progress
I was asked by NATURE to provide a comment on the WHO Traditional Medicine Global Summit: Towards health and well-being for all which is about to take place in India:
The First WHO Traditional Medicine Global Summit will take place on 17 and 18 August 2023 in Gandhinagar, Gujarat, India. It will be held alongside the G20 health ministerial meeting, to mobilize political commitment and evidence-based action on traditional medicine, which is a first port of call for millions of people worldwide to address their health and well-being needs.
The Global Summit will be co-hosted by WHO and the Government of India, which holds the presidency of the G20 in 2023. It will be a platform for all stakeholders, including traditional medicine workers, users and communities, national policymakers, international organizations, academics, private sector and civil society organizations, to share best practices and game-changing evidence, data and innovation on the contribution of traditional medicine to health and sustainable development.
For centuries, traditional and complementary medicine has been an integral resource for health in households and communities. It has been at the frontiers of medicine and science laying the foundation for conventional medical texts. Around 40% of pharmaceutical products today have a natural product basis, and landmark drugs derive from traditional medicine, including aspirin, artemisinin, and childhood cancer treatments. New research, including on genomics and artificial intelligence are entering the field, and there are growing industries for herbal medicines, natural products, health, wellness and related travel. Currently, 170 Member States reported to WHO on the use of traditional medicine and have requested evidence and data to inform policies, standards and regulation for its safe, cost-effective and equitable use.
In response to this increased global interest and demand, WHO, with the support of the Government of India, established in March 2022 the WHO Global Centre for Traditional Medicine as a knowledge hub with a mission to catalyse ancient wisdom and modern science for the health and well-being of people and the planet. The WHO Traditional Medicine Centre scales up WHO’s existing capacity in traditional medicine and supplements the core WHO functions of governance, norms and country support carried out across the six regional Offices and Headquarters.
The Centre focuses on partnership, evidence, data, biodiversity and innovation to optimize the contribution of traditional medicine to global health, universal health coverage, and sustainable development, and is also guided by respect for local heritages, resources and rights.
A cross-regional expert panel will advise on the Summit’s theme, format, topics and issues to address. All updates will be posted here and on the forthcoming webpages for the First WHO Traditional Medicine Global Summit.
In case you are interested, the programme can be seen here.
And my comment? I am afraid, it was not very encouraging. I doubt that Nature will publish it in full. So, allow me to show you my unabridged comment:
We discussed the 2015 Australian NHMRC report on homeopathy many times before, e.g.:
- Homeopathy: the 2015 NHMRC report and its criticism re-analysed
- HOMEOPATHY: the NHMRC report revisited
- Ombudsman investigates ‘flawed’ homeopathic study
- The final verdict on homeopathy: it’s a placebo
In a nutshell, the report was an hugely influential analysis of the effectiveness of homeopathy which came to squarely negative conclusions. Thus it was celebrated as a thorough and conclusive piece evidence demonstrating the madness of homeopathy. Unsurprisingly, homeopaths did not like it at all and produced various criticisms claiming that it was neither thorough nor conclusive.
Now the final evaluation of what has been going on was finally published (ISSUED BY THE COMMONWEALTH OMBUDSMAN, IAIN ANDERSON, ON 4 AUGUST 2023):
The Office of the Commonwealth Ombudsman (the Office) has finalised an investigation relating to the National Health and Medical Research Council’s (NHMRC) review of the evidence for the effectiveness of homeopathy, conducted between 2010 and 2015. We commenced this investigation in September 2017 in response to concerns raised with us about how the NHMRC review had proceeded.
The Office conducts its investigations in private, and the Ombudsman generally does not make a public statement in the absence of a formal report. In the circumstances of this matter, including that the then-Ombudsman released a public statement on 4 June 2021 which acknowledged the Office was investigating, we believe it is important to share publicly the information we can, now that the investigation is complete.
Our investigation was finalised in July 2023. We acknowledge the length of time the investigation has taken. This is in part due to the extensive efforts the Office made to source independent scientific expertise to advise us on some detailed and specific questions of scientific methodology that were raised with our Office, including some that were only brought to our attention as our investigation progressed. Despite our best efforts, it was not possible to engage an expert (or experts) to provide independent advice to our Office on this subject. In the absence of independent, expert scientific expertise we have not been able to conclusively determine those matters of scientific methodology. This did not prevent our Office from forming a view on other aspects of the matter.
