You may have noticed that my patience with homeopathy, homeopaths, and other providers of so-called alternative medicine (SCAM) has diminished. In fact, I do not think much of quacks of all shades and no longer muster much understanding. It is better, so I mean after approximately 30 years of discussions with snake oil salesmen and other charlatans, to offer such people Parole. Facts are facts, and no one should be allowed to ignore that without contradiction.
That was not always the case.
When I began as Chair of Complementary Medicine at Exeter in 1993, I was optimistic. It was clear to me that my task of scrutinizing this field would not be easy and could occasionally bring me into conflict with enthusiasts. But I was determined to build bridges, to remain polite, and to muster as much understanding as necessary.
And so I began to build a multidisciplinary team, conduct research, and publish it. My goal was to do as rigorous science as possible and, if avoidable, not to step on anyone’s toes in the process. Especially with regard to homeopathy, my general attitude was quite positive. Accordingly, my articles were as favorable as the evidence allowed. My goal was to emphasize the good aspects of homeopathy wherever possible.
What, you find that hard to believe?
Then you are in good company!
Homeopaths like to claim that I was out to malign not only homeopathy but all of SCAM from the beginning. That this assumption is not true, I tried to demonstrate in an article entitled ‘Homeopathy and I’. In this paper, I merely extracted typical passages from my publications. From them, you can probably see how my attitude slowly changed over the years. See for yourself (sorry for the length of the list):
- 1. homeopathic remedies are believed by doctors and patients to be almost totally safe (Ernst E, White A. Br J Gen Pract 1995; 45: 629-30)
- 2. it might be argued that arnica … is ineffective but homeopathy may still work (Ernst E. BMJ 1995; 311: 510-1)
- 3. homeopathy, I fear, has soon to come up with … more convincing evidence (Ernst E. Forsch Komplementarmed 1995; 2: 32)
- 4. future evaluations of homeopathy should be performed to a high scientific standard (Ernst E. Br Homeopath J 1995; 84: 229)
- 5. the best way forward is clearly to do rigorous research (Ernst E, Kaptchuk TJ. Arch Intern Med 1996; 156: 2162-4)
- 6. the most pressing question, ‘Is homeopathy clinically more effective than placebo’, needs to be answered conclusively (Ernst E. Br J Clin Pharmacol 1997; 44: 435-7)
- 7. there is evidence that homeopathic treatment can reduce the duration of ileus (Barnes J, Resch KL, Ernst E. J Clin Gastroenterol 1997; 25: 628-33)
- 8. the published evidence to date does not support the hypothesis that homeopathic remedies … are more efficacious than placebo (Ernst E, Barnes J. Perfusion 1998; 11: 4-8)
- 9. the claim that homeopathic arnica is efficacious beyond a placebo effect is not supported by rigorous clinical trials (Ernst E, Pittler MH. Arch Surg 1998; 133: 1187-90)
- 10. … the trial data … do not suggest that homeopathy is effective (Ernst E. J Pain Sympt Manage 1999; 18: 353-7)
- 11. … the re-analysis of Linde et al. can be seen as the ultimate epidemiological proof that homeopathic remedies are, in fact, placebos (Ernst E, Pittler MH.J Clin Epidemiol 2000; 53: 1188)
- 12. … homeopathy is not different from placebo (Ernst E, Pittler MH. J Clin Epidemiol 2002; 55: 103-4)
- 13. … the best clinical evidence … does not warrant positive recommendations (Ernst E. Br J Clin Pharmacol 2002; 54: 577-82)
- 14. the results of this trial do not suggest that homeopathic arnica has an advantage over placebo (Stevinson C, Devaraj VS, Fountain-Barber A, Hawkins S, Ernst E. J R Soc Med 2003; 96: 60-5)
- 15. this study provides no evidence that adjunctive homeopathic remedies … are superior to placebo (White A, Slade P, Hunt C, Hart A, Ernst E. Thorax 2003; 58: 317-21)
- 16. … this systematic review does not provide clear evidence that the phenomenon of homeopathic aggravations exists (Grabia S, Ernst E. Homeopathy 2003; 92: 92-8)
- 17. … the proven benefits of highly dilute homeopathic remedies … do not outweigh the potential for harm (Ernst E.Trends Pharmacol Sci 2005; 26: 547-8)
- 18 Our analysis … found insufficient evidence to support clinical efficacy of homeopathic therapy (Milazzo S, Russell N, Ernst E. Eur J Cancer 2006; 42: 282-9)
- 19. … promotion can be regrettably misleading, or their effectiveness? (Ernst E. J Soc Integr Oncol 2006; 4: 113-5)
- 20. … homeopathy is not based on solid evidence and, over time, this evidence seems to get more negative (Ernst E, Pittler MH, Wider B, Boddy K. Perfusion 2006; 19: 380-2)
- 21. the evidence from rigorous clinical trials … testing homeopathy for childhood and adolescence ailments is not convincing enough for recommendations in any condition (Altunc U, Pittler MH, Ernst E. Mayo Clin Proc 2007; 82: 69-75)
- 22. … context effects of homeopathy … are entirely sufficient to explain the benefit many patients experience (Ernst E. Curr Oncol 2007; 14: 128-30)
- 23. among all the placebos that exist, homeopathy has the potential to be an exceptionally powerful one (Ernst E. Br J Clin Pharmacol 2008; 65: 163-4)
- 24. … recommendations by professional homeopathic associations are not based on the evidence (Ernst E. Br J Gen Pract 2009; 59: 142-3)
These quotes speak for themselves, I think. But what was the reason for the change? As far as I can judge in retrospect, there were three main reasons.
1. The data became clearer and clearer
When I started researching homeopathy, at least the clinical evidence was not clearly negative. In 1991, Jos Kleinjen had published his much-noted systematic review in the BMJ. Here is its conclusion:
At the moment the evidence of clinical trials is positive but not sufficient to draw definitive conclusions because most trials are of low methodological quality and because of the unknown role of publication bias. This indicates that there is a legitimate case for further evaluation of homoeopathy, but only by means of well performed trials.
Subsequently, more and better clinical trials were published, and the overall picture became increasingly negative. Kleinjen, who had become somewhat of a hero in the realm of homeopathy, re-reviewed the evidence in 2000 and concluded that there are currently insufficient data to either recommend homoeopathy as a treatment for any specific condition or to warrant significant changes in the provision of homoeopathy.
The 24 citations above reflect this development quite nicely. Today, there is no longer much doubt that highly-diluted homeopathic remedies are pure placebos. This is perhaps most clearly expressed in the now numerous statements of high-ranking international bodies.
