placebo
This study aimed to evaluate the efficacy of Persian barley water in controlling the clinical outcomes of hospitalized COVID-19 patients. It was designed as a single-blind, add-on therapy, randomized controlled clinical trial and conducted in Shiraz, Iran, from January to March 2021. One hundred hospitalized COVID-19 patients with moderate disease severity were randomly allocated to receive routine treatment (per local protocols) with or without 250 ml of Persian barley water (PBW) daily for two weeks. Clinical outcomes and blood tests were recorded before and after the study period. Multivariable modeling was applied using Stata software for data analysis.
The length of hospital stay (LHS) was 4.5 days shorter in the intervention group than the control group regardless of history of cigarette smoking (95% confidence interval: -7.22, -1.79 days). Also, body temperature, erythrocyte sedimentation rate (ESR), C-reactive protein (CRP), and creatinine significantly dropped in the intervention group compared to the control group. No adverse events related to PBW occurred.
The authors from the Department of Traditional Medicine, Shiraz University of Medical Sciences, Shiraz, Iran, concluded that this clinical trial demonstrated the efficacy of PBW in minimizing the LHS, fever, and levels of ESR, CRP, and creatinine among hospitalized COVID-19 patients with moderate disease severity. More robust trials can help find safe and effective herbal formulations as treatments for COVID-19.
I must admit, I did not know about PBW. The authors explain that PBW is manufactured from Hordeum vulgare via a specific procedure. According to recent studies, barley is rich in constituents such as selenium, tocotrienols, phytic acid, catechin, lutein, vitamin E, and vitamin C; these compounds are responsible for their antioxidant and anti-inflammatory properties. Barley grains also have immune-stimulating effects, antioxidant properties, protective effects on the liver and digestive systems, anti-cancer effects, and act to reduce uric acid levels.
But even if these effects would constitute a plausible mechanism for explaining the observed effects (which I do not think they do), the study itself is more than flimsy.
I do not understand why researchers investigating an important issue do not make sure that their study is as rigorous as possible.
- Why not use an adequately large sample size?
- Why not employ a placebo?
- Why not double-blind?
- Why not report the most important outcome, i.e. mortality?
As it stands, nobody will take this study seriously. Perhaps this is a good thing – but perhaps PBW does have positive effects (I know it’s a long shot) and, in this case, a poor-quality study would only prevent an effective therapy come to light.
Placebo effects are a fascinating subject. In so-called alternative medicine (SCAM), they are particularly important because much of SCAM seems to rely on little more than placebo effects. Therefore, I think this new paper is of some relevance to us.
The aim of this systematic review was to quantify the placebo effect of intraarticular injections for knee osteoarthritis in terms of pain, function, and objective outcomes. Factors influencing placebo effect were investigated.
Out of 2,363 records, 50 articles on 4,076 patients were included. The meta-analysis showed significant improvements up to the 6-month follow-up: Visual Analogue Scale (VAS)-pain −13.4 mean difference (MD) (95% confidence interval [CI]: −21.7/−5.1; P < 0.001), Western Ontario and McMaster Osteoarthritis Index (WOMAC)-pain −3.3 MD (95% CI: −3.9/−2.7; P < 0.001). Other significant improvements were WOMAC-stiffness −1.1 MD (95% CI: −1.6/−0.6; P < 0.001), WOMAC-function −10.1 MD (95% CI: −12.2/−8.0; P < 0.001), and Evaluator Global Assessment −21.4 MD (95% CI: −29.2/−13.6; P < 0.001). The responder rate was 52% (95% CI: 40% to 63%). Improvements were greater than the “minimal clinically important difference” for all outcomes (except 6-month VAS-pain). The level of evidence was moderate for almost all outcomes.
The authors concluded that the placebo effect of knee injections is significant, with functional improvements lasting even longer than those reported for pain perception. The high, long-lasting, and heterogeneous effects on the scales commonly used in clinical trials further highlight that the impact of placebo should not be overlooked in the research on and management of knee osteoarthritis.
