risk
It is not only practitioners of so-called alternative medicine (SCAM) who can be fraudulent charlatans. The study of medicine does not protect you from joining in. Here is an impressive case in point:
It has been reported that a former doctor convicted of fraudulently submitting nearly $120 million in claims related to the 1-800-GET-THIN Lap-Band surgery business has been sentenced to seven years in federal prison.
Julian Omidi, 58, of West Hollywood was sentenced Monday by U.S. District Court Judge Dolly M. Gee. The judge also imposed a five-year probation period on Surgery Center Management LLC, an Omidi-controlled Beverly Hills-based company. In the coming weeks, Gee is expected to hold a separate hearing to decide on restitution and forfeiture in the case, along with setting a fine for the Beverly Hills company.
“Mr. Omidi made millions at the expense of the multiple victim companies he defrauded, and he violated his oath to ‘do no harm’ by callously misleading patients about the need for a sleep study and subsequent weight loss surgery,” said Donald Alway, the assistant director in charge of the FBI’s Los Angeles field office.
Omidi controlled several entities in the GET-THIN network. Prosecutors say Omidi incentivized employees to ensure patients underwent sleep studies and then falsified the results to show that patients had obstructive sleep apnea to help them qualify for insurance coverage for the weight loss surgery. Those results were then filed with insurance companies to pre-approve the Lap-Band weight-loss surgeries. The 1-800-GET-THIN business received approximately $41 million for those procedures, according to prosecutors. While not all patients were approved to receive the surgery, prosecutors say GET-THIN would bill the patient roughly $15,000 for each sleep study, totaling $27 million in payments from insurance providers.
Omidi and his Beverly Hills-based company, Surgery Center Management, were found guilty of 28 counts of wire fraud, three counts of mail fraud, and one count of conspiracy to commit money laundering. Omidi was also found guilty of two counts of making false statements relating to healthcare matters, one count of aggravated identity theft, and two counts of money laundering after a 48-day trial in downtown Los Angeles.
“As found by the jury, the defendant Julian Omidi deliberately and repeatedly acted with an eye towards business and profits, rather than in the interest of GET-THIN’s medical patients, by inducing patients to undergo medical treatment premised on fraud rather than medical necessity, including surgeries that carry significant risks and life-long health impacts,” said U.S. Atty. Martin Estrada. A series of Los Angeles Times columns from 2010 to 2014 detailed how five patients died after they received Lap-Band surgeries at clinics affiliated with 1-800-GET-THIN. During a 2009 inspection, the Department of Health and Human Services found unsanitary conditions, inoperative scrub sinks, one-time-only equipment being reused, and several other deficiencies. The inspector shut down the clinic for a day, but further action was not taken at the time.
Omidi’s medical license was revoked in 2009, and he was arrested. In 2014, federal agencies seized more than $110 million from the 1-800-GET-THIN network in securities and funds.
______________________________
This is a spectacular case, of course. Yet, I fail to see how it differs in principle from the many instances we see on a daily basis in the realm of SCAM. Let me give you just a few examples:
- A chiropractor diagnoses subluxation and subsequently treats his patient with a series of spinal manipulations.
- A naturopath uses iridology to diagnose a weakness of the liver and subsequently treats it with herbal remedies.
- An acupuncturist diagnoses a blockage of chi and follows it up with a series of acupuncture sessions.
- A Heilpraktiker employs bioresonance to diagnose an intoxication which he then treats with a detox program.
The strategy is always the same:
- Charlatans use bogus diagnostic methods.
- They make bogus diagnoses with them.
- They then start expensive and often dangerous treatments.
- They make good money by defrauding the system.
Could someone please explain what the difference in principle is between the case of the fraudulent surgeon and the average SCAM practitioner?
The Charité in Berlin is a medical school with considerable tradition and reputation. It, therefore, seems a little baffling that this institution agreed to the creation of a professorship in anthroposophical medicine, a branch of so-called alternative medicine (SCAM) that is not only highly implausible but also not supported by sound clinical evidence of doing more good than harm.
The TAZ (a well-known and usually reliable German news outlet) has looked into this issue and just published a report of which I translated the main passages (the additions in brackets were added by me):
In December 2010, after a discussion, the Software AG (an anthroposophical Foundation) offered to finance an anthroposophical professorship at the Charité, according to documents available to the taz. The foundation writes on its website that it wants to use its money to advance the “academization of anthroposophic medicine.” A professorship at a famous institution like the Charité seems like a major prize. The Charité is offered the prospect of 250,000 euros per year.
Investing this money is apparently so important to the Foundation that it spends five years courting the Charité for the professorship. When things don’t go fast enough for them, the project manager writes sharp emails to the Charité administration in December 2016: they are “quite irritated and correspondingly annoyed.” They would be happy “if this never-ending story can finally find a positive conclusion.”
The Foundation apparently has already had an idea of who could take up this professorship early on – although professorships are not actually allowed to be advertised “ad personam,” i.e., tailored to a person. In May 2012, it proposes to include the anthroposophical Havelhöhe Hospital in Berlin (we reported about this place before). It would make a clinical area available for this purpose. There had apparently already been an exchange of views on this.
