TCM
Migraines are common headache disorders and risk factors for subsequent strokes. Acupuncture has been widely used in the treatment of migraines; however, few studies have examined whether its use reduces the risk of strokes in migraineurs. This study explored the long-term effects of acupuncture treatment on stroke risk in migraineurs using national real-world data.
A team of Taiwanese researchers collected new migraine patients from the Taiwan National Health Insurance Research Database (NHIRD) from 1 January 2000 to 31 December 2017. Using 1:1 propensity-score matching, they assigned patients to either an acupuncture or non-acupuncture cohort and followed up until the end of 2018. The incidence of stroke in the two cohorts was compared using the Cox proportional hazards regression analysis. Each cohort was composed of 1354 newly diagnosed migraineurs with similar baseline characteristics. Compared with the non-acupuncture cohort, the acupuncture cohort had a significantly reduced risk of stroke (adjusted hazard ratio, 0.4; 95% confidence interval, 0.35–0.46). The Kaplan–Meier model showed a significantly lower cumulative incidence of stroke in migraine patients who received acupuncture during the 19-year follow-up (log-rank test, p < 0.001).
The authors concluded that acupuncture confers protective benefits on migraineurs by reducing the risk of stroke. Our results provide new insights for clinicians and public health experts.
After merely 10 minutes of critical analysis, ‘real-world data’ turn out to be real-bias data, I am afraid.
The first question to ask is, were the groups at all comparable? The answer is, NO; the acupuncture group had
- more young individuals;
- fewer laborers;
- fewer wealthy people;
- fewer people with coronary heart disease;
- fewer individuals with chronic kidney disease;
- fewer people with mental disorders;
- more individuals taking multiple medications.
And that are just the variables that were known to the researcher! There will be dozens that are unknown but might nevertheless impact on a stroke prognosis.
But let’s not be petty and let’s forget (for a minute) about all these inequalities that render the two groups difficult to compare. The potentially more important flaw in this study lies elsewhere.
Imagine a group of people who receive some extra medical attention – such as acupuncture – over a long period of time, administered by a kind and caring therapist; imagine you were one of them. Don’t you think that it is likely that, compared to other people who do not receive this attention, you might feel encouraged to look better after your health? Consequently, you might do more exercise, eat more healthily, smoke less, etc., etc. As a result of such behavioral changes, you would be less likely to suffer a stroke, never mind the acupuncture.
SIMPLE!
I am not saying that such studies are totally useless. What often renders them worthless or even dangerous is the fact that the authors are not more self-critical and don’t draw more cautious conclusions. In the present case, already the title of the article says it all:
Acupuncture Is Effective at Reducing the Risk of Stroke in Patients with Migraines: A Real-World, Large-Scale Cohort Study with 19-Years of Follow-Up
My advice to researchers of so-called alternative medicine (SCAM) and journal editors publishing their papers is this: get your act together, learn about the pitfalls of flawed science (most of my books might assist you in this process), and stop misleading the public. Do it sooner rather than later!
This pilot study tested the feasibility of using US Food and Drug Administration (FDA)–recommended endpoints to evaluate the efficacy of acupuncture in the treatment of IBS. It was designed as a multicenter randomized clinical trial, conducted in 4 tertiary hospitals in China from July 1, 2020, to March 31, 2021, and 14-week data collection was completed in March 2021. Individuals with a diagnosis of IBS with diarrhea (IBS-D) were randomized to 1 of 3 groups:
- acupuncture groups 1 (using specific acupoints [SA])
- acupuncture group 2 (using nonspecific acupoints [NSA])
- sham acupuncture group (non-acupoints [NA])
Patients in all groups received twelve 30-minute sessions over 4 consecutive weeks at 3 sessions per week, ideally every other day.
The primary outcome was the response rate at week 4, which was defined as the proportion of patients whose worst abdominal pain score (score range, 0-10, with 0 indicating no pain and 10 indicating unbearable severe pain) decreased by at least 30% and the number of type 6 or 7 stool days decreased by 50% or greater.
Ninety patients (54 male [60.0%]; mean [SD] age, 34.5 [11.3] years) were enrolled, with 30 patients in each group. There were substantial improvements in the primary outcomes for all groups
- response rates in the SA group = 46.7% [95% CI, 28.8%-65.4%]
- response rate in the NSA group = 46.7% [95% CI, 28.8%-65.4%]
- response rate in the NA group = 26.7% [95% CI, 13.0%-46.2%]
The difference between the groups was not statistically significant (P = .18). The response rates of adequate relief at week 4 were 64.3% (95% CI, 44.1%-80.7%) in the SA group, 62.1% (95% CI, 42.4%-78.7%) in the NSA group, and 55.2% (95% CI, 36.0%-73.0%) in the NA group (P = .76). Adverse events were reported in 2 patients (6.7%) in the SA group and 3 patients (10%) in NSA or NA group.
