pseudo-science
Yes, Today is ‘WORLD SLEEP DAY‘ and you are probably in bed hoping this post will put you back to sleep.
This study aimed to synthesise the best available evidence on the safety and efficacy of using moxibustion and/or acupuncture to manage cancer-related insomnia (CRI).
The PRISMA framework guided the review. Nine databases were searched from its inception to July 2020, published in English or Chinese. Randomised clinical trials (RCTs) of moxibustion and or acupuncture for the treatment of CRI were selected for inclusion. The methodological quality was assessed using the method suggested by the Cochrane collaboration. The Cochrane Review Manager was used to conduct a meta-analysis.
Fourteen RCTs met the eligibility criteria; 7 came from China. Twelve RCTs used the Pittsburgh Sleep Quality Index (PSQI) score as continuous data and a meta-analysis showed positive effects of moxibustion and or acupuncture (n = 997, mean difference (MD) = -1.84, 95% confidence interval (CI) = -2.75 to -0.94, p < 0.01). Five RCTs using continuous data and a meta-analysis in these studies also showed significant difference between two groups (n = 358, risk ratio (RR) = 0.45, 95% CI = 0.26-0.80, I 2 = 39%).
The authors concluded that the meta-analyses demonstrated that moxibustion and or acupuncture showed a positive effect in managing CRI. Such modalities could be considered an add-on option in the current CRI management regimen.
Even at the risk of endangering your sleep, I disagree with this conclusion. Here are some of my reasons:
- Chinese acupuncture trials invariably are positive which means they are as reliable as a 4£ note.
- Most trials were of poor methodological quality.
- Only one made an attempt to control for placebo effects.
- Many followed the A+B versus B design which invariably produces (false-) positive results.
- Only 4 out of 14 studies mentioned adverse events which means that 10 violated research ethics.
Sorry to have disturbed your sleep!
This review assessed the magnitude of reporting bias in trials assessing homeopathic treatments and its impact on evidence syntheses.
A cross-sectional study and meta-analysis. Two persons independently searched Clinicaltrials.gov, the EU Clinical Trials Register and the International Clinical Trials Registry Platform up to April 2019 to identify registered homeopathy trials. To determine whether registered trials were published and to detect published but unregistered trials, two persons independently searched PubMed, Allied and Complementary Medicine Database, Embase and Google Scholar up to April 2021. For meta-analyses, the authors used random effects models to determine the impact of unregistered studies on meta-analytic results.
The investigators reported the proportion of registered but unpublished trials and the proportion of published but unregistered trials. They also assessed whether primary outcomes were consistent between registration and publication
Since 2002, almost 38% of registered homeopathy trials have remained unpublished, and 53% of published randomised controlled trials (RCTs) have not been registered. Retrospective registration was more common than prospective registration. Furthermore, 25% of primary outcomes were altered or changed compared with the registry. Although we could detect a statistically significant trend toward an increase of registrations of homeopathy trials (p=0.001), almost 30% of RCTs published during the past 5 years had not been registered.
A meta-analysis stratified by registration status of RCTs revealed substantially larger treatment effects of unregistered RCTs (SMD: −0.53, 95% CI −0.87 to −0.20) than registered RCTs (SMD: −0.14, 95% CI −0.35 to 0.07).
The authors concluded that registration of published trials was infrequent, many registered trials were not published and primary outcomes were often altered or changed. This likely affects the validity of the body of evidence of homeopathic literature and may overestimate the true treatment effect of homeopathic remedies.
An obvious investigation to do (why did I not have this idea?)!
And a finding that will surprise few (except fans of homeopathy who will, of course, dispute it).
The authors also mention that reporting biases are likely to have a substantial impact on the estimated treatment effect of homeopathy. Using data from a highly cited meta-analysis of homeopathy RCTs, our example showed that unregistered trials yielded substantially larger treatment effects than registered trials. They also caution that, because of the reporting biases identified in their analysis, effect estimates of meta-analyses of homeopathy trials might substantially overestimate the true treatment effect of homeopathic remedies and need to be interpreted cautiously.
