placebo
I recently came across a truly baffling article. As it is in German, I translated it for you:
Supply shortages have kept pharmacies on tenterhooks for months, with more than 400 common medicines missing. The German Central Association of Homeopathic Doctors (DZVhÄ) suggests switching to alternative medicine as a solution: “We have homeopathic medicines that have been tried and tested in practice for more than 200 years and can replace many medicines that are currently not available,” says the president of the DZVhÄ , Dr Michaela Geiger.
The DZVhÄ is convinced that homeopathic medical practices can replace fever-reducing medicines, but in many cases also antibiotics and much more. However, Geiger qualifies: “Due to our medical training, we also know that cancer drugs such as the often cited Tamoxifen cannot be replaced by homeopathy”.
The homeopathic doctors respond directly to the sharpest argument of their critics: “But let’s assume that homeopathy only works via the placebo effect, as is being rumored, even then it would be an option, especially if other options are lacking,” says DZVhÄ vice-president Dr. Ulf Riker. Since homeopathically trained doctors can judge the general course of a disease, they can also distinguish a placebo effect from a medicinal effect.
…
If fever medication for children is lacking, parents should not be deprived of another “therapy option”, Riker said. “If you do not get your conventional fever medication in the coming weeks, visit a specialist pharmacy for naturopathy and homeopathy. If you are due for a medical consultation, experienced homeopathic doctors can prescribe a suitable homeopathic medicine for you,” he says.
Why do I find this so intriguing?
Essentially, what we have learned from the article is the following:
- “Tried and tested in practice for more than 200 years” is ‘homeopathy speak’ for “effective”, even if the evidence tells us otherwise.
- Homeopathic remedies can replace many evidence-based conventional medications such as fever-reducing medicines, antibiotics, and much more, even if the evidence tells us otherwise.
- Homeopaths know that cancer drugs cannot be replaced by homeopathy – except for those homeopaths who seem to have forgotten this simple lesson.
- Homeopathic placebos are a realistic option when there is a supply problem with effective drugs, even if the evidence tells us otherwise.
- Homeopathically trained doctors can distinguish a placebo effect from a medicinal effect, even if there is no evidence that any clinician can reliably do this.
- Homeopathic doctors prescribe suitable homeopathic medicine. Suitable for whom? As it is ineffective, it is unsuitable for the patient. Therefore, Riker is probably talking about the homeopath.
So, what have we really learned from this article? I don’t know about you, but I got the impression that the president and the vice president of the DZVhÄ do not seem to mind putting patients in danger, as long as they can promote homeopathy.
Is acupuncture more than a theatrical placebo? Acupuncture fans are convinced that the answer to this question is YES. Perhaps this paper will make them think again.
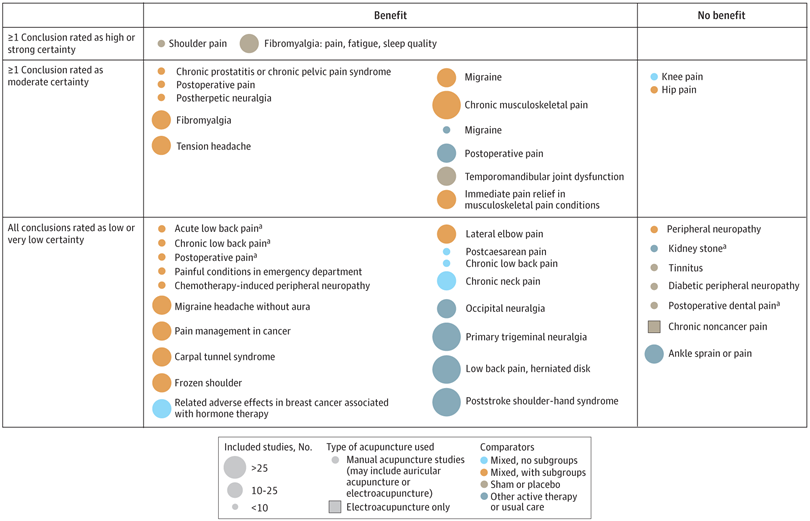
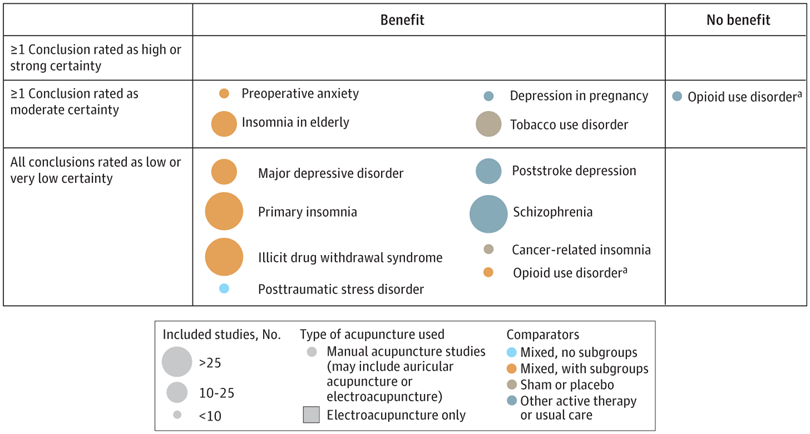