2. The lack of understanding on the part of homeopaths
So the evidence is now clear. But it may not fully explain why my patience with homeopaths diminished. To understand this better, one must consider the utter lack of insight of today’s homeopaths (think, for example, of the incredible Ebola story).
It is of course understandable that a homeopath would be less than enthusiastic about the increasingly negative evidence. But homeopaths are also physicians or at least medically untrained practitioners (lay homeopaths). As such, they have an obligation to acknowledge the overwhelming evidence and act accordingly. That they quite obviously do not do so, is not only regrettable but also highly unethical and shameful. In any case, I find it difficult to have much patience for such people.
3. Personal attacks
In the many years that I have now been scrutinizing SCAM, I have become used to being attacked. The attacks and insults I have received, especially from homeopaths, are legion. For example, when we published our arnica study, we were threatened with letter bombs. However, one should keep one thing in mind: ad hominem attacks are a victory of reason over unreason. If one is personally attacked by one’s opponent, it only shows that he has run out of rational arguments.
Perhaps the most impressive example of an attack was not directed against me personally, but across the board against all who dare to doubt homeopathy. Christian Boiron is the boss of the world’s largest homeopathic manufacturer, Boiron. In an interview he was once asked what he thought of homeopathy critics; his answer: “Il y a un Ku Klux Klan contre l’homéopathie” (There is a Ku Klux Klan against homeopathy).
Yes, many of these attacks even have something comical about them; nevertheless, they are not likely to increase my patience with homeopaths. This does not mean, however, that I will soon hang my opponents from the nearest tree in the old KKK tradition. I’ll gladly leave such tasteless ideas to Christian Boiron.
Acupuncture has been widely used for acute low back pain (LBP), yet there remains continued controversy regarding its efficacy. Therefore, this systematic review aimed at evaluating the evidence.
English and Chinese databases were searched for randomized controlled trials (RCTs) of acupuncture for acute LBP published up to May 2020. Data on the outcomes of pain intensity, functional status, and analgesic use were extracted. The meta-analysis was performed using the Cochrane Collaboration’s RevMan 5.3, and pooled data were expressed as mean differences (MD) with 95% confidence intervals (CIs).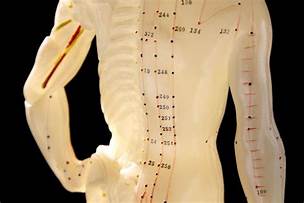
Of the 13 eligible RCTs identified, 9 were from China, one each from Brazil, the United Kingdom, Australia, and South Korea. Four studies were published in English, and 9 were published in Chinese. The 13 RCTs (involving 707 patients) provided moderate-quality evidence that acupuncture has a statistically significant association with improvements in VAS (visual analog scale) score [MD: −1.75 (95% CI: −2.39, −1.12)]. Two studies indicated that acupuncture did not influence the RMDQ (Roland-Morris Disability Questionnaire) scores more than the control treatment [MD: −2.34 (95% CI: −5.34, 0.67)]. Three studies suggested that acupuncture influenced the ODI (Oswestry Disability Index) scores more than the control treatment [MD: −12.84 (95% CI: −23.94, −1.74)]. Two studies suggested that acupuncture influenced the number of pills more than the control treatment [MD: −3.19 (95% CI: −3.45, −2.92)]. Merely 2 RCTs were sham-controlled and only 4 of the 13 RCTs mentioned adverse effects.
The authors concluded that acupuncture treatment of acute LBP was associated with modest improvements in the VAS score, ODI score, and the number of pills, but not the RMDQ score. Our findings should be considered with caution due to the low power original studies. High-quality trials are needed to assess further the role of
acupuncture in the treatment of acute LBP.
I do appreciate the authors’ call for caution in interpreting the findings. Yet, I feel that much more caution than the authors advise is needed here:
- Most studies are from China, and we have often seen that these trials cannot be trusted.
- Only 2 RCTs are sham-controlled which means that most studies failed to control for placebo effects.
- Most studies do not mention adverse effects, confirming the unethically low standards of these investigations.
I am afraid that this new review does not inspire me with confidence that acupuncture is an effective therapy for acute LBP.
A few months ago, I started contributing to a German blog. This has been fun but only moderately successful in terms of readership. This week, I posted something about a homeopath and his strange attitude towards COVID vaccinations. This post was so far read by around 20 000 people!
As it was so unusually successful (and because there is a big conference today on the subject), I decided to translate it for my non-German readers.
Here we go:
A lot of downright silly stuff is currently being written about vaccine side effects at the moment, not least on Twitter where I recently found the following comment from a medical colleague:
I’ve been a doctor for 25 years now. I have never experienced such an amount of vaccine side effects. I can’t imagine that other colleagues feel differently.
This kind of remark naturally makes you think. So let’s think a little bit about these two sentences. In particular, I would like to ask and briefly answer the following questions:
- How reliable is this physician’s impression?
- What does the reliable evidence say?
- Is it conceivable that this doctor is mistaken?
- What might be the causes of his error?
- Who is the author?
- Why is the tweet questionable?
1. How reliable is this doctor’s impression?
A whole 25 years of professional experience! So we are dealing with a thoroughly experienced doctor. His statement about the current unusually large amount of vaccination side effects should therefore be correct. Nevertheless, one should perhaps bear in mind that the incidence of side effects cannot be determined by rough estimations, but must be precisely quantified. In addition, we also need data on the severity and duration of symptoms. For example, is it only mild pain at the injection site or venous thrombosis? Are the symptoms only temporary, long-lasting, or even permanent? In general, it must be said that the experience of a physician, while not completely insignificant, does not constitute evidence. Oscar Wilde once said, “experience is the name we give to our mistakes.”
2. What does the reliable evidence tell us?
Even if the good doctor had 100 years of professional experience and even if he could accurately characterize the side effects, his experience would be trivial compared to the hard data we have on this subject. Nearly 2 billion vaccinations have now been performed worldwide, and we are therefore in the fortunate position of having reliable statistics to guide us. And they show that side effects such as pain at the injection site, fatigue, and headaches are quite common, while serious problems are very rare.[1] A recent summary comes to the following conclusion (my translation)[2]:
The current data suggests that the currently approved mRNA-based COVID-19 vaccines are safe and effective for the vast majority of the population. Furthermore, broad-based vaccine uptake is critical for achieving herd immunity; an essential factor in decreasing future surges of COVID-19 infections. Ensuring sufficient COVID-19 vaccination adoption by the public will involve attending to the rising vaccine hesitancy among a pandemic-weary population. Evidence-based approaches at the federal, state, city, and organizational levels are necessary to improve vaccination efforts and to decrease hesitancy. Educating the general public about the safety of the current and forthcoming vaccines is of vital consequence to public health and ongoing and future large-scale vaccination initiatives.