In other words, the few reviews suggesting that homeopathy works beyond placebo (and are thus celebrated by homeopaths) are most likely false-positive. And the many reviews showing that homeopathy does not work would demonstrate this fact even clearer if the reporting bias had been accounted for.
Or, to put it bluntly:
The body of evidence on homeopathy is rotten to the core and therefore not reliable.
Plantar fasciitis (PF) is a chronic degenerative condition causing marked thickening and fibrosis of the plantar fascia, and collagen necrosis, chondroid metaplasia and calcification. There is little convincing evidence in support of various approaches, including homeopathy, for treating PF. This study was undertaken to examine the efficacy of individualized homeopathic medicines (IHMs) compared with placebo in the treatment of PF.
This double-blind, randomized, placebo-controlled trial was conducted at the outpatient departments of Mahesh Bhattacharyya Homoeopathic Medical College and Hospital, West Bengal, India. Patients were randomized to receive either IHMs or identical-looking placebo in the mutual context of conservative non-medicinal management. The Foot Function Index (FFI) questionnaire, as an outcome measure, was administered at baseline, and every month, up to 3 months. Group differences (unpaired t-tests) and effect sizes (Cohen’s d) were calculated on an intention-to-treat sample. The sample was analyzed statistically after adjusting for baseline differences.
The target sample size was 128; however, only 75 could be enrolled (IHMs: 37; Placebo: 38). Attrition rate was 9.3% (IHMs: 4, Placebo: 3). Differences between groups in total FFI% score favored IHMs against placebo at all the time points, with large effect sizes: month 1 (mean difference, -10.0; 95% confidence interval [CI], -15.7 to -4.2; p = 0.001; d = 0.8); month 2 (mean difference, -14.3; 95% CI, -20.4 to -8.2; p <0.001; d = 1.1); and month 3 (mean difference, -23.3; 95% CI, -30.5 to -16.2; p <0.001; d = 1.5). Similar significant results were also observed on three FFI sub-scales (pain%, disability%, and activity limitation%). Natrum muriaticum (n = 14; 18.7%) and Rhus toxicodendron and Ruta graveolens (n = 11 each; 14.7%) were the most frequently prescribed medicines. No harms, serious adverse events, or intercurrent illnesses were recorded in either of the groups.
The authors concluded that IHMs acted significantly better than placebo in the treatment of PF; however, the trial being underpowered, the results should be interpreted as preliminary only. Independent replications are warranted.
It is nice to see homeopaths stress the importance of independent replication. It is less nice, however, to note their main conclusion:
IHMs acted significantly better than placebo.
This essentially is what will stick in the minds of the pro-homeopathy reader, and this is the information that will enter into future meta-analyses and systematic reviews of homeopathy. But this is also untrue! The qualifier that follows is but a lame excuse for drawing a wrong conclusion. In my view, a correct conclusion would read something like this:
Our study failed to recruit a sufficient number of patients. Therefore, no conclusions about the efficacy of IHM can be drawn from it.
Vaccine hesitancy is currently recognized by the WHO as a major threat to global health. During the COVID-19 pandemic, there has been a growing interest in the role of social media in the propagation of false information and fringe narratives regarding vaccination. Using a sample of approximately 60 billion tweets, Danish investigators conducted a large-scale analysis of the vaccine discourse on Twitter. They used methods from deep learning and transfer learning to estimate the vaccine sentiments expressed in tweets, then categorize individual-level user attitudes towards vaccines. Drawing on an interaction graph representing mutual interactions between users, They analyzed the interplay between vaccine stances, interaction network, and the information sources shared by users in vaccine-related contexts.
The results show that strongly anti-vaccine users frequently share content from sources of a commercial nature; typically sources that sell alternative health products for profit. An interesting aspect of this finding is that concerns regarding commercial conflicts of interests are often cited as one of the major factors in vaccine hesitancy.