The authors concluded that acupuncture in both the SA and NSA groups showed clinically meaningful improvement in IBS-D symptoms, although there were no significant differences among the 3 groups. These findings suggest that acupuncture is feasible and safe; a larger, sufficiently powered trial is needed to accurately assess efficacy.
WHAT A LOAD OF TOSH!
Here are some of the most obvious issues I have with this new study:
- A pilot study is not about reporting effectiveness/efficacy but about testing the feasibility of a study.
- That acupuncture is feasible has been known for ~2000 years.
- The conclusion that acupuncture is safe is not warranted on the basis of the data; for that we would need a much larger investigation.
- The authors seem to have used our sham needle without acknowledging it.
- The authors are affiliated with the International Acupuncture and Moxibustion Innovation Institute, School of Acupuncture-Moxibustion and Tuina, Beijing University of Chinese Medicine, yet they state that they have no conflicts of interest.
- The results are clearly negative, yet the authors seem to attempt to draw a positive conclusion.
The main question that occurs to me is this: how low has the JAMA sunk to publish such junk?
Is so-called alternative medicine (SCAM) compatible with Christian beliefs? This is not a question that often robs me of my sleep, yet it seems an interesting issue to explore during the Christmas holiday. So, I did a few searches and – would you believe it? – found a ‘Christian Checklist’ as applied to SCAM Since it is by no means long, let me present it to you in full:
- Taking into consideration the lack of scientific evidence available, can it be recommended with integrity?
- What are its roots? Is there an eastern religious basis (Taoism or Hinduism)? Is it based on life force or vitalism?
- Are there any specific spiritual dangers involved? Does its method of diagnosis or practice include occult practices, all forms of which are strictly forbidden in Scripture.
Now, let me try to answer the questions that the checklist poses:
- No! – particularly not, if the SCAM endangers the health of the person who uses it (which, as we have discussed so often can occur in multiple ways).
- Most SCAMs have their roots in eastern religions, life force, or vitalism. Very few are based on Christian ideas or assumptions.
- If we define ‘occult’ as anything that is hidden or mysterious, we are bound to see that almost all SCAMs are occult.
What surprises me with the ‘Christian Checklist’ is that it makes no mention of ethics. I would have thought that this might be an important issue for Christians. Am I mistaken? I have often pointed out that the practice of SCAM nearly invariably violates fundamental rules of ethics.
In any case, the checklist makes one thing quite clear: by and large, SCAM is nothing that Christians should ever contemplate employing. This article (which I have quoted before) seems to confirm my point:
The Vatican’s top exorcist has spoken out in condemnation of yoga … , branding [it] as “Satanic” acts that lead[s] to “demonic possession”. Father Cesare Truqui has warned that the Catholic Church has seen a recent spike in worldwide reports of people becoming possessed by demons and that the reason for the sudden uptick is the rise in popularity of pastimes such as watching Harry Potter movies and practicing Vinyasa.
Professor Giuseppe Ferrari … says that … activities such as yoga, “summon satanic spirits” … Monsignor Luigi Negri, the archbishop of Ferrara-Comacchio, who also attended the Vatican crisis meeting, claimed that homosexuality is “another sign” that “Satan is in the Vatican”. The Independent reports: Father Cesare says he’s seen many an individual speaking in tongues and exhibiting unearthly strength, two attributes that his religion says indicate the possibility of evil spirits inhabiting a person’s body. “There are those who try to turn people into vampires and make them drink other people’s blood, or encourage them to have special sexual relations to obtain special powers,” stated Professor Ferrari at the meeting. “These groups are attracted by the so-called beautiful young vampires that we’ve seen so much of in recent years.”
You might take such statements not all that seriously – the scorn of the vatican does not concern you?
Yet, the ‘Christian Checklist’ also raises worries much closer to home. King Charles is the head of the Anglican Church. Undeniably, he also is a long-term, enthusiastic supporter of many of those ‘quasi-satanic’ SCAMs. How are we supposed to reconsile these contradictions, tensions, and conflicts?
Please advise!
Like traditional acupuncture, “cosmetic acupuncture” involves the insertion of needles into the skin. Also called facial rejuvenation acupuncture, cosmetic acupuncture is believed to stimulate collagen and therefore reduce the look of wrinkles. They also claim that cosmetic acupuncture rejuvenates your skin by improving your overall energy and is a great addition to your overall wellness routine – at least, this is what enthusiasts want us to believe. 
No surprise then that many consumers give cosmetic acupuncture a try. But what, if after paying for a session, you don’t notice any difference? What, if you even look worse than before?
Impossible?