Our investigation did not result in any adverse findings about the review or the NHMRC. When finalising investigations, we may offer comments and suggestions to an agency about areas for future improvement. In this instance, we offered comments and suggestions to the NHMRC about how it records and publicly explains decisions about its activities. The NHMRC also independently made several improvements to its processes during the course of our investigation.
________________
In essence, this means that the conclusions of the report stand:
Homeopathy should not be used to treat health conditions that are chronic, serious, or could become serious. People who choose homeopathy may put their health at risk if they reject or delay treatments for which there is good evidence for safety and effectiveness. People who are considering whether to use homeopathy should first get advice from a registered health practitioner. Those who use homeopathy should tell their health practitioner and should keep taking any prescribed treatments.
Thus the matter is closed – that is closed for rational thinkers. For irrationalists, the matter will no doubt continue to be a stone of contention. No, homeopath will be able to accept these conclusions simply because a member of a cult ceases to be a cultist once he/she accepts the criticism agaist the cult.
We have discussed dental amalgam and its risks to human health before. Finally, there is new legislation in sight. The European Commission has revised the EU Mercury Regulation to protect EU citizens and the environment from toxic mercury. Among other things, this will completely ban the use of dental amalgam, for which 40 tons of mercury are currently consumed annually in the EU. The revised mercury ordinance provides for the following:
– No more use of dental amalgam from January 1, 2025; viable mercury-free alternatives are available.
– Ban on the manufacture and export of dental amalgam from the EU from January 1, 2025;
– Ban on the manufacture and export of six mercury-containing lamps from January 1, 2026 and January 1, 2028 (depending on lamp type).
The delegated act adopted under the Mercury Regulation transposes into EU law the decisions taken at the fourth Conference of the Parties (2022) to the Minamata Convention by introducing a ban on the production, import, and export of eight additional mercury-containing products, including mercury-containing lamps and non-electrical equipment.
The Minamata Convention is the main international legal framework for the protection of human health and the environment from anthropogenic emissions and releases of mercury to air, water, and soil. Like the Mercury Regulation, it addresses the entire life cycle of mercury, from primary mercury mining to mercury waste management.
The revised Mercury Regulation must now be approved by the European Parliament and the Council under the ordinary legislative procedure. The delegated act will be sent to the European Parliament and the Council for consideration.
Mercury is a highly toxic chemical that poses a threat to both human health and the environment. When released into the environment, it enters the food chain where it accumulates (mainly in fish). High mercury exposure can damage the brain, lungs, kidneys, and immune system.
Historically, mercury has been used in a wide range of applications, including gold mining, batteries, fluorescent tubes, thermometers, and barometers. Over the last twenty years, the EU has developed a comprehensive body of legislation, in particular the Mercury Regulation, which protects human health and the environment from anthropogenic emissions and releases of mercury, taking into account the entire life cycle of mercury from primary mercury mining to final disposal of mercury waste. It also includes measures on trade in mercury-containing products and mercury pollution.
The Minamata Convention entered into force on August 16, 2017, and has so far been ratified by the European Union and 143 countries, including all EU Member States. The fifth session of the Conference of the Parties to the Minamata Convention on Mercury (COP-5) will be held in Geneva, Switzerland, from October 30 to November 3, 2023.
_____________________________
In the UK – this post is mainly for UK readers – journalists and opinion leaders are currently falling over themselves reporting about a major breakthrough: an Alzheimer’s drug has been shown to slow the disease by around 36%. “After 20 years with no new Alzheimer’s disease drugs in the UK, we now have two potential new drugs in 12 just months,” wrote Dr Richard Oakley, associate director at the Alzheimer’s Society. And the Daily Mail headlined: “New drug which claims to slow mental decline caused by Alzheimer’s by 36% could spell ‘the beginning of the end’ for the degenerative brain disease”.
That’s excellent news!
Many people will have made a sigh of relief!
So, why does it make me angry?
