spinal manipulation
I came across an article entitled “Consent for Paediatric Chiropractic Treatment (Ages 0-16)“. Naturally, it interested me. Here is the full paper; I have only inserted a few numbers in square brackets which refer to my comments below:
By law, all Chiropractors are required to inform you of the risks and benefits of chiropractic spinal manipulation and the other types of care we provide. Chiropractors use manual therapy alongside taking a thorough history, and doing a neurological, orthopaedic and chiropractic examination to both diagnose and to treat spinal, cranial and extremity dysfunction. This may include taking joints to the end range of function, palpating soft tissues (including inside the mouth and the abdomen), mobilisation, soft tissue therapy and very gentle manipulation [1]. Our Chiropractors have been educated to perform highly specific types of bony or soft tissue manipulation and we strive to follow a system of evidence-based care [2]. At the core of our belief system is “Do No Harm”. We recognise that infants and children are not tiny adults. The force of an adjustment used in a child is at least less than half of what we might use with a fully grown adult. Studies by Hawk et al (2016) and Marchand (2013) agreed that Chiropractors use 15 – 35 x less force in the under 3-month age group when compared to medical practitioners doing manipulation (Koch, 2002) [3]. We also use less force in all other paediatrics groups, especially when compared to adults (Marchand, 2013). In addition to using lower force, depth, amplitude and speed in our chiropractic adjustments [4], we utilise different techniques. We expect all children under the age of 16 years to be accompanied by a responsible adult during appointments unless prior permission to treat without a consenting adult e.g., over the age of 14 has been discussed with the treating chiropractor.
Risks
- Research into chiropractic care for children in the past 70 years has shown it to have a low risk of adverse effects (Miller, 2019) [5]. These effects tend to be mild and of short duration e.g., muscular or ligament irritation. Vorhra et al (2007) found the risk of severe of adverse effects (e.g. fracture, quadriplegia, paraplegia, and death) is very, very rare and was more likely to occur in individuals where there is already serious underlying pathology and missed diagnosis by other medical profession [6]. These particular cases occurred more than 25 years ago and is practically unheard of now since research and evidence-based care has become the norm [7].
- The most common side effect in infants following chiropractic treatment includes fussiness or irritability for the first 24 hours, and sleeping longer than usual or more soundly. (Miller and Benfield, 2008) [8]
- In older children, especially if presenting with pain e.g., in the neck or lower back, the greatest risk is that this pain may increase during examination due to increasing the length of involved muscles or ligaments [9]. Similarly, the child may also experience pain, stiffness or irritability after treatment (Miller & Benfield, 2008) [10]. Occasionally children may experience a headache.[11] We find that children experience side effects much less often than adults.[12]
Benefits
- Your child might get better with chiropractic care. [13] If they don’t, we will refer you on [14].
- Low risk of side effects and very rare risk of serious adverse effects [15].
- Drug-free health care. We are not against medication, but we do not prescribe [16].
- Compared with a medical practitioner, manual therapy carried out by a chiropractor is 20 x less likely to result in injury (Koch et al 2002, Miller 2009).[17]
- Children do not often require long courses of treatment (>3 weeks) unless complicating factors are present.[18]
- Studies have shown that parents have a high satisfaction rate with Chiropractic care [19].
- Physical therapies are much less likely to interfere with biomedical treatments. (McCann & Newell 2006) [20]
- You will have a better understanding of diagnosis of any complain and we will let you know what you can do to help.[21]
We invite you to have open discussions and communication with your treating chiropractor at all times. Should you need any further clarification please just ask.
References
- Hawk, C. Shneider, M.J., Vallone, S and Hewitt, E.G. (2016) – Best practises recommendations for chiropractic care of children: A consensus update. JMPT, 39 (3), 158-168.
- Marchand, A. (2013) – A Proposed model with possible implications for safety and technique adaptations for chiropractic spinal manipulative therapy for infants and children. JMPT, 5, 1-14
- Koch L. E., Koch, H, Graumann-Brunnt, S. Stolle, D. Ramirez, J.M., & Saternus, K.S. (2002) – Heart rate changes in response to mild mechanical irritation of the high cervical cord region in infants. Forensic Science International, 128, 168-176
- Miller J (2019) – Evidence-Based Chiropractic Care for Infants: Rational, Therapies and Outcomes. Chapter 11: Safety of Chiropractic care for Infants p111. Praeclarus Press
- Vohra, S. Johnston, B.C. Cramer, K, Humphreys, K. (2007) – Adverse events associated with paediatric spinal manipulation: A Systematic Review. Pediatrics, 119 (1) e275-283
- Miller, J and Benfield (2008) – Adverse effects of spinal manipulative therapy in children younger than 3 years: a retrospective study in a chiropractic teaching clinic. JMPT Jul-Aug;31(6):419-23.