The contract for the “establishment of a temporary W2 endowed professorship for five years” is dated April 15, 2015. It also states that Charité must indicate that the professorship is funded by the Software AG Foundation. Which it then fails to do.
At this point, the professorship has already been publicly advertised. Very specific requirements are formulated in the advertisement: Among other things, expertise in gastroenterology and oncology is desired, as well as research interest in chronic inflammatory bowel diseases. These happen to be the specializations that the medical director of Havelhöhe Hospital has to show: Harald Matthes (we have met him before on this blog).
Matthes lands as “primo et unico loco” on the appointment list, i.e. as the first-ranked and only candidate. Whether anyone else has applied for the professorship at all, the Charité does not want to answer. Normally, there are three people on an appointment list, unless the requirements for the professorship are too niche. When the Faculty Council votes on filling the professorship, it has to take two ballots because the necessary majority is not reached in the first vote. In March 2017, Matthes is finally appointed professor at the Charité. For proponents of anthroposophic medicine, this has historic significance: “It is tantamount to a knighthood for anthroposophic medicine,” says a chronology of the umbrella organization.
Before his appointment, Harald Matthes negotiated a special request: He wants to remain chief physician in Havelhöhe, which is why he formally took a five-year leave of absence on the first day of his professorial career at Charité. This concept is called the “Jülich Model”. Harald Matthes is not the first to exercise his professorship in this way. It is unusual, however, to cooperate with a private hospital; normally, cooperation is arranged with other research institutions.
Matthes’ employer, Havelhöhe Hospital, also benefits financially from the deal. The Charité transfers a large part of the foundation’s money to Havelhöhe – the documents mention an amount equivalent to a W2 salary. In a letter, the dean of the Charité at the time, Axel Radlach Pries, called Matthes’ wishes “unusual and going beyond previous models of endowed professorships at the Charité.”
Also unusual is that Harald Matthes does not teach any courses at Charité, according to the internal course catalog, even though the contract available to taz specifies nine semester hours of teaching per week. In the Jülich model, two hours of teaching per week are the rule.
So Harald Matthes is the big winner in this: He gets a professorial title without many obligations, while at the same time, money flows to his hospital.
But what does the Charité get out of it? The contract for the establishment of the professorship states that new aspects will thus flow into research, teaching, and patient care. Matthes himself says he is convinced that he is contributing to the scientific progress of the institution. Before his professorship expires after five years, he will ask for an extension in August 2021. “I would like to point out that my work and results in research, teaching, and clinical care have led to international recognition and contributed to the reputation of Charité,” he writes. At the time, he is working on the so-called ImpfSurv study, for which people are asked about possible side effects from the Corona vaccine using an online questionnaire. He gets a lot of media attention for it.
In April 2022, for example, Matthes appears on MDR television, his name superimposed under “Charité Berlin.” He presents the interim results of his study: the serious side effects are much more frequent than the Paul Ehrlich Institute, which is responsible for vaccines, would indicate. Only: This cannot be said at all.
The study has methodological flaws, the Charité distances itself from the statements of its professor. People had participated twice in the survey, and it was not scientific to conclude that there was a connection between symptoms and vaccination without the assessment of a doctor. The study is discontinued.
Before that, when the study was still running, the evaluation commission met several times to discuss the extension of the endowed professorship. In doing so, it “thoroughly reviewed all of Prof. Matthes’ achievements.” What exactly the commission recorded is not known. The document released to the taz is extensively redacted.
What is certain is this: In February 2022, the commission votes for the extension for another five years. Anthroposophy may keep its professorship at the Berlin Charité until at least 2027. The anthroposophical foundation now transfers 293,000 euros per year for this.
_______________________________
Social media platforms are frequently used by the general public to access health information, including information relating to complementary and alternative medicine (CAM). The aim of this study was to measure how often naturopathic influencers make evidence-informed recommendations on Instagram, and to examine associations between the level of evidence available or presented, and user engagement.
A retrospective observational study using quantitative content analysis on health-related claims made by naturopathic influencers with 30 000 or more followers on Instagram was conducted. Linear regression was used to measure the association between health-related posts and the number of Likes, and Comments.
A total of 494 health claims were extracted from eight Instagram accounts, of which 242 (49.0%) were supported by evidence and 34 (6.9%) included a link to evidence supporting the claim. Three naturopathic influencers did not provide any evidence to support the health claims they made on Instagram. Posts with links to evidence had fewer Likes (B=-1343.9, 95% CI=-2424.4 to -263.4, X=-0.1, P=0.02) and fewer Comments (B=-82.0, 95% CI=-145.9 to -18.2, X=-0.2, P=0.01), compared to posts without links to evidence. The most common areas of health were claims relating to ‘women’s health’ (n=94; 19.0%), and ‘hair, nail, and skin’ (n=74; 15.0%).
The authors concluded that this study is one of the first to look at the evidence available to support health-related claims by naturopathic influencers on Instagram. Our findings indicate that around half of Instagram posts from popular naturopathic influencers with health claims are supported by high-quality evidence.