The authors furthermore demonstrate that the debate is highly polarized, in the sense that users with similar stances on vaccination interact preferentially with one another. Extending this insight, the authors provide evidence of an epistemic echo chamber effect, where users are exposed to highly dissimilar sources of vaccine information, enforcing the vaccination stance of their contacts.
The authors concluded that their findings highlight the importance of understanding and addressing vaccine mis- and disinformation in the context in which they are disseminated in social networks.
In the article, the authors comment that their findings paint a picture of the vaccine discourse on Twitter as highly polarized, where users who express similar sentiments regarding vaccinations are more likely to interact with one another, and tend to share contents from similar sources. Focusing on users whose vaccination stances are the positive and negative extremes of the spectrum, we observe relatively disjoint ‘epistemic echo chambers’ which imply that members of the two groups of users rarely interact, and in which users experience highly dissimilar ‘information landscapes’ depending on their stance. Finally, we find that strongly anti-vaccine users much more frequently share information from actors with a vested commercial interest in promoting medical misinformation.
One implication of these findings is that online (medical) misinformation may present an even greater problem than previously thought, because beliefs and behaviors in tightly knit, internally homogeneous communities are more resilient, and provide fertile ground for fringe narratives, while mainstream information is attenuated. Furthermore, such polarization of communities may become self-perpetuating, because individuals avoid those not sharing their views, or because exposure to mainstream information might further entrench fringe viewpoints.
The present study investigated the impact of a purposefully designed Islamic religion-based intervention on reducing depression and anxiety disorders among Muslim patients using a randomised controlled trial design. A total of 62 Muslim patients (30 women and 32 men) were divided by gender into two groups, with each group assigned randomly to either treatment or control groups. The participants who received the Islamic-based intervention were compared to participants who received the control intervention.
The Islamic-Based Intervention that was applied to the two experimental groups (i.e. one male, one female) has several components. These components were based on moral and religious concepts and methods, including moral confession, repentance, insight, learning, supplication, seeking Allah’s mercy, seeking forgiveness, remembrance of Allah, patience, trust in Allah, self-consciousness, piety, spiritual values, and moral principles. The techniques implemented in the intervention included the art of asking questions, clarifying, listening, interacting, summarising, persuading, feedback, empathy, training practice, reflecting feelings, discussion, and dialogue, lecturing, brainstorming, reinforcement, modeling, positive self-talk, evaluation, homework, practical applications, activation games (play through activities), emotional venting, stories, presentation, correction of thoughts, and relaxation. The two control groups (i.e. one male, one female) received the energy path program provided by the Al-Nour Centre. This program aimed to enhance self-confidence and modify people’s behavior with anxiety disorders, depression, and obsessive-compulsive disorder. Both interventions comprised 30 sessions over 30 h; two sessions were conducted per week, and each session lasted for 60 min (one hour). The duration of the intervention was 15 weeks.
Taylor’s manifest anxiety scale and Steer and Beck’s depression scale were used for examining the effects on depression and anxiety levels. The results revealed that the Islamic intervention significantly reduced anxiety levels in women and depression levels in men compared to the typical care control groups.
The authors concluded that religious intervention played a vital role in lowering the patients’ level of anxiety among women and depression among men. In general, religious practices prevent individuals from becoming subject to mental disorders, i.e. anxiety and depression.
The authors comment that the Islamic religion-based intervention (RSAFI) significantly reduced the levels of depression and anxiety among the participants. Also, there was a substantial improvement in the patients’ general health after the intervention. They were satisfied and believed that everything happening to them was destined by Allah. These results could be attributed to the different intervention practices that relied on the guidance of the Holy Quran and Sunnah. For instance, Saged et al. (2020) confirmed that the Holy Quran significantly impacts healing patients who suffer from physical, psychological, and mental disorders. In this respect, Moodley et al. (2018) concluded that having faith in Allah offers a relatively quick approach to healing patients suffering from heartache and depression. This goes hand in hand because the recitation of the Quran and remembrance of Allah help patients feel relaxed and peaceful. Muslims believe that the Quran is the word of Allah and that Allah’s words exert a significant impact on the healing of mental health patients, as, ultimately, Almighty Allah is the one who cures illnesses.
