quackery
This systematic review and meta-analysis aimed to evaluate the effectiveness and safety of Chinese herbal medicine (CHM) combined with Western medicine (WM) in comparison with WM in reducing systolic and diastolic blood pressure for patients with primary hypertension (PHTN).
Various literature searches located a total of 29 studies that included 2623 patients. The results showed that the clinical effectiveness in the treatment of hypertension with CHM+WM was considerably higher than that with WM alone, clinical effective (RR 1.23, 95% CI [1.17, 1.30], P < 0.00001), and markedly effective (ME) in the patients (RR 1.66, 95% CI [1.52, 1.80], and P < 0.00001). Random effect in SBP (MD 7.91 mmHg,[6.00, 983], P < 0.00001) and DBP (MD 5.46 mmHg, [3.88, 6.43], P < 0.00001), a subgroup analysis was carried out based on the type of intervention, duration of treatment, and CHM formulas that showed significance. Furthermore, no severe side effects were reported, and no patients stopped treatment or withdrawal due to any severe adverse events.
The authors concluded that compared to WM alone, the therapeutic effectiveness of CHM combined with WM is significantly improved in the treatment of hypertension. Additionally, CHM with WM may safely and efficiently lower systolic blood pressure (SBP) and diastolic blood pressure (DBP) in individuals with PHTN. However, rigorous randomized controlled trials with a large sample, high quality, long duration of treatment, and follow-up are recommended to strengthen this clinical evidence.
The authors can boast of an impressive list of affiliations:
- 1Heilongjiang University of Chinese Medicine, Harbin, 150040, Heilongjiang, China; School of Pharmacy, Lebanese International University, 18644, Sana’a, Yemen.
- 2Heilongjiang University of Chinese Medicine, Harbin, 150040, Heilongjiang, China.
- 3Key Laboratory of Chinese Materia Medica, Ministry of Education of Heilongjiang University of Chinese Medicine, Harbin, 150040, Heilongjiang, China.
- 4Department of Urology, Affiliated Hospital of Qingdao Binhai University, Qingdao, Shandong, China.
- 5Department of Respiratory Diseases, Shandong Second Provincial General Hospital, Shandong University, Shandong, China.
- 6Heilongjiang University of Chinese Medicine, Harbin, 150040, Heilongjiang, China. Electronic address: [email protected].
Impressive in the sense of being impressively prone to bias, particularly knowing that ~80% of Chinese research findings have been shown to be fabricated and considering that Chinese authors as good as never publish anything negative about TCM.
But perhaps you still believe that the results reported here are 100% true? In this case, I might even agree with you. The reason is that the authors demonstrate in exemplary fashion what I have been saying so often before:
Blood pressure is one of the many endpoints that are highly prone to placebo effects. Therefore, even the addition of an ineffective CHM to WM would lower blood pressure more effectively than WM alone.
But there is a third way of explaining the findings of this review: some herbal remedies might actually have a hypotensive effect. The trouble is that this review does come not even close to telling us which.
Guest post by Hans-Werner Bertelsen
As a self-confessed Asterix fan, I made a proposal to the Bremen Medical Association in 2019 that it should no longer orient itself towards the mainstream in the area of further training, but rather towards Klein-Bonum. The board found my proposal very good and unanimously deleted “homeopathy” from the postgraduate training regulations at the next board meeting. The media echo was tremendous. Words of “dam bursting” and “revolution” did the rounds. The “domino effect” was also often quoted in this context, because in the following years, many other German state medical associations followed the Bremen example and removed “homeopathy” from their further training regulations: Saxony-Anhalt, North Rhine, Schleswig-Holstein, Baden-Württemberg, Hamburg, Hesse, Brandenburg, Berlin, Mecklenburg-Western Pomerania, Lower Saxony, Saarland, and Bavaria.
Following the principle of logical plausibility, according to which it makes no sense to support dubious therapies that are not in one’s own training portfolio, but are still reimbursed by many health insurance funds, by convenient billing modalities, the Association of Statutory Health Insurance Physicians Bremen (KVHB) drew a line under the matter and terminated corresponding contracts on my advice. With the termination of the criticized selective contracts, the small federal state of Bremen thus set new standards in 2021. Since the termination, doctors can no longer conveniently provide “homeopathic services” online but have to bill their patients for their services.
But that was not all: the drumbeat of terminated billing contracts had not yet died down in the ears of the “homeopaths”, when only 3 months later, at the meeting of the Federal Medical Association, the next one followed: After a delegate from Bremen (do you want to know if this was a coincidence?) had submitted a motion for the deletion of “homeopathy” from the Model Continuing Medical Education Ordinance (MWBO), this was carried out after a democratic vote at the medical congress in Bremen. The Federal Medical Association thus officially declares this type of sham therapy to be no longer up-to-date, dispensable, and unworthy of further training.
