Necrotizing infection (NI) of the breast associated with underlying malignancy is a rare phenomenon characterized by necrosis of breast parenchyma. It can cause a delay in diagnosis and even lead to sepsis. Researchers from the Aga Khan University Hospital in Karachi, PAK, present a case of a 42-year-old woman with NI of the right breast, while on homeopathic treatment for a right breast lump for six months. Tissue culture showed a polymicrobial infection and histopathology established the diagnosis of breast carcinoma. After treating the NI, her breast cancer was managed as per standard guidelines.
The married, nulliparous, diabetic, hypertensive patient was a non-smoker and presented to the emergency room with complaints of fever, severe pain, and foul-smelling bloody discharge from her right breast for two weeks. She had a history of a right breast lump for six months, for which she had been taking oral homeopathic remedies, the names of which were not recorded. On examination, she had a blood pressure of 132/76 mmHg, a pulse of 84 bpm, a temperature of 99 °F, and a respiratory rate of 14 breaths per minute. The right breast was tender and hard, with a 4 x 3-cm necrotic skin patch on the upper half with bleeding and a palpable right axillary lymph node. The rest of the examination was unremarkable.
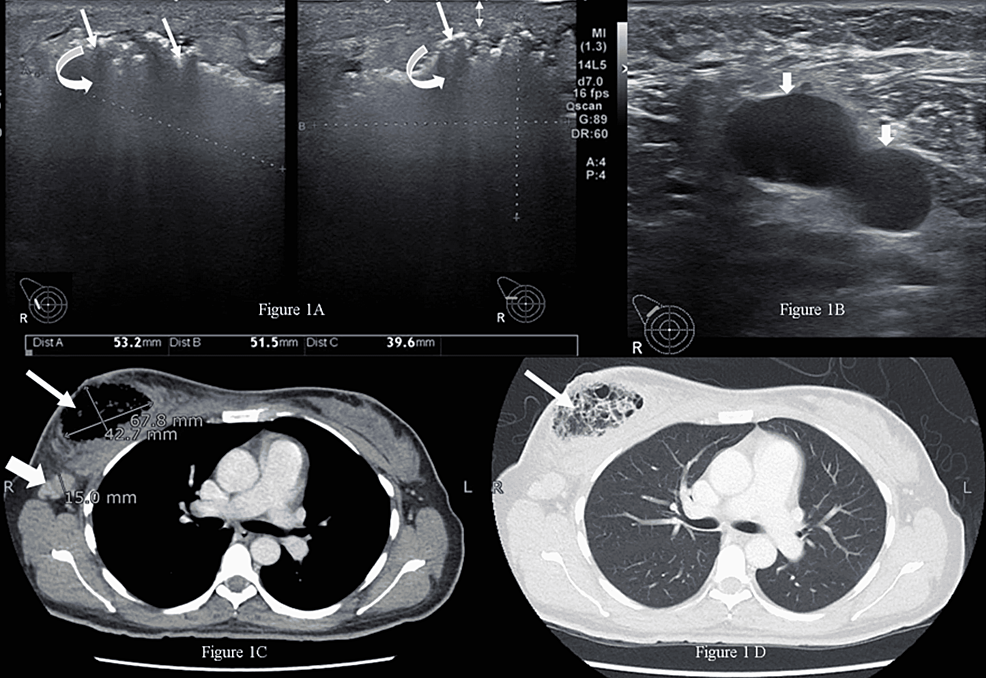
The patient was advised to undergo a metastatic workup in the emergency room, which included a contrast-enhanced CT (CECT) of the chest, abdomen, and pelvis and a bone scan. The CT confirmed the presence of an air-filled cavity in the right breast with thin septations and enlarged right axillary lymph nodes; however, there was no enhancing mass to suggest neoplasm in either breast. The CT and bone scans were negative for metastasis. The presence of severely tender breast on clinical examination and air within the breast on ultrasound suggested the possibility of NI, which warranted an early surgical intervention to prevent impending sepsis.
Microscopic examination of the debrided tissue revealed an invasive breast carcinoma of no special type [invasive ductal carcinoma (IDC), NST grade III] along with extensive necrosis and dense acute and chronic inflammation. The right axillary node biopsy was positive for nodal metastasis, and the patient was staged as cT4N1MO. A tissue culture showed a few colonies of Staphylococcus aureus and Enterococcus species suggestive of NI. After a discussion at a multidisciplinary tumor board meeting, the patient underwent a right modified radical mastectomy. Her postoperative course was unremarkable.
____________________
I have said it often but I am afraid I need to say it again: the homeopathic remedy might be harmless, but that does not mean that homeopathy is not dangerous.