The authors furthermore confirmed that “the main finding of this meta-analysis is that placebo is an important component of the effect of injective treatments for patients with KOA, with saline injections being able to provide relevant and long-lasting results not only in terms of pain relief but also with respect to stiffness resolution and function improvement. These results are both statistically and clinically significant and can be perceived by patients up to 6 months.”
I would dispute that!
To explain why it might help to read our 1995 BMJ paper on the subject:
We often and wrongly equate the response seen in the placebo arm of a clinical trial with the placebo effect. In order to obtain the true placebo effect, other non-specific effects can be identified by including an untreated control group in clinical trials. A review of the literature shows that most authors confuse the perceived placebo effect with the true placebo effect. The true placebo effect is highly variable, depending on several factors that are not fully understood. A distinction between the perceived and the true placebo effects would be helpful in understanding the complex phenomena involved in a placebo response.
In other words, what the authors picked up in their analysis (i.e. the changes that occurred in the placebo groups between the start of a trial and after placebo application) is not just the placebo response; it is, in fact, a combination of a placebo effect, concomitant interventions/care, regression towards the mean, natural history of the condition and possibly other factors.
Does it matter?
Yes, it does!
Placebo effects are not nearly as powerful and long-lasting as the authors conclude. And this means virtually all their implications for clinical practice are incorrect.
Third molar extraction is a painful treatment and thus is often used to investigate the effects of analgesics on pain. Hypnotherapy is said to help to reduce pain and to decrease the intake of postoperative systemic analgesics. Therefore, it seems reasonable to study the effects of hypnotherapy on the pain caused by third molar extraction.
In this study, the effectiveness of a brief hypnotic induction for patients undergoing third molar extractions was investigated. Data were collected from 33 patients with third molar extractions on the right and left sides. Patients received two different types of interventions in this monocentric randomized crossover trial. Third molar extraction was conducted on one side with reduced preoperative local anesthetics and an additional brief hypnotic induction (Dave Elman technique). The other side was conducted with regular preoperative local anesthetics without a brief hypnotic induction (standard care). Intake of postoperative systemic analgesics was allowed in both treatments.
Patients’ expectations about hypnosis were assessed at baseline. The primary outcome was the area under the curve with respect to ground of pain intensity after the treatment. Secondary outcomes were the amount of postoperative analgesics consumed and the preferred treatment.
There was no evidence that the area under the curve with respect to ground of pain differed between the two interventions (controlling for gender). There was, however, evidence to show that the patients’ expectations affected the effectiveness of the brief hypnotic induction. This means that patients with high expectations about hypnosis benefit more from treatment with reduced preoperative local anesthetics and additional brief hypnotic induction.
The authors concluded that, in this study, additional a brief hypnotic induction with reduced preoperative local anesthetic use did not generally reduce posttreatment pain after third molar extraction more than regular local anesthetics. The expectation of the patients about the effectiveness of hypnosis affected the effectiveness of the brief hypnotic induction so that patients with high expectations had a larger benefit from a brief hypnotic induction than patients with low expectations.
The most interesting findings here are, in my view, that:
- Hypnotherapy is not as effective as many enthusiasts claim.
- Expectation influences the outcome of hypnotherapy.
Expectation is, of course, a determinant of the size of the placebo response. Thus, this finding is interesting but far from unexpected. I would go as far as postulating that similar results would be obtained with most treatments regardless of whether they are alternative or conventional. The difference is that, in the case of alternative therapies, the expectation is a major (if not the only) determinant of the outcome, while it merely somewhat improves the outcome of an effective treatment. To put it differently, so-called alternative medicine (SCAM) relies entirely/mostly on expectation, while conventional medicine does not.