In view of the vote democratically given by the Board, it seems bizarre that the Bavarian Medical Association, despite its own decision to remove “homeopathy” from the WBO, now invokes prolongations because of “transitional periods” in order to be able to continue offering courses in “homeopathy”. Contracts in this regard are to be considered secondary and no longer current. Therefore, the justification given by the ÄND proves to be flimsy and not stringent. The protection of patients from dangerous sham therapies in the case of the omission of indication-appropriate therapies saves lives and thus clearly represents the higher legal interest. Calls for “transitional periods” are redundant and negligently endanger the health of many people. On top of that, an unnecessary extension is a disrespect to the decision made by its own members in the democratic process.
But I remain optimistic that logical plausibility – free of backlogs (!) – will prevail in Bavaria as well. The vote has proven that there is a majority for this and that this majority will not be dominated by money or self-deception.
References
https://www.dr-bertelsen.de/documents/Screenshot_2023-02-10_at_11-36-05_Warum_eine_Aerztekammer_noch_immer_Homoeopathie-Kurse_anbietet-AEND.png
https://publikum.net/die-konigl-bayerische-zuckerkugel/
The use of and interest in so-called alternative medicine (SCAM) for animals is often said to be increasing. But only a few reliable data exist on this subject. This survey is based on online research of 1083 German veterinary homepages for contents of veterinary SCAM performed in September and October 2017. “Veterinarian” and “Chamber of Veterinary Surgeons” were used as search items. Homepages of small animal medicine were included. They were surveyed for modes of SCAM treatments and corresponding qualifications of the offering veterinarian.
In total, 60.7 % (n = 657) of homepages showed contents of veterinary SCAM. The highest percentage was found in the Chamber of Veterinary Surgeons of Saarland (91.7 %, n = 11 out of 12). Homeopathy was cited most frequently (58 %, n = 381). Out of all homepages with relevant content, 31.4 % (n = 206) gave information about user qualifications, with continuous education programs named most frequently (52.9 %, n = 109).
The authors concluded that the given data illustrate the high number of German veterinary homepages with contents of veterinary naturopathy and complementary medicine, corresponding to actual data of a high usage in veterinary and human medicine. Therefore further scientific research in this field seems reasonable. Modes of treatment and qualifications are highly diverse and despite of controversial public discussions, homeopathy was the most frequently cited treatment modality on German veterinary homepages.
The authors also added this: We like to thank the Karl and Veronica Carstens-Foundation for the postgraduate scholarship.
The little addendum makes it less puzzling, I think, why the paper is almost totally devoid of any critical input. Animals can obviously not give informed consent to medical treatments. Like humans, they need the most effective therapy when ill. It is hard to deny that homeopathy, for instance, does not belong in that category. Thus, veterinary SCAM is confronted with a considerable ethical problem. It is beyond me how an article about SCAM use in animals can not even mention this or other critical issues.
But at least, you might argue, the paper informs us which SCAMs are currently the most popular. Wrong! SCAM use is highly prone to changes in fashion. This paper tells us merely which SCAMs were popular several years ago! The time lag between doing the research and publishing it is something I find all too often in SCAM.
The two authors have recently published another paper. Have a look at this article:
The international use of and interest in veterinary naturopathy and complementary medicine are increasing. There are diverse modes of treatment, and owners seem to be well informed. However, there is a lack of data that describes the state of naturopathic or complementary veterinary medicine in Germany. This study aims to address the issue by mapping the currently used treatment modalities, indications, existing qualifications, and information pathways. In order to map the ongoing controversy, this study records the advantages and disadvantages of these medicines as experienced by veterinarians. Demographic influences are investigated to describe distributional impacts on using veterinary naturopathy and complementary medicine.
Methods: A standardised questionnaire was used for the cross-sectional survey. It was distributed throughout Germany in a written and digital format from September 2016 to January 2018. Because of the open nature of data collection, the return rate of questionnaires could not be calculated. To establish a feasible timeframe, active data collection stopped when the previously calculated limit of 1061 questionnaires was reached. With the included incoming questionnaires of that day a total of 1087 questionnaires were collected. Completely blank questionnaires and those where participants did not meet the inclusion criteria (were not included, leaving 870 out of 1087 questionnaires to be evaluated. A literature review and the first test run of the questionnaire identified the following treatment modalities: homoeopathy, phytotherapy, traditional Chinese medicine (TCM), biophysical treatments, manual treatments, Bach Flower Remedies, neural therapy, homotoxicology, organotherapy, and hirudotherapy which were included in the questionnaire. Categorical items were processed using descriptive statistics in absolute and relative numbers based on the population of completed answers provided for each item. Multiple choices were possible. Metric data were not normally distributed (Shapiro Wilk Test); hence the median, minimum, and maximum were used for description. The impact of demographic data on the implementation of veterinary naturopathy and complementary techniques was calculated using the Mann-Whitney-U-Test for metric data and the exact Fisher-Test for categorical data.