At first sight, these findings amazed me; I would have thought that the percentage of supported claims was lower. As it turned out, I was not far off: in the paper, the authors differentiate the results into more categories and state that ” of those with evidence clearly available, approximately 10% of health claims were underpinned by high-quality evidence such as systematic reviews of randomised controlled trials.”
Even though interesting, the study has significant limitations. The authors are well aware of them and explain:
A key limitation was relying on the 10 most relevant retrieved articles in PubMed, rather than conducting an extensive search for evidence, when not provided alongside the claim. It is possible we did not identify existing evidence to support some of the claims; however, it would not have been feasible to construct a comprehensive search strategy and screen articles for every health claim made. Our search strategy served as a proxy measure for the evidence to support the claim and it is unlikely that the 10 most relevant articles on PubMed would systematically fail to identify existing supporting evidence.
The risk of subjectivity in the extraction of interventional health claims from Instagram posts and conversion into a PICO is another limitation. The subjectivity of data extraction was minimised using standards which included extracting specific terms used by the naturopathic influencer to perform database searches on PubMed. If not explicitly stated, the intended target audience of the health claims were made using educated guesses based on the intervention and outcome promoted in the claim. For the claim to be considered supported by evidence, study participants must match the intended audience of the health claim on Instagram(e.g., postmenopausal women, athletes). When the study with the highest level of evidence were inconclusive due to reasons such as inadequate cohort size, conflicting results for different cohort (e.g., male vs. females), heterogeneity between studies and poor quality of studies, it was concluded that the evidence did not support the health claim. When there was considerable uncertainty related to the health intervention or outcome, it was excluded from the study.
So, in the end, I guess, it boils down to whether you are an optimist or a pessimist:
About half of the claims made by prominent naturopaths are supported by at least a bit of evidence.
About half of the claims made by prominent naturopaths are not supported by evidence.
I came across an article entitled “Consent for Paediatric Chiropractic Treatment (Ages 0-16)“. Naturally, it interested me. Here is the full paper; I have only inserted a few numbers in square brackets which refer to my comments below:
By law, all Chiropractors are required to inform you of the risks and benefits of chiropractic spinal manipulation and the other types of care we provide. Chiropractors use manual therapy alongside taking a thorough history, and doing a neurological, orthopaedic and chiropractic examination to both diagnose and to treat spinal, cranial and extremity dysfunction. This may include taking joints to the end range of function, palpating soft tissues (including inside the mouth and the abdomen), mobilisation, soft tissue therapy and very gentle manipulation [1]. Our Chiropractors have been educated to perform highly specific types of bony or soft tissue manipulation and we strive to follow a system of evidence-based care [2]. At the core of our belief system is “Do No Harm”. We recognise that infants and children are not tiny adults. The force of an adjustment used in a child is at least less than half of what we might use with a fully grown adult. Studies by Hawk et al (2016) and Marchand (2013) agreed that Chiropractors use 15 – 35 x less force in the under 3-month age group when compared to medical practitioners doing manipulation (Koch, 2002) [3]. We also use less force in all other paediatrics groups, especially when compared to adults (Marchand, 2013). In addition to using lower force, depth, amplitude and speed in our chiropractic adjustments [4], we utilise different techniques. We expect all children under the age of 16 years to be accompanied by a responsible adult during appointments unless prior permission to treat without a consenting adult e.g., over the age of 14 has been discussed with the treating chiropractor.
Risks
- Research into chiropractic care for children in the past 70 years has shown it to have a low risk of adverse effects (Miller, 2019) [5]. These effects tend to be mild and of short duration e.g., muscular or ligament irritation. Vorhra et al (2007) found the risk of severe of adverse effects (e.g. fracture, quadriplegia, paraplegia, and death) is very, very rare and was more likely to occur in individuals where there is already serious underlying pathology and missed diagnosis by other medical profession [6]. These particular cases occurred more than 25 years ago and is practically unheard of now since research and evidence-based care has become the norm [7].
- The most common side effect in infants following chiropractic treatment includes fussiness or irritability for the first 24 hours, and sleeping longer than usual or more soundly. (Miller and Benfield, 2008) [8]
- In older children, especially if presenting with pain e.g., in the neck or lower back, the greatest risk is that this pain may increase during examination due to increasing the length of involved muscles or ligaments [9]. Similarly, the child may also experience pain, stiffness or irritability after treatment (Miller & Benfield, 2008) [10]. Occasionally children may experience a headache.[11] We find that children experience side effects much less often than adults.[12]
Benefits
- Your child might get better with chiropractic care. [13] If they don’t, we will refer you on [14].
- Low risk of side effects and very rare risk of serious adverse effects [15].
- Drug-free health care. We are not against medication, but we do not prescribe [16].
- Compared with a medical practitioner, manual therapy carried out by a chiropractor is 20 x less likely to result in injury (Koch et al 2002, Miller 2009).[17]
- Children do not often require long courses of treatment (>3 weeks) unless complicating factors are present.[18]
- Studies have shown that parents have a high satisfaction rate with Chiropractic care [19].
- Physical therapies are much less likely to interfere with biomedical treatments. (McCann & Newell 2006) [20]
- You will have a better understanding of diagnosis of any complain and we will let you know what you can do to help.[21]
We invite you to have open discussions and communication with your treating chiropractor at all times. Should you need any further clarification please just ask.