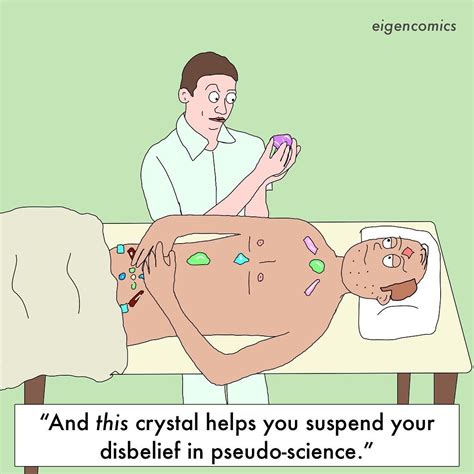
Crystal healing is the treatment of all types of illnesses via the ‘healing energy’ of gemstones. It is as implausible as so-called alternative medicine (SCAM) gets. In my recent analysis of 150 SCAMs, I concluded that “there are no rigorous trials testing the therapeutic value of crystal healing”. This assumption is further confirmed by published papers like this one: 
Recently, crystal healing and gemstone therapy, also known as litho- or gemmotherapy, is extensively promoted in the media, newspapers and the internet. There is also a growing interest of cancer patients in this unconventional treatment, resulting in the need for oncologists to give informed advice to their patients and to prevent them from wasting hope, time and money in an ineffective treatment, and at worst to postpone the necessary treatment of this life threatening disease. In the context of the currently ever-growing New-Age wave, believing in crystal healing has spread widely in the population. It is a historical belief similar to that of charmstones, rather than one based on modern scientific practices and advances. Pleasant feelings or seeming successes of crystal healing can be attributed to the strong placebo effect, or the believers wanting it to be true and seeing only things that back that up: cognitive bias. A scientific proof of any positive effect beyond a placebo effect does not exist. Even though this treatment can be generally regarded as harmless and without toxicity, it should not be recommended to cancer patients. Thereby we will help prevent our patients from wasting hope, time and money in an ineffective treatment, and at worst to postpone the necessary treatment of this life threatening disease, resulting in a worsened prognosis.
Yet, it seems that we were not entirely correct. Recently, I came across an article that mentions such a study:
A study conducted in 2001 by British psychologist Christopher French challenged 80 volunteers to differentiate between real and fake crystals after holding them in their hands for five minutes and meditating. Six people felt nothing at all, and the rest reported feeling some energy, whether in the form of tingling in the body or an improved sense of wellbeing. Both groups, though—whether holding the fake crystals or the real ones—reported similar impressions, suggesting the placebo effect could be at play.
“When scientists conduct robust clinical trials, they want to strip the intervention of these placebo effects to figure out if it has a specific benefit,” Jarry explains. “Alternative medicine’s reputation benefits strongly from these non-specific placebo effects. Enough people will start to feel better after using crystals (because of regression to the mean, self-limiting illness, misremembering, etc.), and they will publicly testify to their improvement, giving the illusion that crystals work. What they don’t know is what would have happened had they not used the crystals.”
So, if you want to keep a hunk of amethyst at your desk to alleviate your grief, or a Tiger’s Eye stone to clear the mind, go ahead: they may not be manipulating a sacred energy field around your body to heal you, but they can certainly manipulate your mind.
Unfortunately, the link provided does not lead directly to the study but to the publication list of Chris French. This in turn leads us to the reference in question:
French, C. C., O’Donnell, H., & Williams, L. (2001). Hypnotic susceptibility, paranormal belief and reports of ‘crystal power’. British Psychological Society Centenary Annual Conference, Glasgow, 28-31 March 2001. (Abstract published in Proceedings of the British Psychological Society, 9(2), 186).
Sadly, I cannot find the paper online and I suspect it exists only as an abstract in a conference book (I have emailed Chris and asked him). In any case, his study did not test the therapeutic value; so, my above statement is not entirely false.
Prof. Fabricio Benedetti is one of the world’s leading experts in the study of placebo effects. I have mentioned his excellent work before, for instance, here where he cautioned that quackery has today one more weapon on its side, which is paradoxically represented by the hard science–supported placebo mechanisms. Now he has expressed his concerns even more clearly in an article entitled “Alternative and natural medicine quackery is on the rise. Here’s why the placebo effect is part of the problem”. Here are a few excerpts from this excellent paper:
For several decades now, many scientists, including me, have been working hard to reveal the full power and scope of the placebo effect — the amazing ability of a simple sugar pill or other non-pharmaceutical “fake intervention” to improve someone’s quality of life. This research has been crucial to giving scientific credibility to a powerful psychological effect. But the advances of science have also backfired, spawning an alternative industry that preys on the vulnerable…
All this means that some alternative medicines can indeed have positive outcomes for patients, though not necessarily through the mechanisms that the therapy’s inventors supposed, but rather through a placebo effect. This holds true for treatments ranging from strange talismans to acupuncture — studies have shown that pain relief is about the same for patients receiving true acupuncture with needles, for example, as for those receiving sham acupuncture with trick needles.