Not at all! One of the few studies on the subject showed that about half of the clients complained of blotchiness and hyperpigmented spots.
Cosmetic acupuncturists are well prepared for this argument and claim that the treatment will take longer to show any results: “Most cosmetic acupuncture treatments are meant to be taken in a series, generally in a group of 10,” says DiLibero. “The effects of acupuncture are cumulative, so follow-up appointments are recommended.”
And what does the evidence tell us about the effectiveness of cosmetic acupuncture?
One study showed “promising results as a therapy for facial elasticity”. Another one “showed clinical potential for facial wrinkles and laxity.”
That’s great!
No, it isn’t; the studies were published in 3rd class journals and did not even have control groups. Sorry, but I don’t call this evidence. In fact, the type of study that merits the term has not emerged. In other words, cosmetic acupuncture is a swindle!
But at least cosmetic acupuncture is not harmful.
Wrong!
- It will cost you a lot of money because the therapist will persuade you that you need 10 treatment sessions or more.
- It can cause blotchiness and hyperpigmented spots, as mentioned above.
- It has been reported to cause extensive facial sclerosing lipogranulomatosis.
So, you want to improve your looks?
I am not sure what therapies work for this purpose. But I do know that cosmetic acupuncture isn’t one of them.
Earlier this year, I started the ‘WORST PAPER OF 2022 COMPETITION’. As a prize, I am offering the winner (that is the lead author of the winning paper) one of my books that best fits his/her subject. I am sure this will overjoy him or her. I hope to identify about 10 candidates for the prize, and towards the end of the year, I let my readers decide democratically on who should be the winner. In this spirit of democratic voting, let me suggest to you entry No 9. Here is the unadulterated abstract:
Background
With the increasing popularity of traditional Chinese medicine (TCM) by the global community, how to teach basic knowledge of TCM to international students and improve the teaching quality are important issues for teachers of TCM. The present study was to analyze the perceptions from both students and teachers on how to improve TCM learning internationally.
Methods
A cross-sectional national survey was conducted at 23 universities/colleges across China. A structured, self-reported on-line questionnaire was administered to 34 Chinese teachers who taught TCM course in English and to 1016 international undergraduates who were enrolled in the TCM course in China between 2017 and 2021.
Results
Thirty-three (97.1%) teachers and 900 (88.6%) undergraduates agreed Chinese culture should be fully integrated into TCM courses. All teachers and 944 (92.9%) undergraduates thought that TCM had important significance in the clinical practice. All teachers and 995 (97.9%) undergraduates agreed that modern research of TCM is valuable. Thirty-three (97.1%) teachers and 959 (94.4%) undergraduates thought comparing traditional medicine in different countries with TCM can help the students better understand TCM. Thirty-two (94.1%) teachers and 962 (94.7%) undergraduates agreed on the use of practical teaching method with case reports. From the perceptions of the undergraduates, the top three beneficial learning styles were practice (34.3%), teacher’s lectures (32.5%), case studies (10.4%). The first choice of learning mode was attending to face-to-face teaching (82.3%). The top three interesting contents were acupuncture (75.5%), Chinese herbal medicine (63.8%), and massage (55.0%).
Conclusion
To improve TCM learning among international undergraduates majoring in conventional medicine, integration of Chinese culture into TCM course, comparison of traditional medicine in different countries with TCM, application of the teaching method with case reports, and emphasization of clinical practice as well as modern research on TCM should be fully considered.