References
- Hawk, C. Shneider, M.J., Vallone, S and Hewitt, E.G. (2016) – Best practises recommendations for chiropractic care of children: A consensus update. JMPT, 39 (3), 158-168.
- Marchand, A. (2013) – A Proposed model with possible implications for safety and technique adaptations for chiropractic spinal manipulative therapy for infants and children. JMPT, 5, 1-14
- Koch L. E., Koch, H, Graumann-Brunnt, S. Stolle, D. Ramirez, J.M., & Saternus, K.S. (2002) – Heart rate changes in response to mild mechanical irritation of the high cervical cord region in infants. Forensic Science International, 128, 168-176
- Miller J (2019) – Evidence-Based Chiropractic Care for Infants: Rational, Therapies and Outcomes. Chapter 11: Safety of Chiropractic care for Infants p111. Praeclarus Press
- Vohra, S. Johnston, B.C. Cramer, K, Humphreys, K. (2007) – Adverse events associated with paediatric spinal manipulation: A Systematic Review. Pediatrics, 119 (1) e275-283
- Miller, J and Benfield (2008) – Adverse effects of spinal manipulative therapy in children younger than 3 years: a retrospective study in a chiropractic teaching clinic. JMPT Jul-Aug;31(6):419-23.
- McCann, L.J. & Newell, S.J. (2006). Survey of paediatric complementary and alternative medicine in health and chronic disease. Archives of Diseases of Childhood, 91, 173-174
- Corso, M., Cancelliere, C. , Mior., Taylor-Vaise, A. Côté, P. (2020) – The safety of spinal manipulative therapy in children under 10 years: a rapid review. Chiropractic Manual therapy 25: 12
___________________________________
- “taking joints to the end range of function” (range of motion, more likely) is arguably not “very gently”;
- “we strive to follow a system of evidence-based care”; I do not think that this is possible because pediatric chiropractic care is hardy evidence-based;
- as a generalizable statement, this seems to be not true;
- ” lower force, depth, amplitude and speed”; I am not sure that there is good evidence for that;
- research has foremost shown that there might be significant under-reporting;
- to blame the medical profession for diagnoses missed by chiropractors seems odd;
- possibly because of under-reporting;
- possibly because of under-reporting;
- possibly because of under-reporting;
- possibly because of under-reporting;
- possibly because of under-reporting;
- your impressions are not evidence;
- your child might get even better without chiropractic care;
- referral rates of chiropractors tend to be low;
- possibly because of under-reporting;
- chiropractors have no prescription rights but some lobby hard for it;
- irrelevant if we consider the intervention useless and thus obsolete;
- any evidence for this statement?;
- satisfaction rates are no substitute for real evidence;
- that does not mean they are effective, safe, or value for money;
- this is perhaps the strangest statement of them all – do chiropractors think they are the optimal diagnosticians for all complaints?
_____________________________________
According to its title, the paper was supposed to deal with consent for chiropractic pediatric care. It almost totally avoided the subject and certainly did not list the information chiropractors must give to parents before commencing treatment.
Considering the arguments that the article did provide has brought me to the conclusion that chiropractors who treat children are out of touch with reality and seem in danger of committing child abuse.
The claim that homeopathy has a role in oncology does not seem to go away. Some enthusiasts say it can be used as a causal therapy, while others insist it might be a helpful symptomatic adjuvant. Almost all oncologists agree that homeopathy has no place at all in cancer care.
Who is right?
This systematic review included clinical studies from 1800 until 2020 to evaluate evidence of the effectiveness of homeopathy on physical and mental conditions in patients during oncological treatment.
In February 2021 a systematic search was conducted searching five electronic databases (Embase, Cochrane, PsychInfo, CINAHL and Medline) to find studies concerning use, effectiveness, and potential harm of homeopathy in cancer patients.
From all 1352 search results, 18 studies with 2016 patients were included in this SR. The patients treated with homeopathy were mainly diagnosed with breast cancer. The therapy concepts included single and combination homeopathic remedies (used systemically or as mouth rinses) of various dilutions. The outcomes assessed were:
- the influence on toxicity of cancer treatment (mostly hot flashes and menopausal symptoms),
- the time to drain removal in breast cancer patients after mastectomy,
- survival,
- quality of life,
- global health,
- subjective well-being,
- anxiety and depression,
- safety and tolerance.
The included studies reported heterogeneous results: some studies described significant differences in quality of life or toxicity of cancer treatment favoring homeopathy, whereas others did not find an effect or reported significant differences to the disadvantage of homeopathy or side effects caused by homeopathy. The majority of the studies had low methodological quality.
The authors concluded that, the results for the effectiveness of homeopathy in cancer patients are heterogeneous, mostly not significant and fail to show an advantage of homeopathy over other active or passive comparison groups. No evidence can be provided that homeopathy exceeds the placebo effect. Furthermore, the majority of the included studies shows numerous and severe methodological weaknesses leading to a high level of bias and are consequently hardly reliable. Therefore, based on the findings of this SR, no evidence for positive effectiveness of homeopathy can be verified.
