progress
Research by the Milner Center for Evolution at the University of Bath, U.K., along with colleagues at the Universities of Oxford and Aberdeen, found that trust in scientists has hugely increased since the COVID-19 pandemic. The study also found that people were more likely to take the COVID-19 vaccine if their trust in the science had increased.
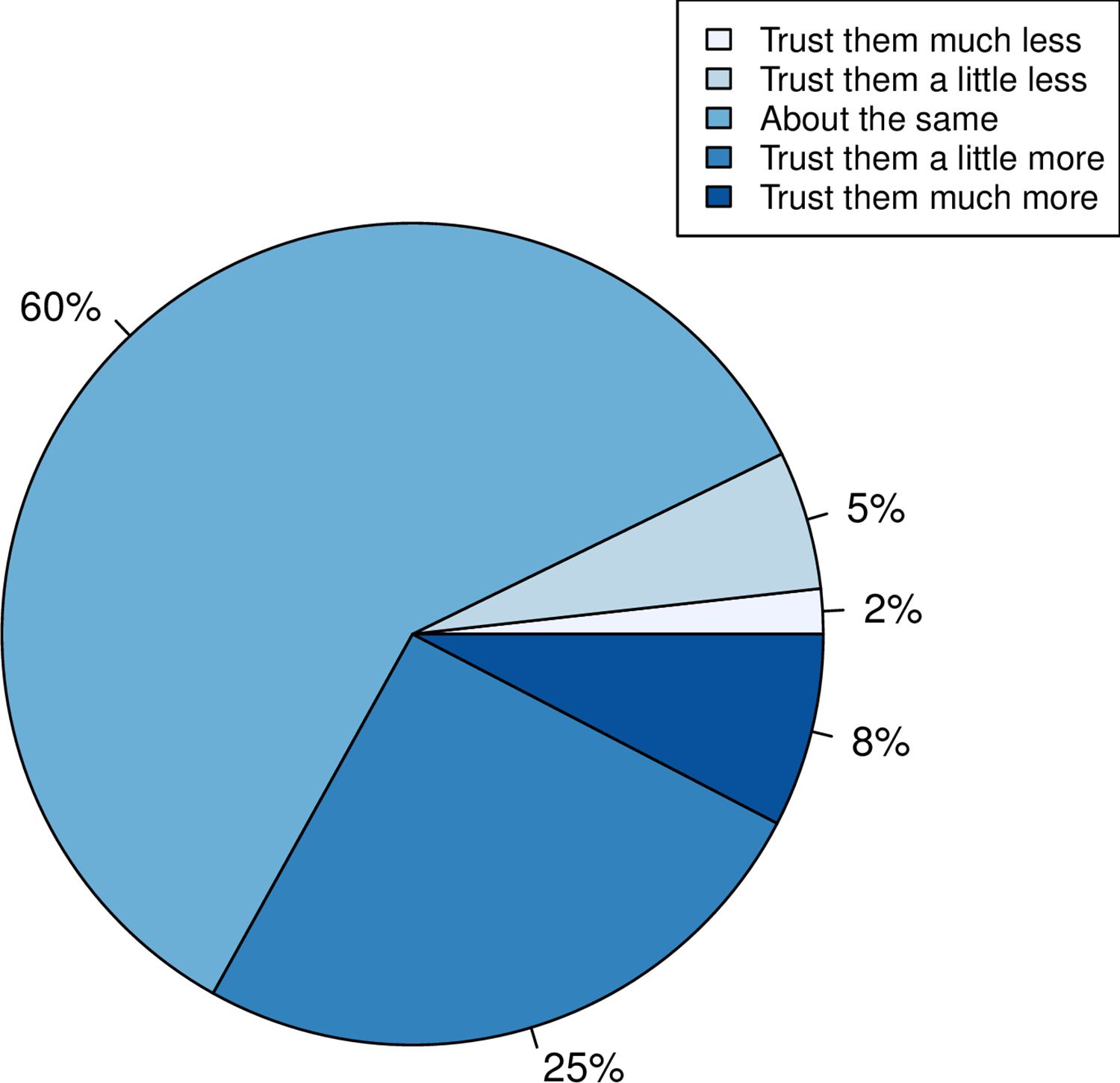
Using data from a survey of more than 2,000 U.K. adults commissioned by the Genetics Society, the team asked individuals whether their trust in scientists had gone up, down, or stayed the same.