Once we listen to the news more closely we learn that:
- the drug only works for patients who are diagnosed early;
- for an early diagnosis, we need a PET scan;
- the UK hardly has any PET scanners, in fact, we have the lowest number among developed countries;
- these scanners are very expensive;
- the costs for the new drug are as yet unknown but will also be high.
Collectively these facts mean that we have a major advance in healthcare that could help many patients. At the same time, we all know that this is mere theory and that the practice will be very different.
Why?
- Because the NHS has been run down and is on its knees.
- Because our government will again say that they have invested xy millions into this area.
- The statement might be true or not, but in any case, the funds will be far too little.
- The UK has become a country where some patients suffering from severe toothache currently resort to pulling out their own teeth at home with pairs of pliers.
- In the foreseeable future, the NHS will not be allocated the money to invest in sufficient numbers of PET scans (not to mention the funds to buy the new and expensive drug).
In other words, the UK celebrates yet another medical advance raising many people’s expectations, while everyone in the know is well aware of the fact that the UK public will not benefit from it.
Does that not make you angry too?
It been reported that the German HEILPRAKTIKER, Holger G. has been sentenced to serve a total of 4 years and three months behind bars. He made himself a pair of glasses out of aluminum foil and appeared at the start of his trial wearing a Corona protective mask. The accusations against him were fierce: He was accused of having issued false Corona vaccination certificates en masse in Munich and of having given medication to patients. A woman, who had contracted Corona and had been treated by Holger G. with vitamin solutions, had died last year.
According to the verdict, Holger G. had violated the German Medicines Act. The court announced he was also convicted of 96 counts of dangerous bodily harm and 102 counts of unauthorized trading in prescription drugs. In addition, the court ordered the HEILPRAKTIKER to be placed in a rehab facility.
The 71-year-old MAN had issued Corona vaccination cards since April 2021, without actually vaccinating the people concerned. For the forged vaccination cards, he charged several tens of thousands of Euros. In addition, the former HEILPRAKTIKER illegally sold prescription drugs. The judgment is so severe because Holger G. has form. He also ordered to bear the costs of the proceedings.
___________________________
I have long criticized the German HEILPRAKTIKER. In my recent book on the subject, I make the following points:
– Today, no one can provide reliable data on the number of HEILPRAKTIKER in Germany.
– The training of HEILPRAKTIKER is woefully inadequate.
– The far-reaching rights of the HEILPRAKTIKER are out of proportion to their overt lack of competence.
– This disproportion poses a serious danger to patients.
– This danger is further increased by the fact that there is no effective control of the activity of the HEILPRAKTIKER does not take place.
– Existing laws are almost never applied to the HEILPRAKTIKER.
– Most HEILPRAKTIKER mislead the public unhindered with untenable therapeutic claims.
– The federal government seems to put off over and over again any serious discussion of the HEILPRAKTIKER.
Cases like the one above show that it is high time for reform – or, should that prove impossible, the discontinuation of this utterly obsolete and highly dangerous profession.
“We are hugely concerned about the welfare of doctors and healthcare workers with long COVID”. These are the first words of a comprehensive survey of UK doctors with post-acute COVID health complications. It reveals that these doctors experience symptoms such as:
- fatigue,
- headaches,
- muscular pain,
- nerve damage,
- joint pain,
- respiratory problems.
Around 60% of doctors said that post-acute COVID ill health has affected their ability to carry out day-to-day activities on a regular basis. 18% reported that they were now unable to work due to their post-acute COVID ill-health, and only 31% said they were working full-time, compared with more than half before the onset of their illness.
The report demands financial support for doctors and healthcare staff with post-acute COVID, post-acute COVID to be recognized as an occupational disease in healthcare workers, with a definition that covers all of the debilitating disease’s symptoms and for improved access to physical and mental health services to aid comprehensive assessment, appropriate investigations and treatment. The report also calls for greater workplace protection for healthcare staff risking their lives for others and better support for post-acute COVID sufferers to return to work safely if they can, including a flexible approach to the use of workplace adjustments.