3. Is it conceivable that this doctor is mistaken?
In answering this question, I agree with Oscar Wilde. The evidence very clearly contradicts the physician’s impression. So the doctor seems to be mistaken — at least about the incidence of side effects that are not completely normal and thus to be expected. Even if indeed ‘other colleagues feel no differently’, such a cumulative experience would still mislead us. The plural of ‘anecdote’ is ‘anecdotes’ and not ‘evidence’.
4. What might be the causes of his error?
I wonder whether our doctor perhaps did not see or did not want to see the following circumstance: It is inevitable that a physician, at a time when soon 50% of all Germans were vaccinated, also sees a lot of patients complaining about side effects. He has never seen anything like that in his 25-year career! That’s because we haven’t been hit by a pandemic in the last 25 years. For a similar reason, the colleague will treat far fewer frostbites in midsummer than during a severe winter. The only surprising thing would be not to see more patients reporting vaccine side effects during the biggest vaccination campaign ever.
5. Who is the author?
At this point, we should ask, who is actually the author and author of the above tweet? Perhaps the answer to this question will provide insight into his motivation for spreading nonsense? Dr. Thomas Quak (no, I did not invent the name) is a practicing homeopath in Fürstenfeldbruck, Germany. Like many homeopaths, this Quak probably has a somewhat disturbed relationship to vaccination. In his case, this goes as far as recommending several vaccine-critical machinations on his website and even offering ‘critical vaccination advice’ as a special service.[3]
Now we can immediately put the Quak tweet in a better perspective. Dr. Quak is a vaccination opponent or critic and wants to warn the public: for heaven’s sake, don’t get vaccinated folks; side effects are more common than ever!!!! Therefore, he also conceals the fact that the side-effects are completely normal, short-term vaccination reactions, which are ultimately of no significance.
6. Why is the tweet concerning?
Perhaps you feel that the Quak and his Quack tweet are irrelevant? What harm can a single tweet do, and who cares about a homeopath from Fürstenfeldbruck? As good as none and nobody! However, the importance does not lie in a single homeopath unsettling the population; it consists in the fact that such things currently happen every day thousandfold.
In their narrow-mindedness, vaccination opponents of all shades want to make us believe that they are concerned about our well-being because they know more than we and all the experts (who are of course bought by the pharmaceutical industry). But if you scratch just a little at the surface of their superficiality, it turns out that the exact opposite is true. They are ill-informed and only interested in spreading their hare-brained, misanthropic ideology.
And why do homeopaths do this? There are certainly several reasons. Although Hahnemann himself was impressed by the success of vaccination, which was invented in his time and hailed as a breakthrough, most of his successors soon sided with vaccination critics. Many do so by warning (like our Quak) of side effects, thinking that they are thus protecting their patients. However, they ignore two very important points:
- Even if the dangers of vaccinations were much greater than they actually are (no one is claiming that they are completely harmless), the benefits would still far outweigh the potential harms.
- If the Quaks (and all the quacks) of this world succeeded in dissuading a sizable percentage of the population from vaccinating and thus save them from the ‘oh-so-dangerous side effects’, they would still be doing a real disservice to public health. With regard to COVID-19, this would mean that the pandemic would remain with us in the long term and cost many more lives.
Whatever the motives of the homeopathic anti-vax brigade, it is certain that their attitude is a threat to our health. This has repeatedly made me state:
The homeopathic pills may be harmless, but unfortunately, the homeopaths are not!
REFERENCES
- COVID-19 vaccine availability: what are the side effects? | British Journal of General Practice (bjgp.org) ︎
- Review the safety of Covid-19 mRNA vaccines: a review – PubMed (nih.gov) ︎
- Vaccination Information (doktor-quak.de) ︎
The integration of so-called alternative medicine (SCAM) into cancer care may reduce the adverse effects of anti-neoplastic treatment but also cause new problems and non-adherence to conventional treatment. Therefore, its net benefit is questionable.
The aim of this randomized controlled study was to investigate the impact of integrative open dialogue about SCAM on cancer patients’ health and quality of life (QoL).
Patients undergoing curative or palliative anti-neoplastic treatment were randomly assigned to standard care (SC) plus SCAM or SC alone. A nurse specialist facilitated SCAM in one or two sessions. The primary endpoint was the
frequency of grade 3–4 adverse events (AE) eight weeks after enrollment. Secondary endpoints were the frequency of grade 1–4 AE and patient-reported QoL, psychological distress, perceived information, attitude towards and use of SCAM 12 and 24 weeks after enrollment. Survival was analyzed post-hoc.
Fifty-seven patients were randomized to SCAM and 55 to SC. No significant differences were found in terms of AEs of cancer patients. A trend towards better QoL, improved survival, and a lower level of anxiety was found in the SCAM group.
The authors concluded that integration of SCAM into daily oncology care is feasible. IOD-CAM was not superior to SC in reducing the frequency of grade 3-4 AEs, but it did not compromise patient safety. Implementation of SCAM
may improve the QoL, anxiety, and emotional well-being of the patients by reducing the level of nausea, vomiting and diarrhea. Finally, SCAM potentially improves the patients’ self-care, which contributes to
increased treatment adherence and improved survival.
This is an interesting paper with a very odd conclusion. The positive trends found failed to be statistically significant. Why employ statistics only to ignore them in our interpretation of the findings?
I can well imagine that the integration of effective treatments into cancer care improves the outcome. I have no problem with this at all – except it is not called INTEGRATIVE MEDICINE but EVIDENCE-BASED MEDICINE!!! If we integrate dubious treatments into cancer care, it’s called INTEGRATIVE MEDICINE, and it’s unlikely to do any good.
In my view, this small study showed just one thing:
Integrative medicine does not reduce adverse effects in cancer patients.
Research can be defined as the process of discovering new knowledge. There are three somewhat overlapping types of research:
- Exploratory research is research around a problem that has not yet been clearly defined. It aims to gain a better understanding of the nature of the issues involved with a view of conducting more in-depth research at a later stage.
- Descriptive research creates knowledge by describing the issues according to their characteristics and population. It focuses on the ‘how’ and ‘what’, but not on the ‘why’.
- Explanatory research is aimed at determining how variables interact and at identifying cause-and-effect relationships. It deals with the ‘why’ of research questions and is therefore often based on experiments.
The motivation behind doing research in medicine does, of course, vary but essentially it should be to help advance our knowledge and thus create progress.