This could not be clearer. Some might argue that, of course, homeopathy cannot change the natural history of cancer, but it might improve the quality of life of those patients who believe in it via a placebo response. I would still oppose this notion: there are many effective treatments in the supportive treatment of cancer, and it seems much better to use those options and tell patients the truth about homeopathy.
Austrian doctors recently received a notice in their mailbox about a postgraduate training event that is remarkable, to say the least.
The Vienna Medical Association is organizing a postgraduate training course on “Complementary Medical Homeopathy for Post- and Long Covid“. The date for the event is 20.4.2023. Registration for it is via the Association’s “Department of Complementary and Integrative Medicine”.
In case you ask, what is wrong with such a course? There is no scientific evidence that homeopathy has a specific, positive effect in long/post covid. Therefore the announced event has about the same validity as a lecture series for:
- BUNGEE JUMPING FOR DIABETES
or
- DOUGHNUT EATING FOR CORONARY HEART DISEASE
or
- CIGARETTE SMOKING IN CANCER PREVENTION
While relevant pseudomedicine training courses have in the past been organized by the relevant Austrian SCAM-organizations, the Vienna Medical Association itself is now joining the ranks of the organizers of pseudomedicine training courses. Whereas pseudomedicine has so far been the domain of physicians in private practice in Austria, it now appears to be promoted by the Vienna Medical Association in hospitals as well.
The Vienna Medical Association boldly claims that MEDICAL ETHICS IS THE BASIS OF OUR WORK. Well guess what, guys: teaching nonsense is not very ethical!
The ‘tasks and goals’ of the Association’s ‘Department for Complementary and Integrative Medicine’ of the Vienna Medical Association are explained on their website:
The aim of our department is to represent doctors with additional diplomas in the medical association and to inform about the value of their special therapeutic approaches better than previously – particularly in cases of serious side effects of conventional therapies.
In the sense of conveying up-to-date, high-quality, medical, and complementary education and training in complementary medicine, our department aims to publish relevant articles and announcements of dates of the respective professional societies in the chamber’s own media.
Practice-oriented introductory lectures or study groups on the following topics are also planned topics:
- medical homeopathy,
- psychosomatic relaxation therapy (bipolar harmonising abdominal breathing, autogenic training),
- acupuncture,
- regulation therapy based on skin resistance measurements at acupuncture points,
- TCM,
- herbal therapy, etc.
“Up-to-date, high-quality, medical, and complementary education and training in complementary medicine” – oh really? If the Association’s “Department of Complementary and Integrative Medicine” is truly interested in this, I herewith offer to give a free lecture series for them that would teach them the high-quality evidence truly shows.
Meanwhile, as there is no good evidence that homeopathy is an effective therapy for post/long Covid, the question of whether the ‘Vienna Medical Association’ has taken leave of its senses, must be answered in the affirmative.
I have often blogged about informed consent. Recently, I have come across a quote about informed consent to medical research that I find remarkable in several ways. It was made by a German physician and I present you with the original and with my translation of it.
The person who correctly guesses the author of the quote will – if he/she wants – receive a free copy of one of my books delivered through the post.
Here we go:
THE ORIGINAL
Zum einen gibt es Versuche, die fuer order mit jemandem auf freiwilliger Basis durchgefuehrt werden; zum anderen solche, die gegen den Willen der betroffenen Person stattfinden. Eine weitere Unterteilung gibt an, of sie besonders gefaehrlich offer vergleichsweise unbedenklich und ohne Gefahrenpotenzial sind. Zu unterscheiden ist ausserdem, ob das Ergebnis des Versuchs wichtig ist oder ob es sich nur um eine laecherliches Spiel einer wissenschaftlich gebildeten Person handelt. Aus diesen sechs Kriterien ergibt sich eine Art Richtlinie, die es einem vom medizinischen Standpunkt aus ermoeglicht JA oder NEIN zu sagen.
MY TRANSLATION
On the one hand, there are experiments that are carried out for or with someone on a voluntary basis; on the other hand, there are those that take place against the will of the person concerned. A further subdivision indicates whether they are particularly dangerous or comparatively harmless and without any potential for danger. A further distinction must be made as to whether the result of the experiment is important or whether it is merely a ridiculous game played by a scientifically educated person. These six criteria form a kind of guideline that enables one to say YES or NO from a medical point of view.
____________________________
I don’t think you will find the author by googling the text. So, don’t bother.
The author, a German physician, is no longer alive but was very famous at one time. I will disclose his – yes it was a man – identity as soon as someone got the correct answer. If nobody does guess correctly, I will disclose it in a few days.
If you are unable to guess the author, I would still be interested in what you think of the quote and the frame of mind of the physician who said these intriguing sentences.
