design their own personalised solutions, i.e. ‘co-produce’ their ‘social prescription’- so that people with social, emotional or practical needs are empowered to find solutions which will improve their health and wellbeing, often using services provided by the voluntary and community sector. It is an innovative and growing movement, with the potential to reduce the financial burden on the NHS and particularly on primary care.
Does social prescribing work?
The UK King’s Fund is mildly optimistic:
There is emerging evidence that social prescribing can lead to a range of positive health and well-being outcomes. Studies have pointed to improvements in areas such as quality of life and emotional wellbeing, mental and general wellbeing, and levels of depression and anxiety. For example, a study into a social prescribing project in Bristol found improvements in anxiety levels and in feelings about general health and quality of life. In general, social prescribing schemes appear to result in high levels of satisfaction from participants, primary care professionals and commissioners.
Social prescribing schemes may also lead to a reduction in the use of NHS services. A study of a scheme in Rotherham (a liaison service helping patients access support from more than 20 voluntary and community sector organisations), showed that for more than 8 in 10 patients referred to the scheme who were followed up three to four months later, there were reductions in NHS use in terms of accident and emergency (A&E) attendance, outpatient appointments and inpatient admissions. The Bristol study also showed reductions in general practice attendance rates for most people who had received the social prescription.
However, robust and systematic evidence on the effectiveness of social prescribing is very limited. Many studies are small scale, do not have a control group, focus on progress rather than outcomes, or relate to individual interventions rather than the social prescribing model. Much of the evidence available is qualitative, and relies on self-reported outcomes. Researchers have also highlighted the challenges of measuring the outcomes of complex interventions, or making meaningful comparisons between very different schemes.
Determining the cost, resource implications and cost effectiveness of social prescribing is particularly difficult. The Bristol study found that positive health and wellbeing outcomes came at a higher cost than routine GP care over the period of a year, but other research has highlighted the importance of looking at cost effectiveness over a longer period of time. Exploratory economic analysis of the Rotherham scheme, for example, suggested that the scheme could pay for itself over 18–24 months in terms of reduced NHS use….
END OF QUOTES
Is there no harder evidence at all?
The only Medline-listed controlled study seems to have been omitted by the King’s Fund – I wonder why. Perhaps because it fails to share the optimism? Here is its abstract:
Social prescribing is targeted at isolated and lonely patients. Practitioners and patients jointly develop bespoke well-being plans to promote social integration and or social reactivation. Our aim was to investigate: whether a social prescribing service could be implemented in a general practice (GP) setting and to evaluate its effect on well-being and primary care resource use. We used a mixed method evaluation approach using patient surveys with matched control groups and a qualitative interview study. The study was conducted in a mixed socio-economic, multi-ethnic, inner city London borough with socially isolated patients who frequently visited their GP. The intervention was implemented by ‘social prescribing coordinators’. Outcomes of interest were psychological and social well-being and health care resource use. At 8 months follow-up there were no differences between patients referred to social prescribing and the controls for general health, depression, anxiety and ‘positive and active engagement in life’. Social prescribing patients had high GP consultation rates, which fell in the year following referral. The qualitative study indicated that most patients had a positive experience with social prescribing but the service was not utilised to its full extent. Changes in general health and well-being following referral were very limited and comprehensive implementation was difficult to optimise. Although GP consultation rates fell, these may have reflected regression to the mean rather than changes related to the intervention. Whether social prescribing can contribute to the health of a nation for social and psychological wellbeing is still to be determined.
So, there is a lack of evidence for social prescribing. Yet, this is not why I feel uneasy about the promotion of this “new thing”. The more i think about it, the more I realise that social prescribing is just good care and decent medicine. It is what I was taught at med school 40 years ago. It therefore seems like a fancy name for something that should be obvious.
But why my unease?
The way I see it, it will be (and perhaps already is) used to smuggle bogus alternative therapies into the mainstream. In this way, it could turn out to serve the same purpose as did the boom in integrative/integrated medicine/healthcare: a smokescreen to incorporate treatments into medical routine which otherwise would not pass muster. If advocates of this approach, like Michael Dixon, subscribe to it, the danger of this happening is hard to deny.
The disservice to patients (and medical ethics) would then be obvious: diabetics unquestionably can benefit from a change of life-style (and to encourage them is part of good conventional medicine), but I very much doubt that they should replace their anti-diabetic medications with auto-hypnosis or other alternative therapies.