Results: Overall 85.4% (n = 679 of total 795 non-blank data sets) of all the questionnaire participants used naturopathy and complementary medicine. The treatments most commonly used were complex homoeopathy (70.4%, n = 478), phytotherapy (60.2%, n = 409), classic homoeopathy (44.3%, n = 301) and biophysical treatments (40.1%, n = 272). The most common indications were orthopedic (n = 1798), geriatric (n = 1428) and metabolic diseases (n = 1124). Over the last five years, owner demand for naturopathy and complementary treatments was rated as growing by 57.9% of respondents (n = 457 of total 789). Veterinarians most commonly used scientific journals and publications as sources for information about naturopathic and complementary contents (60.8%, n = 479 of total 788). These were followed by advanced training acknowledged by the ATF (Academy for Veterinary Continuing Education, an organisation that certifies independent veterinary continuing education in Germany) (48.6%, n = 383). The current information about naturopathy and complementary medicine was rated as adequate or nearly adequate by a plurality (39.5%, n = 308) of the respondents of this question. Further, 27.7% (n = 216) of participants chose the option that they were not confident to answer this question and 91 answers were left blank. The most commonly named advantages in using veterinary naturopathy and complementary medicine were the expansion of treatment modalities (73.5%, n = 566 of total 770), customer satisfaction (70.8%, n = 545) and lower side effects (63.2%, n = 487). The ambiguity of studies, as well as the unclear evidence of mode of action and effectiveness (62.1%, n = 483) and high expectations of owners (50.5%, n = 393) were the disadvantages mentioned most frequently. Classic homoeopathy, in particular, has been named in this context (78.4%, n = 333 of total 425). Age, gender, and type of employment showed a statistically significant impact on the use of naturopathy and complementary medicine by veterinarians (p < 0.001). The university of final graduation showed a weaker but still statistically significant impact (p = 0.027). Users of veterinary naturopathy and complementary medicine tended to be older, female, self-employed and a higher percentage of them completed their studies at the University of Berlin. The working environment (rural or urban space) showed no statistical impact on the veterinary naturopathy or complementary medicine profession.
Conclusion: This is the first study to provide German data on the actual use of naturopathy and complementary medicine in small animal science. Despite a potential bias due to voluntary participation, it shows a large number of applications for various indications. Homoeopathy was mentioned most frequently as the treatment option with the most potential disadvantages. However, it is also the most frequently used treatment option in this study. The presented study, despite its restrictions, supports the need for a discussion about evidence, official regulations, and the need for acknowledged qualifications because of the widespread application of veterinary naturopathy and complementary medicine. More data regarding the effectiveness and the mode of action is needed to enable veterinarians to provide evidence-based advice to pet owners.
This paper seems at first sight a bit more informative. But it suffers very similar problems: the data were outdated before they were even published, and this article too lacks critical input.
So, what purpose might these two articles serve?
None!
Oh, sorry – they probably did manage to get the doctor’s title for one or two poor vet students who had been hoodwinked with the help of the the Karl and Veronica Carstens-Foundation into conducting some rather useless pieces of research.
Turnera diffusa, known as damiana is a shrub native to southern Texas in the United States, Central America, Mexico, South America, and the Caribbean that produces small, aromatic flowers. Damiana is an ingredient in a traditional Mexican liqueur, which is sometimes used in lieu of triple sec in margaritas. Damiana was included in several 19th-century patent medicines, such as Pemberton’s French Wine Coca. The leaves were omitted from that product’s non-alcoholic counterpart, Coca-Cola.
In folklore, the plant was believed to be an aphrodisiac. I looked for evidence from clinical trials but was unable to find any. However, that does not seem to bother PharmaSGP GmbH which produces a drug called Neradin.
The German advertisement of Neradin tells us that:
Bei sexueller Schwäche wie Erektionsstörungen können auch traditionelle Mittel helfen – ohne die Nebenwirkungen mancher chemischer Potenzmittel. Das pflanzliche Arzneimittel Neradin® nutzt dazu erfolgreich Wirkstoffe der mexikanischen Heilpflanze Damiana (Turnera Diffusa).
Die Vorteile von Neradin® auf einen Blick: Fördert die Potenz des Mannes bei sexueller Schwäche
I translated this into English:
Traditional remedies can also help with sexual weakness such as erectile dysfunction – without the side effects of some chemical sexual enhancers. The herbal medicine Neradin® successfully uses active ingredients from the Mexican medicinal plant Damiana (Turnera Diffusa).
The advantages of Neradin® at a glance: Promotes male potency in case of sexual weakness
The patient information leaflet states that “Niradin is a homeopathic drug” and “one tablet Niradin contains 100mg Turnera Diffusa Trit. D4”.
English language sites concur:
Neradin is a homeopathic medicine. Homeopathy is understood as a regulatory therapy for acute and chronic diseases. The areas of application are derived from the homeopathic drug pictures. The following indications are authorised for this medicinal product: Discomfort caused by sexual weakness
So, what we seem to have here is the following:
- A pharma firm that advertises a homeopathic product as a herbal drug.
- A homeopathic remedy that is based on a plant for which there is not a jot of evidence.
- If there were evidence that the plant helps against erectile dysfunction, its homeopathic dilution would, according to the homeopathic ‘like cures like’ axiom, bring about erectile dysfunction.
- A dilution (1:10000) that is too low to have any effect, even if it were made of Viagra.
Am I the only one to think that something is not quite right here?
But don’t let it spoil your HAPPY VALENTINE!
Chiropractors are famous for being against COVID vaccinations and other protective measures. This recent case is an apt example.