I have been a researcher in several areas of medicine: physical medicine and rehabilitation, blood rheology, so-called alternative medicine (SCAM). My kind of research was mostly the explanatory type, i.e. formulating a research question and trying to answer it. Looking back at my ~40 years as an active researcher, I find remarkable differences between doing research in SCAM and the other subjects.
The process of discovering new knowledge is rarely contentious. New knowledge may be useful or useless but it should not generate contention. Of course, there can be debates about the reliability of the findings; this is entirely legitimate, helpful, and necessary. We always need to make sure that results are valid, reproducible, and true. And of course, the debates about the quality of the data can generate a certain amount of tension. Such tensions are stimulating and must be welcomed. I have been lucky to have experienced them in all areas of the research I ever touched.
The tension I experienced while doing SCAM research, however, was of an entirely different nature – so much so that I would not even call it ‘tension’; it was outright hostility. While doing non-SCAM research, it had never been in doubt that my research was honestly aimed at creating progress, this issue became the focal point after I had started SCAM research.
- When my research showed that homeopathy might not be effective, I got PERSONALLY attacked by homeopaths.
- When my research showed that homeopathy might not be safe, I got PERSONALLY attacked by homeopaths.
- When my research showed that chiropractic might not be effective, I got PERSONALLY attacked by chiropractors.
- When my research showed that chiropractic might not be safe, I got PERSONALLY attacked by chiropractors.
- When my research showed that acupuncture might not be effective, I got PERSONALLY attacked by acupuncturists.
- When my research showed that acupuncture might not be safe, I got PERSONALLY attacked by acupuncturists.
- When my research showed that herbalism might not be effective, I got PERSONALLY attacked by herbalists.
- When my research showed that herbalism might not be safe, I got PERSONALLY attacked by herbalists.
- Etc., etc.
Essentially, doing SCAM research felt like doing research not FOR but AGAINST the will of those who should have had the most interest in it.
But why?
As I said, one way to describe research is as a process of discovering new knowledge and creating progress. The main difference between doing research in SCAM and non-SCAM areas is perhaps this: in medicine, almost everyone is interested in discovering new knowledge and creating progress, while in SCAM hardly anyone shares this interest. In SCAM, I now tend to feel, research is not understood as a tool for finding the truth, but one for generating more business. To put it even more bluntly: medicine, in general, is open to research and its consequences hoping to make progress; SCAM is mostly anti-science and not interested in progress.
But why?
To me, the answer seems obvious: the truth or progress would be bad for the business of SCAM.
Prince Charles has claimed that people struggling to return to full health after having the coronavirus should practice yoga. This is what the GUARDIAN reported about it on Friday:
In a video statement on Friday to the virtual yoga and healthcare symposium Wellness After Covid, the heir apparent said doctors should work together with “complementary healthcare specialists” to “build a roadmap to hope and healing” after Covid. “This pandemic has emphasised the importance of preparedness, resilience and the need for an approach which addresses the health and welfare of the whole person as part of society, and which does not merely focus on the symptoms alone,” Charles said. “As part of that approach, therapeutic, evidenced-informed yoga can contribute to health and healing. By its very nature, yoga is an accessible practice which provides practitioners with ways to manage stress, build resilience and promote healing…”
… Charles, who has previously espoused the benefits of yoga, is not the only fan in the royal family. His wife, the Duchess of Cornwall, has said “it makes you less stiff” and “more supple”, while Prince William has also been pictured doing yogic poses. In 2019, the Prince of Wales said yoga had “proven beneficial effects on both body and mind”, and delivered “tremendous social benefits” that help build “discipline, self-reliance and self-care”.
__________________
END OF QUOTE
Yoga is a complex subject because it entails a host of different techniques, attitudes, and life-styles. There have been numerous clinical trials of various yoga techniques. They tend to suffer from poor study design as well as incomplete reporting and are thus no always reliable. Several systematic reviews have summarised the findings of these studies. A 2010 overview included 21 systematic reviews relating to a wide range of conditions. Nine systematic reviews arrived at positive conclusions, but many were associated with a high risk of bias. Unanimously positive evidence emerged only for depression and cardiovascular risk reduction.[1] There is no evidence that yoga speeds the recovery after COVID-19 or any other severe infectious disease, as Charles suggested.
Yoga is generally considered to be safe. However, a large-scale survey found that approximately 30% of yoga class attendees had experienced some type of adverse event. Although the majority had mild symptoms, the survey results indicated that patients with chronic diseases were more likely to experience adverse events.[2] It, therefore, seems unlikely that yoga is suited for many patients recovering from a COVID-19 infection.
The warning by the Vatican’s chief exorcist that yoga leads to ‘demonic possession’[3] might not be taken seriously by rational thinkers. Yet, experts have long warned that many yoga teachers try to recruit their clients into the more cult-like aspects of yoga.[4]
Perhaps the most remarkable expression in Charles’ quotes is the term ‘EVIDENCE-INFORMED‘. It crops up regularly when Charles (or his advisor Dr. Michael Dixon) speaks or writes about so-called alternative medicine (SCAM). It is a clever term that sounds almost like ‘evidence-based’ but means something entirely different. If a SCAM is not evidence-based, it can still be legitimately put under the umbrella of ‘evidence-informed’: we know the evidence is not positive, we were well-informed of this fact, we nevertheless conclude that yoga (or any other SCAM) might be a good idea!
In my view, the regular use of the term ‘evidence-informed’ in the realm of SCAM discloses a lack of clarity that suits all snake-oil salesmen very well.
[1] Ernst E, Lee MS: Focus on Alternative and Complementary Therapies Volume 15(4) December 2010 274–27
[2] Matsushita T, Oka T. A large-scale survey of adverse events experienced in yoga classes. Biopsychosoc Med. 2015 Mar 18;9:9. doi: 10.1186/s13030-015-0037-1. PMID: 25844090; PMCID: PMC4384376.
[3] https://www.social-consciousness.com/2017/06/vaticans-chief-exorcist-warns-that-yoga-causes-demonic-possession.html
[4] https://www.theguardian.com/lifeandstyle/2020/jun/26/experience-my-yoga-class-turned-out-to-be-a-cult
The Indian AYUSH ministry has a track record of doing irresponsible stuff. Now they have published guidelines for treating Mucormycosis (black fungus) with homeopathy. Allow me to show you the crucial passages of their announcement:
… With the increasing cases of special variety of fungal infection, Mucormycosis (black fungus) the present information have been prepared with experience of senior clinicians in treating specific fungal infections and researchers of the system, for efficient treatment of suspected and diagnosed cases of Mucormycosis with Homoeopathy. This condition requires hospital based treatment under supervision and Homoeopathic medicines can be prescribed in an integrated manner. Since mostly immune compromised patients get this infection, strict monitoring of blood sugar and other vitals is required…
As a system with holistic approach, homoeopathy medicines may be selected based on the presenting signs and symptoms of each patient(4). Fungal infections are amenable to homoeopathic treatment. Various research studies undertaken on various fungi in-vitro model showed that homoeopathy medicine could prevent the growth of the fungus(5-8). Clinical studies have shown encouraging results on fungal infections (9-10). The medicines given here are suggestive based on their clinical use.