- McCann, L.J. & Newell, S.J. (2006). Survey of paediatric complementary and alternative medicine in health and chronic disease. Archives of Diseases of Childhood, 91, 173-174
- Corso, M., Cancelliere, C. , Mior., Taylor-Vaise, A. Côté, P. (2020) – The safety of spinal manipulative therapy in children under 10 years: a rapid review. Chiropractic Manual therapy 25: 12
___________________________________
- “taking joints to the end range of function” (range of motion, more likely) is arguably not “very gently”;
- “we strive to follow a system of evidence-based care”; I do not think that this is possible because pediatric chiropractic care is hardy evidence-based;
- as a generalizable statement, this seems to be not true;
- ” lower force, depth, amplitude and speed”; I am not sure that there is good evidence for that;
- research has foremost shown that there might be significant under-reporting;
- to blame the medical profession for diagnoses missed by chiropractors seems odd;
- possibly because of under-reporting;
- possibly because of under-reporting;
- possibly because of under-reporting;
- possibly because of under-reporting;
- possibly because of under-reporting;
- your impressions are not evidence;
- your child might get even better without chiropractic care;
- referral rates of chiropractors tend to be low;
- possibly because of under-reporting;
- chiropractors have no prescription rights but some lobby hard for it;
- irrelevant if we consider the intervention useless and thus obsolete;
- any evidence for this statement?;
- satisfaction rates are no substitute for real evidence;
- that does not mean they are effective, safe, or value for money;
- this is perhaps the strangest statement of them all – do chiropractors think they are the optimal diagnosticians for all complaints?
_____________________________________
According to its title, the paper was supposed to deal with consent for chiropractic pediatric care. It almost totally avoided the subject and certainly did not list the information chiropractors must give to parents before commencing treatment.
Considering the arguments that the article did provide has brought me to the conclusion that chiropractors who treat children are out of touch with reality and seem in danger of committing child abuse.
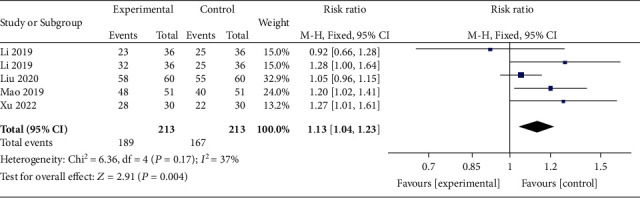
This meta-analysis aimed “to provide better evidence of the efficacy of manual therapy (MT) on adolescent idiopathic scoliosis (AIS)”. 
All RCTs of MT for the management of patients with AIS were included in the present study. The treatment difference between the experimental and control group was mainly MT. The outcomes consisted of the total effective rate, the Cobb angle, and Scoliosis Research Society-22 (SRS-22) questionnaire score. Electronic database searches were conducted from database inception to July 2022, including the Cochrane Library, PubMed, Web of Science, Embase, Wanfang Data, CNKI, and VIP. The pooled data were analyzed using RevMan 5.4 software.
Four RCTs with 213 patients in the experimental groups were finally included. There are 2 studies of standalone MT in the experimental group and 3 studies of MT with identical conservative treatments in the control group. Three trials reported the total effective rate and a statistically significant difference was found (P = 0.004). Three trials reported Cobb angle; a statistical difference was found (P = 0.01). Then, sensitivity analysis showed that there was a significant difference in the additional MT subgroup (P < 0.00001) while not in the standalone MT subgroup (P = 0.41). Three trials reported SRS-22 scores (P = 0.55) without significant differences.
The authors concluded that there is insufficient data to determine the effectiveness of spinal manipulation limited by the very low quality of included studies. High-quality studies with appropriate design and follow-up periods are warranted to determine if MT may be beneficial as an adjunct therapy for AIS. Currently, there is no evidence to support spinal manipulation. 
The treatment of idiopathic scoliosis depends on the age, curve size, and progression of the condition. Therapeutic options include observation, bracing, physiotherapy, and surgery. They do NOT include MT because it is neither a plausible nor effective solution to this problem. It follows that further studies are not warranted and should be discouraged.
And, even if you disagree with me here and feel that further studies might be justified, let me remind you that proper research is never aimed at providing better evidence that a therapy works (as the authors of this odd paper seem to think); it must be aimed at testing whether it is effective!