In November 2021, an online survey investigating the emotional states of depression, anxiety, stress, compassion satisfaction, and compassion fatigue was administered to 78 Italian healthcare workers (HCWs). Between 5 and 20% of the cohort showed the effects of the adverse psychological impact of the pandemic and more than half of them experienced medium levels of compassion fatigue as well as a medium level of compassion satisfaction. The results also show that those with fewer years of clinical practice might be at greater risk of burnout, anxiety, and stress symptoms and might develop a lower level of compassion satisfaction. Moreover, the factors that potentially contribute to poor mental health, compassion fatigue, and compassion satisfaction seem to differ between residents and specialist physicians.
A cross-sectional study was conducted from September 2021 to April 2022 and targeted all physicians working at King Fahd Hospital of the University, Al Khobar, Saudi Arabia. Patient Health Questionnaire-9 and General Anxiety Disorder-7 were used to elicit self-reported data regarding depression and anxiety, respectively. In addition, sociodemographic and job-related data were collected. A total of 438 physicians responded, of which 200 (45.7%) reported symptoms of depression and 190 (43.4%) of anxiety. Being aged 25-30 years, female, resident, and reporting a reduction in work quality were factors significantly associated with both anxiety and depression. Female gender (AOR = 3.570; 95% CI = 2.283-5.582; P < 0.001), working an average 9-11 hours/day (AOR = 2.130; 95% CI = 1.009-4.495; P < 0.047), and self-perceived reduction in work quality (AOR = 3.139; 95% CI = 2.047-4.813; P < 0.001) were significant independent predictors of anxiety. Female gender (AOR = 2.929; 95% CI = 1.845-4.649; P < 0.001) and self-perceived reduction in work quality (AOR = 3.141; 95% CI = 2.053-4.804; P < 0.001) were significant independent predictors of depression.
An observational, multicenter cross-sectional study was conducted at eight tertiary care centers in India. The consenting participants were HCWs between 12 and 52 weeks post-discharge after COVID-19 infection. The mean age of the 679 eligible participants was 31.49 ± 9.54 years. The overall prevalence of COVID sequelae was 30.34%, with fatigue (11.5%) being the most common followed by insomnia (8.5%), difficulty in breathing during activity (6%), and pain in joints (5%). The odds of having any sequelae were significantly higher among participants who had moderate to severe COVID-19 (OR 6.51; 95% CI 3.46-12.23) and lower among males (OR 0.55; 95% CI 0.39-0.76). Besides these, other predictors for having sequelae were age (≥45 years), presence of any comorbidity (especially hypertension and asthma), category of HCW (non-doctors vs doctors), and hospitalization due to COVID-19.
Such data are scary. Not only will we have a tsunami of long-Covid patients from the general public, and not only do we currently lack effective causal treatments for the condition, but also is the number of HCWs who are supposed to deal with all this drastically reduced.
Most if not all countries are going to be affected by these issues. But the UK public might suffer the most, I fear. The reasons are obvious if you read a previous post of mine: in the UK, we have significantly fewer doctors, nurses, hospital beds, and funding (as well as politicians who care and would be able to do something about the problem) than in other comparable countries. To me, this looks like the emergence of a perfect storm.
Yesterday, the NHS turned 75, and virtually all the newspapers have joined in the chorus singing its praise.
RIGHTLY SO!
The idea of nationalized healthcare free for all at the point of delivery is undoubtedly a good one. I’d even say that, for a civilized country, it is an essential concept. The notion that an individual who had the misfortune to fall ill might have to ruin his/her livelihood to get treated is absurd and obscene to me.
The NHS was created the same year that I was born. Even though I did not grow up in the UK, I cannot imagine a healthcare system where people have to pay to get or stay healthy. To me, ‘free’ – it is, of course not free at all but merely free at the point of delivery – is a human right just as freedom of speech or the right to a good education.
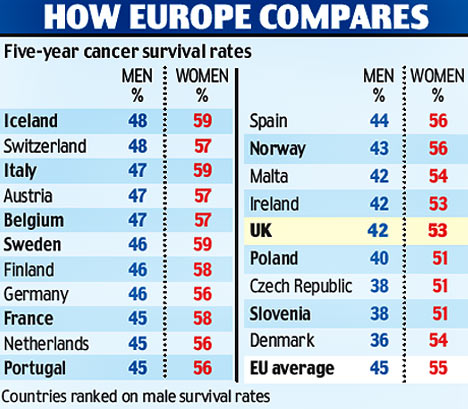
 While reading some of what has been written about the NHS’s 75th birthday, I came across more platitudes than I care to remember. Yes, we are all ever so proud of the NHS but we would be even more proud if our NHS did work adequately. I find it somewhat hypocritical to sing the praise of a system that is clearly not functioning nearly as well as that of comparable European countries (where patients also don’t have to pay out of their own pocket for healthcare). I also find it sickening to listen to politicians paying lip service, while doing little to fundamentally change things. And I find it enraging to see how the conservatives have systematically under-funded the NHS, while pretending to support it adequately.