I did not know what a ‘body modification provider’ is. My first guess was that it is a car mechanic who specializes in making my vehicle look ok again after I had a minor accident. But I was wrong! In fact, it is a new healthcare profession – one that we are well-advised to avoid, as it turns out. A Media Release from the Health Care Complaints Commission of Australia dated 27 May, 2022 informed us that:
The NSW Health Care Complaints Commission (Commission) investigated the conduct of Mr Brendan Russell, a body modification provider.
In his capacity as a body modification provider, conducting invasive surgical procedures and administering sedation, Mr Russell is a non-registered health practitioner and subject to the Code of Conduct for non-registered health practitioners (Code of Conduct) set out in schedule 3 of the Public Health Regulation 2012.
Mr Russell was charged with criminal offences relating to services provided to three clients. One related to the removal of part of a client’s labia. Another related to the death of a client following a subdermal implant of a silicone object into the client’s right hand. Mr Russell also performed abdominal surgery on another client making incisions into her abdominal tissue to remove fat.
Following convictions in November 2021 for Intentionally Causing Grievous Bodily Harm, Aid/Abet/Counsel or Procure Female Genital Mutilation and Manslaughter, Mr Russell has breached numerous clauses of the Code of Conduct, and it has been determined that he poses a risk to the health and safety of members of the public.
An Interim Prohibition order has been in place to protect the public during the criminal proceedings. The Commission has now imposed a Permanent Prohibition Order under section 41A(2)(a) of the Health Care Complaints Act 1993 (Act):
Mr Brendan Russell, a body modification provider, is permanently prohibited from providing any health services, either in paid employment or voluntarily, to any member of the public.
___________________________________
What is all this about? Has this man gone doolally? In particular, what is the removal of a woman’s labia supposed to be for? Here is what Wikipedia says about it:
Labiaplasty (also known as labioplasty, labia minora reduction, and labial reduction) is a plastic surgery procedure for altering the labia minora (inner labia) and the labia majora (outer labia), the folds of skin surrounding the human vulva. There are two main categories of women seeking cosmetic genital surgery: those with congenital conditions such as intersex, and those with no underlying condition who experience physical discomfort or wish to alter the appearance of their genitals because they believe they do not fall within a normal range.[1]
The size, colour, and shape of labia vary significantly, and may change as a result of childbirth, aging, and other events.[1] Conditions addressed by labiaplasty include congenital defects and abnormalities such as vaginal atresia (absent vaginal passage), Müllerian agenesis (malformed uterus and fallopian tubes), intersex conditions (male and female sexual characteristics in a person); and tearing and stretching of the labia minora caused by childbirth, accident, and age. In a male-to-female sexual reassignment vaginoplasty for the creation of a neovagina, labiaplasty creates labia where once there were none.
A 2008 study reported that 32 percent of women who underwent the procedure did so to correct a functional impairment; 31 percent to correct a functional impairment and for aesthetic reasons; and 37 percent for aesthetic reasons alone.[2] According to a 2011 review, overall patient satisfaction is in the 90–95 percent range.[3] Risks include permanent scarring, infections, bleeding, irritation, and nerve damage leading to increased or decreased sensitivity. A change in requirements of publicly funded Australian plastic surgery requiring women to be told about natural variation in labias led to a 28% reduction in the number of surgeries performed.[4] Unlike public hospitals, cosmetic surgeons in private practice are not required to follow these rules, and critics say that “unscrupulous” providers are charging to perform the procedure on women who would not want it if they had more information.[4]
______________________________
So, now we know. The procedure belongs in the hands of plastic surgeons, not some ‘body modification provider’. S0-called alternative medicine (SCAM) really is a scam where anything goes. Homeopaths claim to cure cancer, chiropractors believe they can treat anything from deafness and heart disease, acupuncturists feel they can reduce body weight, and now ‘body modification providers’ think they are plastic surgeons. What is more, the amazing thing is: there are always some people gullible enough to believe them.
Brave new world!
I have written about Bioscan before; for instance here. Now there is more news about the device. In Germany, the manufacturers of Bioscan have been sued and found guilty of fraud.
The two managing directors of the company were sentenced to imprisonment for two and three years respectively and together they have to pay a fine of over 2.5 million euros. The presiding judge considered it proven that the manufacturers had sold useless devices. He said, “A measuring device that measures nothing is about as useful as a car that does not drive.” In addition, a former sales director was sentenced to a fine of 90 daily rates.
The three leading employees of the company were charged with commercial fraud and violations of the Therapeutic Products Advertising Act. The company from Pliezhausen had claimed that their device would measure blood and nutrient values in the body in an uncomplicated way and thus replace a time-consuming laboratory diagnosis.