When discussing the limitations of their study, the authors state that the sample of this study was limited to the patients with anxiety and depression disorders at the Al-Nour Centre in Kuala Lumpur, so the results cannot be generalized to other samples. Furthermore, the treatment of anxiety was restricted to females, whereas the treatment of depression was restricted to males. Additionally, the selection of females and males as samples for the study was based on their pre-measurement of anxiety and depression, which serve as self-report measures.
The authors seem to be unconcerned about the fact that the 2 interventions (verum and control) were clearly distinguishable and their patients thus were not blinded (and neither were the evaluators). This obviously means that the observed effect might have nothing at all to do with the Islamic-Based Intervention but could be entirely due to expectation and persuasion.
Why might the authors not even bother to discuss such an obvious possibility?
A look at their affiliations might provide the answer:
- 1Academy of Islamic Studies, University of Malaya, 50603, Kuala Lumpur, Malaysia. [email protected].
- 2Academy of Islamic Studies, University of Malaya, 50603, Kuala Lumpur, Malaysia.
- 3Faculty of Education, Universiti Teknologi Malaysia, Johor, Malaysia.
- 4Faculty of Education, University of Malaya, 50603, Kuala Lumpur, Malaysia.
- 5Islamic Banking and Finance, International Islamic University Malaysia, Selangor, Malaysia.
- 6Department of Hadith and Associated Sciences, Nourah Bint Abdulrahman University, Riyadh, Saudi Arabia.
On Amazon, someone commented as follows on my biography of Prince Charles:
… Dr. Ernst goes on digressions that mostly seem intended to make Prince Charles look bad. There’s a long chapter on Laurens van der Post, who influenced Prince Charles as a youth, and a lot about somewhat unsavory things he did. So what? …
This made me think. I read the chapter again and find it hard to agree with the comment. To me, this chapter is a short (~2000 words) and essential part of the book. Judge for yourself; here are a few excerpts from it: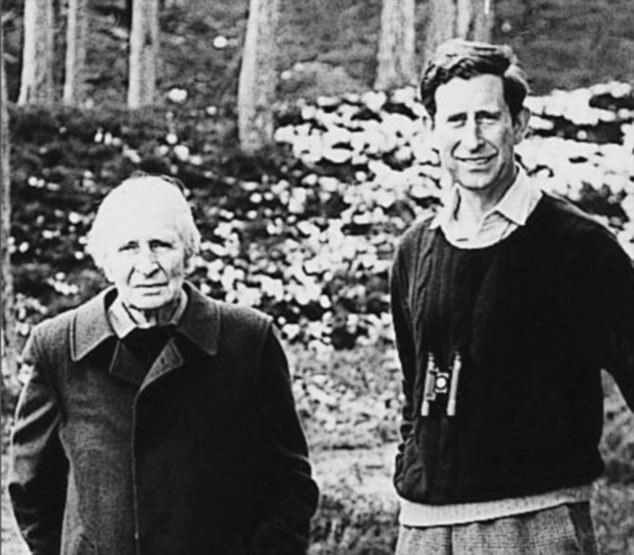
“It seemed to have been a union of mutual needs, between a Prince longing to find meaning in his existence and a storyteller who could weave apparent answers out of thin air.” Laurence van der Post was oozing charm and charisma and sensed that “for the Prince, there was a missing dimension”, as Jonathan Dimbleby put it. By 1975, the two men had formed such a close rapport that van der Post felt able to counsel him about spiritual matters, urging him to explore the ‘old world of the spirit’ and ‘the inward way’ towards truth and understanding. Van der Post suggested the two make a seven week journey into the Kalahari desert. This, he believed, would introduce Charles to the spirit world. Preparations were made in 1977 but, in the end, the plan had to be abandoned. Instead, the two later went to Kenya where they spent 5 days of long walks and “intense conversation”.