It has been reported that the tribunal of Alberta’s regulatory body for chiropractors has ruled against Calgary chiropractor, Curtis Wall, for not wearing a mask during the pandemic. The College of Chiropractors of Alberta (CCA) sought to discipline Wall for not wearing a mask at his clinic, not observing two meters of social distancing while unmasked, not installing a plexiglass barrier in his reception area, and not requiring patients to be masked either, beginning around June 2020. In a statement issued Feb. 1, 2023, the CCA’s hearing tribunal wrote: “[T]he Hearing Tribunal has found Dr. Curtis Wall’s conduct does constitute ‘unprofessional conduct’ and their decision for penalty is forthcoming.”
Lawyer James Kitchen who represented Wall, railed against the ruling: “[T]he decision is riddled with errors of fact and law and is so poorly decided it is an embarrassment to the chiropractic profession. It is shocking the lengths the tribunal went to dismiss the evidence of Dr. Wall, three of his patients, and his four expert witnesses while blithely accepting all the evidence of the College…The decision is an egregious manifestation of pre-determined, results-oriented decision-making.”
In an interview, Kitchen said: “I set this whole case up knowing that the tribunal would likely do whatever the college and the college’s expert told him to do. I set the case up such that if the tribunal did that, they would have to make themselves look very foolish to do so. If I’m really putting my cynical hat on, I don’t know if there’s anything that surprises me, really. It should shock me the degree to which they twisted the evidence, left out the evidence. The only thing that surprises me a little bit is the lack of effort they put in to hide their bias.”
The communications manager of the CCA, Dana Myckan, commented: “Pursuant to the Health Professions Act, all Hearing Tribunal decisions are posted publicly on the CCA website. This is the extent of the information that the CCA can share on behalf of the Hearing Tribunal.”
The ruling noted that Wall initially wore a mask, but in June 2020, he “self-diagnosed as having an anxiety disorder. He believed that his self-diagnosis qualified him for a medical exemption from wearing a mask. As a result, he stopped wearing a mask when treating patients.” It added that Wall never contacted the college to let it know his condition or request an exemption, and said Wall’s son also worked at the clinic and did not wear a mask.
Kitchen said Wall could face a suspension of his practice but will appeal this ruling or any attempt to make him pay the CCA’s legal costs, which the college stated during the hearings were in excess of $200,000. Kitchen said a recent court precedent suggests the CCA will be unable to recoup costs in a ruling.
An appeal would be heard by the council of the college, which is the college’s governing body. It consists of five chiropractors elected by their peers along with five members of the public appointed by the government. Should Wall lose there, he could take his case to the Alberta Court of Appeal. Kitchen said Wall will go the distance. “I warned them that this is how I expected it to go. So he was prepared,” Kitchen said. “He’s still pretty dismayed that people could have this much evidence staring them in the face and just ignore it and follow the narrative. It’s hard for him. He’s an idealist. He’s really big on truth and people doing what’s right.”
________________________
To all of this, I have but two questions:
- Is the CCA not also guilty of professional misconduct for calling Wall “Dr. Wall” without making it clear that he is not medically trained?
- If Wall is “big on truth”, how come he works as a chiropractor?
I recently came across a truly baffling article. As it is in German, I translated it for you:
Supply shortages have kept pharmacies on tenterhooks for months, with more than 400 common medicines missing. The German Central Association of Homeopathic Doctors (DZVhÄ) suggests switching to alternative medicine as a solution: “We have homeopathic medicines that have been tried and tested in practice for more than 200 years and can replace many medicines that are currently not available,” says the president of the DZVhÄ , Dr Michaela Geiger.
The DZVhÄ is convinced that homeopathic medical practices can replace fever-reducing medicines, but in many cases also antibiotics and much more. However, Geiger qualifies: “Due to our medical training, we also know that cancer drugs such as the often cited Tamoxifen cannot be replaced by homeopathy”.
The homeopathic doctors respond directly to the sharpest argument of their critics: “But let’s assume that homeopathy only works via the placebo effect, as is being rumored, even then it would be an option, especially if other options are lacking,” says DZVhÄ vice-president Dr. Ulf Riker. Since homeopathically trained doctors can judge the general course of a disease, they can also distinguish a placebo effect from a medicinal effect.
…
If fever medication for children is lacking, parents should not be deprived of another “therapy option”, Riker said. “If you do not get your conventional fever medication in the coming weeks, visit a specialist pharmacy for naturopathy and homeopathy. If you are due for a medical consultation, experienced homeopathic doctors can prescribe a suitable homeopathic medicine for you,” he says.
Why do I find this so intriguing?
Essentially, what we have learned from the article is the following:
- “Tried and tested in practice for more than 200 years” is ‘homeopathy speak’ for “effective”, even if the evidence tells us otherwise.
- Homeopathic remedies can replace many evidence-based conventional medications such as fever-reducing medicines, antibiotics, and much more, even if the evidence tells us otherwise.
- Homeopaths know that cancer drugs cannot be replaced by homeopathy – except for those homeopaths who seem to have forgotten this simple lesson.