The question whether chiropractic is a truly valuable option for people suffering from back pain has been addressed repeatedly on this blog. My answer was usually negative, but proponents of chiropractic tended to argue that I am biased. Therefore I find it constructive to see what an organisation that hardly can be accused of bias says on this topic. An article by ‘SHOW ME THE EVIDENCE’ has recently provided a comprehensive overview of treatments for back pain. This is what they wrote about chiropractic:
START OF QUOTE
Spinal manipulation, the cranking and tweaking on offer when you visit a traditional chiropractor, is among the most popular approaches to back pain. Practitioners lay their hands on the patient and move their joints to or beyond their range of motion — a technique that’s often accompanied by a pop or crack.
There is some evidence the approach can help people with chronic back pain — but not any more than over-the-counter painkillers or exercise, and you need to take precautions when seeking out a chiropractor.
First, a quick look at the evidence. There are two recent Cochrane reviews on spinal manipulation for low back pain: one focused on people with acute (again, episodic/short duration) pain and the other on chronic pain. The 2011 review on chronic low back pain found that spinal manipulation had small, short-term effects on reducing pain and improving the patient’s functional status — but this effect was about the same as other common therapies for chronic low back pain, such as exercise. That review was published in 2011; UpToDate reviewed the randomized trials that have come out since — and also found that spinal manipulation delivered modest, short-term benefits for chronic back pain sufferers.
The Cochrane review on acute pain found that spinal manipulation worked no better than placebo. So people with a short episode of back pain should probably not bother seeing a chiropractor.
“Based on the evidence,” University of Amsterdam assistant professor Sidney Rubinstein, who is the lead author on the Cochrane reviews, told me, “it would appear [spinal manipulation] works as well as other accepted conservative therapies for chronic low back pain, such as non-prescription medication or exercise, but less well for patients with acute low back pain.”
As a chiropractor himself, he had some advice for patients: They should avoid chiropractors who routinely make X-rays or do advanced diagnostics for low back pain because this adds nothing to the clinical picture, particularly in the case of nonspecific low back pain. Patients should also beware chiropractors who put them on extended programs of care.
“Patients who respond to chiropractic care traditionally respond rather quickly,” he said. “My advice is those patients who have not responded to a short course of chiropractic care or manipulation should consider another type of therapy.”
While the risks of serious side effects from spinal manipulation for back pain are rare — about one in 10 million — the risks associated with chiropractic therapy for neck pain tend to be slightly higher: 1.46 strokes for every million neck adjustments.
The issue is the vertebral artery, which travels from the neck down through the vertebrae. Manipulating the neck can put patients at a higher risk of arterial problems, including stroke or vertebral artery dissection, or the tearing of the vertebral artery (though Rubinstein noted that people in the initial stages of stroke or dissection may also seek out care for their symptoms, such as neck pain, which makes it difficult to untangle how many of health emergencies are brought on by the adjustments).
END OF QUOTE
This all seems fairly reasonable to me – except for the following not entirely unimportant points:
- I am not sure where the evidence about risks of spinal manipulation comes from. In my view, it is not entirely correct: as there is no effective post-marketing surveillance, we cannot possibly name the incidence figures.
- Neck manipulations are clearly more risky than manipulations lower down. But this does not necessarily mean that back patients are safer than those with neck pain. Chiropractors view the spine as a whole organ and will regularly manipulate the neck (if they sense ‘subluxations’ in this area), even if the patient comes with low back pain.
- There are also indirect risks with consulting a chiropractor; for instance, they often give incompetent advice about healthcare. This can include discouraging immunisations or treating serious diseases, such as asthma, colic etc., with chiropractic.
- I think the article should point out that exercise is not just as effective (or as ineffective) as chiropractic, but it is much safer and less expensive.
- What Rubinstein says about responders is debatable, in my view. In particular, most chiropractors will convince their patients to continue treatment, even if they do not ‘respond’. And ‘responding’ might be simply the natural history of the condition and therefore totally unrelated to the therapy.
The bottom line: Chiropractic is not the best treatment for back pain!
US Republican Senator Hatch from Utah (born March 22, 1934) has announced that he is retiring after having been a Senator since 1977. When he leaves, the Senate “will lose its most ardent supporter of alternative medicine“. His decision comes after ‘The Salt Lake Tribune’ published a Christmas Day editorial calling on him to do so. The editorial stated that he has an “utter lack of integrity” that comes from “his unquenchable thirst for power.”