A German newspaper reported the experience of two journalists who went undercover to consult several practitioners of so-called alternative medicine to receive treatment for Hodgkin lymphoma. Here are several passages from their important article (my translation, my bolding)
… Doctor Uwe Reuter invites us in. He is sitting behind an iMac on which he sometimes shows me pictures of his therapies. He is around 50, tall and lean, his face looks particularly serious through frameless glasses. I tell him my story. He listens attentively, and then it seems for a while as if he can’t decide what to advise me. Finally, he has it: I should first do a “diagnostic series” in his clinic, three or even better five days, for about 1000 Euros. This would include “electromagnetic measurements” for the “energy balance of individual organs”. Only then can he determine which therapy might be indicated in my case. “Hypnosis, homeopathy, vitamin B17 infusions” will probably play a role, says Reuter, and a “fever therapy” in which I will be injected with dead bacteria.
“In addition to chemotherapy or alone?”, I ask. The doctor says he can’t make this decision for me, I should make it from my “inside”. I have to understand that my illness does not come from the outside and that therapies only have a supporting effect – the healing “has to come from within”.
… In the end, Reuter suggests postponing chemotherapy for a quarter of a year and using his therapy to “push aside everything that prevents healing” – toxins, distractions, and fears. The cost? Around 10,000 Euros for the entire therapy…
[Next doctor is] the well-known alternative doctor Klaus Maar in Düsseldorf… His wrinkled face is dominated by a large nose, his hair is enviably thick and black for a man of his age. “Well,” he says in his comforting voice, “why don’t you describe what happened to you?” I am nervous. Will he believe that I am terminally ill? I stammer and tell my story. He listens to me, looks at me, answers calmly, and takes his time – and attention that few orthodox doctors can afford today, which is one of the reasons that drive people into the arms of alternative healers.Finally, Maar advises a “heat therapy” in which the tumor is heated locally. Yet Klaus Maar is still one of the more serious healers. He does not directly advise against chemotherapy, but warns about the side effects. In the end, he recommends postponing it for a fortnight and starting the 8,000-euro heat treatment as soon as possible. “But don’t delay, don’t blame me and say I delayed the chemotherapy,” Maar says. I guess that’s his way of hedging his bets: If he were to successfully dissuade me from chemotherapy, my family could sue him one day. I come across such phrases again and again.
… next visit; the alternative practitioner Ursula Stoll specializes in “Germanic New Medicine”. Ryke Geerd Hamer, a former doctor, founded this doctrine in the early 1980s as a reaction to “Jewish” orthodox medicine. No wonder it enjoys great popularity in völkisch circles. Hamer’s abstruse and dangerous theories led to the withdrawal of his license. He continued to practice illegally, however, and several of his patients died… Even Ursula Stoll thinks he was crazy – but not his theory… Stoll practices in Öhringen, an idyllic little town north of Stuttgart, in her nondescript detached house. She wears a white shirt and horn-rimmed glasses, her brown hair pinned back in a plait, an accurate governess with a stern look.
As I tell her about my suffering, she quickly interrupts me: “What is cancer?” she asks. We have to get rid of the term. There is no such thing as cancer. All I have is a swelling of the lymph nodes in my neck. That’s all. The cause: a self-deprecation of a professional nature. In my case, there is also an existential fear, and like a fish on land, I store water in my body in order to survive. Hence the swollen lymph nodes. Metastases? There are none. The medical report? She skims over it casually and asks: Did you sweat when you were sick? Did the sweat smell? Did it have a color? Where exactly was the itch?
I tell her about the lecture I gave and that my boss didn’t like. Yes! That could be the reason for the cancer. She says my symptoms are a reaction to this slight, my body is trying to heal itself, but the first chemotherapy interrupted and disrupted the process. Her advice to beat the cancer: I should move back in with my parents, life as a single person is too much for me, Berlin is a terrible city anyway… I ask again about chemotherapy. “I personally wouldn’t do it,” she says, “and for my children and my parents I would decide the same.” There it is again, this nappy-soft formulation with which the healers evade their legal responsibility. One more question: isn’t it dangerous to forego chemotherapy? The alternative practitioner Ursula Stoll: “Humans can withstand a lot.”
… Since the spiritual healers Wolfgang Bittscheidt and Teresa Schuhl were favorably discussed on German TV, their practice in Siegburg near Bonn has enjoyed great popularity: appointments are made only months in advance. When we are asked into the treatment room, it is dark, the blinds are half closed. A candle burns on the dark wooden desk. Teresa Schuhl is blond, has blue eyes, and seems cool and aloof, gesticulating strangely with her hands. She whispers more than she speaks; I have to lean forward to understand her. Her advice? “If you were my son right now, I would say, hands off chemo!” For herself, she would decide the same. “One possibility is vitamin B17. Have you heard of it?”
I have heard of it. The so-called vitamin B17 is in fact not a vitamin at all, but a toxic substance, related to prussic acid. It is currently experiencing a boom in the alternative scene and has no proven benefit for cancer. Several people have died from overdoses.
Schuhl is now poking around in my spiritual life and in the relationship between me and my parents. She also suspects a trauma behind my cancer. “The thyroid represents the hormonal. The balance between male and female. Do you know where you belong? Male or female?” What is she trying to say?
“I come from Tajikistan,” he says, “where they say: sickness is a sacred time. When you are sick, God talks to you. He tells you what life really is. What we live is not life, it’s shit. Sickness asks us to make a change.” He continues, “Death is the most beautiful thing there is. Like a trip to the Caribbean. Why are we afraid of it? On this tortured planet here?”