- Homeopathic placebos are a realistic option when there is a supply problem with effective drugs, even if the evidence tells us otherwise.
- Homeopathically trained doctors can distinguish a placebo effect from a medicinal effect, even if there is no evidence that any clinician can reliably do this.
- Homeopathic doctors prescribe suitable homeopathic medicine. Suitable for whom? As it is ineffective, it is unsuitable for the patient. Therefore, Riker is probably talking about the homeopath.
So, what have we really learned from this article? I don’t know about you, but I got the impression that the president and the vice president of the DZVhÄ do not seem to mind putting patients in danger, as long as they can promote homeopathy.
Homeopathic remedies are highly diluted formulations without proven clinical benefits, traditionally believed not to cause adverse events. Nonetheless, published literature reveals severe local and non-liver-related systemic side effects. This paper presents the first series on homeopathy-related severe drug-induced liver injury (DILI) from a single center.
A retrospective review of records from January 2019 to February 2022 identified 9 patients with liver injury attributed to homeopathic formulations. Competing causes were comprehensively excluded. Chemical analysis was performed on retrieved formulations using triple quadrupole gas chromatography-mass spectrometry and inductively coupled plasma atomic emission spectroscopy.
Males predominated with a median age of 54 years. The most typical clinical presentation was acute hepatitis, followed by acute on chronic liver failure. All patients developed jaundice, and ascites were notable in one-third of the patients. Five patients had underlying chronic liver disease. COVID-19 prevention was the most common indication for homeopathic use. Probable DILI was seen in 77.8%, and hepatocellular injury predominated (66.7%). Four (44.4%) patients died (3 with chronic liver disease) at a median follow-up of 194 days. Liver histopathology showed necrosis, portal and lobular neutrophilic inflammation, and eosinophilic infiltration with cholestasis. A total of 29 remedies were consumed between 9 patients, and 15 formulations were analyzed. Toxicology revealed industrial solvents, corticosteroids, antibiotics, sedatives, synthetic opioids, heavy metals, and toxic phyto-compounds, even in ‘supposed’ ultra-dilute formulations.
The authors concluded that homeopathic remedies potentially result in severe liver injury, leading to death in those with underlying liver disease. The use of mother tinctures, insufficient dilution, poor manufacturing practices, adulteration and contamination, and the presence of direct hepatotoxic herbals were the reasons for toxicity. Physicians, the public, and patients must realize that Homeopathic drugs are not ‘gentle placebos.’
Over a decade ago, we published a systematic review entitled “Adverse effects of homeopathy: a systematic review of published case reports and case series”:
Aim: The aim of this systematic review was to critically evaluate the evidence regarding the adverse effects (AEs) of homeopathy.
Method: Five electronic databases were searched to identify all relevant case reports and case series.
Results: In total, 38 primary reports met our inclusion criteria. Of those, 30 pertained to direct AEs of homeopathic remedies; and eight were related to AEs caused by the substitution of conventional medicine with homeopathy. The total number of patients who experienced AEs of homeopathy amounted to 1159. Overall, AEs ranged from mild-to-severe and included four fatalities. The most common AEs were allergic reactions and intoxications. Rhus toxidendron was the most frequently implicated homeopathic remedy.
Conclusion: Homeopathy has the potential to harm patients and consumers in both direct and indirect ways. Clinicians should be aware of its risks and advise their patients accordingly.
It caused an outcry from fans of homeopathy who claimed that one cannot insist that homeopathic remedies are ineffective because they contain no active ingredient, while also arguing that they cause severe adverse effects. In a way, they were correct: homeopathic remedies are useless even at causing adverse effects. But this applies only to remedies that are manufactured correctly and that are highly dilute. The trouble is that quality control in homeopathy often seems to be less than adequate. And this is how adverse effects can happen!
The new article from India is an important addition to the literature providing more valuable information about the risks of homeopathy. Its authors were able to do chemical analyses of some of the remedies and could thus show what the reasons for the liver injuries were. The article provides an essential caution for those who delude themselves by assuming that homeopathy is harmless. In fact, the remedies can cause severe problems. But, as we have discussed regularly on this blog, the far greater risk in homeopathy is not the remedy but the homeopath and his/her all too often incompetent advice to patients.