For advocates of alternative medicine, Hatch’s retirement comes as a blow: for decades, the senator has been one of the most powerful defender of quackery. As a young man, Orrin Hatch sold vitamins and supplements. As an old man, he takes them every day—including. “I really believe in them. I use them daily. They make me feel better, as they make millions of Americans feel better. And I hope they give me that little added edge as we work around here”, he was quoted stating.
And his love was returned: Between 1989 and 1994 Herbalife International gave Hatch $49,250; MetaboLife, $31,500; and Rexall Sundown, Nu Skin International, and Starlight International a total of $88,550. In addition, according to his financial disclosures for 2003, Hatch owned 35,621 shares of Pharmics, a Utah-based nutritional supplement company. In the early 1990s, Hatch’s son Scott began working for lobbying groups representing vitamin and supplement makers. Kevin McGuiness, Hatch’s former chief of staff, was also a lobbyist for the industry.
The NYT reported in 2011 that Hatch “was the chief author of a federal law enacted … that allows companies to make general health claims about their products, but exempts them from federal reviews of their safety or effectiveness before they go to market. During the Obama administration, Mr. Hatch has repeatedly intervened with his colleagues in Congress and federal regulators in Washington to fight proposed rules that industry officials consider objectionable…
“Mr. Hatch has been rewarded with hundreds of thousands of dollars in campaign contributions, political loyalty and corporate sponsorship of his favorite causes back home.
“His family and friends have benefited, too, from links to the supplement industry. His son Scott Hatch, is a longtime industry lobbyist in Washington, as are at least five of the senator’s former aides. Mr. Hatch’s grandson and son-in-law increase revenue at their chiropractic clinic near here by selling herbal and nutritional treatments, including $35 “thyroid dysfunction” injections and a weight-loss product, “Slim and Sassy Metabolic Blend.” And Mr. Hatch’s former law partner owns Pharmics, a small nutritional supplement company in Salt Lake City…”

Further information is provided by Wikipedia:
Hatch’s son Scott Hatch is a partner and registered lobbyist at Walker, Martin & Hatch LLC, a Washington lobbying firm. The firm was formed in 2001 with Jack Martin, a staff aide to Hatch for six years, and H. Laird Walker, described as a close associate of the senator. In March 2003, the Los Angeles Times reported that the firm was formed with Hatch’s personal encouragement and that he saw no conflict of interest in working on issues that involved his son’s clients. In 2009, the Washington Times reported that Hatch said “My son, Scott, does not lobby me or anyone in my office”.
In March 2009, the Washington Times reported that the pharmaceutical industry, which has benefited from Hatch’s legislative efforts, had previously unreported connections to Hatch. In 2007, five pharmaceutical companies and the industry’s main trade association, Pharmaceutical Research and Manufacturers of America (PhRMA), donated $172,500 to the Utah Families Foundation—a charitable foundation which Hatch helped start in the 1990s and has continued to support since. Walker, Martin & Hatch LLC was paid $120,000 by PhRMA in 2007 to lobby Congress on pending U.S. Food and Drug Administration legislation.
And finally:
Donald J. TrumpVerified account @realDonaldTrump Jan 2
We should not have to repeat this! But, as it is currently topical and certainly true, let me tell you again:
DETOX IS BUNK!
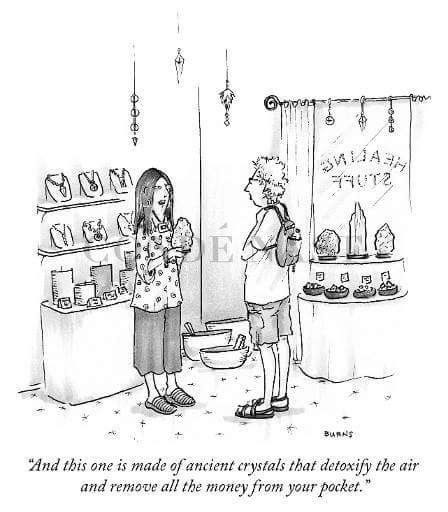
After the season of gluttony, it seems that half the population has fallen victim to the legion of alternative practitioners and entrepreneurs who claim that their particular form of quackery is ideally suited for detoxifying the body – and, sure enough, rid their clients of money instead of poisons. I have pointed out again and again why detox, as promoted in alternative medicine. is bogus and occasionally even harmful – see for instance here, here and here. And years ago, I published a review of the evidence on ‘alternative detox’ (AD); it concluded that “the principles of AD make no sense from a scientific perspective and there is no clinical evidence to support them. The promotion of AD treatments provides income for some entrepreneurs but has the potential to cause harm to patients and consumers. In alternative medicine, simplistic but incorrect concepts such as AD abound. All therapeutic claims should be scientifically tested before being advertised-and AD cannot be an exception.”