A new analysis mapped the systematic reviews, conclusions, and certainty or quality of evidence for outcomes of acupuncture as a treatment for adult health conditions. Computerized search of PubMed and 4 other databases from 2013 to 2021. Systematic reviews of acupuncture (whole body, auricular, or electroacupuncture) for adult health conditions that formally rated the certainty, quality, or strength of evidence for conclusions. Studies of acupressure, fire acupuncture, laser acupuncture, or traditional Chinese medicine without mention of acupuncture were excluded. Health condition, number of included studies, type of acupuncture, type of comparison group, conclusions, and certainty or quality of evidence. Reviews with at least 1 conclusion rated as high-certainty evidence, reviews with at least 1 conclusion rated as moderate-certainty evidence and reviews with all conclusions rated as low- or very low-certainty evidence; full list of all conclusions and certainty of evidence.
A total of 434 systematic reviews of acupuncture for adult health conditions were found; of these, 127 reviews used a formal method to rate the certainty or quality of evidence of their conclusions, and 82 reviews were mapped, covering 56 health conditions. Across these, there were 4 conclusions that were rated as high-certainty evidence and 31 conclusions that were rated as moderate-certainty evidence. All remaining conclusions (>60) were rated as low- or very low-certainty evidence. Approximately 10% of conclusions rated as high or moderate-certainty were that acupuncture was no better than the comparator treatment, and approximately 75% of high- or moderate-certainty evidence conclusions were about acupuncture compared with a sham or no treatment.
Three evidence maps (pain, mental conditions, and other conditions) are shown below
The authors concluded that despite a vast number of randomized trials, systematic reviews of acupuncture for adult health conditions have rated only a minority of conclusions as high- or moderate-certainty evidence, and most of these were about comparisons with sham treatment or had conclusions of no benefit of acupuncture. Conclusions with moderate or high-certainty evidence that acupuncture is superior to other active therapies were rare.
These findings are sobering for those who had hoped that acupuncture might be effective for a range of conditions. Despite the fact that, during recent years, there have been numerous systematic reviews, the evidence remains negative or flimsy. As 34 reviews originate from China, and as we know about the notorious unreliability of Chinese acupuncture research, this overall result is probably even more negative than the authors make it out to be.
Considering such findings, some people (including the authors of this analysis) feel that we now need more and better acupuncture trials. Yet I wonder whether this is the right approach. Would it not be better to call it a day, concede that acupuncture generates no or only relatively minor effects, and focus our efforts on more promising subjects?
This double-blind, randomized study assessed the effectiveness of physiotherapy instrument mobilization (PIM) in patients with low back pain (LBP) and compared it with the effectiveness of manual mobilization.
Thirty-two participants with LBP were randomly assigned to one of two groups:
- The PIM group received lumbar mobilization using an activator instrument, stabilization exercises, and education.
- The manual group received lumbar mobilization using a pisiform grip, stabilization exercises, and education.
Both groups had 4 treatment sessions over 2-3 weeks. The following outcomes were measured before the intervention, and after the first and fourth sessions:
- Numeric Pain Rating Scale (NPRS),
- Oswestry Disability Index (ODI) scale,
- Pressure pain threshold (PPT),
- lumbar spine range of motion (ROM),
- lumbar multifidus muscle activation.