- A third of people reported that their trust in scientists had gone up.
- When Pfizer, a company that made COVID-19 vaccines, was used as an example of the pharma industry, more people reported a positive response than when GlaxoSmithKline, a company not associated with the COVID-19 vaccine, was mentioned.
- The researchers also found that people who reported holding a negative view of science before the pandemic had become even more negative.
- People reporting increased trust were most likely to take the COVID-19 vaccine.
- Those preferring not to do so reported a decline in trust.
This is an interesting study with relevance to many discussions we had on this blog. I recommend reading it in full. Here are the abstract and link to the paper:
While attempts to promote acceptance of well-evidenced science have historically focused on increasing scientific knowledge, it is now thought that for acceptance of science, trust in, rather than simply knowledge of, science is foundational. Here we employ the COVID-19 pandemic as a natural experiment on trust modulation as it has enabled unprecedented exposure of science. We ask whether trust in science has on the average altered, whether trust has changed the same way for all and, if people have responded differently, what predicts these differences? We 1) categorize the nature of self-reported change in trust in “scientists” in a random sample of over 2000 UK adults after the introduction of the first COVID vaccines, 2) ask whether any reported change is likely to be real through consideration of both a negative control and through experiment, and 3) address what predicts change in trust considering sex, educational attainment, religiosity, political attitude, age and pre-pandemic reported trust. We find that many more (33%) report increased trust towards “scientists” than report decreased trust (7%), effects of this magnitude not being seen in negative controls. Only age and prior degree of trust predict change in trust, the older population increasing trust more. The prior degree of trust effect is such that those who say they did not trust science prior to the pandemic are more likely to report becoming less trusting, indicative of both trust polarization and a backfire effect. Since change in trust is predictive of willingness to have a COVID-19 vaccine, it is likely that these changes have public health consequences.
Two years ago, I published a blog about the research activity in SCAM. To demonstrate the volume of SCAM research I looked into Medline to find the number of papers published in 2020 for the SCAMs listed below. Now I repeated the exercise for the year 2022. The respective 1st numbers below are those of 2020, and the second ones refer to 2022 (in bold):
- acupuncture 2 752 – 3,565
- anthroposophic medicine 29 – 28
- aromatherapy 173 – 205
- Ayurvedic medicine 183 – 249
- chiropractic 426 – 498
- dietary supplement 5 739 – 8,915
- essential oil 2 439 – 3,340
- herbal medicine 5 081 – 16,207
- homeopathy 154 – 212
- iridology 0 – 0
- Kampo medicine 132 – 176
- massage 824 – 996
- meditation 780 – 1,016
- mind-body therapies 968 – 1,616
- music therapy 539 – 716
- naturopathy 68 – 92
- osteopathic manipulation 71 – 85
- Pilates 97 – 152
- qigong 97 – 121
- reiki 133 – 158
- tai chi 397 – 470
- Traditional Chinese Medicine 15 277 – 22,586
- yoga 698 – 837
These data suggest the following:
- As before, the research activity in SCAM seems relatively low.
- Most numbers are pretty stable with a slight overall increase.
- The meager numbers for anthroposophic medicine, homeopathy, iridology, Kampo, and naturopathy are remarkable.
- In absolute terms, only acupuncture, dietary supplements, essential oil, herbal medicine, and TCM are impressive; by and large, these are areas where commercial interest and sponsors exist.
- The ‘big winners’ in terms of increase over time are acupuncture, supplements, essential oil, herbal medicine, and TCM; I suspect that much of this is due to the fast-growing (and repeatedly mentioned) influence that China is gaining in SCAM.
When I was still at Exeter, I used to do an average of about 4 peer reviews per week of articles that had been submitted to all sorts of journals for publication. Now I reject most of these invitations and do perhaps just one per month.
Why?
Conducting a peer review is by no means an easy task. You have to realize that the authors have usually put a lot of hard work into their paper and a lot may depend on it in terms of their future. They thus have the right to receive a fair and responsible review. To do the job properly, it took me (even with plenty of experience in reading scientific papers) between 1 and 3 hours per article. Crucially, low-quality articles typically submitted to low-quality journals are more work than papers that adhere to a certain standard.