The Bioscan device consists of two metal rods. You have to take them in your hand, according to the company’s instructions. They would then measure magnetic waves and produce a result. More than 200 medically important health data could allegedly be recorded, for example, cholesterol or testosterone levels. The court had summoned several experts to assess the device. However, they found that the device measured nothing except the current flowing through the cables.
The manufacturers had been doing a huge business with the device for years. The company is said to have earned almost 6 million euros. The devices are still being sold today, for instance, in Austria and Switzerland, among other countries. Despite all the criticism and the court case, the two managing directors had not stopped sales.
________________________
When I googled ‘Bioscan’ yesterday (30/5), the website informed me that:
The BioScan system is an FDA cleared, state of the art testing machine that scans the body’s organs and functions for imbalances using electrodermal screening (EDS).
BioScan SRT
What Is Stress Reduction Testing?
SRT is a remarkable new procedure that combines the disciplines of Acupuncture, Biofeedback and Homeopathy with Laser Light technology. A computerized scan or test is done to see what your body is sensitive to, and how it is out of balance, then help it learn not to be.
Are there any side effects?
No. A small percentage of clients report slight flushing or congestion for a short time (an hour or so) after their session, but this is actually a sign that the body is detoxifying (a good thing)! This process is safe, fast, non-invasive and painless. Unlike skin tests the actual substance is not used, so the body perceives its presence, it as if it were there, but does not act upon it.
What does the BioScan SRT treat?
The BioScan SRT Wellness System does not diagnose or treat any specific condition. Through the use of our FDA-cleared biofeedback technology, the BioScan SRT is able to assess with a very high degree of specificity which substances create increased levels of stress to the body.These specific stress inducing substances are often times what trigger the nervous systems fight or flight reactions which are expressed in a myriad of symptoms that have been scientifically proven to be associated with high levels of stress.
What substances can the BioScan SRT identify as stressors?
The BioScan SRT contains tens of thousands of substances in the main procedure libraries and up to an additional 50,000 substances in the advanced procedure libraries. This technology can identify almost every known substance that could possibly cause a stress reaction.
_________________________
And on the Internet, it takes just a minute to find a Bioscan device for sale. It would set you back by 119.98 Euros.
_________________________
Say no more!
I know only too well that some readers will interpret this post as pompous and self-congratulatory, but I nevertheless feel like telling my readers that I have become a member of the ACADEMIA EUROPAEA. In case you don’t know what this is, Wikipedia provides the following information:
Membership of the Academia Europaea (MAE) is an award conferred by the Academia Europaea to individuals that have demonstrated “sustained academic excellence”.[2] Membership is by invitation only by existing MAE only and judged during a peer review selection process.[3] Members are entitled to use the post-nominal letters MAE.[4]
New members are announced annually, every year since 1988.[5][6] For a more complete list see Category:Members of Academia Europaea..[7][8][9][10][11] Some Members of the Academia Europaea have received very prestigious awards, medals and prizes, such as:
- The Nobel Prize[12] e.g. Christiane Nüsslein-Volhard (1995, Physiology), Arvid Carlsson (2000, Physiology or Medicine), Paul Nurse (2001, Physiology or Medicine), Tim Hunt (2001, Physiology or Medicine), Kurt Wüthrich (2002, Chemistry), John Sulston (2002, Physiology or Medicine), Sydney Brenner 2002, Physiology or Medicine, Aaron Ciechanover (2004, Chemistry), Roy J. Glauber (2005, Physics), Roger D. Kornberg (2006, Chemistry), Gerhard Ertl (2007, Chemistry), Richard Tol (2007, shared winner of the Nobel Peace Prize), Harald zur Hausen (2008, Physiology or Medicine), Luc Montagnier (2008, Physiology or Medicine), Robert G. Edwards (2010, Physiology or Medicine), John B. Gurdon (2012, Physiology or Medicine), Rita Levi-Montalcini (1986, Physiology)
- The Wolf Prize,[13] e.g. Simon Donaldson (2020), Alexander Beilinson (2018), Peter Zoller (2013), Alain Aspect (2010), Anton Zeilinger (2010), Axel Ullrich (2010), David Baulcombe (2010), Howard Cedar (2008), Albert Fert (2006/2007), Alexander Levitzki (2005), Sergei P. Novikov (2005), Alexander Varshavsky (2001), Saharon Shelah (2001), Vladimir I. Arnold (2001).
- The Turing Award,[14] e.g. Joseph Sifakis (2007), Adi Shamir (2002).