This single-blind, randomized, clinical trial was aimed at determining the long-term clinical effects of spinal manipulative therapy (SMT) or mobilization (MOB) as an adjunct to neurodynamic mobilization (NM) in the management of individuals with Lumbar Disc Herniation with Radiculopathy (DHR).
Forty participants diagnosed as having a chronic DHR (≥3 months) were randomly allocated into two groups with 20 participants each in the SMT and MOB groups.
Participants in the SMT group received high-velocity, low-amplitude manipulation, while those in the MOB group received Mulligans’ spinal mobilization with leg movement. Each treatment group also received NM as a co-intervention, administered immediately after the SMT and MOB treatment sessions. Each group received treatment twice a week for 12 weeks.
The following outcomes were measured at baseline, 6, 12, 26, and 52 weeks post-randomization; back pain, leg pain, activity limitation, sciatica bothersomeness, sciatica frequency, functional mobility, quality of life, and global effect. The primary outcomes were pain and activity limitation at 12 weeks post-randomization.
The results indicate that the MOB group improved significantly better than the SMT group in all outcomes (p < 0.05), and at all timelines (6, 12, 26, and 52 weeks post-randomization), except for sensory deficit at 52 weeks, and reflex and motor deficits at 12 and 52 weeks. These improvements were also clinically meaningful for neurodynamic testing and sensory deficits at 12 weeks, back pain intensity at 6 weeks, and for activity limitation, functional mobility, and quality of life outcomes at 6, 12, 26, and 52 weeks of follow-ups. The risk of being improved at 12 weeks post-randomization was 40% lower (RR = 0.6, CI = 0.4 to 0.9, p = 0.007) in the SMT group compared to the MOB group.
The authors concluded that this study found that individuals with DHR demonstrated better improvements when treated with MOB plus NM than when treated with SMT plus NM. These improvements were also clinically meaningful for activity limitation, functional mobility, and quality of life outcomes at long-term follow-up.
Yet again, I find it hard to resist playing the devil’s advocate: had the researchers added a third group with sham-MOB, they would have perhaps found that this group would have recovered even faster. In other words, this study might show that SMT is no good for DHR (which I find unsurprising), but it does NOT demonstrate MOB to be an effective therapy.
On this blog, we are often told that only a few chiros still believe in Palmer’s gospel of subluxation. This 2023 article seems to tell a different story.
The authors claim that the term demonstrates the widespread use and acceptance of the term subluxation and
acknowledges the broader chiropractic interpretation by recognition and adoption of the term outside the profession. In particular, it emphasizes the medical recognition supported by some of the medical evidence incorporating the
construct of a chiropractic vertebral subluxation complex and its utilization in practice.
The vertebral subluxation concept is similar to the terms spinal dysfunction, somatic dysfunction, segmental dysfunction or the vague vertebral lesion. These terms are primarily used by osteopaths, physiotherapists, and medical doctors to focus their manipulative techniques, but they relate primarily to the physical-mechanical aspects. In this respect, these terms are limited in what they signify. The implication of just plain osseous biomechanical dysfunction does not incorporate the wider ramifications of integrated neural, vascular, and internal associations which may involve greater ramifications, and should be more appropriately referred to as a vertebral subluxation complex (VSC).
The authors also claim that, in recognition of acceptance of the subluxation terminology, a 2015 study in North America found that a majority of the 7,455 chiropractic students surveyed agreed or strongly agreed (61.4%) that
the emphasis of chiropractic intervention in practice is to eliminate vertebral subluxations/vertebral subluxation complexes. A further 15.2% neutral, and only 23.3% disagreeing. It is suggested that ‘modulation’ of vertebral subluxations may have attracted an even higher rate of agreement.
The authors conclude that the evidence indicates that medicine, osteopathy, and physiotherapy have all
used the term ‘subluxation’ in the chiropractic sense. However, the more appropriate, and inclusive descriptive term of vertebral subluxation complex is widely adopted in chiropractic and the WHO ICD-10. It would be most incongruous for chiropractic to move away from using subluxation when it is so well established.
A move to deny clarity to the essence of chiropractic may well affect the public image of the profession. As Hart states ‘Identifying the chiropractic profession with a focus on vertebral subluxation would give the profession uniqueness not duplicated by other health care professions and, therefore, might legitimatise the existence of chiropractic as a health care profession. An identity having a focus on vertebral subluxation would also be consistent with the original intent of the founding of the chiropractic profession.’