I do not think that the journal editors who send the submissions out for review appreciate how much work they ask from the reviewers. They normally pay nothing (even if they charge exorbitant handling fees from the authors) and offer you no benefit at all. In addition, many have systems that are more than tedious asking you to register, create a pin number, etc., etc. Then you have to follow certain rules and formats that differ from journal to journal. In a word, they add an administrative burden to the task of reading, understanding, checking a paper, and composing your judgment on it.
All this can be cumbersome but it’s not the reason why I do less and less peer reviews. The true reason is that research papers on so-called alternative medicine (SCAM) are now mostly published in one of the many 3rd class SCAM journals that have recently sprung up. There are so many of them that they, of course, struggle to get enough articles to fill their pages. In turn, this means that they are far too keen to publish anything regardless of its quality or validity. As a consequence, the quality of these articles and their authors are often dismal.
Here is an example of a (rather shocking but not unusual) email I received only today; it might show you what I mean:
Dear Professor!
…
I want to publish some papers in “Areas related to your research field”. Can you help me? I can provide a thank you fee!
For example, I will give you a $2000 thank you fee for helping me write articles. For example, if you add my name to your article, I will give you a $1000 thank you fee. Or I can help you pay for APC.
I know this email is presumptuous, but my friends and I need to publish dozens of papers every year. If you can help me, we can cooperate for a long time. I’m not kidding, I’m very sincere!
If you are offended, please forgive me!
Look forward to your reply!
Warmly Wishes, …
When I do a review for a low-quality SCAM journal and find major defects in an article, my experience has been that the editor then decides to publish it nonetheless. When this happens, I feel frustrated and ask myself: WHY DID THEY ASK FOR MY OPINION IF THEY DO NOT ABIDE BY IT?
Thus I decided that these journals are just as well off without my contributions. So, if you are an editor of a SCAM journal, do me a favor and do not molest me with your invitations to conduct a peer review and
COUNT ME OUT!
Aromatherapy is popular yet it has a problem: there is no indication for it. Yes, it can make you feel better but this is hardly a true medical indication. I know of many things that make me feel better, and I would not call them a THERAPY! But perhaps this new study from Iran offers a solution for the dilemna:
Sleep plays an essential role in infant development. This randomized clinical trial investigated the effect of aromatherapy with rose water on the deep sleep status of premature infants admitted to a neonatal intensive care unit (NICU).
The study was conducted on 64 infants hospitalized in NICUs. In the intervention group, two drops of rose water were poured on gas and placed next to the babies’ heads. The control group was treated in the same way except that distilled water was employed. The ALS scale was used to assess the sleep status.
Of the 66 infants in this study, 30 were female and 36 were male. The average gestational age of the infants was 32.5 ± 1.99 weeks. The results showed that the amount of deep sleep (type A and B) in the intervention group was significantly higher than the control group during and after the intervention (p=0.001).
The authors concluded that, considering the positive impact of rose water in improve of sleep quality in premature babies; it can be used to improve sleeping condition of infants in hospitals, along with main treatment.
The study has many flaws and it is badly written. Yet, I find it interesting. If its results can be confirmed with a more rigorous trial, aromatherapy might finally find a true medical purpose.
Yesterday, it has been reported that Indian scientists found the mode of action of homeopathic remedies. This is the newspaper article:
And this seems to be the abstract of the actual paper:
Homeopathic medicines contain ultra-low concentrations of metal and compounds, and it is challenging to classify homeopathic potencies using modern characterization tools. This work presents a novel experimental tool for classifying various homeopathic medicines under a low-frequency generated electromagnetic (EM) fields. A custom-built primary coil is used for generating EM fields at different excitation frequencies. The potentized test samples were prepared at decimal dilution scale of Ferrum with α‑lactose monohydrate and exhibited significant and distinct induced EM responses in the second sensing coil. The measured responses decrease logarithmically due to reducing Ferrum concentration. The resolution improved in higher potencies from 0.03 µV at 300 Hz to 0.24 µV at 4.8 kHz. Different compounds of homeopathic medicines were also investigated to produce distinct induced EM characteristics. These results were correlated with Raman spectroscopy, impedance analyser, and FT-IR analysis. The experimental investigation confirmed the classification of potencies and the technique developed to detect ultra-low metallic concentrations.