Symptomatic Homoeopathy management of Suspected and Diagnosed cases of Mucormycosis-
Note: -Apart from these lists of medicines any other medicine and any other potency may be
prescribed based on the symptom similarity in each case.
__________________________
END OF QUOTE
Mucormycosis (black fungus) is a disease of immunocompromised patients. Five types can be differentiated:
- rhinocerebral (most common),
- pulmonary,
- cutaneous,
- disseminated,
- gastrointestinal (rare).
Rhinocerebral mucormycosis commonly causes headaches, visual changes, sinusitis, and proptosis. Pulmonary mucormycosis commonly presents as a cough. Late diagnosis may result in dissemination, leading to high mortality. Treatment consists of amphotericin B, surgery, and immune restoration.
It is believed that the current surge of mucormycosis in India has an overall mortality rate of 50% and is triggered by the use of steroids which are often life-saving for critically ill Covid-19 patients. It almost goes without saying that homeopathy has not been shown to be effective against this (or any other) condition. As to the AYUSH ministry, the less they interfere with public health in India, the better for the survival of patients, I fear.
Post-traumatic stress disorder (PTSD), previously known as battle fatigue syndrome or shell shock, is a condition that can be triggered by the experience of some frightening event. PTSD can be debilitating leading to the production of feelings of helplessness, intense fear, and horror. Numerous treatments of PTSD exist but few have been shown to be truly effective. A team of Canadian researchers explored the effects of cannabis on PTSD symptoms, quality of life (QOL), and return to work (RTW). Their systematic review also investigated harms such as adverse effects and dropouts due to adverse effects, inefficacy, and all-cause dropout rates.
Their electronic searches located one RCT and 10 observational studies (n = 4672). Risk of bias (RoB) was assessed with the Cochrane risk of bias tool and ROBINS-I. Evidence from the included studies was mainly based on studies with no comparators. Results from unpooled, high RoB studies suggested that cannabis was associated with a reduction in overall PTSD symptoms and improved QOL. Dry mouth, headaches, and psychoactive effects such as agitation and euphoria were the most commonly reported adverse effects. In most studies, cannabis was well tolerated. A small proportion of patients experienced a worsening of PTSD symptoms.
The authors concluded that the evidence in the current study primarily stems from low quality and high RoB observational studies. Further RCTs investigating cannabis effects on PTSD treatment should be conducted with larger sample sizes and explore a broader range of patient-important outcomes.
Various drugs are currently used for the treatment of PTSD including selective serotonin reuptake inhibitors; tricyclic antidepressants (amitriptyline and isocarboxazid); mood stabilizers (Divalproex and lamotrigine); atypical antipsychotics (aripiprazole and quetiapine) but their effectiveness has not been proven. A recent systematic review included 30 RCTs of a range of heterogeneous non-psychological and non-pharmacological interventions. There was emerging evidence for 6 different approaches:
- acupuncture,
- neurofeedback,
- saikokeishikankyoto (a herbal preparation),
- somatic experiencing,
- transcranial magnetic stimulation,
- yoga.
This list makes me wonder: are these treatments, including cannabis, truly promising, or is PTSD one of those conditions for which nearly every treatment works a little because of its placebo effect?
Google Scholar is quite a fantastic tool; I recently (20/5/2021) glanced at my own profile and decided to have a closer look at the 100 of my papers that have been cited most frequently. The list below shows these ‘top 100’; in the 1st column is the reference (title of the article, authors, journal). In the MIDDLE column are the numbers of times each paper has been cited (if you click on it, you see the articles that cited the paper in question), and the far-right column tells you the year of publication.
Here we go:
| Interactions between herbal medicines and prescribed drugs. AA Izzo, E Ernst: Drugs 61 (15), 2163-2175 | 1608* | 2001 |
| Influence of context effects on health outcomes: a systematic review. Z Di Blasi, E Harkness, E Ernst, A Georgiou, J Kleijnen: Lancet 357 (9258), 757-762 | 1564 | 2001 |
| Fibrinogen as a cardiovascular risk factor: a meta-analysis and review of the literature. E Ernst, KL Resch: Annals of internal medicine 118 (12), 956-963 | 1544 | 1993 |
| The prevalence of complementary/alternative medicine in cancer: a systematic review. E Ernst, B Cassileth: Cancer: Interdisciplinary International Journal of the American Cancer | 1173 | 1998 |
| The desktop guide to complementary and alternative medicine: an evidence-based approach. E Ernst, MH Pittler, C Stevinson, A White | 854 | 2001 |
| Harmless herbs? A review of the recent literature. E Ernst: The American journal of medicine 104 (2), 170-178 | 852 | 1998 |
| The desktop guide to complementary and alternative medicine: an evidence-based approach. E Ernst, MH Pittler, C Stevinson, A White | 837 | 2001 |
| Aloe vera: a systematic review of its clinical effectiveness. BK Vogler, E Ernst: British journal of general practice 49 (447), 823-828 | 767 | 1999 |
| Leukocytes and the risk of ischemic diseases. E Ernst, DE Hammerschmidt, U Bagge, A Matrai, JA Dormandy: Jama 257 (17), 2318-2324 | 754 | 1987 |
| The Risk–Benefit Profile of Commonly Used Herbal Therapies: Ginkgo, St. John’s Wort, Ginseng, Echinacea, Saw Palmetto, and Kava. E Ernst: Annals of internal medicine 136 (1), 42-53 | 726 | 2002 |
| Prevalence of use of complementary/alternative medicine: a systematic review. E Ernst: Bulletin of the world health organization 78, 258-266 | 725 | 2000 |
| The BBC survey of complementary medicine use in the UK. E Ernst, A White: Complementary therapies in medicine 8 (1), 32-36 | 646 | 2000 |
| The efficacy of “distant healing”: a systematic review of randomized trials. JA Astin, E Harkness, E Ernst: Parapsychology, 433-440 | 633 | 2017 |
| Toxic heavy metals and undeclared drugs in Asian herbal medicines. E Ernst: Trends in pharmacological sciences 23 (3), 136-139 | 630 | 2002 |