The term ‘vertebral subluxation’ has been in general use and understanding in the chiropractic profession as is ‘chiropractic subluxation’ and ‘vertebral subluxation complex’ (VSC). It is a part of the profession’s heritage. Critics of concepts regarding subluxation offer no original evidence to support their case, and that appears to be just political opinion rather than providing evidence to substantiate their stand.
The evidence presented in this paper supports the contention that there would be no vertebrogenic symptoms associated with physiologically normal vertebral segments. The term designated by chiropractors to identify abnormal or pathophysiological segmental dysfunction is the vertebral subluxation. It has been a part of chiropractic heritage for over 120 years.
__________________________
Vis a vis such a diatribe of compact BS, I am tempted to point out that “critics of concepts regarding subluxation offer no original evidence to support their case” mainly because it is not they who have to produce the evidence. It is the chiropractic profession that needs to do that.
But they are evidently unable to do it.
Why?
Because chiropractic subluxation is a myth and an invention by their chief charlatan.
It is true that this fabrication is intimately linked to the identity of chiropractic.
It is furthermore true that chiros feel unable to throw it overboard because they would lose their identity.
What follows is simple:
Chiropractic is a fraud.
Yes, this post is yet again about the harm chiropractors do.
No, I am not obsessed with the subject – I merely consider it to be important.
This is a case presentation of a 44-year-old male who was transferred from another emergency department for left homonymous inferior quadrantanopia noted on an optometrist visit. He reported sudden onset left homonymous hemianopia after receiving a high-velocity cervical spine adjustment at a chiropractor appointment for chronic neck pain a few days prior.
The CT angiogram of the head and neck revealed bilateral vertebral artery dissection at the left V2 and right V3 segments. MRI brain confirmed an acute infarct in the right medial occipital lobe. His right PCA stroke was likely embolic from the injured right V3 but possibly from the left V2 as well. As the patient reported progression from a homonymous hemianopia to a quadrantanopia, he likely had a migrating embolus.
The authors discussed that arterial dissection accounts for about 2% of all ischemic strokes, but maybe between 8–25% in patients less than 45 years old. Vertebral artery dissection (VAD) can result from trauma from sports, motor vehicle accidents, and chiropractor neck manipulations to violent coughing/sneezing.
It is estimated that 1 in 20,000 spinal manipulation results in vertebral artery aneurysm/dissection. Patients who have multiple chronic conditions are reporting higher use of so-called alternative medicine (SCAM), including chiropractic manipulation. Education about the association between VAD and chiropractor maneuvers can be beneficial to the public as these are preventable acute ischemic strokes. In addition, VAD symptoms can be subtle and patients presenting to chiropractors may have distracting pain masking their deficits. Evaluating for appropriateness of cervical manipulation in high‐risk patients and detecting early clinical signs of VAD by chiropractors can be beneficial in preventing acute ischemic strokes in young patients.
Here we have a rare instance where the physicians who treated the chiro-victim were sufficiently motivated to present their findings and document them in the medical literature. Their report was published in 2021 as an abstract in conference proceedings. In other words, the report is not easy to find. Even though two years have passed, the full article does not seem to have emerged, and chances are that it will never be published.
The points I am trying to make are as follows:
- Complications after chiropractic manipulation do happen and are probably much more frequent than chiros want us to believe.
- They are only rarely reported in the medical literature because the busy clinicians who end up treating the victims do not consider this a priority and because many cases are settled in or out of court.
- Normally, it would be the ethical/moral duty of the chiros who have inflicted the damage to do the reporting.
- Yet, they seem too busy ripping off more patients by doing neck manipulations that do more harm than good.
- And then they complain that the evidence is insufficient!!!
I came across an article that seems highly relevant to our recurring debates about the dangers of chiropractic. Since few of us might be readers of the Louisville Courier, I take the liberty of reproducing here a shortened version of it:
Amber Burgess, then 33, had never set foot in a chiropractor’s office when she went to Dr. Adam Fulkerson’s Heartland Family Chiropractic in Elizabethtown on May 18, 2020. In contrast, Becca Barlow, 31, had seen Dr. Leah Wright at Louisville Family Chiropractic 29 times for adjustments over three years when she went there on Jan. 7, 2019, seeking relief for “nursing mother’s neck.” Both say they will never see a chiropractor again. “That visit was my first – and last,” said Burgess, a former utility bucket-truck assembler.
In separate lawsuits, they claim they suffered strokes after chiropractic adjustments; Barlow, herself a nurse, said she realized she was having one before she even left the office and told Wright’s staff to call 911.