There were no differences between the PIM and manual groups in any outcome measures. However, over the period of study, there were improvements in both groups in NPRS (PIM: 3.23, Manual: 3.64 points), ODI (PIM: 17.34%, Manual: 14.23%), PPT (PIM: ⩽ 1.25, Manual: ⩽ 0.85 kg.cm2), lumbar spine ROM (PIM: ⩽ 9.49∘, Manual: ⩽ 0.88∘), and/or lumbar multifidus muscle activation (percentage thickness change: PIM: ⩽ 4.71, Manual: ⩽ 4.74 cm; activation ratio: PIM: ⩽ 1.17, Manual: ⩽ 1.15 cm).
The authors concluded that both methods of lumbar spine mobilization demonstrated comparable improvements in pain and disability in patients with LBP, with neither method exhibiting superiority over the other.
If this conclusion is meant to tell us that both treatments were equally effective, I beg to differ. The improvements documented here are consistent with improvements caused by the natural history of the condition, regression towards the mean, and placebo effects. The data do not prove that they are due to the treatments. On the contrary, they seem to imply that patients get better no matter what therapy is used. Thus, I feel that the results are entirely in keeping with the hypothesis that spinal mobilization is a placebo treatment.
So, allow me to re-phrase the authors’ conclusion as follows:
Lumbar mobilizations do not seem to have specific therapeutic effects and might therefore be considered to be ineffective for LBP.
Acupuncture is emerging as a potential therapy for relieving pain, but the effectiveness of acupuncture for relieving low back and/or pelvic pain (LBPP) during pregnancy remains controversial. This meta-analysis aimed to investigate the effects of acupuncture on pain, functional status, and quality of life for women with LBPP pain during pregnancy.
The authors included all RCTs evaluating the effects of acupuncture on LBPP during pregnancy. Data extraction and study quality assessments were independently performed by three reviewers. The mean differences (MDs) with 95% CIs for pooled data were calculated. The primary outcomes were pain, functional status, and quality of life. The secondary outcomes were overall effects (a questionnaire at a post-treatment visit within a week after the last treatment to determine the number of people who received good or excellent help), analgesic consumption, Apgar scores >7 at 5 min, adverse events, gestational age at birth, induction of labor and mode of birth.
Ten studies, reporting on a total of 1040 women, were included. Overall, acupuncture
- relieved pain during pregnancy (MD=1.70, 95% CI: (0.95 to 2.45), p<0.00001, I2=90%),
- improved functional status (MD=12.44, 95% CI: (3.32 to 21.55), p=0.007, I2=94%),
- improved quality of life (MD=−8.89, 95% CI: (−11.90 to –5.88), p<0.00001, I2 = 57%).
There was a significant difference in overall effects (OR=0.13, 95% CI: (0.07 to 0.23), p<0.00001, I2 = 7%). However, there was no significant difference in analgesic consumption during the study period (OR=2.49, 95% CI: (0.08 to 80.25), p=0.61, I2=61%) and Apgar scores of newborns (OR=1.02, 95% CI: (0.37 to 2.83), p=0.97, I2 = 0%). Preterm birth from acupuncture during the study period was reported in two studies. Although preterm contractions were reported in two studies, all infants were in good health at birth. In terms of gestational age at birth, induction of labor, and mode of birth, only one study reported the gestational age at birth (mean gestation 40 weeks).
The authors concluded that acupuncture significantly improved pain, functional status and quality of life in women with LBPP during the pregnancy. Additionally, acupuncture had no observable severe adverse influences on the newborns. More large-scale and well-designed RCTs are still needed to further confirm these results.
What should we make of this paper? 
In case you are in a hurry: NOT A LOT!
In case you need more, here are a few points:
- many trials were of poor quality;
- there was evidence of publication bias;
- there was considerable heterogeneity within the studies.
The most important issue is one studiously avoided in the paper: the treatment of the control groups. One has to dig deep into this paper to find that the control groups could be treated with “other treatments, no intervention, and placebo acupuncture”. Trials comparing acupuncture combined plus other treatments with other treatments were also considered to be eligible. In other words, the analyses included studies that compared acupuncture to no treatment at all as well as studies that followed the infamous ‘A+Bversus B’ design. Seven studies used no intervention or standard of care in the control group thus not controlling for placebo effects.