After this introduction, my head is spinning, but now the actual treatment begins. I lie down on a couch. Schuhl runs her hands over my stomach and holds my shoulder. At the same time, she says prayers. She changes into the extinct Aramaic that is sometimes used in Christian services. Then she leaves me alone. Later, her partner, a licensed doctor, recommends that I read up on vitamin B17, come to them once a month and light a candle in a church in Cologne. I walk out of the practice befuddled…
The practitioners protect themselves legally. They make the patients sign contracts stating that the patient has been informed about orthodox medicine and that they reject it willy-nilly, even though the information is often not worth mentioning. What would be the solution?
… The doctor Achim Schuppert in Bonn suspects mobile phone radiation as the cause of my tumor and wants to measure my magnetic aura. It was important to him to “exclude electrosmog as a possible damaging factor”, he writes later.
Lothar Hollerbach, who runs an alternative practice in a Heidelberg city villa, gives a philosophical lecture: “We are spiritual beings and only for a short time in a mobile home we call a body.” Every crisis is a lesson, he says, but perhaps that lesson is for the next life. One of the things he recommends to me for recovery is Rudolf Steiner‘s lectures. How many patients has he successfully treated? He doesn’t count them, Hollerbach waves off. And after all, it’s not just about surviving. Some of his patients could have led a totally different life “in the next incarnation”. For those who long for death – his practice is highly recommended…
… The “medical director” Elke Tegel, a blonde alternative practitioner, leads me through the bright house, shows me the “inner world travel room” where traumatic situations are processed, the room for “healing music“, and also the impressive machine for “high-frequency therapy“, in which electrical energy is supplied to the cells. Costs: 13670 Euros for five weeks.
Cancer, says the alternative practitioner, is “suppressed anger and suppressed resentment”; Hodgkin’s lymphoma in particular is about guilt. She asks: “Where do you feel guilty? Guilty of being a man?” Later she advises a “biological chemotherapy” of highly concentrated vitamin C. This, she says, is far superior to conventional chemo. She confuses my well-treatable Hodgkin’s lymphoma with the fundamentally different non-Hodgkin’s lymphoma. And justifies herself: “With us, it’s not about diagnosis, that’s not of interest.” …
________________________
What I like about this report is that they exposed both doctors and non-medically trained practitioners, i.e. Heilpraktiker. We see yet again that the study of medicine does not protect people from becoming dangerous charlatans. Yet, there are important differences between doctors and Heilpraktiker:
- Only a very small proportion of doctors would treat Hodgkin lymphoma with ineffective quackery, whereas the proportion with Heilpraktiker would, I guess, be not far from 100%.
- Doctors will get struck off for such behavior, whereas this happens to Heilpraktiker as good as never.
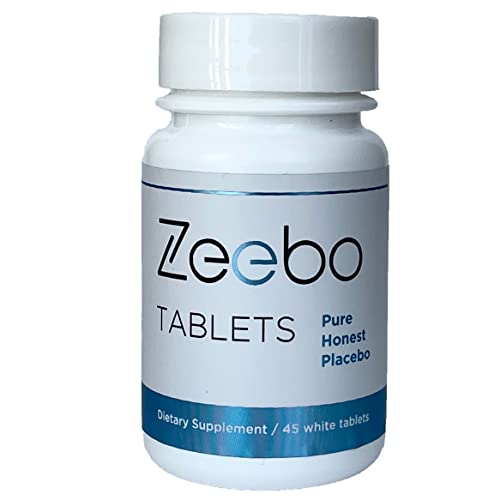
At first, I thought this was an ‘April fools’ joke. Then I looked at it a bit closer and realized that it seemed for real: Amazon is selling a placebo tablet. Here is how it is advertised:
- Honest Placebo Tablets by Zeebo Effect, inert ingredients, halal & kosher
- Focus on symptom relief, concentration, clarity, energy, calm, sleep
- Ze logo on each tablet, the original honest placebo brand trusted since 2014
- Randomized Controlled Trials with Zeebo Published in Journal for Pain, Nature, American Family Physician
- Each bottle is sealed with a transparent, tamper-proof neckband
Zeebo Tablets – Honest placebo tablets (white, round, 250mg each) are designed to help you create a safe placebo experience. Zeebo comes with the Ze logo on each tablet. Zeebo is made from an inert, natural fiber. Vegan, free of sugar or dyes. When it comes to Zeebo, You are the active ingredient. Users of Zeebo Tablets know they are taking a placebo containing only inert ingredients. Zeebo Tablets are taken intentionally obtain stress and pain relief, to release tension, irritability and nervousness, to help with calm and sleep serving as a sleep aid. Some of our customers take Zeebo Tablets to solicit placebo effects for increased mental focus, clarity, concentration, test performance and to sustain higher energy levels during physical exercise. Zeebo tablets are pure placebo, they are non-drowsy, non-homeopathic. There are no known interactions between Zeebo Placebo Tablets and other medications or supplements. Do not use Zeebo to delay or replace medical treatment. Visit zeeboeffect.com to learn about Zeebo. Look for the ebook The Placebo Cure to find out more about how to create your own Honest Placebo experience.