Citing studies on human cadavers and other research, chiropractors claim adjustments are physically incapable of causing tears to arteries that in turn cause strokes by blocking the flow of blood to the brain and other organs. In an opening statement in the trial of Barlow’s suit last March, attorney John Floyd Jr., counsel for Wright and the National Chiropractic Mutual Insurance Co., said no one has ever proved adjustments cause the tears – known as dissection – only that there is an “association” between them. “We associate the crowing of roosters with sunrise,” he told the jury. “But that doesn’t mean roosters cause the sun to come up.” Floyd also cited studies he said prove that when a patient strokes out immediately after adjustments, like Barlow, it is because they already were suffering from artery injuries when they sought treatment from their chiropractor.
Louisville attorney Brian Clare, who represents both Barlow and Burgess, previously settled two cases in Jefferson County, and has another suit pending in Warren Circuit Court. He said in an interview that “every time chiropractors perform adjustments on the neck they are playing with fire. They can go too far, too fast, turning the neck past therapeutic limits,” he said.
The jury in Barlow’s case emphatically rejected the chiropractic profession’s defenses. “We found those claims to be unbelievable,” said jury foreman Joseph Tucker, a lawyer, who noted Barlow had no symptoms before her adjustments. By a 9-3 vote, the jury awarded her $1,130,800, including $380,000 in medical expenses and $750,000 for pain and suffering.
Witnesses testified that Barlow fell off the table and vomited almost immediately after her adjustment, showing classic stroke symptoms, including vertigo, dizziness, numbness, and nausea. She lost consciousness, had to be intubated in an ambulance, then raced to Norton Brownsboro Hospital, where she underwent emergency surgery to restore the flow of blood to her arteries and save her life. Three of the four arteries in her neck had been dissected.
Burgess, in Elizabethtown, suffered a stroke in her spine that her expert, Dr. Louis Caplan, a neurology professor at Harvard University, said also was caused by her cervical manipulations. Caplan says he’s cared for more than 15,000 stroke patients over 45 years.
Fulkerson has denied liability; his lawyer, James Grohman, said he couldn’t comment because the case is pending; the trial is set for Aug. 28 in Hardin Circuit Court Caplan said in a report that Burgess’s stroke left her with partial but permanent paralysis in her arms and legs. She uses a wheelchair and walker with wheels to get around. She said she can’t work, can’t drive, and that while she can dress herself, it takes hours to get ready. She fears they will have to give up their plans to have a baby.
By any measure, strokes associated with adjustments are rare, although their incidence is disputed. The American Chiropractic Association says arteries are damaged in only one to three adjustments out of 100,000 But a 2001 report in the New England Journal of Medicine estimated dissections occur in 1 of 20,000 adjustments. And Dr. Alan Brafman, an Atlanta chiropractor, has said they occur more often than that. Brafman wrote that he’s consulted in 1,100 cases, including Barlow’s, and found in most of them, chiropractors were at fault, causing vascular damage that is “a tragic, life-altering situation for all parties involved.” Wright’s experts themselves divulged they had been retained in 200 cases, according to Clare, which he said suggests chiropractic-related strokes are more common than suspected. A survey at Stanford University in 2008 of 177 neurologists found 55 had patients who suffered strokes after seeing chiropractors, while a 2018 study in West Virginia found one in 48 chiropractors experienced such an event. Neurologists and other physicians point to a 2001 study in STROKE of 582 stroke patients that found they were five times more likely to have seen a chiropractor in the previous five days before their artery dissection than a control group without such injuries. The American Heart Association and other medical groups recommend that patients also be warned about the risks; Barlow said she never would have undergone her final manipulation if she had been informed.
__________________________
Yet again, I am impressed by the number of cases that go to court where a settlement of some sort is reached and further reporting of the incident is prevented. As a consequence, these cases are not published in the medical literature. In turn, this means that chiropractors can continue to claim that these complications do not exist or are exceedingly rare.
- The truth, however, is that NOBODY can provide accurate incidence figures.
- The truth is that, even if such complications were rare, they are devastating.
- The truth is that neck manipulations do not generate any or very little benefit.
- The truth is that their risk/benefit balance is not positive.
- The truth is that we, therefore, have an ethical duty to tell potential patients about it.
I feel that I cannot repeat my warning often enough:
AVOID CHIROPRACTORS.
THEY CAUSE MORE HARM THAN GOOD!
It has been reported that a young woman’s visit to a chiropractor left her unable to walk due to a torn artery.