- The Fields Medal,[15] e.g. Martin Hairer (2014), Elon Lindenstrauss (2010), Stanislav Smirnov (2010), Cédric Villani (2010), Wendelin Werner (2006), Timothy Gowers (1998), Maxim Kontsevich (1998), Jean Bourgain (1994), Pierre-Louis Lions (1994), Simon Donaldson (1986), Enrico Bombieri (1974), Sergei P. Novikov (1970), Michael Atiyah (1966).
- The Lasker Award,[16] e.g. Roy Calne (2012), David Weatherall (2010), John Gurdon (2009), David Baulcombe (2008), Alec Jeffreys (2005), Pierre Chambon (2004), Robert Edwards (2001), Sydney Brenner (2000), Aaron Ciechanover (2000), Alexander Varshavsky (2000).
- The Abel Prize,[17] e.g. Andrew Wiles (2016), Endre Szemerédi (2012), Mikhail Leonidovich Gromov (2009), Jacques Tits (2008), Lennart Carleson (2006), Michael Atiyah (2004).
- The Gödel Prize,[18] e.g. Christos H. Papadimitriou (2012), Johan Hastad (2011, 1994), Alexander Razborov (2007), Noga Alon (2005), László Lovász (2001), Moshe Vardi (2000), Pierre Wolper (2000).
________________________________
The Academia Europaea was founded in 1988, on the initiative of the UK’s Royal Society and other National Academies in Europe. It is a `Not for Profit’ Charity registered in the UK. The Academia Europaea is the only Academy with individual members from the Council of Europe states and from other nations across the world. Currently, there are some 5000 members who cover the full range of academic disciplines.
The objectives of the Academia Europaea are the advancement and propagation of excellence in scholarship in the humanities, law, the economic, social, and political sciences, mathematics, medicine, and all branches of natural and technological sciences anywhere in the world for the public benefit and for the advancement of the education of the public of all ages.
The Academy organizes meetings and workshops, provides scientific and scholarly advice, and publishes the international journal the ‘European Review’ and is associated with Biology Direct. It operates regional knowledge hubs out of Barcelona, Bergen, Budapest, Cardiff, Munich, Tbilisi, and Wroclaw, hosted by Universities and National academies.
_______________________________
I am both proud and thankful that I have been honored in this way.
I have been sent a press release dated 26/5/2022 that might interest some of my readers. As it is in German, I took the liberty of translating it:
The 126th German Medical Congress today in Bremen deleted the additional designation of homeopathy from the further education regulations for doctors (MWBO). The request brought by Bremen delegates was decided by the physician parliament with a large majority.
The Bremen delegates justified their request with the fact that 13 of 17 state medical associations have already deleted the additional designation of homeopathy from their further education regulations. The further education regulation is to create uniform rules for the post-graduate training of doctors. However, there is no longer any question of uniformity if 13 state medical associations do not follow the MWBO.
In the debate, Dr. Johannes Grundmann once again pointed out that it is not a matter of prohibiting people from using homeopathic remedies. “However, it is the task of the medical associations to define and check verifiable learning objectives,” Grundmann said to great applause.
In September 2020, the Bremen Medical Association had become the first such chamber in Germany to remove homeopathy from its education regulations. The complaint of a Bremen physician against it had subsequently been rejected in two instances. Most recently, the Bremen health insurance was the first to terminate three selective contracts for the remuneration of homeopathic services.
____________________________
I feel that this is a nice victory of reason over unreason. I might even go as far as assuming that our petition of 2021 might have helped a little to bring it about:
Dear President Dr Reinhardt,
Dear Ms Lundershausen,
Mrs Held,
Dear Ms Johna,
We, the undersigned doctors, would like to draw your attention to the insistence of individual state medical associations on preserving “homeopathy” as a component of continuing medical education. We hope that you, by virtue of your office, will ensure a nationwide regulation so that this form of sham treatment [1], as has already happened in other European countries, can no longer call itself part of medicine.
We justify our request by the following facts:
-
- After the landmark vote in Bremen in September 2019 to remove “homeopathy” from the medical training regulations, 10 other state medical associations have so far followed Bremen’s example. For reasons of credibility and transparency, it would be desirable if the main features of the training content taught were not coordinated locally in the future, but centrally and uniformly across the country so that there is no “training tourism”. Because changes to a state’s own regulations of postgraduate training are only binding for the examination committee of the respective state, this does not affect national regulations but is reduced to only a symbolic character without sufficient effects on the portfolio of medical education nationwide.
- Medicine always works through the combination of a specifically effective part and non-specific placebo effects. By insisting on a pseudo-medical methodology – as is “homeopathy” represents in our opinion – patients are deprived of the specific effective part and often unnecessarily deprived of therapy appropriate to the indication. Tragically, it happens again and again that the “therapeutic window of opportunity” for an appropriate therapy is missed, tumors can grow to inoperable size, etc.