| Efficacy of ginger for nausea and vomiting: a systematic review of randomized clinical trials. E Ernst, MH Pittler: British journal of anaesthesia 84 (3), 367-371 | 623 | 2000 |
| Meta-analysis: acupuncture for low back pain. E Manheimer, A White, B Berman, K Forys, E Ernst: Annals of internal medicine 142 (8), 651-663 | 600 | 2005 |
| Garlic for treating hypercholesterolemia: a meta-analysis of randomized clinical trials
C Stevinson, MH Pittler, E Ernst: Annals of internal medicine 133 (6), 420-429 |
550 | 2000 |
| Bringing medicinal plants into cultivation: opportunities and challenges for biotechnology. PH Canter, H Thomas, E Ernst: TRENDS in Biotechnology 23 (4), 180-185 | 524 | 2005 |
| St John’s wort: Prozac from the plant kingdom. G Di Carlo, F Borrelli, E Ernst, AA Izzo: Trends in Pharmacological Sciences 22 (6), 292-297 | 500* | 2001 |
| Adverse events following acupuncture: prospective survey of 32 000 consultations with doctors and physiotherapists. A White, S Hayhoe, A Hart, E Ernst: Bmj 323 (7311), 485-486 | 498 | 2001 |
| Concept of true and perceived placebo effects. E Ernst, KL Resch: Bmj 311 (7004), 551-553 | 495 | 1995 |
| A systematic review of systematic reviews of homeopathy. E Ernst: British journal of clinical pharmacology 54 (6), 577-582 | 482 | 2002 |
| Aromatherapy: a systematic review. B Cooke, E Ernst: British journal of general practice 50 (455), 493-496 | 476 | 2000 |
| The efficacy of ginseng. A systematic review of randomised clinical trials. BK Vogler, MH Pittler, E Ernst: European journal of clinical pharmacology 55 (8), 567-575 | 476 | 1999 |
| Second thoughts about safety of St John’s wort. E Ernst: Lancet 354 (9195), 2014-2016 | 475 | 1999 |
| Dietary supplements for body-weight reduction: a systematic review. MH Pittler, E Ernst: The American journal of clinical nutrition 79 (4), 529-536 | 473 | 2004 |
| Herb–drug interactions: review and assessment of report reliability. A Fugh‐Berman, E Ernst: British journal of clinical pharmacology 52 (5), 587-595 | 468 | 2001 |
| Acupuncture for back pain: a meta-analysis of randomized controlled trials. E Ernst, AR White: Archives of internal medicine 158 (20), 2235-2241 | 421 | 1998 |
| Prospective studies of the safety of acupuncture: a systematic review. E Ernst, AR White: The American journal of medicine 110 (6), 481-485 | 411 | 2001 |
| Panax ginseng, JT Coon, E Ernst: Drug safety 25 (5), 323-344 | 408 | 2002 |
| The role of complementary and alternative medicine. E Ernst: Bmj 321 (7269), 1133 | 404 | 2000 |
| Review of randomised controlled trials of traditional Chinese medicine. JL Tang, SY Zhan, E Ernst: Bmj 319 (7203), 160-161 | 388 | 1999 |
| Peppermint oil for irritable bowel syndrome: a critical review and metaanalysis. MH Pittler, E Ernst: The American journal of gastroenterology 93 (7), 1131-1135 | 384 | 1998 |
| Yohimbine for erectile dysfunction: a systematic review and meta-analysis of randomized clinical trials. E Ernst, MH Pittler: The Journal of urology 159 (2), 433-436 | 380 | 1998 |
| Trick or treatment: The undeniable facts about alternative medicine. S Singh, E Ernst: WW Norton & Company | 379* | 2008 |
| Prospective investigation of adverse effects of acupuncture in 97 733 patients. D Melchart, W Weidenhammer, A Streng, S Reitmayr, A Hoppe, E Ernst: Archives of internal medicine 164 (1), 104-105 | 375 | 2004 |
| Adulteration of Chinese herbal medicines with synthetic drugs: a systematic review. E Ernst: Journal of internal medicine 252 (2), 107-113 | 374 | 2002 |
| Mindfulness-based cognitive therapy: evaluating current evidence and informing future research. HF Coelho, PH Canter, E Ernst. Educational Publishing Foundation 1 (S), 97 | 362 | 2013 |
| Acupuncture–a critical analysis. E Ernst: J. Intern Med 259 (2), 125-137 | 357 | 2006 |
| Acupuncture for treating acute ankle sprains in adults. TH Kim, MS Lee, KH Kim, JW Kang, TY Choi, E Ernst: Cochrane database of systematic reviews | 353* | 2014 |
| Kava extract versus placebo for treating anxiety. MH Pittler, E Ernst:Cochrane Database of Systematic Reviews | 352 | 2003 |
| Methods for causality assessment of adverse drug reactions. TB Agbabiaka, J Savović, E Ernst: Drug safety 31 (1), 21-37 | 348 | 2008 |
| Efficacy of kava extract for treating anxiety: systematic review and meta-analysis. MH Pittler, E Ernst: Journal of clinical psychopharmacology 20 (1), 84-89 | 345 | 2000 |
| Horse chestnut seed extract for chronic venous insufficiency. MH Pittler, E Ernst: Cochrane database of systematic reviews | 341 | 2012 |
| A systematic review of randomized controlled trials of acupuncture for neck pain. AR White, E Ernst: Rheumatology (Oxford, England) 38 (2), 143-147 | 334 | 1999 |
| Cardiovascular pharmacotherapy and herbal medicines: the risk of drug interaction. AA Izzo, G Di Carlo, F Borrelli, E Ernst: International journal of cardiology 98 (1), 1-14 | 333 | 2005 |
| Ice freezes pain? A review of the clinical effectiveness of analgesic cold therapy. E Ernst, V Fialka: Journal of pain and symptom management 9 (1), 56-59 | 332 | 1994 |
| Complementary medicine—a definition. E Ernst, KL Resch, S Mills, R Hill, A Mitchell, M Willoughby, A White: The British Journal of General Practice 45 (398), 506 | 331 | 1995 |
| Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. D Moher, A Liberati, J Tetzlaff, DG Altman, D Altman, G Antes, D Atkins, … Journal of Chinese Integrative Medicine 7 (9), 889-896 | 327 | 2009 |
| Validating a new non-penetrating sham acupuncture device: two randomised controlled trials. J Park, A White, C Stevinson, E Ernst, M James: Acupuncture in Medicine 20 (4), 168-174 | 324 | 2002 |
| Herbal medicinal products during pregnancy: are they safe? E Ernst: BJOG: An International Journal of Obstetrics & Gynaecology 109 (3), 227-235 | 322 | 2002 |
| Adverse effects of herbal drugs in dermatology. E Ernst: British Journal of Dermatology 143 (5), 923-929 | 319 | 2000 |
| Plasma fibrinogen—an independent cardiovascular risk factor. E Ernst: Journal of internal medicine 227 (6), 365-372 | 317 | 1990 |
| Green tea (Camellia sinensis) for the prevention of cancer: K Boehm, F Borrelli, E Ernst, G Habacher, SK Hung, S Milazzo, … Cochrane Database of Systematic Reviews | 312 | 2009 |