The scientific advances in understanding placebo are fascinating. But one unfortunate outcome of all this work is that profit-seeking companies and individuals now have a new weapon: It is no longer necessary to demonstrate the effectiveness of their proposed therapies; it is enough to assert that these work because of the placebo effect. I receive myriad eccentric proposals for new therapies, ranging from talismans and concoctions to mascots and weird rituals. Their inventors claim that these are capable of inducing substantial health benefits and often seek my endorsement. These proposals have stepped up sharply in recent years. Sadly, the science of the placebo effect is fueling this new breed of pseudoscience…
So, if a salesperson says: “This concoction (or ritual or talisman) will reduce your pain,” it is not necessarily a lie, as the placebo effect may indeed stimulate pain-relieving circuits in the brain. But anyone could truthfully use these words, within limits.
These marketers often overstate the size of the possible response, claim to provide a “cure” rather than pain relief or incorrectly suggest that only their own expensive products will have this effect. Even worse, they may present the products as an alternative to more effective traditional medications for serious conditions such as cancer. In other words, they prey on the vulnerable by making undeliverable promises, purportedly backed by the science of placebo.
Even if taking a placebo can reduce symptoms such as pain, this isn’t always the best course of action. An apparently trivial pain may, for example, be the first sign of something far more serious. Treating the pain alone may prevent diagnosis by a physician or delay important medical treatments…
…Education, communication and honesty are the best friends of medical practice. Patients and health care professionals deserve to know what placebos can and cannot do.
The research and medical communities must be more transparent about the efficacy of many conventional pharmacological and nonpharmacological treatments, by acknowledging that some of them are useful whereas some others are not. Many over-the-counter products have doubtful efficacy, for example. Honesty will boost patients’ trust and confidence in medicine, which are the best antidotes to quackery.
BRAVO PROF BENEDETTI!
Two million people in UK are estimated to be currently suffering from long COVID, says the Office for National Statistics. Fatigue continues to be the most common symptom – experienced by 55% of those with self-reported long COVID – followed by 32% with shortness of breath, 23% with a cough, and 23% with muscle ache. The problem is only going to increase in the near future. Thus, many people are frantically looking for an effective therapy. Practitioners of so-called alternative medicine (SCAM) are no exception.
This study aimed to evaluate the potential for inhalation of essential oils to improve energy levels among otherwise healthy female survivors of acute COVID-19 who experience a lack of energy more than five months after recovery.
This was a randomized double-blind, placebo-controlled trial to evaluate the potential for inhalation of Longevity™, a proprietary essential oil blend manufactured by Young Living Essential Oils (Lehi, Utah, USA), on energy levels among female survivors of COVID-19 who continue to experience fatigue more than 5 months recovery from the acute infection. Forty women were randomized to two groups: intervention and placebo. The placebo product contained an inert, odorless fractionated coconut oil. Both groups inhaled the assigned product twice daily for fourteen consecutive days. Fatigue scores were measured using the Multidimensional Fatigue Symptom Inventory (MFSI). Secondary outcomes included scores on each of the MFSI’s ten subscales.
Individuals who inhaled the essential oil blend for 2 weeks had significantly lower fatigue scores after controlling for baseline scores, employment status, BMI, olfactory function, and time since diagnosis, with a large effect size (F (1,39) = 6.15, p = .020, partial eta squared = 0.198). Subscale analysis identified subscales of vigor, as well as global, behavioral, general, and mental fatigue as benefiting from the intervention. This study provides evidence that a proprietary aromatherapy blend can significantly improve energy levels among women who are experiencing fatigue after recovering from COVID-19.