But I have, of course, many readers who do not trust a word I am putting on paper. So, please don’t take it from me, take it from others; read for example this recent article:
Detox diets are popular dieting strategies that claim to facilitate toxin elimination and weight loss, thereby promoting health and well-being. The present review examines whether detox diets are necessary, what they involve, whether they are effective and whether they present any dangers. Although the detox industry is booming, there is very little clinical evidence to support the use of these diets. A handful of clinical studies have shown that commercial detox diets enhance liver detoxification and eliminate persistent organic pollutants from the body, although these studies are hampered by flawed methodologies and small sample sizes. There is preliminary evidence to suggest that certain foods such as coriander, nori and olestra have detoxification properties, although the majority of these studies have been performed in animals. To the best of our knowledge, no randomised controlled trials have been conducted to assess the effectiveness of commercial detox diets in humans. This is an area that deserves attention so that consumers can be informed of the potential benefits and risks of detox programmes.
To the best of our knowledge, no randomised controlled trials have been conducted to assess the effectiveness of commercial detox diets in humans. I think that says enough; and it applies not just to detox diets, it applies to all detox methods promoted in alternative medicine.
DETOX IS BUNK!
Save your hard-earned money for stuff that is proven to work.
In 2017, Medline listed just over 1800 articles on ‘complementary alternative medicine’. If you find this number impressively high, consider that, for ‘surgery’ (a subject that has often been branded as less that active in conducting research), there were almost 18 000 Medline-listed papers.
So, the research activity in CAM is relatively small. Vis a vis the plethora of open questions, this inactivity is perhaps lamentable. What I find much more regrettable, however, is the near total lack of investigations into the ethical issues in CAM. In 2017, there were just 11 articles on Medline on ‘ethics and CAM’ (24393 articles on ‘ethics and surgery’).
One of the 11 papers that tackled the ethics directly and that was (in my opinion) one of the best is this article. Here is its concluding paragraph:
When we encounter patients who use or consider the use of complementary and/or alternative medicine, we should respect their autonomy while also fulfilling our obligations of beneficence and nonmaleficence. Physicians should become more knowledgeable about research on CAM therapies and approach discussions in an open, nonjudgmental manner to enhance patient trust. In situations where there is little risk of harm and the possibility of benefit, supporting a patient in their interest in complementary therapies can strengthen the patient-physician relationship. However, when a patient’s desire to utilize alternative therapies poses a health risk, physicians have the ethical obligation to skillfully counsel the patient toward those therapies that are medically appropriate.
I have had a long-lasting and keen interest in the ethics of CAM which resulted in the publication of many papers. Here is a selection:
‘Complementary & Alternative Medicine’ (CAM): Ethical And Policy Issues.
Pharmacists and homeopathic remedies.
Homeopathy, a “helpful placebo” or an unethical intervention?
Advice offered by practitioners of complementary/ alternative medicine: an important ethical issue.
The ethics of British professional homoeopaths.
Evidence-based practice in British complementary and alternative medicine: double standards?
Ethics of complementary medicine: practical issues.
Reporting of ethical standards: differences between complementary and orthodox medicine journals?
Informed consent: a potential dilemma for complementary medicine.
Ethical problems arising in evidence based complementary and alternative medicine.
Complementary medicine: implications for informed consent in general practice.
Ethics and complementary and alternative medicine.
Research ethics questioned in Qigong study.
Informed consent in complementary and alternative medicine.
The ethics of complementary medicine.
For most of the time conducting this research, I felt that I was almost alone in realising the importance of this topic. And all this time, I was convinced that the subject needed more attention and recognition. Therefore, I teamed up with with the excellent ethicist Kevin Smith from the University of Dundee, and together we spent the best part of 2017 writing about it.
Our book is entitled ‘MORE HARM THAN GOOD? THE MORAL MAZE OF COMPLEMENTARY AND ALTERNATIVE MEDICINE’ and will be published shortly by Springer.
It is an attempt to highlight some of the most important topics in this broad and under-researched area. While working on it, I was continually struck by the fact that most of the issues we have been struggling with on this blog are, in the final analysis, ethical by nature.
My hope is that, in 2018, we will see many more high quality papers filling the almost total void of ethical perspectives on CAM. In my view, it is unquestionably an area that needs to be addressed with some urgency.