Van der Post urged Charles to play “a dynamic and as yet unimagined role to suit the future shape of a fundamentally reappraised and renewed modern society”, a reappraisal that would be “so widespread and go so deep that it will involve a prolonged fight for all that is good and creative in the human imagination.” An aspect of this fight, he claimed, would be “to restore the human being to a lost natural aspect of his own spirit; to restore his relevance for life and his love of nature, and to draw closer to the original blueprint and plan of life…”
Laurence left an interview for posthumous publication; in it, he expressed his hope that Charles would never become king, as this would imprison him, it would be more important that Charles continues to be a great prince. “He’s been brought up in a terrible way … He’s a natural Renaissance man, a man who believes in the wholeness and totality of life … Why should it be that if you try to contemplate your natural self that you should be thought to be peculiar?”
“For 20 years they had most intimate conversations and correspondence … with a steady flow of reassurance and encouragement, political and diplomatic advice, memoranda, draft speeches and guidance for reading”. Van der Post introduced Charles to the teachings of Carl Jung and his concept of the ‘collective unconscious’ that binds all humans together regardless whether they are Kalahari bushmen or princes. On the behest of van der Post, Charles began to record his dreams which van der Post then interpreted according to Jung’s theories. In the late 1970s van der Post tried to convince Charles to give up all his duties and withdraw from the world completely in search for an ‘inner world truth’. This plan too was aborted.
All biographers agree that van der Post was the strongest intellectual influence of Charles’ life.
- Charles sought van der Post’s advice and spiritual guidance on numerous occasions.
- When William was born, he made van der Post his godfather.
- When Charles’ marriage to Diana ran into difficulties, the couple was counselled by van der Post.
- Charles invited Laurence regularly to Highgrove, Sandringham and Balmoral.
- Charles visited van der Post on his deathbed.
- After Laurence’s death, Charles created a series of annual lectures hosted in van der Post’s memory which he hosted in St James’ Palace.
…
…
…
Charles’ notions about medicine were unquestionably inspired by van der Post. Laurence. He, for instance, bemoaned the inadequacy of conventional medicine and wrote: “Even if doctors did … use dreams and their decoding as an essential part of their diagnostic equipment and perhaps could confront cancer at the point of entry, how are they to turn it aside, unless they are humble enough to keep their instruments in their cases and look for some new form of navigation over an uncharted sea of the human spirit?” As we will see in the next chapters, van der Post’s influence shines through in many of Charles’ speeches. Moreover, it contributed to the attitude of many critical observers towards Charles. Christopher Hitchens is but one example for many:
“We have known for a long time that Prince Charles’ empty sails are so rigged as to be swelled by any passing waft or breeze of crankiness and cant. He fell for the fake anthropologist Laurens van der Post. He was bowled over by the charms of homeopathic medicine. He has been believably reported as saying that plants do better if you talk to them in a soothing and encouraging way… The heir to the throne seems to possess the ability to surround himself—perhaps by some mysterious ultramagnetic force?—with every moon-faced spoon-bender, shrub-flatterer, and water-diviner within range.”
The following chapters will show that Hitchens might not have been far off the mark.
___________________________
Yes, I do feel that the chapter is essential for the book. It explains how Charles’ love affair with alternative medicine got started and why it would become so intense and durable. Without it, the reader would not be able to understand the rest of the book. Moreover, it is important to demonstrate that van der Post was a charlatan and an accomplished liar. This is relevant because, in later life, Charles’ skill to choose adequate advisors was often wanting.
The Nobel Prize laureate Luc Montagnier has died at the age of 89.
Montagnier became the hero of the realm of homeopathy when he published findings suggesting that ultra-molecular dilutions are not just pure water but might have some activity. In this context, he has been mentioned repeatedly on this blog. During the years that followed his support for homeopathy, things got from bad to worse, and Montagnier managed to alienate most of the scientific community.