- Due to the insistence of individual state medical associations on the “homeopathic doctrine of healing” as part of the medical profession, we are increasingly exposed to the blanket accusation that, by tolerating this doctrine, we are supporting and promoting ways of thinking and world views that are detached from science. This is a dangerous situation, which in times of a pandemic manifests itself in misguided aggression reflected not just in vaccination skepticism and vaccination refusal, but also in unacceptable personal attacks and assaults on vaccinating colleagues in private practice.
Responsible:
Dr. med. Dent. Hans-Werner Bertelsen
Prof. Dr. med. Edzard Ernst
George A. Rausche
_______________________________________
The first reported reactions from politicians are positive, while those of homeopaths are predictably the opposite:
German Health Minister Karl Lauterbach (SPD) expressly welcomed the delegates’ decision, writing via Twitter. “Good medicine stands on the ground of science. For homeopathy, there is no place there. In such a question, one must show one’s colors.”
Paula Piechotta, a Green Party member of parliament, was equally pleased. “… it is good when in times of Fake Facts and right-wing conspiracy theories clarity is provided where clarity is needed. Thank you Ärztetag,” she tweeted.
Michaela Geiger, chairwoman of the German Central Association of Homeopathic Physicians, noted the decision “with astonishment.” Homeopathy has a high acceptance among the population, she claimed.
During their cancer treatment path, cancer patients use numerous drugs,e.g.:
- anticancer medications,
- supportive drugs,
- other prescribed medications,
- herbal remedies,
- other OTC products.
This puts them at risk of significant drug interactions (DIs).
This study describes potential DIs in cancer patients and their prevalence and predictors.
A cross-sectional study was carried out in two centers in the northern West Bank, Palestine. The Lexicomp® Drug Interactions tool (Lexi-Comp, Hudson OH, USA) was applied to check the potential DIs. In addition, the Statistical Package for the Social Sciences (SPSS) was used to show the results and find the associations.
The final analysis included 327 patients. Most of the participants were older than 50 years (61.2%), female (68.5%), and had a solid tumor (74.6%). The total number of potential DIs was 1753, including 1510 drug-drug interactions (DDIs), 24 drug-herb interactions, and 219 drug-food interactions. Importantly, the prevalence of DDIs was 88.1%. In multivariate analysis, the number of potential DDIs significantly decreased with the duration of treatment (p = 0.007), while it increased with the number of comorbidities (p < 0.001) and the number of drugs used (p < 0.001).
The authors concluded that they found a high prevalence of DIs among cancer patients. This required health care providers to develop a comprehensive protocol to monitor and evaluate DIs by improving doctor-pharmacist communication and supporting the role of clinical pharmacists.
What the investigators did not study was the possibility of herb-herb and herb-non-herbal supplement interactions. The reason for this is probably simple: we know too little about these areas to make reasonable judgments. But even in the absence of such considerations, the prevalence of DDIs among cancer patients was high (88.1%). This means that the vast majority of cancer patients had at least one potential DDI. Over half of them were classified as moderately severe or worse.
The lessons seem to be to:
- use only truly necessary drugs and omit all remedies that are of doubtful value,
- educate the public about the risks of interactions,
- be skeptical about the messages of integrative medicine,
- consult a healthcare professional who is competent to make such judgments,
- conduct more rigorous research to increase our knowledge in this complex area.
Naprapathy is an odd variation of chiropractic. To be precise, it has been defined as a system of specific examination, diagnostics, manual treatment, and rehabilitation of pain and dysfunction in the neuromusculoskeletal system. It is aimed at restoring the function of the connective tissue, muscle- and neural tissues within or surrounding the spine and other joints. The evidence that it works is wafer-thin. Therefore rigorous studies are of interest.
The aim of this study was to evaluate the cost-effectiveness of manual therapy compared with advice to stay active for working-age persons with nonspecific back and/or neck pain.
The two interventions were:
- a maximum of 6 manual therapy sessions within 6 weeks, including spinal manipulation/mobilization, massage, and stretching, performed by a naprapath (index group),
- information from a physician on the importance to stay active and on how to cope with pain, according to evidence-based advice, on 2 occasions within 3 weeks (control group).