I am impressed with this paper mainly because to me it does not make any sense at all. To be blunt, I find it farcically nonsensical. What precisely? Everything:
- the research question,
- the methodology,
- the conclusion
- the write-up,
- the list of authors and their affiliations: Department of Chinese Integrative Medicine, Women’s Hospital, School of Medicine, Zhejiang University, Hangzhou, China, Department of Traditional Chinese Medicine, School of Basic Medicine, Qingdao University, Qingdao, China, Department of Chinese Integrative Medicine, The Second Affiliated Hospital of Kunming Medical University, Kunming, China, Department of Traditional Chinese Medicine, The Affiliated Hospital of Xuzhou Medical University, Xuzhou, China, Department of Traditional Chinese Medicine, Medical College, China Three Gorges University, Yichang, China, Basic Teaching and Research Department of Acupuncture and Moxibustion, College of Traditional Chinese Medicine, Xinjiang Medical University, Urumqi, China, Institute of Integrative Medicine, Dalian Medical University, Dalian, China, Department of Chinese and Western Medicine, Chongqing Medical University, Chongqing, China, Department of Chinese and Western Medicine, North Sichuan Medical College, Nanchong, China, Department of Chinese and Western Medicine, School of Medicine, Xiamen University, Xiamen, China, School of Traditional Chinese Medicine, Capital Medical University, Beijing, China, School of Traditional Chinese Medicine, Southern Medical University, Guangzhou, China, Department of Traditional Chinese Medicine, The First Affiliated Hospital of Soochow University, Suzhou, China, Department of Traditional Chinese Medicine, School of Medicine, Xiamen University, Xiamen, China, Department of Chinese Medicine/Department of Chinese Integrative Medicine, The First Affiliated Hospital of Anhui Medical University, Hefei, China, Department of Traditional Chinese Medicine, Shengjing Hospital Affiliated to China Medical University, Shenyang, China, Department of Acupuncture, Affiliated Hospital of Jiangsu University, Zhenjiang, China, Teaching and Research Section of Traditional Chinese Medicine, The Second Affiliated Hospital of Soochow University, Suzhou, China, Department of Traditional Chinese Medicine, The Second Affiliated Hospital of Harbin Medical University, Harbin, China, Department of Chinese Medicine, The First Affiliated Hospital of Anhui Medical University, Hefei, China, Department of Chinese Medicine, The First Affiliated Hospital of Kunming Medical University, Kunming, China, Department of Traditional Chinese Medicine, Shengli Clinical Medical College of Fujian Medical University, Fuzhou, China, Department of Chinese Medicine, The First Affiliated Hospital of Jinzhou Medicine University, Jinzhou, China, Department of Integrated Traditional and Western Medicine, The First Affiliated Hospital of Harbin Medical University, Harbin, China, Department of Chinese Medicine, The Second Affiliated Hospital of Guangzhou Medical University, Guangzhou, China, Department of Traditional Chinese Medicine, The First Affiliated Hospital of Fujian Medical University, Fuzhou, China.
- the journal that had this paper peer-reviewed and published.
But what impressed me most with this paper is the way the authors managed to avoid even the slightest hint of critical thinking. They even included a short paragraph in the discussion section where they elaborate on the limitations of their work without ever discussing the true flaws in the conception and execution of this extraordinary example of pseudoscience.
Is acupuncture more than a theatrical placebo? Acupuncture fans are convinced that the answer to this question is YES. Perhaps this paper will make them think again.
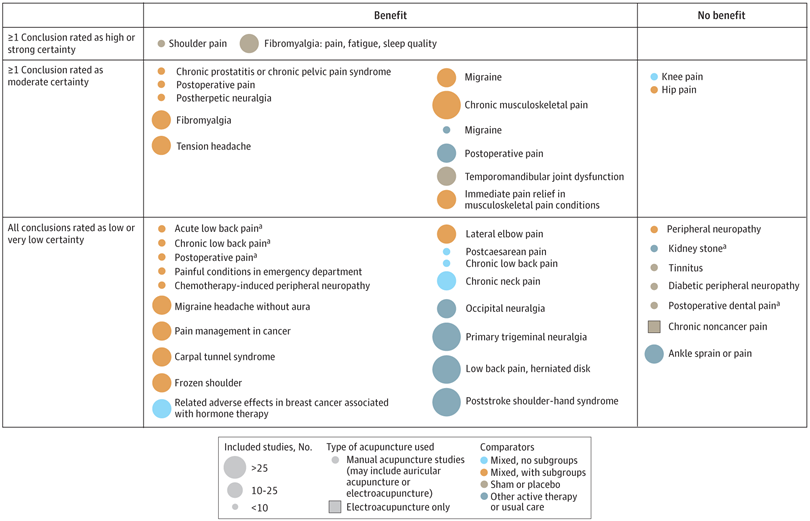
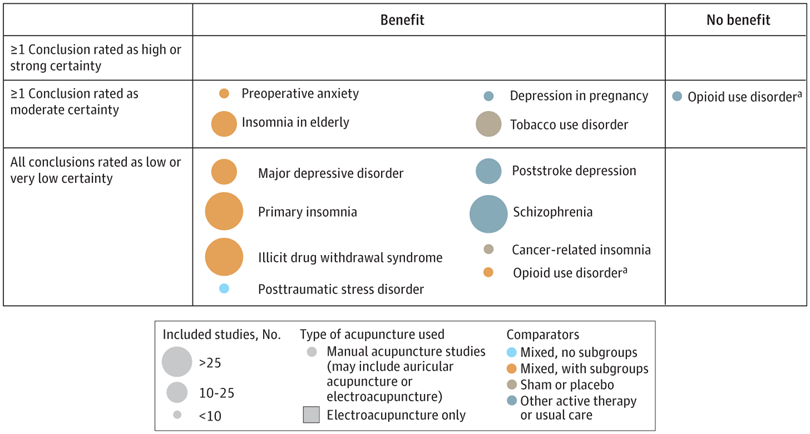
A new analysis mapped the systematic reviews, conclusions, and certainty or quality of evidence for outcomes of acupuncture as a treatment for adult health conditions. Computerized search of PubMed and 4 other databases from 2013 to 2021. Systematic reviews of acupuncture (whole body, auricular, or electroacupuncture) for adult health conditions that formally rated the certainty, quality, or strength of evidence for conclusions. Studies of acupressure, fire acupuncture, laser acupuncture, or traditional Chinese medicine without mention of acupuncture were excluded. Health condition, number of included studies, type of acupuncture, type of comparison group, conclusions, and certainty or quality of evidence. Reviews with at least 1 conclusion rated as high-certainty evidence, reviews with at least 1 conclusion rated as moderate-certainty evidence and reviews with all conclusions rated as low- or very low-certainty evidence; full list of all conclusions and certainty of evidence.