Amongst other things, he became a champion of the anti-vax movement, supported the view that vaccination causes autism, and argued that viral infections including HIV could be cured by diet. During the pandemic, he then claimed that Sars-CoV-2 had originated from a laboratory experiment attempting to combine coronavirus and HIV. On French television, he claimed that vaccination was an “enormous mistake” that would only promote the spread of new variants.
Before Montagnier became a victim of ‘Nobelitis‘, he had a brilliant career as a virologist in his world-famous Paris lab. A co-worker of Montagnier, Barré-Sinoussi, managed to isolate a retrovirus from an AIDS patient in 1983. They called it ‘lymphadenopathy-associated virus’, and concluded that it may be involved in several pathological syndromes, including AIDS.
Meanwhile, in the US, Gallo had identified a family of immunodeficiency retroviruses that he called human T-lymphotropic virus (HTLV). In 1984, Gallo announced that one of these viruses was the cause of AIDS. The US government swiftly patented a blood test for detecting antibodies to it. Thus it became possible to screen for the virus in the blood.
When it became clear that material used in Gallo’s studies included samples that Montagnier had supplied in 1983, one of the fiercest rows in the history of science ensued. Eventually, negotiations between the two governments settled it by resolving that the two scientists should be equally credited. In 2002, Gallo and Montagnier published a joint paper acknowledging each other’s role: Montagnier’s team discovered HIV, and Gallo’s proved it caused AIDS. When Gallo was excluded from the Nobel prize given in 2008 to Montagnier and Barré-Sinoussi, the world of science was stunned. The spectacular dispute between Galo and Montagnier became the subject of a movie and several books.
Montagnier died on 8/2/2022 leaving behind his wife Dorothea and their three children, Anne-Marie, Francine, and Jean-Luc.
The new issue of the BMJ carries an article on acupuncture that cries out for a response. Here, I show you the original article followed by my short comments. For clarity, I have omitted the references from the article and added references that refer to my comments.
_________________________________________
Conventional allopathic medicine [1]—medications and surgery [2] used in conventional systems of medicine to treat or prevent disease [3]—is often expensive, can cause side effects and harm, and is not always the optimal treatment for long term conditions such as chronic pain [4]. Where conventional treatments have not been successful, acupuncture and other traditional and complementary medicines have potential to play a role in optimal patient care [5].
According to the World Health Organisation (WHO) 2019 global report, acupuncture is widely used across the world. [6] In some countries acupuncture is covered by health insurance and established regulations. [7] In the US, practitioners administer over 10 million acupuncture treatments annually. [6] In the UK, clinicians administer over 4 million acupuncture treatments annually, and it is provided on the NHS. [6]
Given the widespread use of acupuncture as a complementary therapy alongside conventional medicine, there has been an increase in global research interest and funding support over recent decades. In 2009, the European Commission launched a Good Practice in Traditional Chinese Medicine Research (GP-TCM) funding initiative in 19 countries. [7] The GP-TCM grant aimed to investigate the safety and efficacy of acupuncture as well as other traditional Chinese medicine interventions.
In China, acupuncture is an important focus of the national research agenda and receives substantial research funding. [8] In 2016, the state council published a national strategy supporting universal access to acupuncture by 2020. China has established more than 79 evidence-based traditional Chinese medicine or integrative medicine research centers. [9]
Given the broad clinical application and rapid increase in funding support for acupuncture research, researchers now have additional opportunities to produce high-quality studies. However, for this to be successful, acupuncture research must address both methodological limitations and unique research challenges.
This new collection of articles, published in The BMJ, analyses the progress of developing high quality research studies on acupuncture, summarises the current status, and provides critical methodological guidance regarding the production of clinical evidence on randomised controlled trials, clinical practice guidelines and health economic evidence. It also assesses the number and quality of systematic reviews of acupuncture. [10] We hope that the collection will help inform the development of clinical practice guidelines, health policy, and reimbursement decisions. [11]
The articles document the progress of acupuncture research. In our view, the emerging evidence base on the use of acupuncture warrants further integration and application of acupuncture into conventional medicine. [12] National, regional, and international organisations and health systems should facilitate this process and support further rigorous acupuncture research.