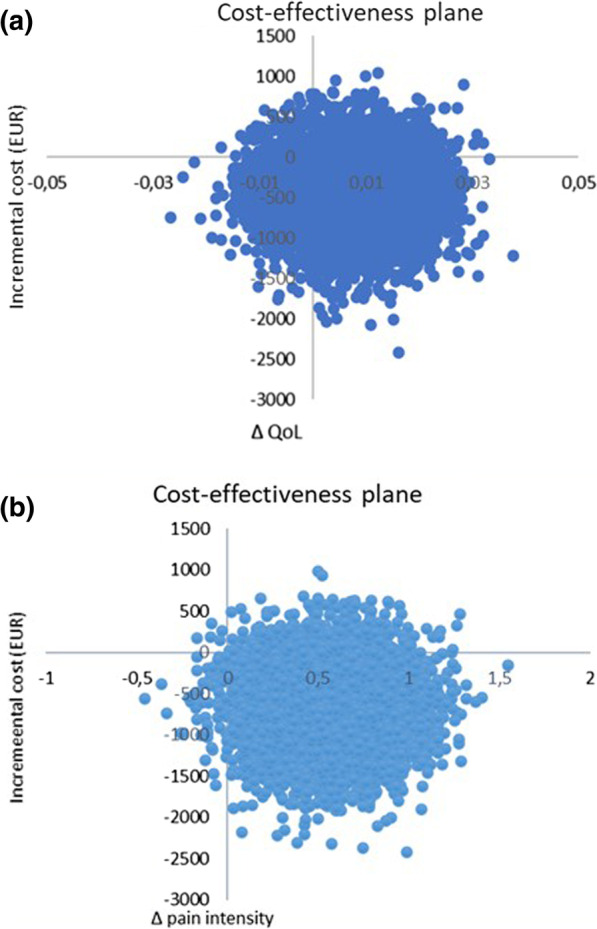
A cost-effectiveness analysis with a societal perspective was performed alongside a randomized controlled trial including 409 persons followed for one year, in 2005. The outcomes were health-related Quality of Life (QoL) encoded from the SF-36 and pain intensity. Direct and indirect costs were calculated based on intervention and medication costs and sickness absence data. An incremental cost per health-related QoL was calculated, and sensitivity analyses were performed.
The difference in QoL gains was 0.007 (95% CI – 0.010 to 0.023) and the mean improvement in pain intensity was 0.6 (95% CI 0.068-1.065) in favor of manual therapy after one year. Concerning the QoL outcome, the differences in mean cost per person were estimated at – 437 EUR (95% CI – 1302 to 371) and for the pain outcome the difference was – 635 EUR (95% CI – 1587 to 246) in favor of manual therapy. The results indicate that manual therapy achieves better outcomes at lower costs compared with advice to stay active. The sensitivity analyses were consistent with the main results.
Cost-effectiveness plane using bootstrapped incremental cost-effectiveness ratios for QoL and pain intensity outcomes
The authors concluded that these results indicate that manual therapy for nonspecific back and/or neck pain is slightly less costly and more beneficial than advice to stay active for this sample of working age persons. Since manual therapy treatment is at least as cost-effective as evidence-based advice from a physician, it may be recommended for neck and low back pain. Further health economic studies that may confirm those findings are warranted.
This is an interesting and well-conducted study. The differences between the groups seem small and of doubtful relevance. The authors acknowledge this fact by stating: “together with the clinical results from previously published studies on the same population the results suggest that manual therapy may be as cost-effective a treatment as evidence-based advice from a physician, for back and neck pain”. Moreover, the data do not convince me that the treatment per se was effective; it might have been the non-specific effects of touch and attention.
I have said it before: there is currently no optimal treatment for neck and back pain. Therefore, the findings even of rigorous cost-effectiveness studies will only generate lukewarm results.
This study used a US nationally representative 11-year sample of office-based visits to physicians from the National Ambulatory Medical Care Survey (NAMCS), to examine a comprehensive list of factors believed to be associated with visits where complementary health approaches were recommended or provided.
NAMCS is a national health care survey designed to collect data on the provision and use of ambulatory medical care services provided by office-based physicians in the United States. Patient medical records were abstracted from a random sample of office-based physician visits. The investigators examined several visit characteristics, including patient demographics, physician specialty, documented health conditions, and reasons for a health visit. They ran chi-square analyses to test bivariate associations between visit factors and whether complementary health approaches were recommended or provided to guide the development of logistic regression models.
Of the 550,114 office visits abstracted, 4.43% contained a report that complementary health approaches were ordered, supplied, administered, or continued. Among complementary health visits, 87% of patient charts mentioned nonvitamin nonmineral dietary supplements. The prevalence of complementary health visits significantly increased from 2% in 2005 to almost 8% in 2015. Returning patient status, survey year, physician specialty and degree, menopause, cardiovascular, and musculoskeletal diagnoses were significantly associated with complementary health visits, as was seeking preventative care or care for a chronic problem.