| Andrographis paniculata in the treatment of upper respiratory tract infections: a systematic review of safety and efficacy. JT Coon, E Ernst: Planta medica 70 (04), 293-298 | 310 | 2004 |
| Different standards for reporting ADRs to herbal remedies and conventional OTC medicines: face‐to‐face interviews with 515 users of herbal remedies: J Barnes, SY Mills, NC Abbot, M Willoughby, E Ernst: British journal of clinical pharmacology 45 (5), 496-500 | 308 | 1998 |
| Complementary and alternative medicine use in England: results from a national survey. KJ Hunt, HF Coelho, B Wider, R Perry, SK Hung, R Terry, E Ernst: International journal of clinical practice 64 (11), 1496-1502 | 305 | 2010 |
| Acupuncture for smoking cessation. AR White, H Rampes, E Ernst: Cochrane Database of Systematic Reviews | 304* | 2002 |
| A review of stroke rehabilitation and physiotherapy. E Ernst: Stroke 21 (7), 1081-1085 | 298 | 1990 |
| Ginkgo biloba extract for the treatment of intermittent claudication: a meta-analysis of randomized trials. MH Pittler, E Ernst: The American journal of medicine 108 (4), 276-281 | 295 | 2000 |
| Adverse effects of spinal manipulation: a systematic review. E Ernst: Journal of the royal society of medicine 100 (7), 330-338 | 290 | 2007 |
| The safety of massage therapy. E Ernst: Rheumatology 42 (9), 1101-1106 | 282 | 2003 |
| Life-threatening adverse reactions after acupuncture? A systematic review. E Ernst, A White: Pain 71 (2), 123-126 | 282 | 1997 |
| Herbal medicines for treatment of bacterial infections: a review of controlled clinical trials. KW Martin, E Ernst: Journal of Antimicrobial Chemotherapy 51 (2), 241-246 | 280 | 2003 |
| Alternative and complementary therapies for the menopause. Borrelli, E Ernst: Maturitas 66 (4), 333-343 | 278 | 2010 |
| Valerian for insomnia: a systematic review of randomized clinical trials. C Stevinson, E Ernst: Sleep medicine 1 (2), 91-99 | 271 | 2000 |
| Adverse effects profile of the herbal antidepressant St. John’s wort (Hypericum perforatum L.). E Ernst, JI Rand, J Barnes, C Stevinson: European journal of clinical pharmacology 54 (8), 589-594 | 271 | 1998 |
| The possible role of hemorheology in atherothrombogenesis. W Koenig, E Ernst: Atherosclerosis 94 (2-3), 93-107 | 269 | 1992 |
| Red ginseng for treating erectile dysfunction: a systematic review. DJ Jang, MS Lee, BC Shin, YC Lee, E Ernst: British journal of clinical pharmacology 66 (4), 444-450 | 263 | 2008 |
| Complementary therapies for depression: an overview. E Ernst, JI Rand, C Stevinson: Archives of general psychiatry 55 (11), 1026-1032 | 260 | 1998 |
| Quality of herbal medicines: challenges and solutions. J Zhang, B Wider, H Shang, X Li, E Ernst: Complementary therapies in medicine 20 (1-2), 100-106 | 257 | 2012 |
| Heavy metals in traditional Indian remedies. E Ernst: European journal of clinical pharmacology 57 (12), 891-896 | 253 | 2002 |
| Heavy metals in traditional Chinese medicines: a systematic review. E Ernst, JT Coon: Clinical Pharmacology & Therapeutics 70 (6), 497-504 | 251 | 2001 |
| Vitex agnus castus. C Daniele, JT Coon, MH Pittler, E Ernst: Drug safety 28 (4), 319-332 | 245 | 2005 |
| Acupuncture for peripheral joint osteoarthritis: a systematic review and meta-analysis. YD Kwon, MH Pittler, E Ernst: Rheumatology 45 (11), 1331-1337 | 242 | 2006 |
| The efficacy of herbal medicine–an overview. E Ernst: Fundamental & clinical pharmacology 19 (4), 405-409 | 242 | 2005 |
| Herb–drug interactions: an overview of systematic reviews. P Posadzki, L Watson, E Ernst. British journal of clinical pharmacology 75 (3), 603-618 | 241 | 2013 |
| Adverse events of herbal food supplements for body weight reduction: systematic review. MH Pittler, K Schmidt, E Ernst: obesity reviews 6 (2), 93-111 | 240 | 2005 |
| Randomized, double-blind trial of chitosan for body weight reduction. MH Pittler, NC Abbot, EF Harkness, E Ernst: European Journal of Clinical Nutrition 53 (5), 379-381 | 237 | 1999 |
| Massage therapy for low back pain: a systematic review. E Ernst: Journal of pain and symptom management 17 (1), 65-69 | 236 | 1999 |
| Feverfew for preventing migraine. MH Pittler, E Ernst: Cochrane database of systematic reviews | 235 | 2004 |
| Intermittent claudication, exercise, and blood rheology. EE Ernst, A Matrai: Circulation 76 (5), 1110-1114 | 235 | 1987 |
| Adverse effects of herbal medicines: an overview of systematic reviews. P Posadzki, LK Watson, E Ernst: Clinical medicine 13 (1), 7 | 233 | 2013 |
| Horse-chestnut seed extract for chronic venous insufficiency: a criteria-based systematic review. MH Pittler, E Ernst: Archives of Dermatology 134 (11), 1356-1360 | 232 | 1998 |
| The effectiveness of acupuncture in treating acute dental pain: a systematic review. E Ernst, MH Pittler: British dental journal 184 (9), 443-447 | 231 | 1998 |
| Complementary therapies for asthma: what patients use. E Ernst: Journal of Asthma 35 (8), 667-671 | 230 | 1998 |
| 87. Acupuncture: does it alleviate pain and are there serious risks? A review of reviews. E Ernst, MS Lee, TY Choi: PAIN 152 (4), 755-764 | 229 | 2011 |
| The effectiveness of spinal manipulation for the treatment of headache disorders: a systematic review of randomized clinical trials. JA Astin, E Ernst: Cephalalgia 22 (8), 617-623 | 228 | 2002 |
| Hawthorn extract for treating chronic heart failure: meta-analysis of randomized trials. MH Pittler, K Schmidt, E Ernst: The American journal of medicine 114 (8), 665-674 | 227 | 2003 |
| Complementary medicine: what physicians think of it: a meta-analysis. E Ernst, KL Resch, AR White: Archives of internal medicine 155 (22), 2405-2408 | 226 | 1995 |
| A brief history of acupuncture. A White, E Ernst: Rheumatology 43 (5), 662-663 | 225 | 2004 |
| Hawthorn extract for treating chronic heart failure. R Guo, MH Pittler, E Ernst: Cochrane Database of Systematic Reviews | 221 | 2008 |
| Prevalence of use of complementary and alternative medicine (CAM) by patients/consumers in the UK: systematic review of surveys. P Posadzki, LK Watson, A Alotaibi, E Ernst: Clinical medicine 13 (2), 126 | 220 | 2013 |
| Herbal medicines for asthma: a systematic review. A Huntley, E Ernst: Thorax 55 (11), 925-929 | 218 | 2000 |