While reading some of what has been written about the NHS’s 75th birthday, I came across more platitudes than I care to remember. Yes, we are all ever so proud of the NHS but we would be even more proud if our NHS did work adequately. I find it somewhat hypocritical to sing the praise of a system that is clearly not functioning nearly as well as that of comparable European countries (where patients also don’t have to pay out of their own pocket for healthcare). I also find it sickening to listen to politicians paying lip service, while doing little to fundamentally change things. And I find it enraging to see how the conservatives have systematically under-funded the NHS, while pretending to support it adequately.
How can we be truly proud of the NHS when it seems to be dying a slow and agonizing death due to political neglect? In the UK, politicians like to be ‘world beating’ with everything, and I am sure some Tories want you to believe that, under their leadership, a world-beating healthcare system has been established in the UK.
Let me tell you: it’s not true. I have personal experience with the healthcare systems of 5 different nations and worked as a doctor in 3 of them. In Austria, France, and Germany for instance, the system is significantly better and no patient’s finances are ruined through illness.
Now there is talk about reform – yet again! Let us please not look towards the US when thinking of reforming the NHS. I have lived for a while in America and can tell you one thing: when it comes to healthcare, the US is not a civilized country. If reform of the NHS is again on the cards, let us please look towards the more civilized parts of the world!
This analysis was aimed at quantifying how many studies registered on the Open Science Framework (OSF) up to November 2017 are performed but not shared after at least 4 years. Examining a sample of 315 registrations, of which 169 were research studies, the researchers found that 104 (62%) were published. They estimated that 5550 out of 9544 (58%) registered studies on the OSF are published.
Researchers use registries to make unpublished studies public, and the OSF policy to open registrations after a four-year embargo substantially increases the number of studies that become known to the scientific community. In responses to emails asking researchers why studies remained unpublished logistical issues (e.g., lack of time, researchers changing jobs) were the most common cause, followed by null results, and rejections during peer review.
The authors concluded that their study shows that a substantial amount of studies researchers perform remain unpublished.
I find this truly shocking!
Researchers are able to do research only because they receive financial and other support from elsewhere. Therefore they have an ethical obligation to publish it. The reasons frequently given for not publishing research are nothing well and truly invalid:
- Lack of time is a mere excuse; if researchers had the time to get the grants, permissions, etc. they simply must have the time to finish the job properly.
- Researchers changing jobs is an equally flawed excuse; if someone changes position, he/she is obliged to finish the job they were doing. A surgeon can also not leave mid-surgery because he has a better offer.
- ‘Null results’ is even worse as a reason. Null results are just as important as positive findings – occasionally they are even more important. If researchers fail to realize this, they simply disqualify themselves as researchers.
- ‘Rejections during peer review’ is complete nonsense. Everyone who submits papers for publication gets rejected once in a while. In this case, one learns from the peer-review comments, improves the paper in question, and re-submits it to another journal.
I have seen many studies of so-called alternative medicine (SCAM) that, for this or that reason, never were published. And I feel strongly that this is a serious violation of research ethics – so much so that I would ban researchers who are guilty of this crime from conducting research in the future. I also feel that, in order to receive the necessary support (financial and other), researchers should sign that they will publish their findings within a given time after finishing their study. Failing to comply could then incur a penalty such as paying back part of the funds wasted. I think such measures would very quickly clear up the current intolerable situation.
Enthusiasts of so-called alternative medicine (SCAM) sometimes remind me of the French philosopher, Blaire Pascal, and his famous wager. Blaise Pascal (1623-1662) argued that, because it is impossible to either prove or disprove the existence of God, it would probably be best to wager in favor of his existence. In case one got it wrong, little would be lost; in case one was correct, everything was gained.