The authors concluded that these data confirm the growing popularity of complementary health approaches in the United States, provide a baseline for further studies, and inform subsequent investigations of integrative health care.
The authors used the same dataset for a 2nd paper which examined the reasons why office-based physicians do or do not recommend four selected complementary health approaches to their patients in the context of the Andersen Behavioral Model. Descriptive estimates were employed of physician-level data from the 2012 National Ambulatory Medical Care Survey (NAMCS) Physician Induction Interview, a nationally representative survey of office-based physicians (N = 5622, weighted response rate = 59.7%). The endpoints were the reasons for the recommendation or lack thereof to patients for:
- herbs,
- other non-vitamin supplements,
- chiropractic/osteopathic manipulation,
- acupuncture,
- mind-body therapies (including meditation, guided imagery, and progressive relaxation).
Differences by physician sex and medical specialty were described.
For each of the four complementary health approaches, more than half of the physicians who made recommendations indicated that they were influenced by scientific evidence in peer-reviewed journals (ranging from 52.0% for chiropractic/osteopathic manipulation [95% confidence interval, CI = 47.6-56.3] to 71.3% for herbs and other non-vitamin supplements [95% CI = 66.9-75.4]). More than 60% of all physicians recommended each of the four complementary health approaches because of patient requests. A higher percentage of female physicians reported evidence in peer-reviewed journals as a rationale for recommending herbs and non-vitamin supplements or chiropractic/osteopathic manipulation when compared with male physicians (herbs and non-vitamin supplements: 78.8% [95% CI = 72.4-84.3] vs. 66.6% [95% CI = 60.8-72.2]; chiropractic/osteopathic manipulation: 62.3% [95% CI = 54.7-69.4] vs. 47.5% [95% CI = 42.3-52.7]).
For each of the four complementary health approaches, a lack of perceived benefit was the most frequently reported reason by both sexes for not recommending. Lack of information sources was reported more often by female versus male physicians as a reason to not recommend herbs and non-vitamin supplements (31.4% [95% CI = 26.8-36.3] vs. 23.4% [95% CI = 21.0-25.9]).
The authors concluded that there are limited nationally representative data on the reasons as to why office-based physicians decide to recommend complementary health approaches to patients. Developing a more nuanced understanding of influencing factors in physicians’ decision making regarding complementary health approaches may better inform researchers and educators, and aid physicians in making evidence-based recommendations for patients.
I am not sure what these papers really offer in terms of information that is not obvious or that makes a meaningful contribution to progress. It almost seems that, because the data of such surveys are available, such analyses get done and published. The far better reason for doing research is, of course, the desire to answer a burning and relevant research question.
A problem then arises when researchers, who perceive the use of so-called alternative medicine (SCAM) as a fundamentally good thing, write a paper that smells more of SCAM promotion than meaningful science. Having said that, I find it encouraging to read in the two papers that
- the prevalence of SCAM remains quite low,
- more than 60% of all physicians recommended SCAM not because they were convinced of its value but because of patient requests,
- the lack of perceived benefit was the most frequently reported reason for not recommending it.
Osteopathic visceral manipulation (VM) is a bizarre so-called alternative medicine (SCAM) that has been featured on this blog with some regularity, e.g.:
- Osteopathic visceral manipulation: a new study fails to convince anyone
- Visceral manipulation…you couldn’t make it up
- Intravaginal manipulations by (German) osteopaths: a new low point for clinical research into alternative medicine?
- Visceral osteopathy is implausible and does not work … SO, LET’S FORGET ABOUT IT ONCE AND FOR ALL
Rigorous trials fail to show that it works for anything. So, the obvious solution to this dilemma is to conduct dodgy trials!
This study tested the effects of VM on dysmenorrhea, irregular, delayed, and/or absent menses, and premenstrual symptoms in PCOS patients.
Thirty Egyptian women with polycystic ovary syndrome (PCOS), with menstruation-related complaints and free from systematic diseases and/or adrenal gland abnormalities, participated in a single-blinded, randomized controlled trial. They were recruited from the women’s health outpatient clinic in the faculty of physical therapy at Cairo University, with an age of 20-34 years, and a body mass index (BMI) ≥25, <30 kg/m2. Patients were randomly allocated into two equal groups (15 patients); the control group received a low-calorie diet for 3 months, and the study group that received the same hypocaloric diet added to VM to the pelvic organs and their related structures for eight sessions over 3 months. Evaluations for body weight, BMI, and menstrual problems were done by weight-height scale, and menstruation-domain of Polycystic Ovary Syndrome Health-Related Quality of Life Questionnaire (PCOSQ), respectively, at baseline and after 3 months from interventions. Data were described as mean, standard deviation, range, and percentage whenever applicable.