I might be a bit slow on the uptake – but I don’t see how this investigation proves anything. Perhaps someone can explain it to me?
I had all but forgotten about these trials until a comment by ‘Mojo’ (thanks Mojo!) reminded me of this article in the JRSM by M.E. Dean. It reviewed these early trials of homeopathy back in 2006. Here are the crucial excerpts:
The homeopath in both trials was a Dr Herrmann, who received a 1-year contract in February 1829 to test homeopathy with the Russian military.3 The first study took place at the Military Hospital in the market town of Tulzyn, in the province of Podolya, Ukraine.4 At the end of 3 months, 164 patients had been admitted, 123 pronounced cured, 18 were convalescing, 18 still sick, and six had died. The homeopathic ward received many gravely ill patients, and the small number of deaths was shown at autopsy to be due to advanced gross pathologies. The results were interesting enough for the Russian government to order Herrmann to the Regional Military Hospital at St Petersburg to take part in a larger trial, supervised by a Dr Gigler. Patients were admitted to an experimental homeopathic ward, for treatment by Herrmann, and comparisons were made with the success rate in the allopathic wards, as happened in Tulzyn. The novelty was Gigler’s inclusion of a ‘no treatment’ ward where patients were not subject to conventional drugging and bleeding, or homeopathic dosing. The untreated patients benefited from baths, tisanes, good nutrition and rest, but also:
‘During this period, the patients were additionally subjects of an innocent deception. In order to deflect the suspicion that they were not being given any medicine, they were prescribed pills made of white breadcrumbs or cocoa, lactose powder or salep infusions, as happened in the homeopathic ward.’3 (page 415)
The ‘no treatment’ patients, in fact, did better than those in both the allopathic and homeopathic wards. The trial had important implications not just for homeopathy but also for the excessive allopathic drugging and bleeding that was prevalent. As a result of the report, homeopathy was banned in Russia for some years, although allopathy was not.
… A well-known opponent of homeopathy, Carl von Seidlitz, witnessed the St Petersburg trial and wrote a hostile report.5 He then conducted a homeopathic drug test in February 1834 at the Naval Hospital in the same city in which healthy nursing staff received homeopathically-prepared vegetable charcoal or placebo in a single-blind cross-over design.6 Within a few months, Armand Trousseau and colleagues were giving placebo pills to their Parisian patients; perhaps in the belief that they were testing homeopathy, and fully aware they were testing a placebo response.7,8 A placebo-controlled homeopathic proving took place in Nuremberg in 1835 and even included a primitive form of random assignment—identical vials of active and placebo treatment were shuffled before distribution.9 Around the same time in England, Sir John Forbes treated a diarrhoea outbreak after dividing his patients into two groups: half received allopathic ‘treatment as usual’ and half got bread pills. He saw no difference in outcome, and when he reported the experiment in 1846 he added that the placebos could just as easily have been homeopathic tablets.10 In 1861, a French doctor gave placebo pills to patients with neurotic symptoms, and his attitude is representative: he called the placebo ‘orthodox homeopathy’, because, as he said, ‘Bread pills or globules of Aconitum 30c or 40c amount to the same thing’.11
References:
Alzheimer’s is a devastating disease against which conventional healthcare has little to offer. No wonder, therefore, that so-called alternative medicine (SCAM) claims to have a wide range of effective treatments. But how good are they really? The present review aimed to explore the role of SCAM in the treatment of Alzheimer’s disease (AD).
Literature searches were conducted using Ovid MEDLINE, CINAHL, Cochrane, and PubMed databases and reference lists up to November 30, 2021. Only randomized clinical trials were included and appraised using the National Institute of Health framework. Data analysis showed that herbs like Gingko Biloba, Melissa Officinalis, Salvia officinalis, Ginseng, and saffron alone or in combination with curcumin, a low-fat diet, NuAD-Trail, and soy lecithin showed significant positive effects on AD. Moreover, the combination of natural and pharmaceuticals has far better effects than only allopathic treatment. The authors concluded that different herbal remedies in combination with FDA approved drugs are effective and more promising in the treatment of AD.