Nobody can thus be in the slightest surprised that the overall result of the meta-analysis was positive – false positive, that is! And the worst is that this glaring limitation was not discussed as a feature that prevents firm conclusions.
Dishonest researchers?
Biased reviewers?
Incompetent editors?
Truly unbelievable!!!
In consideration of these points, let me rephrase the conclusions:
The well-documented placebo (and other non-specific) effects of aacupuncture improved pain, functional status and quality of life in women with LBPP during the pregnancy. Unsurprisingly, acupuncture had no observable severe adverse influences on the newborns. More large-scale and well-designed RCTs are not needed to further confirm these results.
PS
I find it exasperating to see that more and more (formerly) reputable journals are misleading us with such rubbish!!!
The aim of this evaluator-blinded randomized clinical trial was to determine if manual therapy added to a therapeutic exercise program produced greater improvements than a sham manual therapy added to the same exercise program in patients with non-specific shoulder pain. 
Forty-five subjects were randomly allocated into one of three groups:
- manual therapy (glenohumeral mobilization technique and rib-cage technique);
- thoracic sham manual therapy (glenohumeral mobilization technique and rib-cage sham technique);
- sham manual therapy (sham glenohumeral mobilization technique and rib-cage sham technique).
All groups also received a therapeutic exercise program. Pain intensity, disability, and pain-free active shoulder range of motion were measured post-treatment and at 4-week and 12-week follow-ups. Mixed-model analyses of variance and post hoc pairwise comparisons with Bonferroni corrections were constructed for the analysis of the outcome measures.
All groups reported improved pain intensity, disability, and pain-free active shoulder range of motion. However, there were no between-group differences in these outcome measures.
The authors concluded that the addition of the manual therapy techniques applied in the present study to a therapeutic exercise protocol did not seem to add benefits to the management of subjects with non-specific shoulder pain.
What does that mean?
I think it means that the improvements observed in this study were due to 1) exercise and 2) a range of non-specific effects, and that they were not due to the manual techniques tested.
I cannot say that I find this enormously surprising. But I would also find it unsurprising if fans of these methods would claim that the results show that the physios applied the techniques not correctly.
In any case, I feel this is an interesting study, not least because of its use of sham therapy. But I somehow doubt that the patients were unable to distinguish sham from verum. If so, the study was not patient-blind which obviously is difficult to achieve with manual treatments.
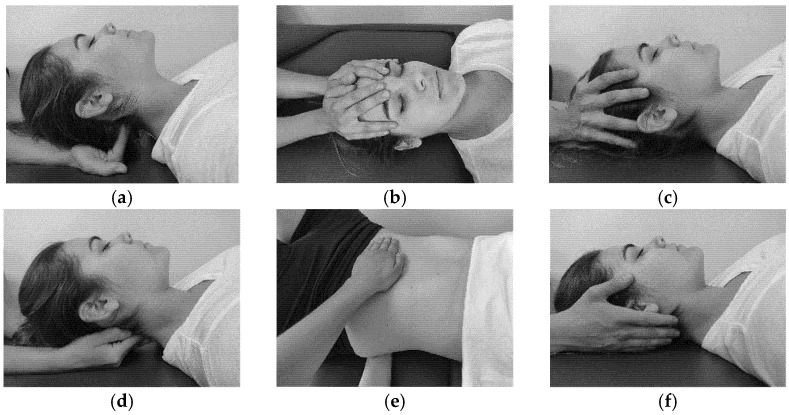
The aim of this study was to evaluate the effectiveness of craniosacral therapy on different features in migraine patients.
Fifty individuals with migraine were randomly divided into two groups (n = 25 per group):
- craniosacral therapy group (CTG),
- sham control group (SCG).
The interventions were carried out with the patient in the supine position. The CTG received a manual therapy treatment focused on the craniosacral region including five techniques, and the SCG received a hands-on placebo intervention. After the intervention, individuals remained supine with a neutral neck and head position for 10 min, to relax and diminish tension after treatment. The techniques were executed by the same experienced physiotherapist in both groups.
The analyzed variables were pain, migraine severity, and frequency of episodes, functional, emotional, and overall disability, medication intake, and self-reported perceived changes, at baseline, after a 4-week intervention, and at an 8-week follow-up.