The authors concluded that the use of aromatherapy with Longevity™ essential oil blend to boost energy levels in women who have recovered from COVID-19 provides a novel, non-invasive approach to improving quality of life in this population. This intervention is particularly beneficial for global and mental fatigue, as well as vigor. Other subdomains may experience improvements to energy levels with a smaller effect size; future studies should be conducted to explore this potential.
This trial was funded by Young Living Essential Oils. Perhaps, this explains why there is no mention of the elephant in the room: the trial was not blind! Participants in the verum group knew that they received aromatherapy. Likewise, participants in the placebo group knew that they received the placebo.
Could this fact have influenced the outcome? Certainly!
Could the trial have been designed better? Certainly!
All the investigators needed to do is to use a nice-smelling oil that, according to aromatherapists, does not boost energy, as the placebo.
As it stands, we have no idea whether the authors’ assumption that the verum oil caused the effect is true.
Pity!
Or maybe not?
Perhaps Young Living Essential Oils, the sponsor of the study and producer of the oil never wanted to know the truth. Maybe they are happy to abuse science as a marketing tool?
Osteopathic visceral manipulation (VM) is a bizarre so-called alternative medicine (SCAM) that has been featured on this blog with some regularity, e.g.:
- Osteopathic visceral manipulation: a new study fails to convince anyone
- Visceral manipulation…you couldn’t make it up
- Intravaginal manipulations by (German) osteopaths: a new low point for clinical research into alternative medicine?
- Visceral osteopathy is implausible and does not work … SO, LET’S FORGET ABOUT IT ONCE AND FOR ALL
Rigorous trials fail to show that it works for anything. So, the obvious solution to this dilemma is to conduct dodgy trials!
This study tested the effects of VM on dysmenorrhea, irregular, delayed, and/or absent menses, and premenstrual symptoms in PCOS patients.
Thirty Egyptian women with polycystic ovary syndrome (PCOS), with menstruation-related complaints and free from systematic diseases and/or adrenal gland abnormalities, participated in a single-blinded, randomized controlled trial. They were recruited from the women’s health outpatient clinic in the faculty of physical therapy at Cairo University, with an age of 20-34 years, and a body mass index (BMI) ≥25, <30 kg/m2. Patients were randomly allocated into two equal groups (15 patients); the control group received a low-calorie diet for 3 months, and the study group that received the same hypocaloric diet added to VM to the pelvic organs and their related structures for eight sessions over 3 months. Evaluations for body weight, BMI, and menstrual problems were done by weight-height scale, and menstruation-domain of Polycystic Ovary Syndrome Health-Related Quality of Life Questionnaire (PCOSQ), respectively, at baseline and after 3 months from interventions. Data were described as mean, standard deviation, range, and percentage whenever applicable.
Of 60 Egyptian women with PCOS, 30 patients were included, with baseline mean age, weight, BMI, and a menstruation domain score of 27.5 ± 2.2 years, 77.7 ± 4.3 kg, 28.6 ± 0.7 kg/m2, and 3.4 ± 1.0, respectively, for the control group, and 26.2 ± 4.7 years, 74.6 ± 3.5 kg, 28.2 ± 1.1 kg/m2, and 2.9 ± 1.0, respectively, for the study group. Out of the 15 patients in the study group, uterine adhesions were found in 14 patients (93.3%), followed by restricted uterine mobility in 13 patients (86.7%), restricted ovarian/broad ligament mobility (9, 60%), and restricted motility (6, 40%). At baseline, there was no significant difference (p>0.05) in any of the demographics (age, height), or dependent variables (weight, BMI, menstruation domain score) among both groups. Post-study, there was a statistically significant reduction (p=0.000) in weight, and BMI mean values for the diet group (71.2 ± 4.2 kg, and 26.4 ± 0.8 kg/m2, respectively) and the diet + VM group (69.2 ± 3.7 kg; 26.1 ± 0.9 kg/m2, respectively). For the improvement in the menstrual complaints, a significant increase (p<0.05) in the menstruation domain mean score was shown in the diet group (3.9 ± 1.0), and the diet + VM group (4.6 ± 0.5). On comparing both groups post-study, there was a statistically significant improvement (p=0.024) in the severity of menstruation-related problems in favor of the diet + VM group.