Mariah Bond, 29, went to visit a chiropractor in the hope to get some relief from her neck pain. During the appointment, the chiropractor quickly twisted her neck from side to side. “It cracked both ways and I’d seen chiropractor videos so I thought it was normal but when I stood up I got super dizzy,” Mariah recalled. Next, Mariah started profusely vomiting and her hand began to tingle. Then she was rushed to a hospital.
It took a few hours before the doctors could find the diagnosis. “I was still throwing up constantly, it was non-stop. I couldn’t open my eyes because if I did I’d start throwing up because I was so dizzy,” Mariah said. “I was transferred via ambulance to another hospital where they did a CT scan and confirmed that I was having a stroke.”
It turned out that Mariah’s chiropractor dissected an artery in her neck which then limited the blood supply to the brain. Mariah was kept in the hospital for five days while her condition was monitored. During that time, she was left unable to walk. But slowly she did become able to rely on a zimmer frame to get around. “I couldn’t walk properly or correctly use my hands to eat, it was like I was a child. It was very weird. My brain was there but I couldn’t do it,” she stated. “My first stroke was a cerebral stroke and they were saying that I probably had a mini-stroke as I was having weird feelings in my legs. They were very confused because that wasn’t common with the stroke I had, so they said that I probably had two.”
Within a fortnight, Mariah was able to walk again but had to have physiotherapy for two months before she could return to work. After her last CT scan, she received the good news that the dissected vessel had completely healed. She said: “I was very strong-willed at the time because everyone was telling me how well I was handling this. I think my husband was more scared than I was, poor thing.”
Mariah has vowed never to visit a chiropractor again and is doing her best to raise awareness of the damage they can cause. “I was shocked because I’m so young and you don’t really hear about young people having strokes, especially from the chiropractor. I’m pretty paranoid with my neck now. I know I probably shouldn’t be but sometimes if I have a weird feeling in my head, it would probably be called PTSD, I automatically start thinking am I having a stroke? I start freaking out. I’d tell people not to go to a chiropractor. I’ve already told a million people not to do it. Just don’t go or at least don’t let them do your neck.”
____________________________
I would be surprised if this case ever got written up as a proper case report and published in a medical journal. We did a survey years ago where we found over 35 cases of severe complications after chiropractic in the UK within a period of 12 months. The most amazing result was that none of these cases had been published. In other words, under-reporting was precisely 100%.
Mariah’s case might be a true rarety, or it might be a fairly common event. It might be a most devastating occurrence, or there could be far worse events.
We simply do not know because under-reporting is huge.
Meanwhile, chiropractors – the professionals who should long have made sure that under-reporting becomes minimal or non-existent – claim that there is no evidence that strokes happen at all or regularly or often. They can do this because the medical literature seems to confirm their opinion. The only reporting system that seems to exist, the “chiropractic patient incident reporting and learning system” (CPiRLS), is for several reasons woefully inadequate and also plagued by under-reporting.
So, what advice can I possibly give to consumers in such a situation? I feel that the only thing one can recommend is to
stay well clear of chiropractors
until they finally present us with sufficient and convincing data.
In one of my last posts, I was rather dismissive of veterinary chiropractic.
Was I too harsh?
I did ask readers who disagree with my judgment to send me their evidence.
Sadly, none arrived!
Therefore, I did several further literature searches and found a recent review of the topic. It included 14 studies; 13 were equine and one was a canine study. Seven of these were cohort studies and seven were randomized controlled clinical trials. . Study quality was low (n = 4), moderate (n = 7), and high (n = 3) and included a wide array of outcome parameters with varying levels of efficacy and duration of therapeutic effects, which prevented further meta-analysis. The authors concluded that it was difficult to draw firm conclusions despite all studies reporting positive effects. Optimal technique indications and dosages need to be determined to improve the standardization of these treatment options.
This, I think, can hardly be called good evidence. But I also found this more recent paper:
Chiropractic care is a common treatment modality used in equine practice to manage back pain and stiffness but has limited evidence for treating lameness. The objective of this blinded, controlled clinical trial was to evaluate the effect of chiropractic treatment on chronic lameness and concurrent axial skeleton pain and dysfunction. Two groups of horses with multiple limb lameness (polo) or isolated hind limb lameness (Quarter Horses) were enrolled. Outcome measures included subjective and objective measures of lameness, spinal pain and stiffness, epaxial muscle hypertonicity, and mechanical nociceptive thresholds collected on days 0, 14, and 28. Chiropractic treatment was applied on days 0, 7, 14, and 21. No treatment was applied to control horses. Data was analyzed by a mixed model fit separately for each response variable (p < 0.05) and was examined within each group of horses individually. Significant treatment effects were noted in subjective measures of hind limb and whole-body lameness scores and vertebral stiffness. Limited or inconsistent therapeutic effects were noted in objective lameness scores and other measures of axial skeleton pain and dysfunction. The lack of pathoanatomical diagnoses, multilimb lameness, and lack of validated outcome measures likely had negative impacts on the results.