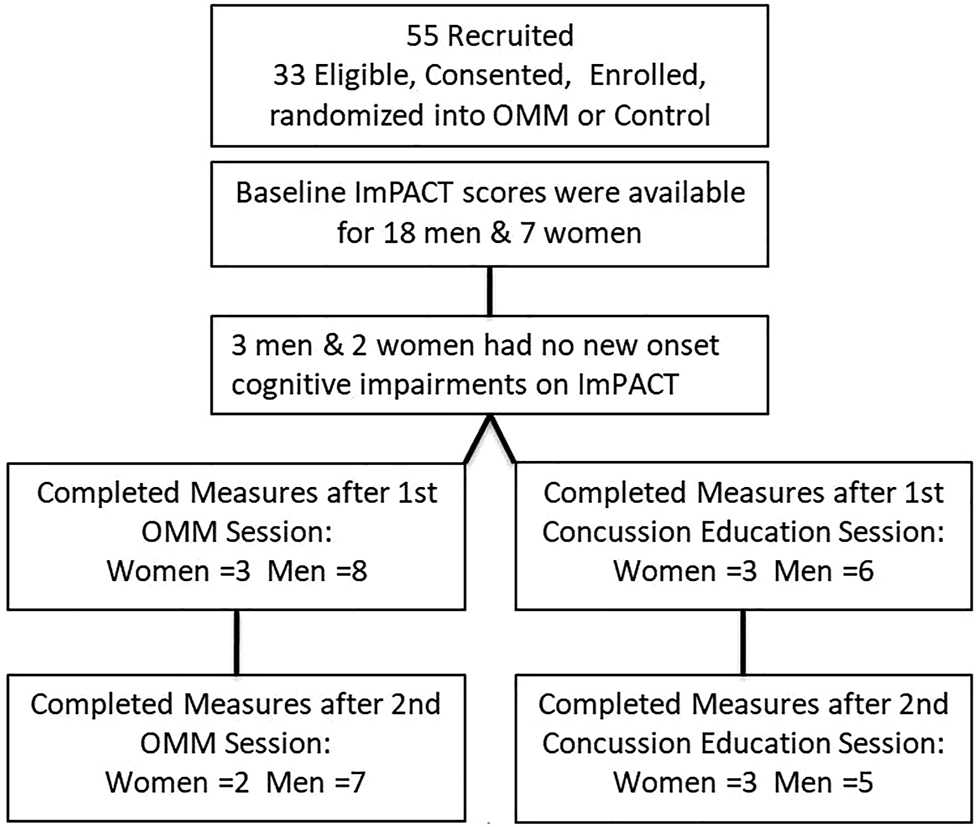
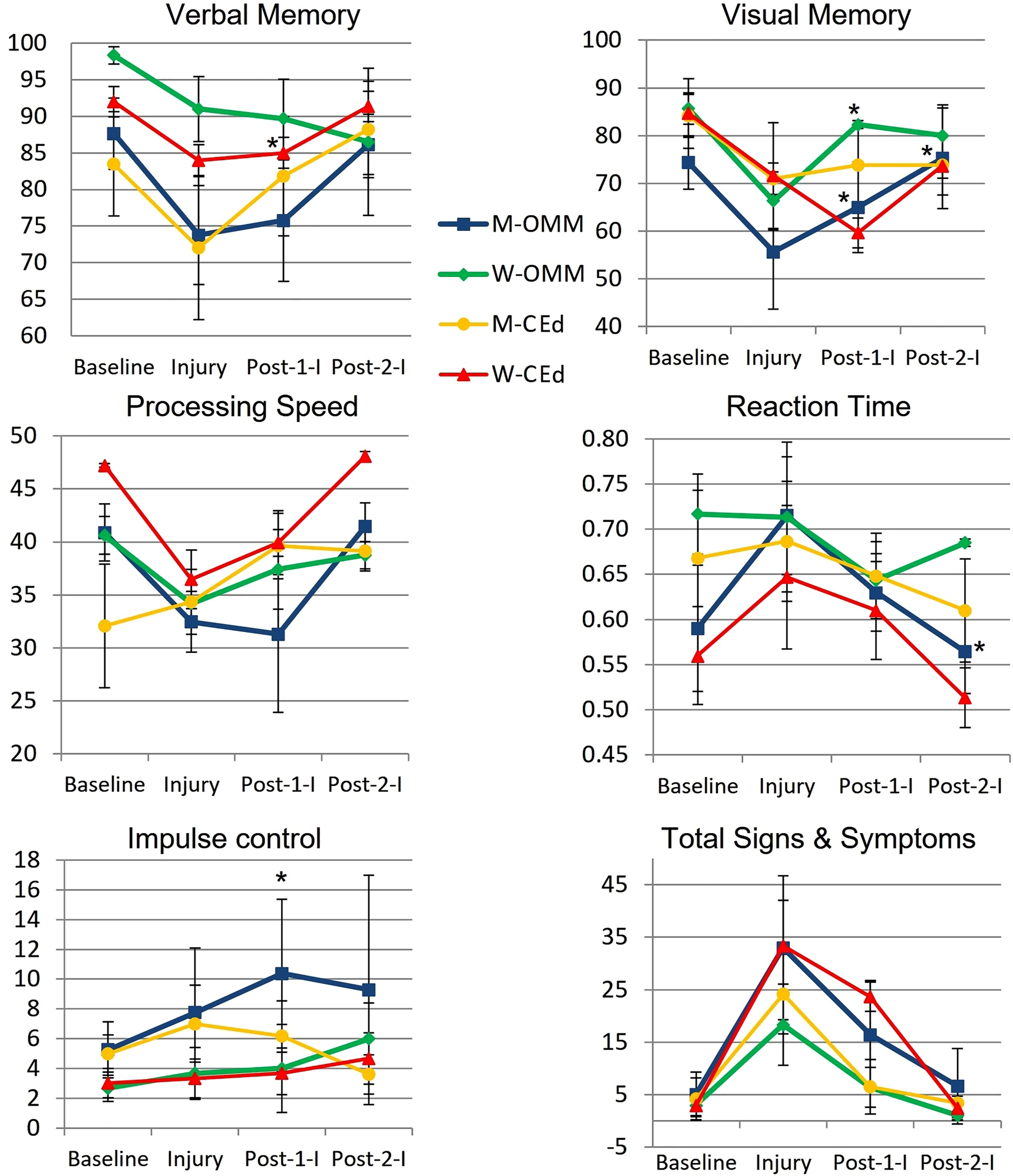
This study from the department of Osteopathic Manipulative Medicine, New York Institute of Technology College of Osteopathic Medicine tested whether new-onset impairments (NOI) of neurological functions identified by Immediate Post-Concussion Assessment and Cognitive Testing (ImPACT) will improve more so after osteopathic manipulative medicine (OMM) than after concussion-education.