After the intervention, the CTG significantly reduced pain (p = 0.01), frequency of episodes (p = 0.001), functional (p = 0.001) and overall disability (p = 0.02), and medication intake (p = 0.01), as well as led to a significantly higher self-reported perception of change (p = 0.01), when compared to SCG. The results were maintained at follow-up evaluation in all variables.
The authors concluded that a protocol based on craniosacral therapy is effective in improving pain, frequency of episodes, functional and overall disability, and medication intake in migraineurs. This protocol may be considered as a therapeutic approach in migraine patients.
Sorry, but I disagree!
And I have several reasons for it:
- The study was far too small for such strong conclusions.
- For considering any treatment as a therapeutic approach in migraine patients, we would need at least one independent replication.
- There is no plausible rationale for craniosacral therapy to work for migraine.
- The blinding of patients was not checked, and it is likely that some patients knew what group they belonged to.
- There could have been a considerable influence of the non-blinded therapists on the outcomes.
- There was a near-total absence of a placebo response in the control group.
Altogether, the findings seem far too good to be true.
This study aimed to evaluate the number of craniosacral therapy sessions that can be helpful to obtain a resolution of the symptoms of infantile colic and to observe if there are any differences in the evolution obtained by the groups that received a different number of Craniosacral Therapy sessions at 24 days of treatment, compared with the control group which did not received any treatment.
Fifty-eight infants with colic were randomized into two groups:
- 29 babies in the control group received no treatment;
- babies in the experimental group received 1-3 sessions of craniosacral therapy (CST) until symptoms were resolved.
Evaluations were performed until day 24 of the study. Crying hours served as the primary outcome measure. The secondary outcome measures were the hours of sleep and the severity, measured by an Infantile Colic Severity Questionnaire (ICSQ).
Statistically significant differences were observed in favor of the experimental group compared to the control group on day 24 in all outcome measures:
- crying hours (mean difference = 2.94, at 95 %CI = 2.30-3.58; p < 0.001);
- hours of sleep (mean difference = 2.80; at 95 %CI = – 3.85 to – 1.73; p < 0.001);
- colic severity (mean difference = 17.24; at 95 %CI = 14.42-20.05; p < 0.001).
Also, the differences between the groups ≤ 2 CST sessions (n = 19), 3 CST sessions (n = 10), and control (n = 25) were statistically significant on day 24 of the treatment for crying, sleep and colic severity outcomes (p < 0.001).
The authors concluded that babies with infantile colic may obtain a complete resolution of symptoms on day 24 by receiving 2 or 3 CST sessions compared to the control group, which did not receive any treatment.
Why do SCAM researchers so often have no problem leaving the control group of patients in clinical trials without any treatment at all, while shying away from administering a placebo? Is it because they enjoy being the laughingstock of the science community? Probably not.
I suspect the reason might be that often they know that their treatments are placebos and that their trials would otherwise generate negative findings. Whatever the reasons, this new study demonstrates three things many of us already knew:
- Colic in babies always resolves on its own but can be helped by a placebo response (e.g. via the non-blinded parents), by holding the infant, and by paying attention to the child.
- Flawed trials lend themselves to drawing the wrong conclusions.
- Craniosacral therapy is not biologically plausible and most likely not effective beyond placebo.
One of the numerous conditions chiropractors, osteopaths, and other manual therapists claim to treat effectively is tension-type headache (TTH). For this purpose, they (in particular, chiropractors) often use high-velocity, low-amplitude manipulations of the neck. They do so despite the fact that the evidence for these techniques is less than convincing.
This systematic review evaluated the evidence about the effectiveness of manual therapy (MT) on pain intensity, frequency, and impact of pain in individuals with tension-type headache (TTH).
Medline, Embase, Scopus, Web of Science, CENTRAL, and PEDro were searched in June 2020. Randomized clinical trials that applied MT not associated with other interventions for TTH were selected. The level of evidence was synthesized using GRADE, and Standardized Mean Differences (SMD) were calculated for meta-analysis.
Fifteen studies were included with a total sample of 1131 individuals. The analyses show that high-velocity, low-amplitude techniques were not superior to no treatment in reducing pain intensity (SMD = 0.01, low evidence) and frequency (SMD = -0.27, moderate evidence). Soft tissue interventions were superior to no treatment in reducing pain intensity (SMD = -0.86, low evidence) and frequency of pain (SMD = -1.45, low evidence). Dry needling was superior to no treatment in reducing pain intensity (SMD = -5.16, moderate evidence) and frequency (SMD = -2.14, moderate evidence). Soft tissue interventions were not superior to no treatment and other treatments on the impact of headache.