| Plasma viscosity and the risk of coronary heart disease: results from the MONICA-Augsburg Cohort Study, 1984 to 1992. W Koenig, M Sund, B Filipiak, A Doring, H Lowel, E Ernst: Arteriosclerosis, thrombosis, and vascular biology 18 (5), 768-772 | 215 | 1998 |
| Alternative therapy bias. E Ernst, MH Pittler: Nature 385 (6616), 480-480 | 214 | 1997 |
| Systematic review: hepatotoxic events associated with herbal medicinal products. MH Pittler, E Ernst: Aliment Pharmacol & Therapeutics 18 (5), 451-471 | 212 | 2003 |
| Anthocyanosides of Vaccinium myrtillus (bilberry) for night vision—a systematic review of placebo-controlled trials. PH Canter, E Ernst: Survey of ophthalmology 49 (1), 38-50 | 210 | 2004 |
| Prevalence of complementary/alternative medicine for children: a systematic review. E Ernst: European journal of pediatrics 158 (1), 7-11 | 210 | 1999 |
| Homeopathy for postoperative ileus?: a meta-analysis. J Barnes, KL Resch, E Ernst: Journal of Clinical Gastroenterology 25 (4), 628-633 |
What my analysis of these data suggests is the following:
- Only relatively few articles (n=8) are in the ‘top 100’ that I published before I took up the Exeter post starting full-time research into so-called alternative medicine (SCAM).
- Despite the fact that in any such analysis older papers are at a significant advantage over newer articles, the vast majority of these 100 papers are relatively recent.
- Very few of our clinical trials are in the ‘top 100’, even though I did publish well over 50 during my career.
- Systematic reviews dominate by far and amount to 49 of the ‘top 100’.
- Even some of my ‘letters to the editor’ did make it into the ‘top 100’.
- Six of the 100 papers are surveys.
- As to the SCAM topics, most articles are on herbal medicine (n=39), followed by acupuncture (13), manual therapies (4), and homeopathy (2).
- A total of 21 of the papers have their main focus on safety issues.
- The vast majority of the papers are co-authored by more than one member of my team.
- A total of 22 articles were produced in collaboration with researchers who were not members of my team.
- Seventeen papers were single-author papers by myself.
- Even though I certainly did publish a lot in journals specialized in so-called alternative medicine (SCAM), only very few of these articles made it into this list.
There are many things that I find interesting in all this. Perhaps just a few points:
- The two SCAM areas in which I have published many articles and do get a lot of flack for what I have written are homeopathy and chiropractic. Surprisingly, not many of these papers are in the ‘top 100’. I am not sure whether this is meaningful and if so how I should interpret this.
- The fact that hardly any papers published in SCAM journals made the ‘top 100’ is interesting but not surprising. It means that researchers who want to see their work cited – and who doesn’t? – should avoid such journals (there are, of course, other reasons as well for avoiding such journals).
- The fact that even ‘letters to the editors’ can get cited so frequently seems unexpected but I find it encouraging.
- Collaboration with researchers who are not from one’s own team can be, in my experience, cumbersome but it is worth it and often fruitful.
- If you asked me, is there a correlation between the quality of a paper and the frequency with which it is cited, I’d have to say NO.
- If you asked me, is there a correlation between the importance of a paper and the frequency with which it is cited, I’d have to say NO again.
Due to polypharmacy and the rising popularity of so-called alternative medicines (SCAM), oncology patients are particularly at risk of drug-drug interactions (DDI) or herb-drug interactions (HDI). The aims of this study were to assess DDI and HDI in outpatients taking oral anticancer drugs.
All prescribed and non-prescribed medications, including SCAMs, were prospectively collected by hospital pharmacists during a structured interview with the patient. DDI and HDI were analyzed using four interaction software programs: Thériaque®, Drugs.com®, Hédrine, and Memorial Sloan Kettering Cancer Center (MSKCC) database. All detected interactions were characterized by severity, risk, and action mechanism. The need for pharmaceutical intervention to modify drug use was determined on a case-by-case basis.
A total of 294 patients were included, with a mean age of 67 years [55-79]. The median number of chronic drugs per patient was 8 [1-29] and 55% of patients used at least one SCAM. At least 1 interaction was found for 267 patients (90.8%): 263 (89.4%) with DDI, 68 (23.1%) with HDI, and 64 (21.7%) with both DDI and HDI. Only 13% of the DDI were found in Thériaque® and Drugs.com® databases, and 125 (2.5%) were reported with a similar level of risk on both databases. 104 HDI were identified with only 9.5% of the interactions found in both databases. 103 pharmaceutical interventions were performed, involving 61 patients (20.7%).
The authors concluded that potentially clinically relevant drug interactions were frequently identified in this study, showing that several databases and structured screening are required to detect more interactions and optimize medication safety.
These data imply that DDIs are more frequent than HDIs. This does, however, not tell us which are more important. One crucial difference between DDIs and HDIs is that the former are usually known to the oncology team who should thus be able to prevent them or deal with them appropriately; in contrast, HDIs are often not known to the oncology team because many patients fail to disclose the fact that they take herbal remedies. Some forget, some do not think of herbals as medicine, others may be worried about their physician’s reaction.
It follows that firstly, conventional healthcare practitioners should always ask about the usage of herbal remedies, and secondly, they need to be informed about which herbal remedy might interact with which drug. The first can easily be implemented into routine history-taking; the second is more problematic, not least because our knowledge about HDIs is still woefully incomplete. In view of this, it might often be wise to tell patients to stop taking herbal remedies while they are on prescription drugs.




