The authors concluded that VM yielded greater improvement in menstrual pain, irregularities, and premenstrual symptoms in PCOS patients when added to caloric restriction than utilizing the low-calorie diet alone in treating that condition.
WHERE TO START?
- Tiny sample size.
- A trail design (A+B vs B) which will inevitably generate a positive result.
- Questionable ethics.
VM is a relatively invasive and potentially embarrassing intervention for any woman; I imagine that this is all the more true in Egypt. In such circumstances, it is mandatory to ask whether a planned study is ethically justifiable. I would answer this question related to an implausible treatment like VM with a straight NO!
I realize that there may be people who disagree with me. But even those guys should accept that, at the very minimum, such a study must be designed such that it leads to a clear answer – is VM effective or not? The present trial merely suggests that the placebo effect associated with VM is powerful (which is hardly surprising for a therapy like VM).
A recent article in LE PARISIEN entitled “L’homéopathie vétérinaire, c’est sans effet… mais pas sans risque” – Veterinary homeopathy is without effect … but not without risk, tells it like it is. Here are a few excerpts that I translated for you.
More than 77% of French people have tried homeopathy in their lifetime. But have you ever given it to your pet? Harmless in most cases, its use can be dangerous when it replaces a treatment whose effectiveness is scientifically proven … from a safety point of view, the tiny granules are indeed irreproachable: their use does not induce any drug interaction or undesirable side effects, nor does it run the risk of overdosing or addiction … homeopathic preparations owe their harmlessness to their lack of proper effects. “Neither in human medicine nor in veterinary medicine, at the current stage, clinical studies of all levels do not provide sufficient scientific evidence to support the therapeutic efficacy of homeopathic preparations”, stated the French Veterinary Academy in May 2021. These conclusions are in line with those of the French Academies of Medicine and Pharmacy, the British Royal College of Veterinary Surgeons, and all the international scientific bodies that have given their opinion on the subject.
Therefore, when homeopathy delays diagnosis or is used in place of proven effective treatments, its use represents a “loss of opportunity” for your pet. The greatest danger of homeopathy is not that the remedies are ineffective, but that some homeopaths believe that their therapies can be used as a substitute for genuine medical treatment,” summarizes a petition to the UK veterinary regulatory body signed by more than 1,000 British veterinarians. At best, this claim is misleading and, at worst, it can lead to unnecessary suffering and death.”
But how can we explain the number of testimonies from pet owners who say that “it works”? “I am very satisfied with the Kalium Bichromicum granules for my cat with an eye ulcer, which is healing very well”… These improvements, real or supposed, can be explained by “contextual effects”, among which the famous placebo effect (which is not specific to humans), your subjective interpretation of his symptoms, or the natural history of the disease.
When these contextual effects are ignored or misunderstood, the spontaneous resolution or reduction of the disease can be wrongly attributed to homeopathy, and thus maintain the illusion of its effectiveness. This confusion is all the more likely because homeopathy owes much of its popularity to its use to treat “everyday ailments”: nausea, allergies, fatigue, bruises, nervousness, etc., which tend to get better on their own with time, or which have a fluctuating expression…
In April 2019, the association published an open letter addressed to the National Council of the Order of Veterinarians, calling on it to take a position on the compatibility of homeopathy with the “ethical and scientific requirements” of the profession. The organization, whose official function is to guarantee the quality of the service rendered to the public by the 20,000 veterinarians practicing in France, issued its conclusions last October. It invited veterinary training centers to remove homeopathy from their curricula, under penalty of having their accreditation withdrawn, and thus their ability to deliver training credits.
In my view, this is a remarkably good and informative text. How often do homeopathy fans claim IT WORKS FOR ANIMALS AND THUS CANNOT BE A PLACEBO! The truth is that, as we have so often discussed on this blog, homeopathy does not work beyond placebo for animals. This renders veterinary homeopathy:
- a waste of money,
- potentially dangerous,
- in the worst cases a form of animal abuse.