Great! So, we finally have an RCT of chiropractic for horses. Unfortunately, the study is less than convincing:
- It included just 20 polo horses plus 18 horses active in ridden or competitive work all suffering from lameness.
- The authors state that ‘horses were numerically randomized to treatment and control groups’; yet I am not sure what this means.
- Treatment consisted of high-velocity, low-amplitude, manually applied thrusts to sites of perceived pain or stiffness with the axial and appendicular articulations. Treatment was applied on days 0, 7, 14, and 21 by a single examiner. The control group received no treatment and was restrained quietly for 15 min to simulate the time required for chiropractic treatment. In other words, no placebo controls were used.
- The validity of the many outcome measures is unknown.
- The statistical analyses seem odd to me.
- No correction for multiple statistical tests was done.
- Most of the outcomes show no significant effect.
- Overall, there were some small positive treatment effects based on subjective assessment of lameness, but no measurable treatment effects on objective measures of limb lameness.
- The polo horses began their competition season at the beginning of the study which would have confounded the outcomes.
What does all this tell us about veterinary chiropractic?
Not a lot.
All we can safely say, I think, is that veterinary chiropractic is not evidence-based and that claims to the contrary are certainly ill-informed and most probably of a promotional nature.
This study examined the incidence and severity of adverse events (AEs) of patients receiving chiropractic spinal manipulative therapy (SMT), with the hypothesis that < 1 per 100,000 SMT sessions results in a grade ≥ 3 (severe) AE. A secondary objective was to examine independent predictors of grade ≥ 3 AEs.
The researchers retrospectively identified patients with SMT-related AEs from January 2017 through August 2022 across 30 chiropractic clinics in Hong Kong. AE data were extracted from a complaint log, including solicited patient surveys, complaints, and clinician reports, and corroborated by medical records. AEs were independently graded 1–5 based on severity (1-mild, 2-moderate, 3-severe, 4-life-threatening, 5-death).
Among 960,140 SMT sessions for 54,846 patients, 39 AEs were identified, two were grade 3, both of which were rib fractures occurring in women age > 60 with osteoporosis, while none were grade ≥ 4, yielding an incidence of grade ≥ 3 AEs of 0.21 per 100,000 SMT sessions (95% CI 0.00, 0.56 per 100,000). There were no AEs related to stroke or cauda equina syndrome. The sample size was insufficient to identify predictors of grade ≥ 3 AEs using multiple logistic regression.
The authors concluded that, in this study, severe SMT-related AEs were reassuringly very rare.
This is good news for all patients who consult chiropractors. However, there seem to be several problems with this study:
- Data originated from 30 affiliated chiropractic clinics with 38 chiropractors (New York Chiropractic & Physiotherapy Center, EC Healthcare, Hong Kong). These clinics are integrated into a larger healthcare organization, including several medical specialties and imaging and laboratory testing centers that utilize a shared medical records system. The 38 chiropractors represent only a little more than 10% of all chiropractors working in Hanh Kong and are thus not representative of all chiropractors in that region. Is it possible that the participating chiropractors were better trained, more gentle, or more careful than the rest?
- Data regarding AEs was obtained from a detailed complaint log that was routinely aggregated from several sources by a customer service department. One source of AEs in this log was a custom survey administered to patients after their 1st, 2nd, and 16th visits. Additional AEs derived from follow-up phone calls by a personal health manager. This means that not all AE might have been noted. Some patients might not have complained, others might have been too ill to do so. And, of course, dead patients cannot complain. The authors state that “the response to the SMS questionnaire was low. It is possible that severe AEs occurred but were not reported or recorded through these or other methods of ascertainment”.