A total of 434 systematic reviews of acupuncture for adult health conditions were found; of these, 127 reviews used a formal method to rate the certainty or quality of evidence of their conclusions, and 82 reviews were mapped, covering 56 health conditions. Across these, there were 4 conclusions that were rated as high-certainty evidence and 31 conclusions that were rated as moderate-certainty evidence. All remaining conclusions (>60) were rated as low- or very low-certainty evidence. Approximately 10% of conclusions rated as high or moderate-certainty were that acupuncture was no better than the comparator treatment, and approximately 75% of high- or moderate-certainty evidence conclusions were about acupuncture compared with a sham or no treatment.
Three evidence maps (pain, mental conditions, and other conditions) are shown below
The authors concluded that despite a vast number of randomized trials, systematic reviews of acupuncture for adult health conditions have rated only a minority of conclusions as high- or moderate-certainty evidence, and most of these were about comparisons with sham treatment or had conclusions of no benefit of acupuncture. Conclusions with moderate or high-certainty evidence that acupuncture is superior to other active therapies were rare.
These findings are sobering for those who had hoped that acupuncture might be effective for a range of conditions. Despite the fact that, during recent years, there have been numerous systematic reviews, the evidence remains negative or flimsy. As 34 reviews originate from China, and as we know about the notorious unreliability of Chinese acupuncture research, this overall result is probably even more negative than the authors make it out to be.
Considering such findings, some people (including the authors of this analysis) feel that we now need more and better acupuncture trials. Yet I wonder whether this is the right approach. Would it not be better to call it a day, concede that acupuncture generates no or only relatively minor effects, and focus our efforts on more promising subjects?
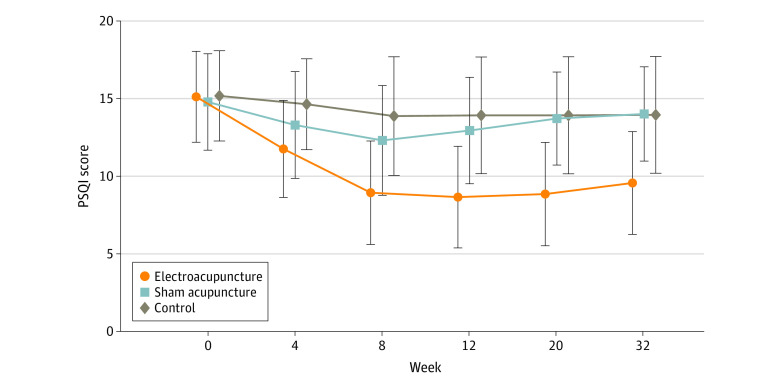
Electroacupuncture (EA) is often advocated for depression and sleep disorders but its efficacy remains uncertain. The aim of this study was, therefore, to “assess the efficacy and safety of EA as an alternative therapy in improving sleep quality and mental state for patients with insomnia and depression.”
A 32-week patient- and assessor-blinded, randomized, sham-controlled clinical trial (8-week intervention plus 24-week follow-up) was conducted from September 1, 2016, to July 30, 2019, at 3 tertiary hospitals in Shanghai, China. Patients were randomized to receive
- EA treatment and standard care,
- sham acupuncture (SA) treatment and standard care,
- standard care only as control.
Patients in the EA or SA groups received a 30-minute treatment 3 times per week (usually every other day except Sunday) for 8 consecutive weeks. All treatments were performed by licensed acupuncturists with at least 5 years of clinical experience. A total of 6 acupuncturists (2 at each center; including X.Y. and S.Z.) performed EA and SA, and they received standardized training on the intervention method before the trial. The regular acupuncture method was applied at the Baihui (GV20), Shenting (GV24), Yintang (GV29), Anmian (EX-HN22), Shenmen (HT7), Neiguan (PC6), and SanYinjiao (SP6) acupuncture points, with 0.25 × 25-mm and 0.30 × 40-mm real needles (Wuxi Jiajian Medical Device Co, Ltd), or 0.30 × 30-mm sham needles (Streitberger sham device [Asia-med GmbH]).