My advice is that, as soon as a vet recommends homeopathy, you look for the exit.
Horticultural therapy (HT)?
What on earth is that?
Don’t worry, it was new to me too and I first thought of the treatment of plants.
HT is said to be a “time-proven practice. The therapeutic benefits of garden environments have been documented since ancient times. In the 19th century, Dr. Benjamin Rush, a signer of the Declaration of Independence and recognized as the “Father of American Psychiatry,” was first to document the positive effect working in the garden had on individuals with mental illness. In the 1940s and 1950s, rehabilitative care of hospitalized war veterans significantly expanded acceptance of the practice. No longer limited to treating mental illness, horticultural therapy practice gained in credibility and was embraced for a much wider range of diagnoses and therapeutic options. Today, horticultural therapy is accepted as a beneficial and effective therapeutic modality. It is widely used within a broad range of rehabilitative, vocational, and community settings. Horticultural therapy techniques are employed to assist participants to learn new skills or regain those that are lost. Horticultural therapy helps improve memory, cognitive abilities, task initiation, language skills, and socialization. In physical rehabilitation, horticultural therapy can help strengthen muscles and improve coordination, balance, and endurance. In vocational horticultural therapy settings, people learn to work independently, problem solve, and follow directions. Horticultural therapists are professionals with specific education, training, and credentials in the use of horticulture for therapy and rehabilitation. Read the formal definition of the role of horticultural therapists.”
As always, the question is DOES IT WORK?
This systematic review and meta-analysis aimed to evaluate HT for general health in older adults. Electronic databases as well as grey literature databases, and clinical trials registers were searched from inception to March 2021. Randomized controlled trials (RCTs), quasi-RCTs (QRCTs), and cohort studies about HT for adults aged over 60 were included in this review. Outcome measures were physical function, quality of life, BMI, mood tested by self-reported questionnaire and the expression of the immune cells.
Fifteen studies (thirteen RCTs and two cohort studies) involving 1046 older participants were included. Meta-analysis showed that HT resulted in better quality of life (MD 2.09, 95% CI [1.33, 2.85], P<0. 01) and physical function (SMD 0.82, 95% [0.36, 1.29], P<0.01) compared with no-gardener; the similar findings showed in BMI (SMD -0.30, 95% [-0.57, -0.04], P = 0.02) and mood tested by self-reported questionnaire (SMD 2.80, 95% CI [1.82, 3.79], P<0. 01). And HT might be beneficial for blood pressure and immunity, while all the evidence was moderate-quality judged by GRADE.
The authors concluded that HT may improve physical function and quality of life in older adults, reduce BMI and enhance positive mood. A suitable duration of HT may be between 60 to 120 minutes per week lasting 1.5 to 12 months. However, it remains unclear as to what constitutes an optimal recommendation.
I have considerable problems with this review and its conclusion:
- It is simply untrue that there were 13 RCTs; several of these studies were clearly not randomized.
- Most of the studies are of very poor quality. For instance, they often did not make the slightest attempt to control for non-specific effects, yet they concluded that the observed outcome was a specific effect of HT.
My biggest problem does, however, not relate to methodological issues. My main issue with this paper is one of definition. What is a ‘therapy’ and what not? If we call a bit of gardening a ‘therapy’ are we not descending to the level of those who call a bit of shopping ‘retail therapy’? To put it differently, is HT superior to retail therapy? And do we need RCTs to answer this question?
What is wrong with encouraging people who like gardening to just do it? I, for instance, like drumming; but I do not believe we need a few RCTs to prove that it is healthy. Not every past-time or hobby that makes you feel good is a therapy and needs to be scrutinized as such.
The new issue of the BMJ carries an article on acupuncture that cries out for a response. Here, I show you the original article followed by my short comments. For clarity, I have omitted the references from the article and added references that refer to my comments.
_________________________________________
Conventional allopathic medicine [1]—medications and surgery [2] used in conventional systems of medicine to treat or prevent disease [3]—is often expensive, can cause side effects and harm, and is not always the optimal treatment for long term conditions such as chronic pain [4]. Where conventional treatments have not been successful, acupuncture and other traditional and complementary medicines have potential to play a role in optimal patient care [5].