To these findings we need to add a study that is too recent to have been included in the review:
The aim of the randomized clinical trial (RCT) was to investigate the effects of fenugreek seed extract on memory, depression, quality of life, blood pressure, and serum malondialdehyde (MDA) and total antioxidant capacity (TAC) levels in adult AD patients. The study participants included 82 AD patients with mild-to-moderate memory deficits. Patients in the intervention group received 5 cc of fenugreek seed extract for 4 months and subjects in the control group received a placebo. Memory, depression, quality of life, and BP levels, as well as serum MDA and TAC, were assessed before and after the intervention.
There was a significant increase in serum levels of TAC (p < 0.001) and a reduction in serum MDA status (p < 0.001) after 4 months of fenugreek seed extract supplementation. In addition, increasing levels of memory (p < 0.001) and quality of life (p < 0.001), as well as reduction of depression (p = 0.002), systolic BP (p < 0.001), and diastolic BP (p < 0.001) levels were detected in the intervention group compared with baseline.
The authors concluded that Fenugreek seed extract supplementation in AD patients shows promising positive effects on memory, quality of life, BP, and selective oxidative indices levels.
So, there is hope! Some of the evidence is promising but far from convincing. What we need – obviously – is more and better research.
This review investigated the characteristics, hotspots, and frontiers of global scientific output in acupuncture research for chronic pain over the past decade. the authors retrieved publications on acupuncture for chronic pain published from 2011 to 2022 from the Science Citation Index Expanded (SCI-expanded) of the Web of Science Core Collection (WoSCC). The co-occurrence relationships of journals/countries/institutions/authors/keywords were performed using VOSviewer V6.1.2, and CiteSpace V1.6.18 analyzed the clustering and burst analysis of keywords and co-cited references.
A total of 1616 articles were retrieved. The results showed that:
- the number of annual publications on acupuncture for chronic pain has increased over time;
- the main types of literature are original articles (1091 articles, 67.5 %) and review articles (351 articles, 21.7 %);
- China had the most publications (598 articles, 37 %), with Beijing University of Traditional Chinese Medicine (93 articles, 5.8 %);
- Evidence-based Complementary and Alternative Medicine ranked first (169 articles, 10.45 %) as the most prolific affiliate and journal, respectively;
- Liang FR was the most productive author (43 articles);
- the article published by Vickers Andrew J in 2012 had the highest number of citations (625 citations).
Recently, “acupuncture” and “pain” appeared most frequently. The hot topics in acupuncture for chronic pain based on keywords clustering analysis were experimental design, hot diseases, interventions, and mechanism studies. According to burst analysis, the main research frontiers were functional connectivity (FC), depression, and risk.
The authors concluded that this study provides an in-depth perspective on acupuncture for chronic pain studies, revealing pivotal points, research hotspots, and research trends. Valuable ideas are provided for future research activities.
I might disagree with the authors’ conclusion and would argue that they have demonstrated that:
- the acupuncture literature is dominated by China, which is concerning because we know that 1) these studies are of poor quality, 2) never report negative findings, and 3) are often fabricated;
- the articles tend to be published in journals that are more than a little suspect.
As we have seen recently, the reliable evidence that acupuncture remains effective is wafer-thin. Therefore, I feel that we are currently being misled by a flurry of rubbish publications that have one main aim: to distract from the fact that acupuncture might be nonsense.
I have featured the ‘Münster Circle‘ before. The reason why I do it again today is that we have just published a new Memorandum entitled HOMEOPATHY IN THE PHARMACY. Here is its summary which I translated into English:
Due to questionable regulations in German pharmaceutical law, homeopathic medicines can be given the status of a medicinal product without having to provide valid proof of efficacy. As medicinal products, these preparations may then only be dispensed to customers in pharmacies, which, however, creates an obligation to also supply them on request or prescription. Many pharmacies go far beyond this and advertise homeopathic medicines as a useful therapy option by advertising them prominently in the window. In addition, customers are recommended to use them, corresponding lecture events are supported, and much more. Often, homeopathic preparations are even produced according to pharmacies’ own formulations and marketed under their own name.
For pharmacists and pharmaceutical technical assistants (PTAs) to perform their important task in the proper supply of medicines to the population, they must have successfully completed a scientific study of pharmacy or state-regulated training. This is to ensure that customers are informed and properly advised about their medicines according to the current state of knowledge.