Of 60 Egyptian women with PCOS, 30 patients were included, with baseline mean age, weight, BMI, and a menstruation domain score of 27.5 ± 2.2 years, 77.7 ± 4.3 kg, 28.6 ± 0.7 kg/m2, and 3.4 ± 1.0, respectively, for the control group, and 26.2 ± 4.7 years, 74.6 ± 3.5 kg, 28.2 ± 1.1 kg/m2, and 2.9 ± 1.0, respectively, for the study group. Out of the 15 patients in the study group, uterine adhesions were found in 14 patients (93.3%), followed by restricted uterine mobility in 13 patients (86.7%), restricted ovarian/broad ligament mobility (9, 60%), and restricted motility (6, 40%). At baseline, there was no significant difference (p>0.05) in any of the demographics (age, height), or dependent variables (weight, BMI, menstruation domain score) among both groups. Post-study, there was a statistically significant reduction (p=0.000) in weight, and BMI mean values for the diet group (71.2 ± 4.2 kg, and 26.4 ± 0.8 kg/m2, respectively) and the diet + VM group (69.2 ± 3.7 kg; 26.1 ± 0.9 kg/m2, respectively). For the improvement in the menstrual complaints, a significant increase (p<0.05) in the menstruation domain mean score was shown in the diet group (3.9 ± 1.0), and the diet + VM group (4.6 ± 0.5). On comparing both groups post-study, there was a statistically significant improvement (p=0.024) in the severity of menstruation-related problems in favor of the diet + VM group.
The authors concluded that VM yielded greater improvement in menstrual pain, irregularities, and premenstrual symptoms in PCOS patients when added to caloric restriction than utilizing the low-calorie diet alone in treating that condition.
WHERE TO START?
- Tiny sample size.
- A trail design (A+B vs B) which will inevitably generate a positive result.
- Questionable ethics.
VM is a relatively invasive and potentially embarrassing intervention for any woman; I imagine that this is all the more true in Egypt. In such circumstances, it is mandatory to ask whether a planned study is ethically justifiable. I would answer this question related to an implausible treatment like VM with a straight NO!
I realize that there may be people who disagree with me. But even those guys should accept that, at the very minimum, such a study must be designed such that it leads to a clear answer – is VM effective or not? The present trial merely suggests that the placebo effect associated with VM is powerful (which is hardly surprising for a therapy like VM).
Acupuncture is often promoted as a therapeutic option for obesity and weight control. The aim of this study was to investigate the effects of electroacupuncture (EA) on body weight, body mass index (BMI), skin fold thickness, waist circumference and skin temperature of the abdominal region in non-obese women with excessive abdominal subcutaneous fat.
A total of 50 women with excessive abdominal subcutaneous fat (and average BMI of 22) were randomly assigned to one of two groups:
- an EA group (n = 25) receiving 10 EA sessions (insertion of needles connected to an electrical stimulator at a frequency of 40 Hz for 40 min),
- a control group (n = 25) that received no treatment.
Outcome measures evaluated included waist circumference, supra-iliac and abdominal skinfolds, body composition and superficial skin temperature (measured by cutaneous thermography) before and after treatment.
Compared with the untreated group, women in the EA group exhibited decreased supra-iliac and abdominal skin folds (p < 0.001), waist circumference (p < 0.001), percentage body fat (p = 0.001) and percentage abdominal fat (p < 0.001). In addition, the EA group showed an elevated skin temperature at the site of the treatment. However, EA did not significantly impact body weight (p = 0.01) or BMI (p = 0.2).
The authors concluded that EA promoted a reduction in abdominal waist circumference, supra-iliac and abdominal skin folds, and percentage body and abdominal fat in women of normal BMI with excessive abdominal subcutaneous fat, as well as an increase in the superficial skin temperature of the abdominal region.
If we did not know that acupuncture researchers were all honest investigators testing hypotheses the best they can, we could almost assume that some are trying to fool us. The set-up of this study is ideally suited to introduce a proper placebo treatment. All one has to do is to not switch on the electrical stimulator in the control group. Why did the researchers not do that? Surely not because they wanted to increase the chances of generating a positive result; that would have been dishonest!!!
So, as it stands, what does the study tell us? I think it shows that, compared to patients who receive no treatment, patients who do receive the ritual of EA are better motivated to adhere to calorie restrictions and dietary advice. Thus, I suggest to re-phrase the conclusions of this trial as follows:
The extra attention of the EA treatment motivated obese patients to eat less which caused a reduction in abdominal waist circumference, supra-iliac and abdominal skin folds, and percentage body and abdominal fat in women of normal BMI with excessive abdominal subcutaneous fat.