Footnotes
This article is part of a collection funded by the special purpose funds for the belt and road, China Academy of Chinese Medical Sciences, National Natural Science Foundation of China, the National Center for Complementary and Integrative Health, the Innovation Team and Talents Cultivation Program of the National Administration of Traditional Chinese Medicine, the Special Project of “Lingnan Modernization of Traditional Chinese Medicine” of the 2019 Guangdong Key Research and Development Program, and the Project of First Class Universities and High-level Dual Discipline for Guangzhou University of Chinese Medicine. The BMJ commissioned, peer reviewed, edited, and made the decision to publish. Kamran Abbasi was the lead editor for The BMJ. Yu-Qing Zhang advised on commissioning for the collection, designed the topic of the series, and coordinated the author teams. Gordon Guyatt provided valuable advice and guidance. [13]
1. Allopathic medicine is the term Samuel Hahnemann coined for defaming conventional medicine. Using it in the first sentence of the article sets the scene very well.
2. Medicine is much more than ‘medications and surgery’. To imply otherwise is a strawman fallacy.
3. What about rehabilitation medicine?
4. ‘Conventional medicine is not always the optimal treatment’? This statement is very confusing and wrong. It is true that conventional medicine is not always effective. However, it is by definition the best we currently have and therefore it IS optimal.
5. Another fallacy: non sequitur
6. Another fallacy: appeal to popularity.
7. Yet another fallacy: appeal to authority.
8. TCM is heavily promoted by China not least because it is a most lucrative source of income.
9. Several research groups have shown that 100% of acupuncture research coming out of China report positive results. This casts serious doubt on the reliability of these studies (see, for instance, here, here, and here).
10. It has been noted that more than 80 percent of clinical data from China is fabricated.
11. Based on the points raised above, it seems to me that the collection’s aim is not to provide objective information but uncritical promotion.
12. I find it telling that the authors do not even consider the possibility that rigorous research might demonstrate that acupuncture cannot generate more good than harm.
13. This statement essentially admits that the series of articles constitutes paid advertising for TCM. The BMJ’s peer-review process must have been less than rigorous in this case.
Stress is associated with a multitude of physical and psychological health impairments. To tackle these health disorders, over-the-counter (OTC) products like Neurodoron® are popular since they are considered safe and tolerable. One tablet of this anthroposophic remedy contains the following active ingredients:
- 83.3 mg Aurum metallicum praeparatum trituration (trit.) D10,
- 83.3 mg Kalium phosphoricicum trit. D6,
- 8.3 mg Ferrum-Quarz trit. D2.
Experience reports and first studies indicate that Neurodoron® is efficient in the treatment of stress-associated health symptoms. “To confirm this” (!!!), a non-interventional study (NIS) with pharmacies was conducted.
The NIS was planned to enroll female and male patients who suffered from nervous exhaustion with symptoms caused by acute and/or chronic stress. The main outcome measures were characteristic stress symptoms, stress burden, and perceived stress. Further outcome measures included perceived efficacy and tolerability of the product as assessed by the patients and collection of adverse drug reactions (ADRs). A study duration of about 21 days with a recommended daily dose of 3–4 tablets was set.
In total, 279 patients were enrolled at 74 German pharmacies. The analyzed set (AS) included 272 patients (mean age 44.8 ± 14.4 years, 73.9% female). 175 patients of the AS completed the NIS. During the study, all stress symptoms declined significantly (total score 18.1 vs. 12.1 (of max. 39 points), < 0.0001). Furthermore, a reduction of stress burden (relative difference in stress burden, VAS = −29.1%, < 0.0001) was observed. For most patients, perceived stress was reduced at the study end (PSQ total score decreased in 70.9% of the patients). 75.9% of the study population rated the product efficacy as “good” or “very good” and 96.6% rated its tolerability as “good” or “very good.” One uncritical ADR was reported.