College athletes presenting to the outpatient academic healthcare center (AHCC) with concussion due to head injury within the preceding 2 weeks were recruited for this IRB-approved, randomized, single-blinded trial. Consented men and women were randomized into two groups:
- the verum group received two OMM treatments;
- the control group received two concussion-education sessions.
Preseason, Baseline, ImPACT was compared to Post-Injury scores to determine NOI. Baseline, Post-Injury, and Post-Interventions ImPACTs were compared by analysis of variance (ANOVA, α≤0.05). Post-Injury correlations and mean changes in King-Devick (KD) scores were analyzed.
Post-Injury NOI were found in 77.8% (14/18) men and 85.7% (6/7) women, including ImPACT subscore indices for verbal and visual memory, processing speed (PS), and reaction time (RT). Of those with NOI, mean visual memory recovered by 50.0% following one and by 104.9% (p=0.032) following two OMM treatments in men and by 82.8% (p=0.046) following one treatment in women. Following two interventions, the mean RT in men receiving OMM improved by 0.10 more than education (p=0.0496). The effect sizes of OMM were large (Cohen’s d=1.33) on visual memory and small (Cohen’s d=0.31) on RT.
The authors concluded that NOI in visual memory and RT following concussion significantly improved in the OMM group compared to the education group. Integrating OMM utilizing physical exam and this treatment was a safe individualized approach in athletes with acute uncomplicated concussions. Further research is warranted to improve the utilization of OMM for individuals with concussion.
What the abstract does not tell you is that the two groups were extremely small and that they became even smaller, as some patients were lost to follow-up.
In addition, the results were all over the place.
Furthermore, it is noteworthy that neither the therapists nor the patients were blinded and the observation period was short. Finally, the authors state in their conclusions that OMM is safe. Considering the sample size and the attrition rate (perhaps all those patients lost to follow-up died?), this is of course ridiculously wishful thinking.
So, what can we conclude from this study? I don’t know about you, but I conclude that the department of Osteopathic Manipulative Medicine, New York Institute of Technology College of Osteopathic Medicine could do with a good science teacher.
Wellness seems to be everywhere these days – I mean of course the term, not the state or condition. On Medline, we find in excess of 500 000 articles on wellness, just for the year 2022! Wellness is en vogue, sexy, politically correct, etc. It looks good to talk and write about it. Most importantly it is good business. A report by the Global Wellness Institute stated that in 2020 the wellness industry was valued at $4.5 trillion and continues to grow at a frightening rate.
Having studied some of the recent literature on the subject, I get the impression that, for many, wellness is foremost an excuse for waffling utter nonsense. Let me, therefore, today ask just 5 simple questions about wellness that are likely to reduce the wellness of the ‘wellness brigade’:
1.What is wellness?
It is quite evidently a sector that is unable to define itself. Here are just a few of the definitions that have been suggested. Wellness is:
- the active pursuit of activities, choices and lifestyles that lead to a state of holistic health
- the result of personal initiative, seeking a more optimal, holistic and balanced state of health and well-being across multiple dimensions
- an active process of becoming aware of and making choices towards a healthy and fulfilling life
- the state of being in good health, especially as an actively pursued goal
- a state beyond absence of illness but rather aims to optimize well-being
- the act of practicing healthy habits on a daily basis to attain better physical and mental health outcomes
- an active process through which people become aware of, and make choices toward, a more successful existence
- the optimal state of health of individuals and groups
A 2018 review revealed that there is a lack of a uniform definition of wellness and showed that there is insufficient evidence to support the clinical utility of a single particular wellness instrument.
2. How do we measure wellness?
The short answer to this question is: nobody is quite sure. There simply is no generally accepted, well-validated measure. A few domains come to mind:
- physical functioning,
- somatic symptoms, e.g. pain,
- psychological symptoms,
- social functioning,
- needs and satisfaction.
But there is no simple means to quantify wellness. If you think that I am exaggerating, consider this recent review: 79 mental wellness instruments were identified. Most studies did not provide a definition for mental wellness. We identified thirteen mental wellness concepts from 97 studies, namely: life satisfaction, mental wellbeing [general], resilience, self-efficacy, self- esteem, connectedness, coping, self-control, mindfulness/spiritual, hope, sense of coherence, happiness, and life purpose.