- The 39 AEs potentially related to chiropractic SMT included increased symptoms related to the patient’s chief complaint (n = 28), chest pain without a fracture on imaging (n = 4), jaw pain (n = 3), rib fracture confirmed by imaging (n = 2), headache and dizziness without evidence of stroke (n = 1), and new radicular symptoms (n = 1). Of the 39 AEs, grade 2 were most common (n = 32, 82%), followed by grade 1 (n = 5, 13%), and grade 3 (n = 2, 5%). There were no cases of stroke, transient ischemic attack (TIA), vertebral or carotid artery dissection, cauda equina syndrome, or spinal fracture. Yet, headache and dizziness could be signs of a TIA.
- Calculating the rate of AEs per SMT session might be misleading and of questionable value. Are incidence rates of AEs not usually expressed as AE/patient? In this case, the % rate would be almost 20 times higher.
Altogether, this is a laudable effort to generate evidence for the risks of SMT. The findings seem reassuring but sadly they are not fully convincing.
The McTimoney College of Chiropractic just announced that it has established a new four-year program in veterinary chiropractic for college students:
It means that those without a prior degree can undertake the training and education necessary to enter this coveted career. To date, animal chiropractors were required to have a prior qualification in human chiropractic or a degree in the relevant sciences.
Applications for the new program are being accepted from September 2023. Students will attend Abingdon-based University, Oxford, and a variety of practical locations, enabling the development of academic knowledge and the application of practical skills together . Modules include anatomy and physiology, veterinary science, practice and professionalism, and clinical skills, with a research dissertation running over the four-year course.
University director Christina Cunliffe said the new program was an exciting step in the development of chiropractic care for animals.
“Building on our decades of experience graduating confident, competent, and highly-skilled animal chiropractors, now is the time to open up this exciting career opportunity to college students.”
For the past 50 years, McTimoney College of Chiropractic has been training and educating human chiropractors to the highest regulatory standards. Over the past 20 years, animal chiropractic has developed to meet the requirements for this gentle, holistic treatment in the veterinary world.
Prospective students are invited to a Open House at McTimoney College of Chiropractic in Abingdon on February 16.
McTimoney Chiropractic for Animals identifies areas of stiffness, asymmetry, and poor range of motion within the skeletal system, particularly the spine and pelvis. This affects the muscles that surround these structures, as well as the nerve impulses that pass from the central nervous system to the periphery of the body. The adjustments are very light and fast, stimulating an instant response in the affected soft tissues and joints, promoting relaxation of muscle spasms, improving nerve function, and helping the skeletal structure regain better symmetry and movement again.
In many cases, animals suffer from underlying conditions such as arthritic changes or degenerative diseases that force them to compensate in their posture and movement in an attempt to remain comfortable. However, these offsets become increasingly entrenched and can be painful or uncomfortable, requiring chiropractic care to provide some relief. In other cases, the animals are working hard or competing and as such accumulate tension and asymmetries due to the demands of their work. Once again, chiropractic care helps relieve pain and promote performance, whether it’s faster speeds over hurdles for racehorses and events, better jumping style in showjumpers, or more extravagant movements for dressage stars.
Two recent graduates of the school’s Master of Animal Handling (Chiropractic) program did not hesitate to recommend the university. Natalie McQuiggan said that she had wanted to do McTimoney Chiropractic from a very young age, “but the process of doing it always seemed really daunting.
“But from the start, the staff and teachers were lovely and welcoming, and queries were answered promptly. I have really enjoyed my two years in the Master of Animal Handling (Chiropractic) program and would recommend anyone thinking of doing it to just do it.”
Pollyanna Fitzgerald said the university offered a supportive and welcoming learning environment, allowing her to grow and develop as a student and future professional. “There is always someone to talk to and offer encouragement when needed. As a student I have learned a lot and have been encouraged to believe in myself and it has been a wonderful place to learn.”
A free webinar, McTimoney’s Animal Chiropractic as a Careeron January 24 at 7:30 p.m. (GMT), is open to those who wish to learn more about the McTimoney technique and its application, and the training paths available to those interested in becoming a McTimoney Animal Chiropractor.
________________________
I think this announcement is puzzling on several levels:
- I was unable to find an ‘Abingdon-based University, Oxford’; could it be this institution that is a college and not a university?
- Christina Cunliffe seems to be (or has been?) affiliated with the McTimoney College of Chiropractic which is a bit odd, in my opinion.
- The college does not have ‘decades of experience’; it was founded only in 2001.
- Most importantly, I am unable to find a jot of good evidence that veterinary chiropractic is effective for any condition (see also here, here, and here). In case anyone is aware of any, please let me know. I’d be delighted to revise my judgment.
If I am right, the new course could be a fine example of quackademia where students are ripped off and taught to later rip off the owners of animals after the academically trained quacks have mistreated them.