The authors concluded that this study adds information on the beneficial effects of Neurodoron® in self-medication. The results from this NIS showed a marked reduction in stress burden and perceived stress, along with an excellent safety profile of the medicinal product (MP) Neurodoron®. Further trials are required to confirm these results.
I beg to differ!
The study had no control group and therefore one cannot possibly attribute any of the observed changes to the anthroposophic remedy. They are more likely to be due to:
- the natural history of the condition,
- regression towards the mean,
- a placebo effects,
- other treatments administered during the trial period.
Sadly, the authors discuss none of these possibilities in their paper.
In view of this, I am tempted to rephrase their conclusions as follows:
This study adds no valuable information on the effects of Neurodoron® in self-medication. The results from this NIS showed what utter nonsense the Weleda marketing team is capable of producing in an attempt to boost sales.
PS
These declarations of the 4 study authors and the sponsorship are revealing, I thought:
RH and CS are employees of Weleda AG, Germany. JH and KS work for daacro GmbH & Co. KG, a clinical research organization, Germany. The authors declare that there are no conflicts of interest.
This study was financed by the pharmaceutical company Weleda AG, Arlesheim, the employer of RH and CS. Weleda commissioned the CRO daacro for their contribution to the manuscript.
Bioresonance is an alternative therapeutic and diagnostic method employing a device developed in Germany by Scientology member Franz Morell in 1977. The bioresonance machine was further developed and marketed by Morell’s son-in-law Erich Rasche and is also known as ‘MORA’ therapy (MOrell + RAsche). Bioresonance is based on the notion that one can diagnose and treat illness with electromagnetic waves and that, via resonance, such waves can influence disease on a cellular level.
On this blog, we have discussed the idiocy bioresonance several times (for instance, here and here). My favorite study of bioresonance is the one where German investigators showed that the device cannot even differentiate between living and non-living materials. Despite the lack of plausibility and proof of efficacy, research into bioresonance continues.
The aim of this study was to evaluate if bioresonance therapy can offer quantifiable results in patients with recurrent major depressive disorder and with mild, moderate, or severe depressive episodes.
The study included 140 patients suffering from depression, divided into three groups.
- The first group (40 patients) received solely bioresonance therapy.
- The second group (40 patients) received pharmacological treatment with antidepressants combined with bioresonance therapy.
- The third group (60 patients) received solely pharmacological treatment with antidepressants.
The assessment of depression was made using the Hamilton Depression Rating Scale, with 17 items, at the beginning of the bioresonance treatment and the end of the five weeks of treatment.
The results showed a statistically significant difference for the treatment methods applied to the analyzed groups (p=0.0001). The authors also found that the therapy accelerates the healing process in patients with depressive disorders. Improvement was observed for the analyzed groups, with a decrease of the mean values between the initial and final phase of the level of depression, of delta for Hamilton score of 3.1, 3.8 and 2.3, respectively.
The authors concluded that the bioresonance therapy could be useful in the treatment of recurrent major depressive disorder with moderate depressive episodes independently or as a complementary therapy to antidepressants.
One could almost think that this is a reasonably sound study. But why did it generate such a surprising result?
When reading the full paper, the first thing one notices is that it is poorly presented and badly written. Thus there is much confusion and little clarity. The questions keep coming until one comes across this unexpected remark: the study was a retrospective study…
This explains some of the confusion and it certainly explains the surprising results. It remains unclear how the patients were selected/recruited but it is obvious that the groups were not comparable in several ways. It also becomes very clear that with the methodology used, one can make any nonsense look effective.
In the end, I am left with the impression that mutton is being presented as lamb, even worse: I think someone here is misleading us by trying to convince us that an utterly bogus therapy is effective. In my view, this study is as clear an example of scientific misconduct as I have seen for a long time.