For patients in the EA group, rotating or lifting-thrusting manipulation was applied for deqi sensation after needle insertion. The 2 electrodes of the electrostimulator (CMNS6-1 [Wuxi Jiajian Medical Device Co, Ltd]) were connected to the needles at GV20 and GV29, delivering a continuous wave based on the patient’s tolerance. Patients in the SA group felt a pricking sensation when the blunt needle tip touched the skin, but without needle insertion. All indicators of the nearby electrostimulator were set to 0, with the light switched on. Standard care (also known as treatment as usual or routine care) was used in the control group. Patients receiving standard care were recommended by the researchers to get regular exercise, eat a healthy diet, and manage their stress level during the trial. They were asked to keep the regular administration of antidepressants, sedatives, or hypnotics as well. Psychiatrists in the Shanghai Mental Health Center (including X.L.) guided all patients’ standard care treatment and provided professional advice when a patient’s condition changed.
The primary outcome was change in Pittsburgh Sleep Quality Index (PSQI) from baseline to week 8. Secondary outcomes included PSQI at 12, 20, and 32 weeks of follow-up; sleep parameters recorded in actigraphy; Insomnia Severity Index; 17-item Hamilton Depression Rating Scale score; and Self-rating Anxiety Scale score.
Among the 270 patients (194 women [71.9%] and 76 men [28.1%]; mean [SD] age, 50.3 [14.2] years) included in the intention-to-treat analysis, 247 (91.5%) completed all outcome measurements at week 32, and 23 (8.5%) dropped out of the trial. The mean difference in PSQI from baseline to week 8 within the EA group was -6.2 (95% CI, -6.9 to -5.6). At week 8, the difference in PSQI score was -3.6 (95% CI, -4.4 to -2.8; P < .001) between the EA and SA groups and -5.1 (95% CI, -6.0 to -4.2; P < .001) between the EA and control groups. The efficacy of EA in treating insomnia was sustained during the 24-week postintervention follow-up. Significant improvement in the 17-item Hamilton Depression Rating Scale (-10.7 [95% CI, -11.8 to -9.7]), Insomnia Severity Index (-7.6 [95% CI, -8.5 to -6.7]), and Self-rating Anxiety Scale (-2.9 [95% CI, -4.1 to -1.7]) scores and the total sleep time recorded in the actigraphy (29.1 [95% CI, 21.5-36.7] minutes) was observed in the EA group during the 8-week intervention period (P < .001 for all). No between-group differences were found in the frequency of sleep awakenings. No serious adverse events were reported.
The result of the blinding assessment showed that 56 patients (62.2%) in the SA group guessed wrongly about their group assignment (Bang blinding index, −0.4 [95% CI, −0.6 to −0.3]), whereas 15 (16.7%) in the EA group also guessed wrongly (Bang blinding index, 0.5 [95% CI, 0.4-0.7]). This indicated a relatively higher degree of blinding in the SA group.
The authors concluded that, in this randomized clinical trial of EA treatment for insomnia in patients with depression, quality of sleep improved significantly in the EA group compared with the SA or control group at week 8 and was sustained at week 32.
This trial seems rigorous, it has a sizable sample size, uses a credible placebo procedure, and is reported in sufficient detail. Why then am I skeptical?
- Perhaps because we have often discussed how untrustworthy acupuncture studies from China are?
- Perhaps because I fail to see a plausible mechanism of action?
- Perhaps because the acupuncturists could not be blinded and thus might have influenced the outcome?
- Perhaps because the effects of sham acupuncture seem unreasonably small?
- Perhaps because I cannot be sure whether the acupuncture or the electrical current is supposed to have caused the effects?
- Perhaps because the authors of the study are from institutions such as the Shanghai Municipal Hospital of Traditional Chinese Medicine, the Department of Acupuncture and Moxibustion, Huadong Hospital, Fudan University, Shanghai,
- Perhaps because the results seem too good to be true?
If you have other and better reasons, I’d be most interested to hear them.
Camilla spent ten days at the end of October in a sophisticated meditation and fitness center in southern India. Life has recently been hectic for the Queen Consort: at 75, she has been in a non-stop succession of various ceremonies for the funeral of Elizabeth II, always one step behind her husband, not to mention her new status as sovereign… Enough to block her chakras in no time.
She came to the resort with her bodyguards and a handful of friends and was able to take advantage of the tailor-made treatments concocted for her by the master of the house, Dr Issac Mathai, who created this high-end holistic centre on a dozen hectares of scented gardens near Bangalore. The program includes massages, herbal steam baths, yoga, naturopathy, homeopathy, meditation, and Ayurvedic treatments to “cleanse, de-stress, soothe and revitalize the mind, body and soul”, as the establishment’s website states.