According to the World Health Organisation (WHO) 2019 global report, acupuncture is widely used across the world. [6] In some countries acupuncture is covered by health insurance and established regulations. [7] In the US, practitioners administer over 10 million acupuncture treatments annually. [6] In the UK, clinicians administer over 4 million acupuncture treatments annually, and it is provided on the NHS. [6]
Given the widespread use of acupuncture as a complementary therapy alongside conventional medicine, there has been an increase in global research interest and funding support over recent decades. In 2009, the European Commission launched a Good Practice in Traditional Chinese Medicine Research (GP-TCM) funding initiative in 19 countries. [7] The GP-TCM grant aimed to investigate the safety and efficacy of acupuncture as well as other traditional Chinese medicine interventions.
In China, acupuncture is an important focus of the national research agenda and receives substantial research funding. [8] In 2016, the state council published a national strategy supporting universal access to acupuncture by 2020. China has established more than 79 evidence-based traditional Chinese medicine or integrative medicine research centers. [9]
Given the broad clinical application and rapid increase in funding support for acupuncture research, researchers now have additional opportunities to produce high-quality studies. However, for this to be successful, acupuncture research must address both methodological limitations and unique research challenges.
This new collection of articles, published in The BMJ, analyses the progress of developing high quality research studies on acupuncture, summarises the current status, and provides critical methodological guidance regarding the production of clinical evidence on randomised controlled trials, clinical practice guidelines and health economic evidence. It also assesses the number and quality of systematic reviews of acupuncture. [10] We hope that the collection will help inform the development of clinical practice guidelines, health policy, and reimbursement decisions. [11]
The articles document the progress of acupuncture research. In our view, the emerging evidence base on the use of acupuncture warrants further integration and application of acupuncture into conventional medicine. [12] National, regional, and international organisations and health systems should facilitate this process and support further rigorous acupuncture research.
Footnotes
This article is part of a collection funded by the special purpose funds for the belt and road, China Academy of Chinese Medical Sciences, National Natural Science Foundation of China, the National Center for Complementary and Integrative Health, the Innovation Team and Talents Cultivation Program of the National Administration of Traditional Chinese Medicine, the Special Project of “Lingnan Modernization of Traditional Chinese Medicine” of the 2019 Guangdong Key Research and Development Program, and the Project of First Class Universities and High-level Dual Discipline for Guangzhou University of Chinese Medicine. The BMJ commissioned, peer reviewed, edited, and made the decision to publish. Kamran Abbasi was the lead editor for The BMJ. Yu-Qing Zhang advised on commissioning for the collection, designed the topic of the series, and coordinated the author teams. Gordon Guyatt provided valuable advice and guidance. [13]
1. Allopathic medicine is the term Samuel Hahnemann coined for defaming conventional medicine. Using it in the first sentence of the article sets the scene very well.
2. Medicine is much more than ‘medications and surgery’. To imply otherwise is a strawman fallacy.
3. What about rehabilitation medicine?
4. ‘Conventional medicine is not always the optimal treatment’? This statement is very confusing and wrong. It is true that conventional medicine is not always effective. However, it is by definition the best we currently have and therefore it IS optimal.
5. Another fallacy: non sequitur
6. Another fallacy: appeal to popularity.
7. Yet another fallacy: appeal to authority.
8. TCM is heavily promoted by China not least because it is a most lucrative source of income.
9. Several research groups have shown that 100% of acupuncture research coming out of China report positive results. This casts serious doubt on the reliability of these studies (see, for instance, here, here, and here).
10. It has been noted that more than 80 percent of clinical data from China is fabricated.
11. Based on the points raised above, it seems to me that the collection’s aim is not to provide objective information but uncritical promotion.
12. I find it telling that the authors do not even consider the possibility that rigorous research might demonstrate that acupuncture cannot generate more good than harm.
13. This statement essentially admits that the series of articles constitutes paid advertising for TCM. The BMJ’s peer-review process must have been less than rigorous in this case.