After successfully completing their training or studies, PTAs and pharmacists are undoubtedly able to recognize that homeopathic medicines cannot be effective beyond placebo. They do not have any significant content of active ingredients – if, for example, the high potencies that are considered to be particularly effective still have any active ingredients at all. Consequently, pharmacists and PTAs act against their better knowledge to the detriment of their customers if they create the impression through their actions that homeopathic medicines represent a sensible therapeutic option and customers are thereby encouraged to buy and use them.
Although homeopathics have no potential for direct harm in the absence of relevant amounts of pharmacologically active substances in the preparations, their distribution should nevertheless be viewed critically. The use of homeopathy can mean losing valuable time and delaying the start of effective therapy. It is often accompanied by criticism, even rejection of scientifically oriented medicine and public health, for example when homeopathy is presented as the antithesis to a threatening “pharmaceutical mafia”.
The Münster Circle appeals to pharmacists and PTAs to stop advertising homeopathic medicines as an effective therapeutic option, to stop producing and marketing them themselves, and to advise their customers that homeopathic preparations are not more effective than placebo. The professional organizations of pharmacists and other providers of further training are called upon to no longer offer courses on homeopathy – except for convincingly refuting the often abstruse claims of the supporters.
_______________________
I have pointed out for at least 20 years now that pharmacists have an ethical duty toward their clients. And this duty does not involve misleading them and selling them useless homeopathic remedies. On the contrary, it involves advising them on the basis of the best existing evidence.
When I started writing and talking about this, pharmacists seemed quite interested (or perhaps just amused?). They invited me to give lectures, I published an entire series of articles in the PJ, etc. Of late, they seem to be fed up with hearing this message and the invitations have well and truly stopped.
They may be frustrated with my message – but not as frustrated as I am with their inertia. In my view, it is nothing short of a scandal that homeopathic remedies and similarly bogus treatments still feature in pharmacies across the globe.
This happens with such a regularity that I have decided to write about it; in fact, I shall do that in the form of an ‘open letter‘ to all concerned.
Background
A person or group of persons compose a complaint about my work in which they allege that I am engaged in a decade-long vendetta specifically against their particular form of so-called alternative medicine (SCAM). This letter is sent to me, or to a publisher of my articles/books, or to my peers at the university, or to anyone else they consider appropriate. Such interventions can at times be quite entertaining or even hilariously funny, but if they occur too often, they are also mildly irritating and wasteful. Foremost, they are based on a fundamental misunderstanding that might be worth clearing up with this …
Open Letter
Dear advocate of the specific SCAM in question,
Dear professional organization of the specific SCAM in question,
I am sorry that my lecture/article/blog post/book/interview caused concern and led you to feel that I am running a long-term campaign or vendetta against the specific SCAM that you advocate. This letter is to assure you that your feeling is entirely erroneous: I am in no way targeting your specific SCAM.
If you have a look at my most recent book, for instance, you will see that, in it, I discuss a total of 202 different forms of SCAM and that – with good reason – I am highly critical of the vast majority of these methods. Imagine what it would mean to run a vendetta or campaign against all of these specific SCAMs. I would need a sizable team of co-workers involving lawyers, researchers, administrators, etc. to manage the task. I would also need plenty of funds to support the campaign, and I would most likely have more legal cases going than I have hair on my head.
The truth is that, since my retirement ~10 years ago, I do my research with no assistance whatsoever, I get no financial support or compensation for my work, and I am in contact with lawyers only when they ask me to serve as an expert witness. There simply is no evidence for the campaign that you feel does exist and you evidently misjudge my motives for criticizing your specific SCAM.
My aim is not to defame your specific SCAM or SCAM in general. I have no reason to do this. My aim is simply to inform the public responsibly and to prevent vulnerable people from getting harmed or ripped off. As I have studied the subject systematically for three decades, I feel I am competent, entitles, and duty-bound to try and do this.
I sincerely hope you are able to see the difference: you seem to think that I am destructively out to get you or your SCAM, while in truth I am constructively doing what responsible healthcare professionals (should) do.
Now that this misunderstanding has been cleared up, I thank you for reconsidering your position and stopping to claim things about me that are not true.
Best regards
Edzard Ernst