Guests are required to follow an individualized, meat-free diet, with organic food from the resort’s vegetable gardens, based on lots of salads or soups – Camilla is said to be a fan of sweet corn soup with spinach. Cigarettes and mobile phones are not allowed, although it is assumed that Camilla must have some privileges due to her status… and the basic rate for the suites, which starts at $950 a night – the price of the rooms varies between $260 and $760, the rate including a consultation with the doctors.
Charles and Camilla have been fans of the Soukya Centre in India for a decade. The place corresponds in every way to their deep-rooted convictions about health. Like her husband, Camilla is a follower of organic food, she also practices yoga and treats her face with creams made from nettle and bee venom. For his part, Charles has long been an advocate of alternative medicine, homeopathy, acupuncture, aromatherapy, and also hypnosis… He even set up a foundation to support complementary medicine by lobbying the British health service to include it in complementary therapies for certain patients, which caused an uproar among the pundits of traditional medicine.
________________________
If you suspected I was (yet again) sarcastic about the royal couple, you are mistaken. The text above is only my (slightly shortened) translation of an article published in the French magazine LE POINT (even the title is theirs). I found the article amusing and interesting; so, I looked up the Indian health center. Here are some of the things I found:
The 1st impression is that they are not shy about promotion calling themselves THE WORLD’S BEST AYURVEDA TREATMENT CENTER. The doctor in charge was once a ‘Consultant Physician’ at the Hale Clinic in London, where he treated a number of high-profile people. As his professional background, he offers this:
M.D. (Homeopathy); Hahnemann Post-Graduate Institute of Homeopathy, London M.R.C.H, London; Chinese Pulse Diagnosis and Acupuncture, WHO Institute of Traditional Chinese Medicine, Nanjing, China; Trained (Mind-Body Medicine Programme) at Harvard Medical School, USA
The approach of the center is described as follows:
The fundamental principle underlying Holistic Treatment is that the natural defense and immune system of an individual when strengthened, has the potential to heal and prevent diseases. In the age of super-specialisation where human beings are often viewed as a conglomeration of organs, it is crucial to understand ourselves as multi-dimensional beings with a body, mind and spirit. These interconnected dimensions need to be in perfect harmony to ensure real well-being.
And about homeopathy, they claim this:
Homeopathy originated in 1796 in Germany, and was discovered by Dr. Samuel Hahnemann, a German scientist. Homeopathy is popular today as a non-intrusive, holistic system of medicine. Instead of different medicines for different parts of the body, one single constitutional remedy is prescribed. As a system of medicine, Homeopathy is highly scientific, safe, logical and an extremely effective method of healing. For over 200 years people have used Homeopathy to maintain their good health, and also to treat and cure a wide range of illnesses like allergies, metabolic disorders, atopic dermatitis, Rheumatoid arthritis, Auto-immune disorders.
At this stage, I felt I had seen enough. Yes, you are right, we did not learn a lot from this little exploration. No, hold on! We did learn that homeopathy is highly scientific, safe, logical, and extremely effective!
The question, however, is should we believe it?
Yesterday, L’EXPRESS published an interview with me. It was introduced with these words (my translation):
Professor emeritus at the University of Exeter in the United Kingdom, Edzard Ernst is certainly the best connoisseur of unconventional healing practices. For 25 years, he has been sifting through the scientific evaluation of these so-called “alternative” medicines. With a single goal: to provide an objective view, based on solid evidence, of the reality of the benefits and risks of these therapies. While this former homeopathic doctor initially thought he was bringing them a certain legitimacy, he has become one of their most enlightened critics. It is notable as a result of his work that the British health system, the NHS, gave up covering homeopathy. Since then, he has never ceased to alert us to the abuses and lies associated with these practices. For L’Express, he looks back at the challenges of regulating this vast sector and deciphers the main concepts put forward by “wellness” professionals – holism, detox, prevention, strengthening the immune system, etc.
The interview itself is quite extraordinary, in my view. While UK, US, and German journalists usually are at pains to tone down my often outspoken answers, the French journalists (there were two doing the interview with me) did nothing of the sort. This starts with the title of the piece: “Homeopathy is implausible but energy healing takes the biscuit”.
The overall result is one of the most outspoken interviews of my entire career. Let me offer you a few examples (again my translation):
Why are you so critical of celebrities like Gwyneth Paltrow who promote these wellness methods?
Sadly, we have gone from evidence-based medicine to celebrity-based medicine. A celebrity without any medical background becomes infatuated with a certain method. They popularize this form of treatment, very often making money from it. The best example of this is Prince Charles, sorry Charles III, who spent forty years of his life promoting very strange things under the guise of defending alternative medicine. He even tried to market a “detox” tincture, based on artichoke and dandelion, which was quickly withdrawn from the market.