Likewise, enthusiasts of SCAM often argue that, because of the lack of evidence for many SCAMs, one cannot be sure whether they work or not. Thus it would probably be best to wager in favor of SCAM and make use of it. In case one got it wrong, little would be lost; in case one was correct, everything was gained.
This line of thinking is common and, at first glance, it seems to be “a safe bet”. However, once we analyze it critically, it quickly falls apart. To explain, it might be best to choose a concrete example. Let’s assume, therefore, that we are talking about a cancer patient who wants to leave no stone unturned to cure her cancer.
So, she goes on the Internet and does her ‘research’. As soon as she has found a SCAM that might suit her, another one crops up, and then another, and then dozens. Which SCAM should she use? There are hundreds of SCAM cancer “cures” being promoted to the unsuspecting and vulnerable. Since one is as unproven as the next, our patient has a hard time deciding which SCAM to try. Applying all simultaneously or consecutively would be “betting on the safe side,” but is not a realistic option. If nothing else, it would be an unaffordable full-time job.
A further flaw in Pascal’s approach to SCAM relates to the fact that we are unable to prove the existence of God, but scientists are entirely capable of finding out about SCAM and its effects on cancer patients. After all, that’s what clinical trials are designed for. If for a particular SCAM, no studies are available (which is often the case), it probably means that it is not worth the effort of testing the claims that are being made for it. SCAM cancer cures are ‘alternatives’ for one main reason: they are implausible, so much so that the chances of them doing more good than harm usually approach zero.
And there is yet another caveat: while accepting the existence of God might be not associated with major harm (I know, some people would dispute this), many SCAMs are by no means free of risks. Therefore it is simply not true to assume that “little is lost” in case they do not work.
Direct harm can occur through the interactions of some form of SCAM with prescription drugs, for instance. But the potential for indirect harm is much more important. Here the risks range from raising false hopes or financial exploitation to undermining rationality in a much more general sense. By far the biggest indirect risk is that SCAM is used as a replacement for effective treatments. Most patients do not approach SCAM to give up conventional medicine entirely. But SCAM practitioners can be most persuasive, and some over-enthusiastic SCAM therapists do try to convince their patients to abandon life-saving treatments.
Pascal’s wager was disputed when it was first published. As a result of the ensuing discussions, significant advances were made, for instance, in the area of probability theory. Applying Pascal’s wager to SCAM, as many enthusiasts do, is however a very different matter. I am afraid, the benefits of doing so might not outweigh the risks.
This survey evaluated the attitude of healthcare professionals toward the use of so-called alternative medicine (SCAM) to improve current care. A questionnaire on the current practice and opinions about SCAM use was sent to healthcare professionals in Amsterdam UMC, who work for the department of hematology or oncology. Oncologists, hematologists, residents, (specialized) nurses, dieticians, (hospital)pharmacists, and pharmacy technicians were asked to participate.
Among eligible healthcare professionals, 77 responded to the questionnaire (34%). Overall, 87% of healthcare
professionals indicated it is important to be aware of their patient’s SCAM use, and all find the potential of drug–herb interactions important. However, more than half of the healthcare professionals inquire about the patient’s SCAM use infrequently. In addition, only 15% of the healthcare professionals stated they had sufficient knowledge of SCAM to advise patients on their use of SCAM.
The authors concluded that healthcare professionals are aware of the potential risks of SCAM use in combination with anti-cancer treatment. However, SCAM use is not yet discussed with every patient. This may be due to healthcare professionals’ lack of knowledge about SCAM.
This survey would in itself be fairly irrelevant; it employed only a tiny convenience sample and its findings cannot be generalized. Yet, it produced results that have been shown dozens of times before, and it might therefore be a good idea to remind ourselves of their relevance and implications.
- Patients use SCAM whether we want it or not.
- Contrary to what is often said, SCAM is not harmless.
- Therefore conventional healthcare professionals need to know about their patients’ SCAM use.
- To find out, healthcare professionals need to ask specific questions about SCAM.
- Next, they must advise their patients responsibly (this is an ethical obligation, not a choice).
- In order to do that they need to learn the essentials about SCAM.
- Failing to do this means failing their patients.