The authors concluded that manual therapy may have positive effects on pain intensity and frequency, but more studies are necessary to strengthen the evidence of the effects of manual therapy on subjects with tension-type headache. Implications for rehabilitation soft tissue interventions and dry needling can be used to improve pain intensity and frequency in patients with tension type headache. High velocity and low amplitude thrust manipulations were not effective for improving pain intensity and frequency in patients with tension type headache. Manual therapy was not effective for improving the impact of headache in patients with tension type headache.
So, this review shows that:
- soft tissue interventions are better than no treatment,
- dry needling is better than no treatment.
These two results fail to impress me. Due to a placebo effect, almost any treatment should be better than no therapy at all.
ALMOST, because high-velocity, low-amplitude techniques were not superior to no treatment in reducing the intensity and frequency of pain. This, I feel, is an important finding that needs an explanation.
As it is only logical that high-velocity, low-amplitude techniques must also produce a positive placebo effect, the finding can only mean that these manipulations also generate a negative effect that is strong enough to cancel the positive response to placebo. (In addition, they can also cause severe complications via arterial dissections, as discussed often on this blog.)
Too complicated?
Perhaps; let me, therefore, put it simply and use the blunt words of a neurologist who once was quoted saying this:
DON’T LET THE BUGGARS TOUCH YOUR NECK!
Advocates of so-called alternative medicine (SCAM) often sound like a broken record to me. They bring up the same ‘arguments’ over and over again, no matter whether they happen to be defending acupuncture, energy healing, homeopathy, or any other form of SCAM. Here are some of the most popular of these generic ‘arguments’:
1. It helped me
The supporters of SCAM regularly cite their own good experiences with their particular form of treatment and think that this is proof enough. However, they forget that any symptomatic improvement they may have felt can be the result of several factors that are unrelated to the SCAM in question. To mention just a few:
- Placebo
- Regression towards the mean
- Natural history of the disease
2. My SCAM is without risk
Since homeopathic remedies, for instance, are highly diluted, it makes sense to assume that they cannot cause side effects. Several other forms of SCAM are equally unlikely to cause adverse effects. So, the notion is seemingly correct. However, this ‘argument’ ignores the fact that it is not the therapy itself that can pose a risk, but the SCAM practitioner. For example, it is well documented – and, on this blog, we have discussed it often – that many of them advise against vaccination, which can undoubtedly cause serious harm.
3. SCAM has stood the test of time
It is true that many SCAMs have survived for hundreds or even thousands of years. It is also true that millions still use it even today. This, according to enthusiasts, is sufficient proof of SCAM’s efficacy. But they forget that many therapies have survived for centuries, only to be proved useless in the end. Just think of bloodletting or mercury preparations from past times.
4 The evidence is not nearly as negative as skeptics pretend
Yes, there are plenty of positive studies on some SCAMs This is not surprising. Firstly, from a purely statistical point of view, if we have, for instance, 1 000 studies of a particular SCAM, it is to be expected that, at the 5% level of statistical significance, about 50 of them will produce a significantly positive result. Secondly, this number becomes considerably larger if we factor in the fact that most of the studies are methodologically poor and were conducted by SCAM enthusiasts with a corresponding bias (see my ALTERNATIVE MEDICINE HALL OF FAME on this blog). However, if we base our judgment on the totality of the most robust studies, the bottom line is almost invariably that there is no overall convincingly positive result.
5. The pharmaceutical industry is suppressing SCAM
SCAM is said to be so amazingly effective that the pharmaceutical industry would simply go bust if this fact became common knowledge. Therefore Big Pharma is using its considerable resources to destroy SCAM. This argument is fallacious because:
- there is no evidence to support it,
- far from opposing SCAM, the pharmaceutical industry is heavily involved in SCAM (for example, by manufacturing homeopathic remedies, dietary supplements, etc.)
6 SCAM could save a lot of money
It is true that SCAMs are on average much cheaper than conventional medicines. However, one must also bear in mind that price alone can never be the decisive factor. We also need to consider other issues such as the risk/benefit balance. And a reduction in healthcare costs can never be achieved by ineffective therapies. Without effectiveness, there can be no cost-effectiveness.