How to regulate this sector of wellness and alternative medicines? Today, anyone can present himself as a naturopath or yoga teacher…
Each country has its own regulation, or rather its own lack of regulation. In Germany, for instance, we have the “Heilpraktikter”. Anyone can get this paramedical status, you just have to pass an exam showing that you are not a danger to the public. You can retake this exam as often as you want. Even the dumbest will eventually pass. But these practitioners have an incredible amount of freedom, they even may give infusions and injections. So there is a two-tier health care system, with university-trained doctors and these practitioners.
In France, you have non-medical practitioners who are fighting for recognition. Osteopaths are a good example. They are not officially recognized as a health profession. Many schools have popped up to train them, promising a good income to their students, but today there are too many osteopaths compared to the demand of the patients (knowing that nobody really needs an osteopath to begin with…). Naturopaths are in the same situation.
In Great Britain, osteopaths and chiropractors are regulated by statute. There is even a Royal College dedicated to chiropractic. It’s a bit like having a Royal College for hairdressers! It’s stupid, but we have that. We also have professionals like naturopaths, acupuncturists, or herbalists who have an intermediate status. So it’s a very complex area, depending on the state. It is high time to have more uniform regulations in Europe.
But what would adequate regulation look like?
From my point of view, if you really regulate a profession like homeopaths, it means that these professionals may only practice according to the best scientific evidence available. Which, in practice, means that a homeopath cannot practice homeopathy. This is why these practitioners have a schizophrenic attitude toward regulation. On the one hand, they would like to be recognized to gain credibility. But on the other hand, they know very well that a real regulation would mean that they would have to close shop…
What about the side effects of these practices?
If you ask an alternative practitioner about the risks involved, he or she will take exception. The problem is that there is no system in alternative medicine to monitor side effects and risks. However, there have been cases where chiropractors or acupuncturists have killed people. These cases end up in court, but not in the medical literature. The acupuncturists have no problem saying that a hundred deaths due to acupuncture – a figure that can be found in the scientific literature – is negligible compared to the millions of treatments performed every day in this discipline. But this is only the tip of the iceberg. There are many cases that are not published and therefore not included in the data, because there is no real surveillance system for these disciplines.
Do you see a connection between the wellness sector and conspiracy theories? In the US, we saw that Qanon was thriving in the yoga sector, for example…
Several studies have confirmed these links: people who adhere to conspiracy theories also tend to turn to alternative medicine. If you think about it, alternative medicine is itself a conspiracy theory. It is the idea that conventional medicine, in the name of pharmaceutical interests, in particular, wants to suppress certain treatments, which can therefore only exist in an alternative world. But in reality, the pharmaceutical industry is only too eager to take advantage of this craze for alternative products and well-being. Similarly, universities, hospitals, and other health organizations are all too willing to open their doors to these disciplines, despite the lack of evidence of their effectiveness.
The objective of this study was to evaluate the effect of acupuncture on cognitive task performance in college students.
Sixty students aged 18-25 years were randomly allocated into acupuncture group (AG) (n=30) and control group (CG) (n=30). The AG underwent 20 min of acupuncture/day, while the CG underwent their normal routine for 10 days. Assessments were performed before and after the intervention.
Between-group analysis showed a significant increase in AG’s six-letter cancellation test (SLCT) score compared with CG. Within-group analysis showed a significant increase in the scores of all tests (i.e. SLCT, forward and backward Digit span test [DST]) in AG, while a significant increase in backward DST was observed in CG.
The authors concluded that acupuncture has a beneficial effect on improving the cognitive function of college students.
I am unable to access the full paper [it is behind a paywall]. Thus, I am unable to assess the study in further detail. As I am skeptical about the validity of the effect, I can only assume that it is due to the expectation of the volunteers receiving acupuncture. There was not even an attempt to control for placebo effects!
The over-stated conclusion made me wonder what else the 1st author has published. It turns out he has three more Medline-listed papers to his name all of which are about so-called alternative medicine (SCAM).
The 1st one is an RCT similar to the one above, i.e. without an attempt to control for placebo effects. Its conclusion is equally over-stated: Acupuncture could be considered as an effective treatment modality for the management of primary dysmenorrhea.
The other two papers refer to one case report each. Despite the fact that case reports (as any researcher must know) do not lend themselves to conclusions about the effectiveness of the treatments employed, the authors’ conclusions seem to again over-state the case:
- This suggests that integrative Naturopathy and Yoga therapies could be considered as an adjuvant to conventional medicine in rheumatoid arthritis associated with type-2 diabetes and essential hypertension.
- Though the results are encouraging, further studies are required with larger sample size and advanced inflammatory markers.
What does that tell us?
I don’t know about you, but I would not rely on acupuncture to improve my mental performance.