Take as needed. You may or may not respond to placebo. Do not use Zeebo to replace or delay medical treatment. Use Zeebo without deceit.*
* These statements have not been evaluated by the FDA. This product is not intended to diagnose, cure, treat, or prevent any disease.
Statements regarding dietary supplements have not been evaluated by the FDA and are not intended to diagnose, treat, cure, or prevent any disease or health condition.
Zeebo Tablets are an ethical placebo. People take it knowing it is a placebo. Take it without self-deceit. Zeebo is not made to look like any other ingestible. In fact, we think that the Zeebo branding can help enhance the experience. Have a look into ethical placebo or honest placebo studies. You will find a lot of research there, published in the journals Nature, Pain, for example. No need to trick yourself.
_________________________
After reading all this, I am again not entirely sure whether this is a hoax. If it is, I failed to get the fun of it. If it isn’t, there might be reasons for concern. When a placebo was marketed, a few years ago, THE GUARDIAN published opinions about the idea:
Jennifer Buettner, whose company Efficacy is marketing the placebo, says it can stimulate “the body’s ability to repair itself and the miracle power of the brain”. She said the company planned to distribute the pills, which cost £3 for 50, in the UK. “When drugs are not needed and the patient still thinks that medicine would help, we believe that the placebo effect can work,” she said.
But Dr Clare Gerada, vice-chair of the Royal College of GPs, described the pill as “medicalising love”, adding: “This placebo disempowers parents. It is telling them that unless you give your children this pill there’s nothing else.” Douglas Kamerow, associate editor of the British Medical Journal, said giving placebos to children was a “deeply bad idea”. Writing in the latest edition of the journal, he said: “The problems are numerous. Firstly, whom are we treating here, children or their parents?” He added that if parents used placebos to comfort their children they were teaching them that tablets are the answer for all life’s aches and pains.
As we have seen previously, the evidence on ‘open placebos’ is less impressive than many think. It makes me wonder whether the sale of placebo tablets is a good idea.
WHAT DO YOU THINK?
During the coronavirus disease 2019 pandemic, Ayurvedic herbal supplements and homeopathic remedies were promoted as immune boosters (IBs) and disease-preventive agents. This happened in most parts of the world but nowhere more intensely than in India.
The present study examined the clinical outcomes among patients with chronic liver disease who presented with complications of portal hypertension or liver dysfunction temporally associated with the use of IBs in the absence of other competing causes. This Indian single-center retrospective observational cohort study included patients with chronic liver disease admitted for the evaluation and management of jaundice, ascites, or hepatic encephalopathy temporally associated with the consumption of IBs and followed up for 180 days. Chemical analysis was performed on the retrieved IBs.
From April 2020 to May 2021, 1022 patients with cirrhosis were screened, and 178 (19.8%) were found to have consumed complementary and alternative medicines. Nineteen patients with cirrhosis (10.7%), jaundice, ascites, hepatic encephalopathy, or their combination related to IBs use were included. The patients were predominantly male (89.5%). At admission, 14 (73.75%) patients had jaundice, 9 (47.4%) had ascites, 2 (10.5%) presented with acute kidney injury, and 1 (5.3%) had overt encephalopathy. Eight patients (42.1%) died at the end of the follow-up period. Hepatic necrosis and portal-based neutrophilic inflammation were the predominant features of liver biopsies.
Ten samples of IBs, including locally made ashwagandha powder, giloy juice, Indian gooseberry extracts, pure giloy tablets, multiherbal immune-boosting powder, other multiherbal tablets, and the homeopathic remedy, Arsenicum album 30C, were retrieved from our study patients. Samples were analyzed for potential hepatotoxic prescription drugs, known hepatotoxic adulterants, pesticides, and insecticides, which were not present in any of the samples. Detectable levels of arsenic (40%), lead (60%), and mercury (60%) were found in the samples analyzed. A host of other plant-derived compounds, industrial solvents, chemicals, and anticoagulants was identified using GC–MS/MS. These include glycosides, terpenoids, phytosteroids, and sterols, such as sitosterol, lupeol, trilinolein, hydroxy menthol, methoxyphenol, butyl alcohol, and coumaran derivatives.
The authors concluded that Ayurvedic and Homeopathic supplements sold as IBs potentially cause the worsening of preexisting liver disease. Responsible dissemination of scientifically validated, evidence-based medical health information from regulatory bodies and media may help ameliorate this modifiable liver health burden.
The authors comment that Ayurvedic herbal supplements and homeopathic remedies sold as IBs, potentially induce idiosyncratic liver injury in patients with preexisting liver disease. Using such untested advertised products can lead to the worsening of CLD in the form of liver failure or portal hypertension events, which are associated with a high risk of mortality compared to those with severe AH-related liver decompensation in the absence of timely liver transplantation. Severe mixed portal inflammation and varying levels of hepatic necrosis are common findings on liver histopathology in IB-related liver injury. Health regulatory authorities and print and visual media must ensure the dissemination of responsible and factual scientific evidence-based information on herbal and homeopathic “immune boosters” and health supplements to the public, specifically to the at-risk patient population.