3. What affects wellness?
The short answer is: potentially everything. My very own wellness, for instance, deteriorates sharply, if I have to read yet another nonsensical article about it.
4. Which interventions improve wellness?
As we have seen in my previous post, this is where so-called alternative medicine (SCAM) comes in. Since there is no measure to quantify wellness, we just have to take the word of SCAM proponents for it: SCAM improves wellness!!!
Which specific SCAM?
Can I see the evidence?
Sorry, no questions allowed!
And if you dare to insist on evidence, the ‘wellness brigade’ would just give you a pitiful smile and say: wellness has to be experienced, not measured.
5. Are there risks?
Yes, of course! Here are just some of them:
- The treatments advocated for wellness almost invariably cost money.
- The treatments advocated for wellness almost invariably cause direct and indirect harm, as discussed in many of my previous posts.
- Wellness treatments tend to give the impression that one can buy wellness like an expensive piece of clothing without putting in any real effort oneself.
Considering all this, I’d like to offer my very own definition of the sector:
Wellness is a fashionable paradise for charlatans in which they are protected from scientific scrutiny and feel at liberty to bullshit to their hearts’ content.
The All-Party Parliamentary Group (APPG) on Beauty and Wellbeing, UK, has undertaken an investigation into the ‘complementary therapies sector’, to consider how the sector can support everyone’s physical health, mental health, and well-being and take pressure off the NHS. In their recent document, they state:
The complementary therapies industry is an integral part of the Personal Care sector, which includes beauty, wellbeing, and alternative therapies. These therapies can be key to supporting everyone’s health and mental wellbeing…
To ensure complementary therapies can adequately support the NHS, we need to attract more talent into the sector and ensure all therapists receive the right training to become highly skilled professionals.
We also need to enhance the perception of the professionalism within the sector, so that it is no longer seen as ‘frivolous and fluffy’ and non-essential. Building awareness and understanding of its value in supporting our nation’s health is one step. However, it also important to crack down on any bad practice and the ‘underground market’ of poor treatment…
The committee makes the following recommendations:
1. The Government must work with NHS England to better promote the benefits of social prescribing with GPs, nurses and other health and care professionals, and how they can refer people to non-clinical complementary therapy services.
2. The Personal Care sector team in the Department for Business, Energy, Industry and Strategy must work with officials within the Department for Health and Social Care responsible for social prescribing to better integrate complementary therapy services into the NHS, and produce guidance to support health professionals and therapists in doing so.
3. The Department for Health and Social Care must undertake or fund research studies to demonstrate the value of integrating complementary therapy services into the NHS through social prescribing.
4. The Department for Education must revisit the gap between the apprentice wage and minimum wage for apprentices aged 19+, and provide financial incentives for employers to take on learners on any ‘job ready ‘qualification.
5. The Government must give Environmental health officers (EHOs) greater powers to act quickly to deal with bad practice and lead a crack-down on tax evading businesses that are driving down prices and undermining legitimate businesses under pressure.
…
…
…
Conclusions
The evidence that we have received during this investigation clearly demonstrate that greater support
and recognition is needed for the complementary therapies sector to ensure that they are able support
everyone’s physical health, mental health and wellbeing and take pressure off the NHS.
We hope the Government will review our recommendations in order to support the complementary
therapies sector and ensure they have adequate funding and acknowledgement.
In case you are wondering what therapies they refer to, here is their complete list of the treatments (including links to what they seem to think about them):
This could have made me laugh, had it not been so serious. The committee is composed of MPs who might be full of goodwill. Yet, they seem utterly clueless regarding the ‘complementary therapies sector’. For instance, they seem to be unaware of the evidence for some of the treatments they want to promote, e.g. craniosacral therapy, aromatherapy, Reiki, shiatsu, energy healing, or reflexology (which is far less positive than they seem to assume); and they aim at enhancing the “perception of the professionalism” instead of improving the PROFESSIONALISM of the therapists (which obviously would include adherence to evidence-based practice). And perhaps the committee might have given some thought to the question of whether it is ethical to push dubious therapies onto the unsuspecting public.
I could go on, but the perplexing wooliness of the document speaks for itself, I think.
And in case you are wondering who the MP members of the committee are, here is the list of its members:
• Carolyn Harris MP – Co-Chair
• Judith Cummins MP – Co-Chair
• Jessica Morden MP – Vice-Chair
• Jackie Doyle-Price MP – Vice-Chair
• Peter Dowd MP – Treasurer
• Nick Smith MP – Secretary
• Caroline Nokes MP – Member
• Sarah Champion MP – Member
• Alex Davies-Jones MP – Member
• Kate Osamor MP – Member
• John McNally MP – Member
• Kevan Jones MP – Member
• Gagan Mohindra MP- Member
The Secretariat for this APPG is Dentons Global Advisors with support from the National Hair and Beauty Federation, the Federation of Holistic Therapists and spabreaks.com.
PS
Two hours after having posted this, I begin to feel bad about being so dismissive. Let me thus try to do something constructive: I herewith offer to give one or more lectures to the committee about the evidence as it pertains to the therapies they included in their report.