7 Many conventional medicines are also not evidence-based
Sure, there are some treatments in conventional medicine that are not solidly supported by evidence. So why do we insist on solid evidence for SCAM? The answer is simple: in all areas of healthcare, intensive work is going on aimed at filling the gaps and improving the situation. As soon as a significant deficit is identified, studies are initiated to establish a reliable basis. Depending on the results, appropriate measures are eventually taken. In the case of negative findings, the appropriate measure is to exclude treatments from routine healthcare, regardless of whether the treatment in question is conventional or alternative. In other words, this is work in progress. SCAM enthusiasts should ask themselves how many treatments they have discarded so far. The answer, I think, is zero.
8 SCAM cannot be forced into the straitjacket of a clinical trial
This ‘argument’ surprisingly popular. It supposes that SCAM is so individualized, holistic, subtle, etc., that it defies science. The ‘argument’ is false, and SCAM advocates know it, not least because they regularly and enthusiastically cite those scientific papers that seemingly support their pet therapy.
9 SCAM is holistic
This may or may not be true, but the claim of holism is not a monopoly of SCAM. All good medicine is holistic, and in order to care for our patients holistically, we certainly do not need SCAM.
1o SCAM complements conventional medicine
This argument might be true: SCAM is often used as an adjunct to conventional treatments. Yet, there is no good reason why a complementary treatment should not be shown to be worth the effort and expense to add it to another therapy. If, for instance, you pay for an upgrade on a flight, you also want to make sure that it is worth the extra expenditure.
11 In Switzerland it works, too
That’s right, in Switzerland, a small range of SCAMs was included in basic health care by referendum. However, it has been reported that the consequences of this decision are far from positive. It brought no discernible benefit and only caused very considerable costs.
I am sure there are many more such ‘arguments’. Feel free to post your favorites!
My point here is this:
the ‘arguments’ used in defense of SCAM are not truly arguments; they are fallacies, misunderstandings, and sometimes even outright lies.
It is not often that I publish a paper with a philosopher in a leading journal of philosophy. In fact, it is the first time, and I am rather proud of it – so much so that I must show my readers (the article is freely available via the link below and I encourage everyone to read the full text) the abstract of our article entitled WHY HOMOEOPATHY IS PSEUDOSCIENCE (Synthese (2022) 200:394):
Homoeopathy is commonly recognised as pseudoscience. However, there is, to date, no systematic discussion that seeks to establish this view. In this paper, we try to fill this gap. We explain the nature of homoeopathy, discuss the notion of pseudoscience, and provide illustrative examples from the literature indicating why homoeopathy fits the
bill. Our argument contains a conceptual and an empirical part.
In the conceptual part, we introduce the premise that a doctrine qualifies as a pseudoscience if, firstly, its proponents claim scientific standing for it and, secondly, if they produce bullshit to defend it, such that, unlike science, it cannot be viewed as the most reliable knowledge on its topic. In the empirical part, we provide evidence that homoeopathy fulfils both criteria. The first is quickly established since homoeopaths often explicitly claim scientificity.
To establish the second, we dive into the pseudo-academic literature on homoeopathy to provide evidence of bullshit in the arguments of homoeopaths. Specifically, we show that they make bizarre ontological claims incompatible with natural science, illegitimately shift the burden of proof to sceptics, and mischaracterise, cherry-pick, and misreport the evidence. Furthermore, we demonstrate that they reject essential parts of established scientific methodology and use epistemically unfair strategies to immunise their doctrine against recalcitrant evidence.
And here is our conclusion:
At the beginning of the paper, we noted that homoeopathy is commonly named one of the prototypical pseudosciences. However, there has been, to date, no comprehensive discussion as to what makes it a pseudoscience. Moreover, the problem is not trivial since the most well-known and influential demarcation criteria, such as Popper’s falsifiability criterion and Kuhn’s problem-solving criterion, cannot account for it, as we have shown. We have tried to fill this research gap using a novel bullshitology-based approach to the demarcation problem. Following this approach, we have argued that homoeopathy should be regarded as pseudoscience because its proponents claim scientific standing for it and produce argumentative bullshit to defend it, thus violating important epistemic standards central to science.